

The 24th International Symposium on the Autonomic Nervous System was chock full of potential insights for people with chronic fatigue syndrome. We used Dysautonomia International’s excellent overview of the relevant studies as a starting point. (Thanks to Issie for alerting me to the overview.)
Is the autonomic nervous system going to be ground zero for chronic fatigue syndrome and fibromyalgia? This overview suggests, at the very least, it’s going to be a major factor.
Dysautonomia / Dysauto – “immunomia” – The Autoimmune Connections to Dysautonomia Grow
The autoimmune connection in dysautonomia (autonomic nervous system disorders) and the autonomic nervous system connection in autoimmune disorders are growing.
Postural Orthostatic Tachycardia Syndrome (POTS)
A study suggested that POTS, a disorder associated with ME/CFS, may be an autoimmune disorder as well. Starting off their abstract by noting that POTS is often triggered by a viral infection, these Oklahoma and Vanderbilt University researchers reported that their small study (14 POTS patients) found increased alpha- and beta-adrenergic receptor activity that they were able to stop by using an alpha-adrenergic receptor blocker.

Autoimmune disorders with autonomic nervous system issues and vice versa; the autoimmune-autonomic nervous system connection is growing
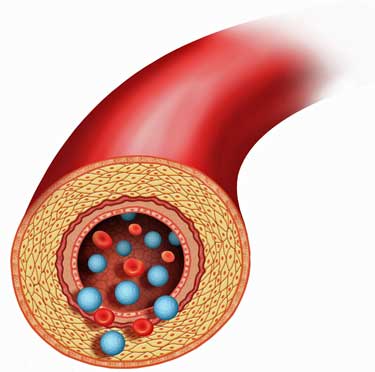
The POTS patients had elevated levels of a1AR autoantibodies and some had beta-adrenergic antibodies. The high levels of the a1AR antibodies suggested POTS patients had to produce more norepinephrine and increase their heart rates more rapidly; i.e. they had to put their sympathetic nervous system in overdrive in order to get blood out to the tissues.
The Lights’s finding of increased gene expression of all alpha– and beta-adrenergic receptors in ME/CFS compared to controls after exercise suggested that these pivotal blood vessel components were disturbed in both disorders.
The authors believe their findings provide “strong support for an autoimmune basis for the increased upright plasma norepinephrine and excessive tachycardia observed in POTS patients.”
Taking a look at few other disorders, we can see a growing autonomic nervous system/autoimmune connection and some serious overlap with chronic fatigue syndrome.
Primary Biliary Cirrhosis
We know that Dr. Julia Newton is engaged in a Rituximab trial in primary biliary cirrhosis (PBC), an autoimmune disorder with high rates of fatigue as well as autonomic issues. The overlap between this autoimmune disease and chronic fatigue syndrome in astonishing. Similar muscle pH problems occur in both PBC and ME/CFS. Newton has stated that PBC has exactly the same cardiac energetics and similar autonomic nervous system dynamics as ME/CFS. Both feature reduced heart rate variability. Autonomic and sensory nerve fiber neuropathy is common in PBC and may be common in ME/CFS and FM.
Newton appears to have found the same type of increased ‘cerebrovascular resistance’ — which I believe refers to narrowed blood vessels — in PBC as is found in POTS and ME/CFS (see below}. Newton recently proposed that people with PBC show accelerated cardiac ‘aging’. She believes the autonomic nervous system problems in PBC may simply be an attempt to compensate for deficiencies elsewhere (as do some ME/CFS and POTS researchers).
Primary biliary cirrhosis has been known to be an autoimmune disease since the 1970s. However, only in the last 6 years or so, largely due to Dr. Newton’s efforts, has anyone looked at the autonomic nervous system. Dr. Newton appears to have locked onto PBC because of the enormous fatigue issues which she believes may be the result of autonomic nervous system dysfunction. Dr. Newton has begun the same process, and has been getting similar results, in Sjogren’s Syndrome, another autoimmune disorder. It took researchers about 50 years to glom onto Sjogren’s Syndrome’s autonomic nervous system issues.
Complex Regional Pain Syndrome
On the flip side, we know that studies suggest that CRPS, which is chockfull of autonomic nervous system issues, may end up being an autoimmune disorder as well. CRPS was described decades ago, but it only became associated with autoimmunity in the last 10 years, and only seriously associated in about the last five. It can take considerable time for researchers to begin to look for and then pin down a state of autoimmunity, and, in fact, the autoimmunity present in CRPS is atypical.
