In Wyller’s eyes chronic fatigue syndrome is not a ‘chronic fatigue’ disorder; it’s an autonomic nervous system disorder. Wyller has been studying ME/CFS for about five years; he knows the vast array of symptoms present in this disease and one gets the feeling he’s more than a little tweaked at the overwhelming focus on fatigue.
As well he should… this disorder is, after all, very, very good at producing all sorts of symptoms; why bury all that richness under one symptom? Once fatigue was put in the name it was inevitable that that symptom took central stage but that doesn’t mean other symptoms won’t end up being more important.
Wyller’s results indicate you never know what’s going to pop out in a study..and how it might redefine what you’re studying.

Instead of taking the mean, Wyller went to the edges, and found something that could help redefine this disorder
A New Focus: the More Severely Ill
In this study Wyller set out to figure out which symptoms contributed most to disability, what role the autonomic nervous system might play in producing those symptoms and where the standard definition for chronic fatigue syndrome fits into all that.
Wyller’s focus on more disabled patients suggests he believes you have to see it at its worst (and weirdest)… in order to understand at its more moderate; the most severely ill patients provide the best roadmap to learning for this disorder.
The most common denominators of this disease (fatigue, pain, poor sleep, etc.) are just too common to really tell you anything about cause. Since these symptoms can be caused by so many different things, taking this disorder to its limit and seeing what pops up there, and then reinterpreting it in the light of that, probably makes sense.
The Study
Wyller got clinical data, data on symptom severity, ability to meet the CDC criteria, disability and autonomic measures taken during a tilt table test (20 degrees for 15 minutes) from adolescents with severe fatigue (but not necessarily ME/CFS) and then did linear regression analyses to see what was associated with what.
The patients had to meet Wyller’s definition of chronic fatigue syndrome which is an interesting blend of the Oxford and Canadian Consensus definitions: patients had to suffer from three or more consecutive months of unexplained disabling fatigue which was worsened by physical or mental exertion.
The patients were asked to provide clinical information below and their BMI was measured and Wyller determined whether they met the CDC criteria for CFS.
They rated their symptom levels () which were put into the following categories
|
Wyller then looked at which symptoms were most associated with what he determined were the most disabled patients. (Bear in mind that these youngsters were healthy enough to get to Wyller and get tested etc; these are not the really, really disabled patients. They are, however, the most disabled of their set.)
Analysis of More Disabled Patients Prompts Reassessment
It turned out that disability was associated with cognitive symptoms, hypersensitivity symptoms, high fatigue score, and older age; i.e., the more disabled patients tended to have more cognitive symptoms, more hypersensitivity symptoms, be more fatigued and be older.
Fatigue was higher in the disabled patients but let’s throw that and older age out for now. That leaves us with the more disabled patients displaying more cognitive and hypersensitivity symptoms and, of these, the hypersensitivity symptoms (to sound and light) stand out like a red flare because of how unusual they are.
Hypersensitivity to sound and light is something relatively distinct to ME/CFS and that’s what we were looking for; something that would allow us to distinguish this disorder from others. If hypersensitivity and cognitive issues show up more in disabled patients then we have to consider if the same things causing these symptoms are also responsible for the fatigue, pain and other more common symptoms present.
The symptoms that weren’t increased in the more disabled patients give us another reference point. Gender differences didn’t matter, nor did fatigue duration (these were young people) nor did sleep, pain, dizziness or immune symptoms. (Wyller only measured insomnia for sleep). In short, many of the key symptoms in the International Definition such as muscle, joint and head pain and painful lymph nodes weren’t really associated with disability; they were probably high (or low) in everybody.
Linking Central Symptoms with Physiological Problems; Getting at Cause?
The two key symptom sets that Wyller’s analysis uncovered were associated with ANS irregularities. Hypersensitivity was associated with increased heart rates during tilt table testing and decreased heart rate variability, and cognitive issues were associated with increased heart rates during tilt and at baseline.
This suggested that sympathetic nervous system activation could be involved in producing both those problems.
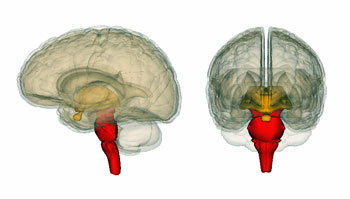
Wyller’s earlier studies suggest to him that ME/CFS is a disorder of ‘sustained arousal’ and this study suggested it originates in a part of the brain stem called the locus coeruleus (LD). Because the LC produces the excitatory catecholamine norepinephrine (noradrenaline) and regulates sympathetic nervous system activity, it could be responsible for the increased heart rate at rest, low heart rate variability and the exaggerated heart rate responses.
That’s not all…Brain stem hyperactivity can overwhelm the prefrontal cortex impairing our ability to perform executive functioning processes (working memory, attention, problem solving, planning, etc.) which are impaired in ME/CFS. The brain stems ability to amplify sensory signals coming from the body means its hyperactivity could also cause the hypersensitivity issues. Every issue Wyller’s study has raised; cognitive problems, hypersensitivity issues and autonomic problem could all originate in the brain stem.
Exciting Stuff! (Too Exciting…)
The idea of central nervous system over-activation has gotten around. The central sensitization theory that covers FM, ME/CFS, IBS, etc. relies on it; Ashok Gupta proposed the fear center of the brain, the amygdala, plays a key role in this disorder, Jason Leonard proposes a process called ‘kindling’ has set ME/CFS patients brains aflame (so to speak), and Marco on Health Rising recently published a neuroinflammatory model of ME/CFS that pegs glutamate, the main excitatory neurotransmitter as potentially a key factor in ME/CFS.
- Dig Deeper : Glutamate – One More Piece in the Chronic Fatigue Syndrome Puzzle? A Neuroinflammatory Model of ME/CFS: Pt II
Now Wyller has proposed that another important excitatory compound, norepinephrine (noradrenaline), plays a key role. Norepinephrine directly increases heart rate, heart contractions, etc., regulates amygdala functioning and is released in the body in same postganglionic neurons the Lights think may be pounding ME/CFS patients brains with stimuli. Norepinephrine also appears to regulate the release of a key pain factor in fibromyalgia (substance P) from these postganglionic neurons.
Possible Hypersensitivity-Cognition Connection
Hypersensitivity and cognitive problems could go hand in hand. Sensory processing or ‘gating’ problems could flood the brain with so much information that it becomes difficult to concentrate on outside stimuli. The ‘low working memories’ in chronic fatigue syndrome could reflect how difficult it is divert ones attention from the constant flow of body stimuli flooding the brain. Could a constant din of sensory data be blunting ME/CFS patients ability to focus on something else? (One part of Gupta’s Amygdala Retraining model is to turn the focus away from body stimuli…)
Marco’s recent blog suggesting ME/CFS could be a ‘sensory gating’ disorder attempts to redefine this disorder in a similar fashion.

