Day 7 (Mon) – The Dreaded Lumbar Puncture
My L.P. is scheduled first thing in the morning. I am prepped by Dr. P.’s wonderful nurse of 17 years. Her voice, her actions, everything about her is calming. The test is done in a regular exam room, nothing exceptional is done and street clothes remain on. By 9 AM it’s over. The few pricks felt as the Dr. finds the right spot to withdraw the fluid are nothing to write home about as I lie in
The nurse talks me through the process and Dr. P. never speaks until it’s over. His first words “Excellent, you’re the poster child for the LP”. Ha, Ha, guess been skinny has its advantages… for a while anyway… because now comes the worst part… lying flat on a hard-as-a-rock exam table till 5 PM. Yes, 8 hours! Being skinny means no padding and an eventual bruise on my left hip. I am allowed to move to my other side or on my back and that’s it.
While on the table blood is drawn for AM/PM cortisol levels. I am also given almost 2 L of fluid to see if they will help raise my normally too low blood pressure… which they do. I’m hoping they’ll also help me recover from the ordeal of the entire week – perhaps keep me from ‘crashing’ – but mostly, help my body replenish extracted spinal fluid.
A liter of fluid will fill up your bladder fast so it wasn’t long before I am taught the contorted procedure of how to use the restroom. My head must remain level with my heart at all times. Keep in mind that the reason for all this “flatness” is to avoid the dreaded headache. Supposedly if you raise your head, your brain will sense the missing fluid and will basically “freak out”. Not immediately, however, and that’s the tricky part. The price would be paid two days later. So the goal is to give your body time to replenish the spinal fluid before you sit up.
Not to be chauvinistic but Dr. P.’s nurse told me it’s usually men who suffer the worse headaches after the LP, simply because they don’t follow instructions. She said oftentimes they’ll try sitting up the next day and when they don’t notice any discomfort they figure it’s okay to remain upright even though it’s only been 24 hours or less post-LP. She said it isn’t until the third day that they are hit hard… major headache. After hearing that, I decided to remain supine for two days.
Again, the RV really made things much easier. The biggest plus? The bathroom was only about 3 feet from my bed! Walking bent over at the waist is not as easy as it sounds and because I’ve been instructed to drink 8 ounces of H2O each hour it was necessary to make that bathroom trip quite often.
So for the first 12 hours after the test I lie completely flat. After that. I was allowed to use a very small pillow for the next 24 hours. Simple as it may seem, it was a godsend. Lying perfectly flat made it very difficult to breathe through my nose. All the liquids I’d ingested seemed to collect in my head. My eyes were puffy, my sinuses filled, and my ears had sharp pains when I yawned or coughed. Even my teeth hurt! The addition of a small pillow relieved all that.
At 36 hours post L.P. I would be allowed to slowly start sitting up on the side of the bed for a few minutes at a time.
Day 8 (Tues) All For Naught
I was scheduled to see Dr. P. today at 5 PM even though it would be only approximately 32 hours post L.P. We were squeezed in because of time restraints and our desire to hit the road ASAP. I had not slept well that night – sleeping flat is not my forte. I believe the contortions I went through to dress, brush my teeth and hair, wash my face, etc. all contributed to how I would pay later. And after all that, even after having reached Dr. P.’s office door in my wheelchair, we were met by staff who informed us we would have to return the next morning as Dr. P. was two hours behind schedule and it was already 5PM. We were told he would gladly meet us at 7:30 AM the next day. At the time I was extremely disappointed… but as you will see it worked out for the best.
Day 9 (Wed) Final Appointment
Normally Dr. P. does not schedule patients on Wednesdays, so postponing our appointment until this morning turned out to be a blessing….. we had him all to ourselves. He seemed 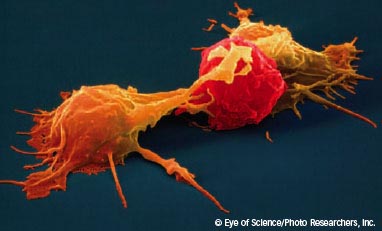
We covered a wide range of topics: the dysfunctional medical system; Medicare; pharmaceutical companies; how difficult it is for doctors to doctor these days; and the depressing stat that only a very small percentage of doctors surveyed in his county knew what a natural killer cell was! He explain how difficult it is with this present medical system to give the chronically ill the time and help they need; and, of course, we talked about CFS/ME.