ME/CFS Next?
We know autonomic nervous system problems are present in ME/CFS/FM. We know that Rituximab works in subset of ME/CFS patients. Is it just a matter of time before an autoimmune disorder is documented in subset of ME/CFS patients?
Hyperadrenergic POTS – Meet Chronic Fatigue Syndrome
An astounding case of research mimicry took place when POTS researchers essentially duplicated the results of a recent UK study on ME/CFS. This POTS study found that hyperadrenergic POTS patients hyperventilate when they stand, lowering their blood CO2 levels. This causes the blood vessels in their brains to constrict reducing blood flow to the brain.
POTS patients had an immediate 30 percent reduction in cerebral blood flow upon being tilted up. Struggling to make up the deficiency, their hearts exploded into action with their heart rates almost doubling from a normal 78 bpm to 130 bpm. They at least partially succeeded, as cardiac output — driven by the intense heart rate — remained stable.
If I’m reading this correctly, the 30 percent reduction in blood flow to the brain did not occur because of blood pooling in the legs (‘no excessive regional blood volume shifts occurred’). Rather, it occurred because narrowed blood vessels reduced blood flow to the brain.
Panic Time – Muscle sympathetic nervous activity started out normal, but it increased so much during the tilt table test that the test was stopped due to MSNA-produced feelings of panic and anxiety.
Hyperventilation – The hyperventilation that ensued that caused severely low CO2 levels. Arterial blood flows to the brain via the carotid arteries were so reduced as to produce a condition called ischemic hypoxia. Ischemic hypoxia or ‘stagnant hypoxia’ occurs when slowed movement of the blood reduces oxygen delivery to the tissues even when oxygen content and saturation of the blood is normal. The ‘Bohr effect’ which decreases CO2 levels when blood pH levels drop contributed to further hypoxia. The sympathetic nervous system apparently kicked in to try to remedy the situation by increasing blood flows, but further reduced CO levels and, as we saw, induced feelings of panic.

Too little CO2 in the blood/ too much CO2 in the atmosphere – neither is good for human or planetary health
CO2 Connection
The kicker was that giving the POTS patients carbon dioxide during the tilt test normalized the blood flows to their brains, and stopped their tachycardia (rapid heart beats) and their hyperventilation. (For some reason they did not suggest patients start breathing carbon dioxide.)
This study was more complete, but its results followed almost word for word Dr. Newton’s recent finding in a small group of chronic fatigue syndrome patients. Was she testing ME/CFS patients with hyperadrenergic POTS or were these ME/CFS patients? My guess is that they were ME/CFS patients, or maybe they were both. Or maybe it’s a moot point, and the next abstract suggests why.
Your Next Diagnosis is… POTS
In the tilt table version of an ME/CFS repeat exercise test, patients whose heart rate increased during standing but who did not meet the criteria for POTS were given another, longer, tilt test. Almost half of them ended up meeting the criteria for POTS.
This, like the repeat exercise test employed in chronic fatigue syndrome, much more accurately reflects functionality because it more reflects the stressors of every day life: getting up and down again and again, standing for long periods, etc.
This finding suggests that POTS may be much more common (and much more underdiagnosed) than previously thought, and that the diagnostic criteria should be broadened. The takeaway from this is that If you have problems standing or remaining upright, and your doctor didn’t think you have POTS, you still might.
My guess is that the more the researchers dig into the standing problem the more they’ll find, and they’re just understanding the grosser aspects of it now. Who with chronic fatigue syndrome, after all, doesn’t have some problems with standing?
The Deconditioning Theory Takes a Hit
Because deconditioning can actually cause orthostatic intolerance (OI), the question of how much deconditioning contributes to orthostatic intolerance is HUGE. One train of thought has been that a considerable number of people with ME/CFS become immobile when they become sick, and then they become orthostatically intolerant by staying in bed so much. They’re so freaked out by their symptoms at that point that they never really get up again.

Repeat after me….Deconditioning present in OI but it doesn’t cause it…Deconditioning is present in OI, but it doesn’t cause it…Decondition….
The problem is that staying in bed can cause orthostatic intolerance, and this makes it difficult to determine if orthostatic intolerance is from deconditioning or from a physiological problem.