Hypersensitivity could contribute to the some of the cognitive problems found in chronic fatigue syndrome (ME/CFS_
Studies have shown the brains of ME/CFS patients have difficulty in turning their attention away from innocuous stimuli such as background noises and light (sound and light :)) to the task at hand. This difficulty could suggest a kind of ‘fight/flight’ situation in which the brain feels the need to monitor everything. Studies also suggest that cognitive problems even show up in such basic things as movement and coordination. Could the loss of physical grace that so many people with chronic fatigue syndrome experience be partially due to cognitive problems (linked to sensory issues?)
What about the more normal symptoms found in chronic fatigue syndrome such as pain and sleep problems? What about post-exertional malaise? Do hypersensitivity and cognitive issues provide a clue to how those symptomsare caused?
Pain is essentially defined as a hypersensitivity issue in fibromyalgia and sensory overload could surely complicate getting relaxing sleep. Dr. Klimas finding that autonomic nervous system irregularities (fight or flight response) early in the exercise period trigger an immune cascade that causes post-exertional malaise fits well with Wyller’s model of brain stem issues ramping up the sympathetic nervous system which in turn triggers an immune response putting post-exertional malaise and possibly hypersensitivity issues into play.
Defining Moments
The fact that the CDC definition was not associated with any autonomic measures or disability suggests the definition is missing some key elements. If Wyller’s study is correct, if you were to take a lot of people with ‘chronic fatigue’ and then picked out the most disabled ones – they would not be the ones that met the CDC definition for CFS. Certainly some disabled people would meet the criteria but others would not. Nor does the definition pluck out people with autonomic nervous system issues; a worrying situation given how important that research field is becoming.
Wyller’s analysis, interestingly, enough suggested to him that this really is all one disorder. In fact, he appears to believe that chronic fatigue syndrome, fibromyalgia, irritable bowel syndrome are all the same type of disorder.
Preliminary
This study comes with a number of proviso’s and Wyller called the study ‘exploratory’. These types of studies uncover associations but never prove causality. The small size of the study limited the number of symptoms Wyller could measure and it’s overall power. Wyller used his own unvalidated measure of disability and the studies focus on adolescents means it may not apply to adults. On the plus side the very strong ‘significance’ values (p<.000x) suggested Wyller may very well be onto something.
- Next Up: we take a deeper look at what Wyller believes is the seat of it all – the Brain Stem and Chronic Fatigue Syndrome







Hi Cort,
This is very interesting. Can we see the study somewhere? Thanks.
Whoops..I put the link in there and here it is as well – http://www.ncbi.nlm.nih.gov/pubmed/23388153 – its a freebie by the way.
Great information!! Sounds pretty damn accurate!
Thanks Mike, it’s been awhile..hope you’re doing well…I well remember the hypersensitivity issues you had (whew…)
finally, this connection is made! i agree with you mike as far as accuracy is concerned, the hypersensitivity is the worst part for the very severely ill. at my worst, i would crash if someone quietly whispered two words to me, or if i tried to open my eyes and look at the wall … i wonder if they also included touch and being moved as criteria for hypersensitivity to account for those of us who’ve not been able to have a carer change our top or bedsheets for weeks.
thanks for the great article, cort.
i hope it gets more people interested in Gupta and/or DNRS because honestly, waiting for a complete pharma ‘cure’ (or even alternative) fades the more this kind of info gets published. a multi-disciplinary approach is needed.
I remember hearing of Mike being in a dark room because he was too sensitive to sound and light to handle them. When he went out…crawled out apparently…he was wearing his sunglasses…the lights had to be dimmed in the doctor’s office….he was the picture of hypersensitivity..
I have had my own separate issues with chemical sensitivities…To be honest those have gotten much better and the only reason that I can tell, since I’ve never worked specifically on them, is that I’ve reduced the amount of arousal in my body…the fight/flight activation…by doing stress reduction exercises and more pacing..Over exercise always tends to ramp up my chemical sensitivities.
There’s still alot of arousal left to go around but at least my sensitivities are less… 🙂
Even trying to think was too stimulating!
Yes..noise, light, touch..really brutal
I think everyone who has ever known several people with severe CFS/ME knows has noticed that almost all of them have severe hypersensitivity to light and sound, many also to touch and other things. It’s good to get proper validation of this.
If “chronic fatigue syndrome is not a ‘chronic fatigue’ disorder” then surely chronic fatigue syndrome has to be a rather unfortunate choice of name.
I wonder why the need was felt to use another unrecognised set of diagnostic criteria rather than one set oa agreed criteria.
I don’t know. Wyller’s been using that for awhile I think but I don’t know his reasoning. It could be that the thinks FM, IBS, IC etc. all fit together and he’d rather use a definition that can include them all.
Because the definitions that are being used don’t always adequately describe what is happening to us. Yes, it would be nice to have everyone agree on one set of definitions but you can easily see that that has not happened. Maybe stirring the pot will get people to take notice and stop with their own agenda on what should be and should not be in the definiton. And just maybe if he can improve on the definition we could get some better criteria of what to study.
Thanks, Cort
In any other illness I suspect that the most severely-affected patients would be the first port of call for researchers, not the last, so congratulations to Wyller for taking this approach.
However, this is very much a preliminary study: he looked at an awful lot of variables given a sample of just 38 patients, and uses both unvalidated measures and an unvalidated definition. I hope he will be attempting to replicate these interesting findings on a larger and independent sample, preferably using validated measures of disability etc. promising, though.
Thanks,as always, Simon for keeping us honest :). Wyller recognized it was a pretty preliminary study (although he loved the significance fators :)); I hope he or somebody else can get that bigger, better study done.
Hi Cort,
This sure sounds like like me. I have two rounds of it and both started with panic attacks. I knew I was getting sick again when they started. I am very sensitive..can almost read some people’s minds. I sometimes can. It scares me. I don’t try to it just happens as in be careful with this person. I have feling that something not good is going to happen and pass it off and it happens. A doctor once told me we were all so sensitive we knew things. I rarely trust it though but it is always right. I am very senitive to weather changes and know beofore the weather people when a storm is coming. I have heard of others the same. Anyone else?
Dr. Klimas has said the stress mechanism is broken, then the ANS goes down and then the immune system and out come the latent viruses,
It is very hard to meditate but I keep trying. We recently did a Video Heath Study with the U of Miamai. It was ten weeks and I learned a lot. Blood and saliva are taken 4 times, one more time for that. I am anxious to see what the cytokines show.
I did the Gupta traning for a while but in time his voice bothered me. I was getting stressed trying to do the relaxation.
I learned some other relaxation exercises in the Video Training class. I still have not found a perfect fit. It is hardest for the people that need it the most.