We discussed research and the coolest thing was learning that he reads all the articles like we do!… and he likes to print them out instead of reading them online (like I do!) (By now I’m sure all you wives out there have to be thinking that Mrs. P. must be a saint!!) Also cool was when I asked him what he thought of Dr. Chia’s oxymatrine. He said he had just had a conference call regarding it the other day. He told me how Dr. Klimas attributes low NK cells to them just being plain worn out (overworked) rather than being a genetic abnormality or destroyed by environmental factors (toxins or radiation). As far as I was concerned my goal had been attained – I had finally seen a Dr. who knew as much (more!!) about this illness than I did.
I was also given a chance to ask a few questions. (I am the Queen of ?’s after all). (answers are paraphrased)
#1. Do you find any difference in the course of the illness between male and female patients?
A. Not really, except perhaps I don’t see as many male patients who I would classify as bed ridden and I’m not sure why.
#2. If a PWC/ME is menopausal do you find HRT of any help with this illness?
A. No, though many may lead you to believe it helps, I haven’t found it to?
#3. Can my body be “creating” CFS in order to survive?
A. Very good question. He went on to explain how Dr. Kerr in London has found that some patients have turned on their ‘hibernation gene’, a gene that was important to our ancestors for survival of the cold winters and limited food resources. The genes activation would lower heart rate, blood pressure, induce weight gain, lower thyroid, etc. – just make you feel like you want to nap all day (sound familiar?). And this gene is much more prominent in females. Why? Because it’s common knowledge that for survival of a species is more important that the female is better adapted to survive (for childbearing and rearing, etc.). Here’s where we had a good chuckle – as Dr. P explained how the male of the species is basically a sperm donor and if one dies, there’s always another to take his place.
#4. Re: viral activation, is it because of opportunistic viruses taking advantage of a dysfunctional immune system or is the immune system dysfunctional because of a virus?
A. That’s the $64 million question. We don’t know yet.
#5. While showing him my list of supplements I asked him if I was wasting my money.
A. You’re never wasting your money on COQ10. He was also a fan of acetyl- L.-carnitine and vitamin D, but not of D-ribose (perhaps just for my situation).
By now I was well aware that Dr. P. is not about just treating symptoms. He’s about tests and finding the root causes to your illness which was exactly what I was looking for. I was tired of the “drug for symptom” approach, I wanted to get to the core and I left believing that this is the man to do it. As we said our goodbyes I made certain that I grabbed his hand, shook it and sincerely thanked him (for all of us) for never giving up for the last 25 years. He may have heard it before but I was sure another “thank you” would not be unappreciated. If I’m not mistaken I believe I detected a hint of moisture in is baby blues as he accepted my gesture.
Day 8 (cont) On the Road Again
Meanwhile, a few minutes before we left I started experiencing some discomfort at the base of my skull, an area where I often had pain. This was my first day completely upright since the LP but I didn’t yet connect the two. Soon after leaving Incline Village in the RV I became a bit nauseous as the pain became intense. It resembled muscle spasms rather than a headache so I attributed it to the contorted position I’ve been holding my head in for the last two days.
About 100 miles down the road it became completely unbearable…” the worse pain I’ve ever had”. I’d taken half an Aleve in the a.m., so I took ½ more (yes, I’m chemically sensitive!). We were able to pull over so I could lie down. (I have to watch the road or get motion sickness, so lying down while my husband drove was not an option). I wasn’t sure if this was something urgent (blood clot?) so I called Dr. P.’s office and quickly received a return call from the nurse. She told me there was no need for the E.R., that Dr. P. said this sometimes happens. She advised me to rest, use heat, ice or whatever helped best.