Mayo Clinic researchers believe, though, that they have a way. A Mayo Clinic study finding that markers of deconditioning are ‘only marginally associated’ with heart rate response in a group of people with OI suggested that deconditioning is “unlikely to be the primary causative factor in orthostatic intolerance.”
They acknowledged that deconditioning is rampant in orthostatic intolerance, and reported that ‘reconditioning programs’ can be very helpful. But they concluded that deconditioning itself is only marginally relevant in causing orthostatic intolerance.
Conclusion
I think we’re getting somewhere. I think it’s time for the NIH to pony up for a Symposium on Chronic Fatigue Syndrome/POTS/Fibromyalgia and the Autonomic Nervous System.






Thanks Cort. Last year I got up from taking an echogram to go to the bathroom and when I returned for the treadmill portion my pulse was up 30-40 beats per minute. Instead of the treadmill, the doc put me on the cardiac ward for 3 days. I had no idea my pulse had increased this much and felt ok. Have no problems standing. Do you know if any of the folks who took the longer tilt test were free of symptoms and only had a significant increase in pulse?
I haven’t read the study you refer to, but I have POTS and see an autonomic specialist for it, and from what I understand from my doctor, the diagnostic criteria requires that symptoms must accompany the increase in heart rate. If you get a tilt table test, they will repeatedly ask you to report your symptoms in order to correlate them with your vitals.
However, I wear a HR monitor a lot and I can get a high HR (150+) without symptoms. There isn’t always a strong correlation between my HR and how I feel. On good days, I can be upright 30 minutes or so without symptoms, as long as I’m constantly moving and walking around. But if I stand still for 10 minutes, I’m always absolutely miserable. That’s the point of the tilt table – to make you completely still, not flexing legs, to prevent your body from relying on it’s compensatory measures. Unless you’ve stood completely still for 30 minutes or so, you may not know exactly how your body responds to standing.
Of course another possibility is (I know this is a dreaded word for us)…deconditioning. If you are deconditioned, “exercise” (in your case walking to the bathroom) could raise your HR more than normal.
Good question – heart rate does normally increase when we stand. I assume that their increases were higher than normal but didn’t meet the criteria for POTS. Normal heart rate increases are up to 30 bpm upon being tilted upright on a tilt table.
I don’t know about symptoms but my guess is that they were symptomatic on the first tilt table test. I was but otherwise tested out normal..
Thanks Elizabeth and Cort. I didnt know it could be normal for the heart to increase that much upon standing, or that a tilt test included standing perfectly still afterwards for up to 30 minutes. I thought when people say they have problems standing it could mean waiting in line for groceries, cooking, or other ADL’s where there is some movement. Interesting.
I was a bit off – it’s 30 bpm or more on the tilt table test…In the tilt table you’re strapped so that your leg muscles can’t assist you in maintaining blood flows to the upper body – it’s a more severe test of being upright than standing.
This is all fascinating.
I have some symptoms of inflammatory arthritis [without rheum blood markers], some of Sjogrens; some of psorasis; lots of osteoarthritis; and lots of FM. [and perhaps POTS???]. I believe they MUST all be linked, so would ALL be autoimmune to a degree. Not that my medical experts agree. So if there is a common trigger in the background, the autonomic nervous system is a good suspect!
Barbara
I was diagnosed with CFS in 2007 (bedridden for 3 years). I just had the most thorough tilt table test I’ve ever had on Friday with an amazing doctor. Just as this article confirmed, I didn’t becomes a POTS patient until after the “ten minute” time envelope used for POTS. However, my blood pressure dropped steadily from the moment they stood me up. At 13 minutes my heart rate went into the definition for POTS. So I completely agree that many of us must be asked to stand longer than 10 minutes, maybe even 20 or 30 (if we make it that long without passing out). I have severe orthostatic intolerance which started with the onset of a virus in June of 2007. Thanks again for a wonderful article.
Very interesting, Laura – thanks for passing that on…
And it started with a virus – Ha! The more they dig into this – the more interesting it gets…:)
Where was this great tilt table test done, I had a test that was stopped after 3 minutes and was usless. thanks,ester
I had two tilt table test (TTT) both done at Mayo in AZ. The first one was 45 minutes done through Cardiology and with that one I nearly passed out, and I’m not a POTS patient that faints. But this one had my body demonstrate all my POTS symptoms.- including some pretty bad tremors when its bad. The second TTT was a 10 minute one, done through Neurology. I showed up with POTS both times. It depends on what type of doctor runs the test and if they are aware of POTS and know what they are seeing when it presents itself.