I am anxious to hear more about this. Thanks for reporting.
Marg
I agree Marj…=Stress reduction is good for me and it’s really hard as well; there’s something about this disorder – at least for me – that makes those exercises really difficult…I enjoyed meditating before I got ill, by the way. Some of that could be due to finally having to confront all the noise (stimuli) hitting us….you can jam that down to some extent but when you’re meditating it all comes up.
I find mindfulness exercises easier.
Good luck with your practice.
Marg- Wow -This sounds just like me. I almost always know when something is bad for me ahead of time.
If I don’t listen to that I ALWAYS get sick. People, trips, Doctors, or whatever. Too much of anything makes me sick. I too can read people pretty well. Not that I always listen.
Thanks for your comment. Hope Wyller is onto something that will help soon. Also thanks Cort for all the new information.
San Diego #1
I’m sensitive to everything, sound, the lower sounds I can hear roadwork going on miles away the noise the trucks make a night idling drives my insane. Lights, especially overhead lights in a store. I don’t have to worry about that anymore now I am completely house bound.
I have photosensitivity in a bad way, meaning if the sun comes out I can not be outside. I tried covering up every part of my body and sit in the shadow in the yard, still my immune system sees the UV rays as invaders and make me I violently ill. Those days I will go and sit in the yard when it’s dark.
I’m also sensitive to barometric pressure and for that we chose an excellent place to live in, the Pacific NorthWest. The barometric pressure doe change here every half hour:-) it affects my emotional state. I can go from being the sweetest person to the ugliest witch on the planet. My husband is a saint. 🙂
I must say that I was very confused by the report, it mentioned ‘severely ill’ people. Exciting! I’m in the 25% group, finally someone who is paying attention to us. But I was disappointed to discover what they call severely ill to me are high functioning people with CFS. They could travel! And survived the TTT! Those are definetly not severely ill people!
My TTT threw my in a violent relapse after a cardiac arrest on the able while they injected my for fun with Isoproterenol to see how high my heart rate would go. I already had a positive by fainting. When I came to it they injected me and my heart said up yours, this is too much and it quit.
I hope that they will stop labeling moderately ill people as severely ill. If they are severely ill than what are we? The living death? Well, at least Montoya was right about that!
Thanks Christine, what a story you have. The sound sensitivity is amazing…When I was worse off I remember being troubled by the lawnmowers down the block and your story brings me back to Dan Moricoli’s story who often had to escape into utter darkness to calm his system down. He would describe certain sounds as kind of tearing at his brain…It sounds very painful.
The ‘severely ill’ issue was more my fault; I meant to call them the ‘more severely ill’ and only in the context of those patients. There were no housebound patients in the study I don’t believe.
Good luck with everything.
It seems that symptoms change over the decades (I got it the summer I was 8) and am 60. I had a massive venous thrombosis in the spring of 1992. My Doctor contacted Dr. Peterson who walked him through the physical examination and both examined the films and tests done in 1986–I saw 28 doctors that year, had various CNS studies etc. I had a biopsy and Dr. Miller who retired to the Sierra HMO in Auburn.
The changes between the 1986 brain studies and those in 1992 were found by my GP to be the most convincing. The 1986 study and the study in 1992, which showed plaques, fuzz and lesions.
matched
1992-2002 and 2002-2012 showed changes as well. Take evert precaution with your records and Films. In addition I think States should have dedicated archives for ME/CFS, integrated into the State Archives and maintained by a dedicated librarian who has no medical or any other agenda.
Records are kept for 7-10 years and generally dumped or shredded, often they are just ripped out of your records by hospital staff, doctors or surgeons with agendas.
If the disease symptoms change over the years, they may not fully match your symptoms at 5, 10, or 12 years when your symptoms fully matched the criteria. Some viruses or other pathogens may go dormant, only to be reactivated in a good year that goes bad.
Symptoms and findings are not mutually exclusive. The notion that they are, I believe, one of the most counterproductive in the baby-boomers’ natural disease history. The loss of critical, evidentiary information. Dr. Miller strongly emphasized that I had what I had and would always have, and I should never allow anyone to put me through as many test as I had had at that time. Keep them safe even if your Doctor is not finding them relative to the diagnostic paradigm of 2013.
They may be critical in the future.
I agree with keeping your records yourself. Most of my conventional Dr. do not even look at the retesting from CFIDS Dr. My CFID Dr. looks at everything!!!
Thanks,
San Diego
Wyller is a known Wessely school doctor and despised by most ME patients in Norway. He has publicly denounced the work and results of Fluge and Mella, and is known for manipulating criteria to fit his own theories. Careful what you wish for !
Wyller does prescribe CBT and LP AND he’s also been a key figure in uncovering the autonomic nervous system problems in ME/CFS…I’m not in Norway, obviously but, based on his research, he doesn’t fit in a ‘Wessely school approach’.. Wessely is not doing autonomic nervous system research (or an biologically based research) nor is he citing brainstem abnormalities as a possible cause of ME/CFS. I recognize there are issues over there but I’m looking from the research end; I think I’m seeing him differently.
At least on the research end I think you could say he’s in the “Newton School of autonomic dysfunction’ since his results track closely with hers.
In the end I think we should determine each studies worth by examining each study. I don’t think Wyller’s finding here should alarm anyone; intuitively it makes sense to me.
Again I don’t know anything about his comments in Norway but here’s his research over the past couple of years.
Relationship between autonomic cardiovascular control, case definition, clinical symptoms, and functional disability in adolescent chronic fatigue syndrome: an exploratory study.
Wyller VB, Helland IB.
Biopsychosoc Med. 2013 Feb 7;7(1):5. doi: 10.1186/1751-0759-7-5.
PMID: 23388153 [PubMed] Free Article
Related citations
2.
Clonidine in the treatment of adolescent chronic fatigue syndrome: a pilot study for the NorCAPITAL trial.
Fagermoen E, Sulheim D, Winger A, Andersen AM, Vethe NT, Saul JP, Thaulow E, Wyller VB.
BMC Res Notes. 2012 Aug 7;5:418. doi: 10.1186/1756-0500-5-418.
PMID: 22871021 [PubMed – indexed for MEDLINE] Free PMC Article
Related citations
3.
Adolescent chronic fatigue syndrome; a follow-up study displays concurrent improvement of circulatory abnormalities and clinical symptoms.
Sulheim D, Hurum H, Helland IB, Thaulow E, Wyller VB.
Biopsychosoc Med. 2012 Mar 21;6:10. doi: 10.1186/1751-0759-6-10.
PMID: 22436201 [PubMed] Free PMC Article
Related citations
4.
Chronic fatigue syndrome: a qualitative investigation of young patient’s beliefs and coping strategies.
Hareide L, Finset A, Wyller VB.
Disabil Rehabil. 2011;33(23-24):2255-63. doi: 10.3109/09638288.2011.568663. Epub 2011 Apr 7.