My thoughts went back to the day of the LP when I was offered an injection of Tramadol before I was released. I was told it was an anti-inflammatory with analgesic properties that could help with muscle spasms that sometimes occur after lying flat for two days. I was told that some patients feel its effects for up to a week, so being chemically sensitive as I am, I passed. Who knows how I would react to a new drug and I didn’t want to find out while on the road. Muscle spasms…. big deal, I wasn’t prone to FM-like symptoms so I was sure I’d be able to handle a little muscle discomfort, so I thought! If I had to do it again I’d take a small dose of the tramadol.
Meanwhile, resting the weight of my head off my neck, along with the Aleve, was taking a bit of the edge off. We were on a schedule so I didn’t have the option to rest – so how could I keep my eyes on the road and the weight of my head off my neck so that the muscles would remain relaxed?
My dear husband, ever the “Fix It Guy”, came up with a contraption made from a nylon strap. He made me a noose! Yes, I know what you’re thinking…” Poor guys finally fed up with his high maintenance wife”. Nope. This noose hung from the overhead bunk and fit perfectly around the back of my head, behind my ears, cradling its weight as I reclined in the captain’s chair seated high enough to still keep my eyes on the road. Perfect! It was a godsend, though I must’ve looked pretty strange to the truckers who drove by.
Home at Last: after a total of 2 1/2 weeks and 1600 miles I was safely home. I would like to conclude my journal by answering a few questions that you might have…
Costs: How much did it cost? Travel costs aside (even in a gas guzzler, for me
First let me be clear that this reflects my particular situation and that it may be different for someone else. I have no supplemental insurance other than Medicare Parts A, B and D (but thankfully Dr. P is a medicare provider and accepts medicare payment!) and the tests requested for me may not be the ones requested for you, but here goes.
It has now been six months since my visit. Medicare has covered most of the MRI, the brain SPECT and a long list of blood tests done by the conventional labs. I was asked to pay up front for the exercise stress test ($650) and Dr. P’s consultation ($350) but Medicare has reimbursed me for these. I was also asked to pay in advance for some of the virology and immune system testing. This came to approximately $3000 and I was told in advance that Medicare would not cover these.
Medicare has also paid their portion of the Lumbar Puncture along with the EKG and BP monitoring tests. So, as of today my guesstimate regarding my total costs is somewhere around $4000. Not cheap, but in my opinion not out of line considering all the tests done (literally pages and pages). Dr. P.’s consultation fee (including two reports to my family physician and the many follow-up questions he has taken the time to answer), seemed extremely fair as I have paid as much for one visit to other specialists (neurologists, etc.,) most of whom are ignorant of CFS/ME.
Would I do it again? Immediately following the trip I do remember saying “Boy, that was hard. I’m not sure I’d do it again”. But after three months of hindsight and journaling… a resounding “Yes!!” And to be able to say I am now a patient of Dr. Peterson’s…well, it’s priceless!
The Physical Cost – My crash actually began the Friday before the LP. Once I arrived home I was pretty incapacitated for an additional week or so but nothing out of the ordinary for me as I am considered moderates to severely disabled and I’m often bedridden. In my opinion the “punishment fit the crime”. (Recovery period: 2-3 weeks)
Repeat Visits? At the time Dr. P did not want to schedule a follow-up visit but has since done so. His goal is to eventually be able to work collaboratively with my GP… if my GP is willing. He has already sent him a preliminary report but has yet to send the final report with the final test results.
Treatment Options
Treatment so far has been limited to Procrit (I’m assuming with the hopes of raising my RBC volume and my blood pressure). Dr. P. said that some patients find great benefit with it, but he also told me to just try it without having any expectations. So far it hasn’t done a whole lot physically but it has improved some of my numbers. For me it just feels good to be trying something. It isn’t overly expensive ($120/month), but isn’t covered by my insurance. He would like me to continue using it until our next appointment, which is in a few weeks. Now that all my test results are in I will be anxious to see where he goes from here, where a fit in his”categorizing” of patients, and what new tests he recommends (xmrv?) when I return.