Issie
I also contracted either a viral or bacterial infection in one lung,upon travelling fro Europe back into Canada…Interesting fact of mine is…I had 10 very dirty bearded & long haired men seated across from me at the very back rows of the Plane…7 days upon my arrival home..I had a fever of 104F and was completely unable to walk or stand from the severe pain in ALL of joints and therefore Hospitalized for 10 days and was semi-comatose for 7 of them.!! This happened in 1995 and have not been my normal healthy self since.! I have huge issues with standing & dizziness and every single joint,even toes & fingers are affected with chronic pain and I also break out in a hot sweat when my Bowels need to move(without constipation) I have been basically housebound ever since and still struggle to find answers to this day,in a small city in central Alberta Canada.!! I have not had the tilt test,but most everything else that is available for testing.!! My end point is this…That men with filthy beards & dirty long hair & are unkempt altogether,can carry an array of bad Pathogens.!! Then again it could have been the sick Jellyfish that stung me or other stuff in the MED. SEA that had a go at me.??I went from fit & healthy to literally bed-ridden in 10 days…Frustration & Anger haunts me all these years…HELP
What a story Maria….
It’s impossible to tell what the trigger was….the jellyfish sting, something you picked up from those men, something you ate…so many things can set whatever happened off – off. For one person it was a concussion. We just have to support our researchers and others until it becomes clear. The Canary in the Coal mine film should be very helpful – as in several ways her story is yours; athletic, fit person all of a sudden collapses – what a medical mystery it is and I’ve got to believe that as more researchers learn about it the more they’ll be interested in figuring it out.
I’M INTERESTED TO KNOW WHERE IN ALBERTA? I LIVE CLOSE TO EDMONTON. MAYBE WE CAN CONNECT??
While you’re here, look up L-Carnitine on WebMD. RP
why?
Hey Cort,
I love this! The research your talking about here is, with the exception of Professor Newton’s work, all being conduced by researchers on the Medical Advisory Board of Dysautonomia International. We are so thankful for the work they are doing – POTS antibodies (Dr. Raj at Vanderbilt), POTS hypocapnic hyperapnea (Dr. Stewart the NY Medical College), late POTS (Dr. Chemali at Eastern Virginia Medical School), and “it’s not just deconditioning” (Dr. Sandroni at Mayo). We’re huge fans of Professor Newton, so we should probably invite her to the board too!
Like you, I am increasingly convinced there is an underlying autoimmune/inflammatory connection to all of these conditions. Maybe not every single POTS/CFS/CRPS/fibro patient, but I do believe the vast majority of us have an autoimmune underpinning. It’s going to take more collaborative research to figure this out.
Are you following us on Facebook? That’s where we posted the research update from the Symposium and where we post other new autonomic research from time to time.
http://www.facebook.com/dysautonomiainternational
We posted something this evening that you might be interested in – major insurers are changing their plans to no longer cover ANY autonomic testing. We are flooding the CEO’s inbox with angry patient e-mails. Come join us!
Cheers,
Lauren
Thanks Laura
That’s a great board…Definitely get Dr. Newton on board if you can; she’s covering ANS issues in ME/CFS, Sjogrens and Primary biliary cirrhosis. She has a Rituximab study going in PBC. She’s pumping out small studies all the time..Get her on board to, if nothing else, get her in touch with Stewart, Raj and the others. I hope she joins.
Hey, everyone Dysautonomia International has a GREAT Facebook site. The reason its great is that they update it ALL THE TIME. (I just glomed onto it yesterday)….If you want to keep up on dysautonomia issues – that’s the place to do..
But oh no!!! That’s bad news about the insurers……
Great review Cort. I have felt all along that genetics came first and then autoimmune issues with inflammation running neck to neck with that. Now whether a virus, vaccine, protoza triggered it -would depend on the person and each persons own unique genetics that would also determine the integrity of the immune system. Working on supporting the immune system with diet and known deficiencies, eliminating known virus and pathogens, and trying to take some of the strain off the heart by attempting to pump the blood to our hearts and head by getting the other major pumping muscles helping -the legs, should help to calm down the tachycardia that this blood flow problem creates.
I know with myself, working on my immune system, changing my diet, addressing overactive mast cells has been my best help so far. I really think things are starting to come together. The puzzle pieces are starting to make the picture become more clear.