PMID: 21473686 [PubMed – indexed for MEDLINE]
Related citations
5.
No differences in cardiovascular autonomic responses to mental stress in chronic fatigue syndrome adolescents as compared to healthy controls.
Egge C, Wyller VB.
Biopsychosoc Med. 2010 Dec 14;4:22. doi: 10.1186/1751-0759-4-22.
PMID: 21156045 [PubMed] Free PMC Article
Related citations
6.
Elevated nocturnal blood pressure and heart rate in adolescent chronic fatigue syndrome.
Hurum H, Sulheim D, Thaulow E, Wyller VB.
Acta Paediatr. 2011 Feb;100(2):289-92. doi: 10.1111/j.1651-2227.2010.02073.x. Epub 2010 Nov 17.
PMID: 21059182 [PubMed – indexed for MEDLINE]
Related citations
7.
Polymorphisms of adrenergic cardiovascular control genes are associated with adolescent chronic fatigue syndrome.
Sommerfeldt L, Portilla H, Jacobsen L, Gjerstad J, Wyller VB.
Acta Paediatr. 2011 Feb;100(2):293-8. doi: 10.1111/j.1651-2227.2010.02072.x. Epub 2010 Nov 18.
PMID: 21059181 [PubMed – indexed for MEDLINE]
Related citations
8.
Blood pressure variability and closed-loop baroreflex assessment in adolescent chronic fatigue syndrome during supine rest and orthostatic stress.
Wyller VB, Barbieri R, Saul JP.
Eur J Appl Physiol. 2011 Mar;111(3):497-507. doi: 10.1007/s00421-010-1670-9. Epub 2010 Oct 2.
PMID: 20890710 [PubMed – indexed for MEDLINE] Free PMC Article
Related citations
9.
Hormonal alterations in adolescent chronic fatigue syndrome.
Wyller VB, Evang JA, Godang K, Solhjell KK, Bollerslev J.
Acta Paediatr. 2010 May;99(5):770-3. doi: 10.1111/j.1651-2227.2010.01701.x. Epub 2010 Mar 1.
PMID: 20199497 [PubMed – indexed for MEDLINE]
Related citations
10.
Can sustained arousal explain the Chronic Fatigue Syndrome?
Wyller VB, Eriksen HR, Malterud K.
Behav Brain Funct. 2009 Feb 23;5:10. doi: 10.1186/1744-9081-5-10.
PMID: 19236717 [PubMed] Free PMC Article
Related citations
11.
Enhanced vagal withdrawal during mild orthostatic stress in adolescents with chronic fatigue.
Wyller VB, Barbieri R, Thaulow E, Saul JP.
Ann Noninvasive Electrocardiol. 2008 Jan;13(1):67-73. doi: 10.1111/j.1542-474X.2007.00202.x.
PMID: 18234008 [PubMed – indexed for MEDLINE]
Related citations
12.
Sympathetic cardiovascular control during orthostatic stress and isometric exercise in adolescent chronic fatigue syndrome.
Wyller VB, Saul JP, Walløe L, Thaulow E.
Eur J Appl Physiol. 2008 Apr;102(6):623-32. Epub 2007 Dec 8.
PMID: 18066580 [PubMed – indexed for MEDLINE]
Related citations
13.
Abnormal thermoregulatory responses in adolescents with chronic fatigue syndrome: relation to clinical symptoms.
Reading through the full text, without being aware of the researchers’ backgrounds, as soon as I saw the prefrontal cortex mentioned I thought fine – reductions in PF volume have been found in ME/CFS and in a number of ‘psychiatric’ conditions and CBT has been claimed to restore lost PF volume.
So while this study lends some support to my own model there are a variety of interpretations of the findings. Therefore I wouldn’t discount the findings because of the ‘philosophical’ background of the authors.
I’ll give an example. Frequent attempts have been made to link various ‘maladaptive personality types’ with ME/CFS including ‘perfectionism’.
One interpretation of perfectionism is the tendency to focus on relatively trivial negative details or an inability to see the ‘big picture’. A psychological interpretation would posit this ‘trait’ as a (probably learned) aberrant thought process that can most likely be ‘cured’ by cognitive therapies.
On the other hand, a NEUROLOGICAL deficit that results in the INABILITY to screen out even trivial sensory information would likely result in behaviour that might be classed as ‘perfectionist’.
I wouldn’t rule out the possibility that some cognitive therapies (or less value laden therapies such as meditation/mindfulness) may help ‘attenuate’ this inability to filter incoming sensory signals but a pharmaceutical intervention is much more likely to get to the root of the problem.
Thanks so much, Cort, for bringing us another concise, readable review of a study that makes me feel better.
One of the more difficult things for me to adjust to since I’ve been ill has been light and sound sensitivity. It’s so contrary to being “normal.” I asked myself how crazy a person would have to be to grit their teeth or at least want to scream out because of the sound the car is making in idle. I thought of myself primarily as “crazy” for quite awhile. But the aversion to certain sounds and always to sounds competing for my attention, as well as feeling bright light as pain, I now know is just part of this disease.
I’m heartened to know that learned people who can concentrate are taking these symptoms seriously and are studying them as hallmarks of what’s the matter with us. Every bit of hope counts.
Thanks again for your work and for bringing this to us. I’ll stay tuned….
Sarah
Being in Scandinavia and having followed Wyllers work (clinical as well as scientific, plus his public statements and role in the ME debate) I strongly agree with Lars. Wyller is a hugely problematic figure in the ME field in Scandinavia. He talks about “chronic fatigue” rather than ME and refuses to use narrow definitions like CCC. He is obstructing for children and adolescents (he is a pediatrician) to recieve the same biomedically based care as adults now do in Olso (at Aker Hospital), and as Lars writes, he is opposing the Rituximab studies.
I think these problems are present in his research work too. As long as he uses his own very broad definition, not many conclusions can be drawn for the actual ME/CFS patient group (as defined by CCC or ICC).
It is probably in his interest to fashion his results towards CBT as a solution, since this is his position in the debate, so maybe his stubborn choice of broad criteria is rooted in that.
I would advise strong caution while interpreting Wyller’s work.
I understand the caution but I’d be careful about thinking that he’s fashioning his research results towards having CBT be an answer. I would suggest that it’s maybe other way around; that his research has shown that autonomic nervous system problems are present and that the fight/flight response is activated and that one way to calm down the ANS is through relaxation exercises, mindfulness activities, etc.
I guess my big question is is he really saying that CBT is a cure for CFS? Several well known doctors in the US (Bateman, Klimas and even surprisingly Peterson) have said these types of therapies can be helpful but they put them in the context of many other therapies. That’s perfectly fine for me; if CBT-like therapies are helpful for other disorders I don’t see why they wouldn’t be helpful for some people with ME/CFS. These physicians are certainly not saying just do CBT or the Amygdala Retraining Program; they’re just more tools in their toolkits.
For me there’s no reason a physician can’t believe there’s a physiological basis to this disorder and support the use of therapies like that. Stress reduction plays important roles in disorders as different as asthma and heart problems.
That’s very, very different from saying CBT cures CFS. If that’s what Wyller’s saying then he’s way off and I don’t understand why he would be doing this research, actually.
Check this out:
What’s so different about that and CFS? Both after all, have autonomic nervous system and, I believe, circulatory issues. The main difference is probably that they’re getting treatment for their heart condition along with the stress reduction therapies….
As to the definition, yes I would rather he use CCC or ICC altho he is using post-exertional malaise as a filter and he’s appears to have alot of cognitively challenged patients in that study so he’s got the two core symptoms in both those definitions present at least in this study.
But here we are talking more about the researcher than the study. ..
In this case you are showing a frightening ignorance to the realities on the ground, and also the context and work of Wyller. You need to do your homework before you write stuff like this, because you are promoting the work of a guy who is actively trying to stop any further study on Rituximab in Norway through his powerful network. If you want to stay on the record defending this, you will alienate a lot of people and indirectly contribute to halting one of the few real hopes for ME/CFS patients worldwide.
What is most interesting, and also most distressing, is that when a genetically susceptible person is exposed to toxic mold, the exact symptoms he describes present themselves. I still believe that these “syndrome diseases,” like CFS and FM, are due to toxic mold exposure, but researchers continue to look at symptoms instead of causes. How many of the studied group were tested for HLA DR genes? How many of them had elevated levels of c4a, MMP9, VGFB-1, and other inflammatory markers? How many of them were checked for high levels of recirculating toxins? Why spend all this time, effort, and money looking at effects when the cause is so blatantly obvious to those of us who have found it in ourselves?
In his doctoral thesis “The pathophysiology of CFS in adolescents» Wüller explains about his view on the CDC criteria.
https://www.duo.uio.no/handle/123456789/28571
Example: “Fourth, the ambiguity of the CDC-definition, specifically emphasized in a recent, authoritative review (63), suggests a modification of it. We therefore omitted the bicriterion (4 of 8 accompanying symptoms, see 1.1.1), and included patients solely based upon the fulfillment of the main criterion, as will be further outlined below (see 2.1.1).
The study he quotes is: Cho HJ, Skowera A, Cleare A, Wessely S. Chronic fatigue syndrome: an update focusing on phenomenology and pathophysiology. Curr Opin Psychiatry 2006; 19: 67-73.
Ie: the Wessely school.
And the participants in his study are: 12-18 years of age > 3 months of chronic fatigue with severe disability resulting from fatigue, and where well-defined somatic or psychiatric disease that might explain the fatigue is excluded.
I do not see the difference between this and the Oxford criteria for CFS, with the exception of 3 months duration for adolescents, but he also says in the thesis that most of the participants had fatigue for over 6 month.
And as far as I know he has used the same criteria in all of his studies, e.g. “Relationship between autonomic cardiovascular control, case definition, clinical symptoms, and functional disability in adolescent chronic fatigue
syndrome: an exploratory study” in Biopsychosolcial Medicne”:
http://www.bpsmedicine.com/content/pdf/1751-0759-7-5.pdf
His true belief that CFS is a biopsychosocial disease is also why Lars and Emma put him in the “Wessely school”
I admit that I have not read this last research study, but from the recent discussion on the new guidelines from The Norwegian Directorate of Health I do not he has changed his views.
My conclusion is that when he states that CDC definition is whacked, he believes that it is ok to omit the bicriterias, and only use chronic fatigue as inclusion criteria.
Which is not ME
I would note that the definition that he’s using has demonstrated autonomic nervous system problems in people with ‘ME/CFS’ in quite a few studies and that those problems are similar to those found by other researchers using other definitions including Dr. Newton and others.
Like I said all I can do is read the research. I can’t reach into Norwegian politics and discern what’s going on there. I really can’t be expected to do that honestly. I understand that he’s considered a problematic figure and I hope he’s not stopping any Rituximab trials but I’m looking at the research; that’s the context I’m looking from, and when I look at Wyller’s research it’s not finding anything different in his field than what other researchers are finding; it’s not indicating ME/CFS is a biopsychosocial illness, it’s not on CBT, it’s physiological research using tilt table and other testing to tease out the abnormalities in the ANS system.
Now you can say you don’t like his definition but since his definition is consistently finding autonomic problems my reply to that basically, is, yes it could probably be improved and it looks like it’s doing alright so far. Its definitions that don’t find anything that I worry about. It it’s finding something and that something makes sense then worry about it? The definition is proving itself so to speak.
Below is a fuller list of his research and here are some of the conclusions from his studies;
1.
Relationship between autonomic cardiovascular control, case definition, clinical symptoms, and functional disability in adolescent chronic fatigue syndrome: an exploratory study.
Wyller VB, Helland IB.
Biopsychosoc Med. 2013 Feb 7;7(1):5. doi: 10.1186/1751-0759-7-5.
PMID: 23388153 [PubMed] Free Article
Related citations
2.
Clonidine in the treatment of adolescent chronic fatigue syndrome: a pilot study for the NorCAPITAL trial.
Fagermoen E, Sulheim D, Winger A, Andersen AM, Vethe NT, Saul JP, Thaulow E, Wyller VB.
BMC Res Notes. 2012 Aug 7;5:418. doi: 10.1186/1756-0500-5-418.
PMID: 22871021 [PubMed – indexed for MEDLINE] Free PMC Article
Related citations
3.
Adolescent chronic fatigue syndrome; a follow-up study displays concurrent improvement of circulatory abnormalities and clinical symptoms.
Sulheim D, Hurum H, Helland IB, Thaulow E, Wyller VB.
Biopsychosoc Med. 2012 Mar 21;6:10. doi: 10.1186/1751-0759-6-10.
PMID: 22436201 [PubMed] Free PMC Article
Related citations
4.
Chronic fatigue syndrome: a qualitative investigation of young patient’s beliefs and coping strategies.
Hareide L, Finset A, Wyller VB.
Disabil Rehabil. 2011;33(23-24):2255-63. doi: 10.3109/09638288.2011.568663. Epub 2011 Apr 7.
PMID: 21473686 [PubMed – indexed for MEDLINE]
Related citations
5.
No differences in cardiovascular autonomic responses to mental stress in chronic fatigue syndrome adolescents as compared to healthy controls.
Egge C, Wyller VB.
Biopsychosoc Med. 2010 Dec 14;4:22. doi: 10.1186/1751-0759-4-22.
PMID: 21156045 [PubMed] Free PMC Article
Related citations
6.