Issie
Issie, are you saying the autonomic dysfunction seen in ME patients is probably autoimmune by you mentioning working on the immune system and by addressing the dysfunctional immune system the autonomic dysfunction is reversible? Many thanks
Hi cort, Good article! I have POTS and this is not due to deconditioning. My tachycardia started at one point in time (at one moment) when i had a very good condition. It did not started after lying down in bed for a long time. I also have a decrease (33%) bloodflow to my brain. I think the autonomic overdrive is to compensate this problem but can be the cause also. The central problem is the bloodflow in many patiënts with POTS and ME or both. This subgroup can be seperated by measuring the bloodflow into the blood vessels (in the neck) to the the brain in upright position (sitting, standing) with echo doppler. In Holland professor Visser (cardiologist you wrote about) measure this phenomenon. He finds abnormal low bloodflow to the brain in many CFS/ME patiënts. I hope he will publish his data.
Sudden onset tachycardia! Great!
Yes, some of these researchers think the ANS is the hero in all this – it’s jumping in and working as hard as it can to correct for other problems – perhaps a broken chemoreflex response…(this was the first time I’d of that).
I hope Visser publishes on this. I know he’s got something in the works. I’ve just got to think blood flow is the key or a major key. I’m so glad they’re glad they’re making progress.
Thanks
As someone with severe orthostatic intolerance (which came on overnight so was not due to deconditioning, although now having been bedridden for almost a year this can’t be helping) I am very interested in any articles on the autonomic nervous system dysfunction.
The only thing is I wish I understood science better. The bit about increased receptor antibodies went over my head. Is the theory in the most basic of terms that antibodies to these receptors should not be existing in a healthy person and these antibodies increase the various autonomic responses in a dysfunctional way? Many thanks
Yes, autoantibodies for receptors will attack the receptors. If say 20% of the receptors are dysfunctional the sympathetic nervous system will have to pump out more catecholamines to get the job done; this could account for the sympathetic nervous system arousal – if I have this right 🙂
Virtually everything in a cell works when substances contact receptors on the surface of the cell and tell it to do ‘x’ or ‘y’. If you jam up the receptors the cell can’t function…
Thanks for the clear explanation, much appreciated
Good to see that someone is starting to put these things together.
Kudos also to Julia Newton and her team for the cross-cutting approach they’re taking.
I do wonder though, how many, if any of our ME/CFS ‘experts’ would attend a symposium such as this that isn’t billed as ‘Chronic Fatigue’?
Easy mistake to make in the context – but a slight correction. It’s ‘complex’ regional pain syndrome.
It certainly makes me want to attend the symposium…..
Outside of the select few that do autonomic nervous system research. I imagine that few ME/CFS researchers were there…Hopefully that will change over time.
The other thing I can’t work out is the autonomic dysfunction seen in ME due to actual damage to the nerves or a change in signalling? Many thanks
My guess is there are three possibilities:the autonomic ‘dysfunction’ could be the ANS trying to compensate for problems elsewhere; in other words the ANS is working fine. Or it could be dysfunctional due to damage to the nerves (aka small fiber neuropathy) or the signalling could just be off
Thanks, I really appreciate you taking the time to explain it all.
There could also be a problem with proper functioning of the veins, either due to improper constriction or blockage. With me, my doc feels that the biofilm that the protozoa (virus etc) live in – adheres to the walls of the veins and impairs blood flow. This may not be the entire problem in my case, but could explain a lot. This can also be attributed to immune system not recognizing and eliminating things that it should.
So if this is the case, like Cort suggested, the autonomic nervous systems response could also be a compensatory response.
Issie
Thanks Issie, appreciate the reply
Taking Magnesium ASPARTATE, L-Carnitine and Omega three fish oil on a daily basis is the only thing that got my Atrial fibrillation under control. None of the drugs had any effect.
According to testing, my body would not accept Coumadin, or a daily aspirin regimen to prevent red platelet aggregation (clumping) to prevent another heart attack, such as the one I had in 1998.
Since then, I have relied on the above, especially the fish oil to lube the red platelets to prevent aggregation. Is it working? RP
ps If I do not avoid the two foods I’m reactive too, wheat and citric acid, my gut inflames and the threat of Afib increases exponentially! The ANS is largely in the gut.
Sorry, if I’m preaching to the choir.