Elevated nocturnal blood pressure and heart rate in adolescent chronic fatigue syndrome.
Hurum H, Sulheim D, Thaulow E, Wyller VB.
Acta Paediatr. 2011 Feb;100(2):289-92. doi: 10.1111/j.1651-2227.2010.02073.x. Epub 2010 Nov 17.
PMID: 21059182 [PubMed – indexed for MEDLINE]
Related citations
7.
Polymorphisms of adrenergic cardiovascular control genes are associated with adolescent chronic fatigue syndrome.
Sommerfeldt L, Portilla H, Jacobsen L, Gjerstad J, Wyller VB.
Acta Paediatr. 2011 Feb;100(2):293-8. doi: 10.1111/j.1651-2227.2010.02072.x. Epub 2010 Nov 18.
PMID: 21059181 [PubMed – indexed for MEDLINE]
Related citations
8.
Blood pressure variability and closed-loop baroreflex assessment in adolescent chronic fatigue syndrome during supine rest and orthostatic stress.
Wyller VB, Barbieri R, Saul JP.
Eur J Appl Physiol. 2011 Mar;111(3):497-507. doi: 10.1007/s00421-010-1670-9. Epub 2010 Oct 2.
PMID: 20890710 [PubMed – indexed for MEDLINE] Free PMC Article
Related citations
9.
Hormonal alterations in adolescent chronic fatigue syndrome.
Wyller VB, Evang JA, Godang K, Solhjell KK, Bollerslev J.
Acta Paediatr. 2010 May;99(5):770-3. doi: 10.1111/j.1651-2227.2010.01701.x. Epub 2010 Mar 1.
PMID: 20199497 [PubMed – indexed for MEDLINE]
Related citations
10.
Can sustained arousal explain the Chronic Fatigue Syndrome?
Wyller VB, Eriksen HR, Malterud K.
Behav Brain Funct. 2009 Feb 23;5:10. doi: 10.1186/1744-9081-5-10.
PMID: 19236717 [PubMed] Free PMC Article
Related citations
11.
Enhanced vagal withdrawal during mild orthostatic stress in adolescents with chronic fatigue.
Wyller VB, Barbieri R, Thaulow E, Saul JP.
Ann Noninvasive Electrocardiol. 2008 Jan;13(1):67-73. doi: 10.1111/j.1542-474X.2007.00202.x.
PMID: 18234008 [PubMed – indexed for MEDLINE]
Related citations
12.
Sympathetic cardiovascular control during orthostatic stress and isometric exercise in adolescent chronic fatigue syndrome.
Wyller VB, Saul JP, Walløe L, Thaulow E.
Eur J Appl Physiol. 2008 Apr;102(6):623-32. Epub 2007 Dec 8.
PMID: 18066580 [PubMed – indexed for MEDLINE]
Related citations
13.
Abnormal thermoregulatory responses in adolescents with chronic fatigue syndrome: relation to clinical symptoms.
Wyller VB, Godang K, Mørkrid L, Saul JP, Thaulow E, Walløe L.
Pediatrics. 2007 Jul;120(1):e129-37.
PMID: 17606539 [PubMed – indexed for MEDLINE] Free Article
Related citations
14.
Sympathetic predominance of cardiovascular regulation during mild orthostatic stress in adolescents with chronic fatigue.
Wyller VB, Saul JP, Amlie JP, Thaulow E.
Clin Physiol Funct Imaging. 2007 Jul;27(4):231-8.
PMID: 17564672 [PubMed – indexed for MEDLINE]
Related citations
15.
Treatment of chronic fatigue and orthostatic intolerance with propranolol.
Wyller VB, Thaulow E, Amlie JP.
J Pediatr. 2007 Jun;150(6):654-5.
PMID: 17517256 [PubMed – indexed for MEDLINE]
Related citations
16.
The chronic fatigue syndrome–an update.
Wyller VB.
Acta Neurol Scand Suppl. 2007;187:7-14. Review.
PMID: 17419822 [PubMed – indexed for MEDLINE]
Related citations
17.
Usefulness of an abnormal cardiovascular response during low-grade head-up tilt-test for discriminating adolescents with chronic fatigue from healthy controls.
Wyller VB, Due R, Saul JP, Amlie JP, Thaulow E.
Am J Cardiol. 2007 Apr 1;99(7):997-1001. Epub 2007 Feb 16.
PMID: 17398200 [PubMed – indexed for MEDLINE]
Related citations
Hi Cort,
I’m new to your blog and newsletter. WOW and THANK YOU.
I have been waiting for an easily digestible summary of this information since I was diagnosed 2 years ago. The specialist I saw explained exactly what Wyller has studied here and I have since learnt a little about the parasympathetic nervous system in my psychology degree. It all makes perfect sense but the neurological details were never clear to me.
Thank you again,
Lordy
Glad to hear it Lordy. I think if you could say this paper was by Byller or Tyller; ie if we could get by the name (I guess there’s too much upset in Norway with Wyller to do that), and I’m sorry to unintentionally offended them, but if everyone could get by the name of the author…I think the paper looks pretty darn good. Next the brainstem…
This is not about Wyller¨s name or about norwegians, you simply display arrogance and ignorance to what his research is about. Maybe you would be better served by taking seriously people who have followed all his research closely for 6 years and all his lectures, editorials etc. This guy is the purest form of biopsychosocial researcher you will find. One of his closest allies is Trudi Chalder. I rest my case.
Well, Lars there’s obviously alot I don’t know about Dr. Wyller. I do like his research -and I disagree with you about that – but it appears that his clinical stance is something I wouldn’t have expected so it is a learning experience to me.
Yeah….I went to all the trouble of logging in, to text (with my one brain cell and one finger) lololol .
Putting the name of the researcher aside, I think this research is problematic in itself because of the broad criteria used.
We in the ME/CFS community are generally – rightly – upset when authors of various treatment studies use broad definitions (basically studying “chronic fatigue”, not ME/CFS), right? I think we should judge all studies by the same standards.
As long as the researchers aren’t using narrow ME/CFS criteria (preferably CCC = Canadian Criteria or perhaps the new ICC, but at the very least CDC Fukuda 1994) I am sceptical of viewing the studies as ME/CFS research.
I don’t fault Cort for dissecting Wyller; his information and the comments here all valuable. Wyler is just another emerging infectious element we have to watch. As said, Wyller isn’t finding much of anything different than others have: it’s what he plans to do with it once he takes some credit. Even Dr. Reeves proclaimed this was a multi-systemic brain illness, while never intent on earnestly getting to the root causes or extent of physical breakdown. Likewise, CBT, GET, LP, amygdala retraining, etc. all posit a mind-over-matter solution ignoring these. The Wessely-APA-IDSA-insurance alliance is definitely counting on DSM-V for help.
Re: perfectionism – By DSM-V, I’d wager I should have been a straight-A’s pill-popper decades ago. Perfectionism may have not always been beneficial, but it’s a far cry from what I have now, sometimes similar to the Lyme patient who almost starved himself to death playing video games. The lost “big picture” went from what was most critical to a project at work, to being able to jumble food (with no appetite), sleep (without proper pituitary secretion), house chores, and calling family matters – none helped by the extra hours stolen by the mattress. The thicker the fishbowl glass is that day, the harder it is to track and prioritize, even moment-to-moment. Especially if that CNS is continually infected and/or poisoned, a simple kick-in-the-rear from some psychiatrist isn’t going to cut it.
It is my very humble opinion that ALL research data ( along with any tentative and/or adamant conclusions) have potential to contain clues that might prove useful to all researchers, to the entire patient community. And that is one reason I love this site: all opinions are welcome , not just those which are ‘fully funded ‘or overseen by those with monetary stakes in the game.
I have seen this as Cort’s main objective from Day One: to give all a voice and to co-ordinate news/data for the good of all.
If anyone is desperate for a ‘fix’, a cure, I am. I am 62 years old. And I have been incapacitated with this since Feb. 3, 1993 @ 11:30 a.m. Before that, I was ill, but ..struggling was the norm for me. As a child I ran constant fevers, suffered inexplicable hypothermnia ( frequent, life threatening) , passed out suddenly with no prodrome, had a dx of rheumatic fever later doubted by the diagnosing physician, wanted to be supine whenever possible ( read a lot) , had even then an alochol and med intolerance..and a penchant for climbing to reach the hidden antihistamine syrups when I was a child. .
I have been sick all my life. I lost a promising career as a flutist and then one as a journalist. I have lost my IQ, the last 20 years and.. a marriage to this illness. I desperately want one model for CFIDS/ME/wtfever to be THE model. And I want a fix, a magic bullet.
Meanwhile, I welcome all voices, input. And hope for civility, and the best research…that which ..suspends ‘belief’, and looks at ALL the facts.
Thanks to all. I know its rough.
I find this component very interesting because patients who are appropriately diagnosised , by leading CFS/ME practitioners, and not being used as a dump for family dr., will all agree this is the most disabling portion of the illness and causes the most relapses. I have had CFS/ME for 20 years. I was in remission during the time I was on Valcyte and Valtrex, but due to pre-morbid liver issues can not take the Valcyte any longer. Since this relapse, the sound and light sensitives have directly correlated to frequent “crashes”, which any patients will attest to as well. What I find interesting, is that I have now been diagnoses with Hemiplegic Migraines, and will have full left or right sided neuro. strokes, (aphasic, left sided weakness or paralysis, flexer pattern with both arm and leg) as well as full paralysis on 2 occasions. My only known triggers….lights and sounds. (failed 10 medications and mineral supplements due to being over sensitive to the drugs) I have to wear ear plugs and sunglasses at all times. I am positive there is a direct correlation to my CFS/ME and these Hemiplegic Migraines. I am just waiting for research to prove it.
Deborah Ann, I’m sorry to hear your story. I too welcome all input and hope to learn from it. I also appreciate the way Cort keeps presenting new information for us to work through. And I take the point of others who are here urging caution. Lynne.
This paper’s conclusion of brain stem dysfunction seems plausible. The methodology, though, prevents me from being swayed by the paper’s conclusions.
This study is an exercise in data mining. There’s nothing wrong with data mining, but it can throw up highly unreliable findings – especially when using a small patient cohort, as is the case here. Also, the cohort wasn’t split to provide any attempt at validation. By way of comparison, the relatively recent study by Duffy and Komaroff on spectral coherence analysis involved data mining, but the Harvard researchers split their cohort into two, performing data mining on one part of their cohort, and testing the findings of that data mining on the other part of their cohort. As Wyller and colleague acknowledge in the text, their study “should be regarded as a framework for explorative analyses only.”
More provocatively, the authors employ an unconventional research concept. Ordinarily, you would seek to identify a well characterised sample, and from this hope to be able to draw conclusions that have generalisable relevance to those with less well characterised pathologies. In contrast, this paper starts with a vaguely defined cohort, and seeks to draw conclusions that pertain to those with far less vague pathologies. This is logically problematic.
Also, implicit in this paper is the assumption that fatigue severity among a group of fatigued adolescents is a basis upon which to rely in seeking to identify the defining characterists of ME/CFS. There is no logical reason to make this assumption.
Two independent papers are cited as the pretext for the employment of such a loosely characterised cohort. These are papers from journals of psychological and psychosomatic medicine. One of the two was a 2004 CDC paper for which Bill Reeves was the senior author (J Psychosom Res 2004, 56:171–178). This was a preliminary paper to the CDC’s empirical case definition. It is interesting that the data mining approach of Reeves and colleagues in that paper is conceptually analogous to the approach employed in Wyller’s paper. This quote from the Reeves study illustrates this point by explaining that his study:
“measured the occurrence of 21 symptoms in 1391 chronically fatigued subjects who did not report fatigue-associated medical or psychiatric conditions. We used factor analyses to identify symptom dimensions of fatigue and cluster analysis to assign subjects to subgroups.”
That is to say, both the Reeves and Wyller papers used data mining to try to hone in on the nature of the illness, and both started with loosely characterised fatigue cohorts. Such approaches are prone to unreliable findings. Reeves’ findings are now widely understood to have proved unreliable.
In general, the research tactic of employing a loosely characterised cohort is undesirable, because it decreases the probability of reliable findings. Rationalisation of this approach in the case of ME/CFS invariably comes from the psychological and psychiatric literature. It is impossible to ignore the elephant in the room in relation to this approach in ME/CFS research, namely that encouraging the use of this approach is one of the main tactics employed by the Wessely School in their attempts to reconceptualise ME/CFS as a psychosomatic condition. Aside from such agendas, it is puzzling why any researcher would choose to use a loosely characterised cohort.
I have been following research for these disorders plus doing my own for 17 years now and I agree with Wyller that all these disorders are of the same cause. I do not believe though that the brainstem (reptilian brain) is the where it all starts but rather the limbic system (animal brain) and that we are actually reverting to the reptilian brain in order to survive. The brain filters in the limbic system are faulty which result in hypersensitivity and this has been shown by a reduction in gray matter in these areas and this is only one example. There has been little research in the area of steroid hormones even though some studies have shown severe problems in this area proving a continual switching on of the fight/flight response. An over production of cortisol will result in a shortage of pregnenolone which is the steroid hormone precursor and which is produced by the mitochondria (itself an ageing evolutionary addition to the human body). A shortage of pregnenolone will lead to decreased levels of sex hormones and accelerate ageing. These disorders have often been described as rapid ageing and with ageing comes weakened muscles, muscles filled with trigger points caused by an imbalance in hormones. The faulty animal brain will gradually weaken the reptilian brain as well because a diminished supply of steroid hormones will affect the supply of norepinephrine from the LC. Pregnenolone is neurogenic and can help repair damaged areas of the brain but whether it can stop the hypothalamus from pumping out CRH is anyones’s guess.