I so agree that Diet could be one of our main helps. Food can definitely be our medicine. I used to think that I was eating healthy and I know so much about alternative treatments (herbs, vitamins, supplements) and felt like everyone should supplement. Even though I still use some supplements myself now, I no longer feel that supplements in such concentrated forms are the best way to go. We should get it in our foods with all the support ingredients that are in whole foods. The body recognizes this better and uses it better. I have found that a whole food, low fat, gluten free, Vegan diet is very good for me. Im becoming a different person with what I’m doing. Things are improving for me in so many ways. This addresses the immune system at gut level and we truly are what we eat. Its the one thing we have complete control over. And, its the one thing people refuse to change. It takes determination and it doesn’t happen over night. But I can say for me, this is one of the best things I’ve done for 1myself. Ive reversed Chronic kidney disease, lost weight, gotten my usually high liable blood pressures to level out. Have days of not even qualifying to have POTS – when I was so bad I was in a wheelchair and homebound for awhile. Today I went snorkeling in the ocean for two hours and yesterday took a 2 mile walk with my hubby. Who would have ever thought this to be possible for me only 9 months ago when I started this lifestyle. All from a diet change, and addressing my immune system with low dose antibiotics, antimalarial herbs (due to FL1953 and coinfection related to Lyme), and addressing my immune system with MACS protocol (Allegra, Zantac, GastroCrom). I also think movement is absolutely imperative. I had to start out very slowly, and can see myself getting stronger with every new attempt. Hope this gives others hope! When I met a doctor a few weeks ago that has POTS and was at one time bed bound and depending on family to care for him, who is doing the same protocol that I’m doing refer to POTS in past tense and riding his bike this year thousands of miles – it for sure gives me hope that in three years, like this doctor, I’ll be able to tell people my story in a past tense sense too.
Issie
Issie
Can you give me the exact diet that have you ?
And can you tell me what Macs protocol is ? Who is your Doctor name ?
My son is 27years old and he stays at home from 5 years, can you give me your advise ?
Thank you very much,
Anna
Thanks Cort, interesting.
However, not sure about your interpretation re: repeat tilt testing. I followed that up in the link and it says:
==
8. Researchers at Eastern Virginia Medical School found that repeating tilt tests on patients who had increased orthostatic tachycardia, but not enough to meet the 30 bpm adult diagnostic criteria for POTS, resulted in 48% of them being diagnosed with POTS on the second tilt, when the tilt test was extended to 30 minutes. During the prolonged tilt, “patients who reached POTS criteria did so between the onset and 30 min of tilt, suggesting that tilting to a maximum of 30 min will diagnose the large majority of ‘‘late POTS’’ patients.
==
There is no mention this was done on the same day as the first test.
Whatever day they did it on – and I assume that it was on the same day, but if it wasn’t – it was the repeat aspect that was critical; they stressed the patients out with the same test again and when they did that – 50% of them failed.
If they simply took them in a month (say) later, it would have been nothing to do with the first test. I read it that it could simply mean testing people for longer than 10 minutes may be necessary. Hopefully more info will become available eventually.
The CAA are funding a study looking at the effects of carbon dioxide in the ME/CFS at New York Medical College (http://solvecfs.org/research/cfidsaa-research-program-for-researchers/brain-fog-in-cfs-whats-going-on/) including testing:
——
“- Breathing supplemental carbon dioxide to prevent the tilt-induced rapid breathing/reduced CO2
– Administering intravenous phenylephrine, a drug used to increase blood pressure, to prevent the rapid breathing/reduced CO2”
——
“This study involves 15 people with ME/CFS and orthostasis, 15 with ME/CFS but no orthostasis, and 15 healthy controls, all ages 15-29.”
Some of us POTS people have experimented with phenylephrine, which would work similar to midodrine and constricts the veins. Despite some of us having higher blood pressures and high standing NE levels, it didn’t seem to cause our bp’s to increase. Also, some felt less dizzy and better with it. However, the benefits wore off on the third day.
One thing I did today while snorkling (this usually causes me to get POTS in the water and to hyperventilate) was to take my “cocktail” for MCAS before I started – and – I didn’t have the problem today.
Issie
Great to hear – thanks Tom 🙂
Cort, so glad to see you are working and do such great journalism!
I have a couple of questions or so.
1. Is POTS the same as neurally mediated hypotension? I don’t think I ever have my heart rate go up, but I did pass out at 28 minutes on a tilt table with no measurable blood pressure. I never pass out otherwise, but do get lightheaded while standing in line or even sitting in a chair for several minutes.
2. I am kind of a freak about so-called “autoimmune diseases.” I still think there is ongoing infection not discovered because we have no valid tests for the freakin’ infections. DOES NOT MEAN THEY ARE NOT THERE. This would especially be true if the infections were in bone marrow or brain tissue. We now know that heart attacks are caused by c. pneumonia causing inflammation in arteries. Who would have figured that 15 years ago? Furthermore, how the heck did all these “autoimmune diseases” become epidemics around the 1980s? Huh?
3. I am getting old and just want to get rid of my headache of 8 years and counting. I will live with cfs but the headache is killing me. I think the headache is fungus infection in my brain, but how are you gonna prove that or get any treatment? I have started saying, I wish I had AIDS since 1995 and not CFS.
Okay, I will shut up now.
Hi Paula, long time no hear from.
Neurally mediated hypotension refers to blood pressure reductions when standing. POTS is heart rate increases…Both can occur together. It sounds like you have NMH.
We’ll have a blog coming up soon about ‘hidden’ infections.
Good luck with that darn headache – that’s a long time to have a headache….
The diet Im on is a low fat, whole food, vegan diet. Similiar to Dr. McDougal, Fork over Knives and Engine 2. My doctor is Dr. Stephen Fry in Scottsdale, AZ. He is the doctor that discovered the protozoa that I was found to have. Addressing this with diet, supplements and low dose antibiotics and enzymes to break down biofilms – is also helping my autoimmune issues and my POTS. I also have more energy.
There is a mistype on the above post. It should have said doing the MCAS (mast cell activation syndrome) protocol is helping. That consist of an H1 (Allegra), H2 (Zantac) and a mast cell stablizer (GastroCrom). I also use supplements to help with this.
Im sorry to hear about your son. I cant give advice, only say whats working for me. Not knowing what your son is dealing with or what his DX is it would be impossible for me to make suggestions.
If you want to read more about what Im doing, I have a really long thread on another site that Im keeping current with what Im doing and my response. If you look up Dr. Fry and protozoa – it should come up for you.
Issie
Izzie,
I also tested positive several years ago on Fry’s test. I was told by a well-respected lyme lab director that since he runs his own lab, protozoa is found in almost all patients.
I have two questions. Maybe you could explain what mast cell activation is and how one tests for it and if it’s something that people with CFIDS commonly have.
My other question is the tremors you had while having til table test. When I had standing orthostatic test, I started having bad head tremor. I was in auto accident and my head was tremoring and I had terrible pains in legs. To this day have problems with this.
I also have peripheral neuropathy in legs. Someone posted that they were tested for small fiber neuropathy through lab in Los Angelos. Can you go to a good hospital like Hopkins and have biopsy done or have it done by any neurologist who does this?
I have been told by one of his nurses that not everyone they check comes up positive. You have to keep in mind though that who goes to see him goes with certain issues and to see if one of the problems could be connected to this. So I would think there would be more positives just because of the type patient who goes there and the greater chance of likelihood of there being a positive finding. I knew some of my symptoms could be this. I knew when I had a tick bite and what my symptoms were when I found it. Also knew that my growing up in the South with all the mosquitoes gave me a stronger chance of a positive too. I also compared my pictures with my friends, and she had a very few and I had a significant amount. My immune system already was compromised and hers wasnt to the degree that mine was. I had months of testing earlier at Mayo and knew all the issues I had, but not the why. I had the DX, but no real good way of correcting any of the many things. I needed a plan of correction. Knowing what all was wrong, wasn’t changing anything. Dr. FRY suggested ths diet first off and thats all to start with. Later, I added meds and supplements -when I asked for more than just the diet. I was ready to be more agressive.
MCAS is hard to detect and is something that symptoms and testing are all taken into consideration. I had an extensive immunological and allergy workup at MAYO. And also a very bad attack that landed me in the hospital. There are some very good sites and forums you can join to learn more about it. Treating this has really improved my health.
Many of us with POTS are found to have neuropathies. Some neurologist test for this, as does Mayo and I’m sure some of the larger places may do this testing.
My tremors were not just with the TTT. They come and go and vary in intensity. It can be an internal feel that is not visible, or it can be more intense and very visible. Im not sure what causes them or why they happen. But, I’ve talked to many POTS people and it seems to happen to many of us.
Issie