I don’t know alot about pregnonolone but I do know of one person who does very well on it. I looked it up; its a really interesting neurohormone; its neuroproective and it may be able to improve cognition. It’s produced in the brain. It’s also has anti-anxiety properties.
I forgot to add that studies showing increases in gray matter in areas of the neocortex reveal, I believe, that the human brain is trying to overcome the faulty animal brain and to prevent complete reversion to the reptilian brain. It is more successful in this in fibromyalgia rather than ME/CFS which is a more acute form and has had less time for significant brain changes to occur.
Great, more brain , nervous system stuff!
This is where the gold lies, forget the viral research – that is going nowhere, a total waste of time and money.
Focus on the brain!!!!!!!!!!!!
Thanks for this Cort. I do think the ANS is the core problem. (I’ve had tests that show all the ANS dysfunctions that Whyller talks about.)
I’m interested in what he says about norepinephrine. I haven’t been able to access the full article – is he implying that we have too much of it, or is this too simple? The thing is, my pain and wired feelings have been reduced by duloxetine (Cymbalta) which increases the availability of norepinephrine. This drug seems to be quite effective for about 50% of fibromyalgia patients. On the face of it, this seems rather at odds with what Whyller is saying, if he is arguing that we have too much.
Wyller found increased NE in a study about 5 years ago…but NE appears to be reduced in FM and SNRI’s like Duloexetine are recommended. Yes, it is directly opposite to what he’s suggesting. On the other hand low NE levels appear to be associated with increased pain sensitivity….so your example fits as well. Wyller didn’t measure NE in these patients so he’s going on conjecture as the cause of the hypersensitivity.
My question concerns the part that norepinephrine plays in this process. Many patients with ME/CFS also have fibromyalgia and are prescribed SNRI’s such as Cymbalta. Am I understanding correctly that a norepinephrine re-uptake inhibitor would actually make our symptoms worse?? It definitely increases my anxiety!
I would approach Wyller’s conclusions with caution given that he did not measure NE. He found NE increased in a couple of studies about 5 years ago but people with FM appear to have low NE – which is associated with increased pain. I think more research needs to be done until we can say confidence anything about NE and ME/CFS.
Autonomic dysfunction and hypersensitivity as originating in the brain are very clear parts of this illness, in my opinion, so I’m glad it’s being discussed. However, I don’t understand the seemingly random hypothesis being thrown out there that M.E. may be the same illness as FM, IBS, etc. He lost me – what is the evidence for this? There are people who have solely one of these and appear not to have the other: there are people with Fibro who do not have broken immune systems nor the symptoms that come with the more permanently debilitating M.E., there are people who have IBS but do not have Fibro, there are people who have M.E. who do not necessarily have the other two. How can these all be the same illness, if for those who have an isolated set of symptoms that do not include the other 2 illnesses, treatment and even cure is possible that directly conflicts with what works for the others?
For instance, for those who have Fibro for a time, say after an accident, so many have been proven to go into remission, if not cure, with a careful program of gradual graded exercise. On the other hand, it has been proved that for those with M.E., that same program is the kiss of death for their systems. Those with IBS may be cured through wiping out a yeast issue, but that same tactic would not by any means cure a person of M.E., or of Fibro.
Consider that I have dealt with all 3: the IBS ended through following protocols for yeast, and also Dr. Chia’s Equilibrant for intestinal-born illness/Coxsackie B1-6; the Fibro was all but cured (I’ll say put into remission, as it still can rearise but has essentially been put to sleep) through a year and a half of LDN – anti-depressants and graded exercise were not safe options for me as they are for other patients who may have had only FM; and yet, the M.E. continues, and my NK cell count is abysmal. My brain is a little confused today, so it’s hard to explain what I mean here, but it would seem to me that if contraindicated treatments/cures such as graded exercise and no graded exercise are appropriate for FM vs. M.E., and issues like IBS can be cured without affecting the other two, how can these all be the same illness with the same cause? It didn’t seem to me that he cited any clear reasoning for this that would take into account the evidence to the contrary, so if anyone has comment about this, or can explain the reasoning for me, please do. I was trying to follow what he was saying, bu it seemed a little vague and scattered in parts. But again, the original premise that autonomic dysfunction and hypersensitivity are markers for the disease in the brain and might be tied to the cause seemed good. But I don’t understand how that indicates that M.E., FM, IBS, etc. are all the same illness – there are other potential biomarkers, such as low NK count, and high viral counts that they do not have in common for all patients, and they can be be independently treated with opposing treatments.
Cort,
you do a lot of good things with this blog, and you should have praise for that, but your embrace of Wyller research and your wrongful and incorrect interpretation of what this is about for international patients and readers are absolutely appaling. When you also are trying to correct representatives of one of the Norwegian patient organisations, Eirik Randsborg, about the reality of Wyller and his research you simply do not know what you are talking about. These are people who have sat around the table with Wyller for several years, trying to fight Wyllers´ insistence of adapting NICE guidelines in Norway, as Wyller has been one of the chief advisors to the Norwegian health authorities for several years.
To all readers and patients out there, you need to know that Dr. Wyller is to Norway what Simon Wessely is to the UK and what William Reeves used to be to the U.S. He has no interest in doing anything meaningful for people with ME/CFS.
I was touched by the efforts of Bob Miller on Ampligen, and shared the heartbreak of US patients seeing Dr. Komaroff voting it down. It is therefore with anger, frustration and disbelief see Cort promoting the “smoke and mirrors” of Wyller, in a time when patients more than ever need to come together on a global basis to support eachother.
Cort, who covers the topic of ME/CFS on a continuous basis should be expected to understand this. Ignorance and good intentions are not an excuse.
I understand your frustration, Lars but I hope others have a more even-handed take on this. As I noted previously I didn’t know the situation in Norway and really can’t be expected to. (I do now).
So far as correcting Eirik on Wyller’s research by posting the conclusions of Wyller’s studies on a comment; I fully stand by that. Whatever Wyller’s doing with his research in Norway, most of his research, as I noted, fits in well with other researchers findings and no has cared to rebut that.
Call me naive but I am really, really opposed to trashing a study or work based on the author of it. We had the same attitude with regards Reeves in the US; that whatever he did was wrong but Reeves did pen several fundamentally important studies including studies that verified the huge economic impact of ME/CFS. Those studies have been immense assets to the ME/CFS community. I think its better to take each research study on its own merits.
I want to make very clear what I am for and what I am opposed to on the treatment end. I’m for anything that works…for somebody. That means that if some people feel better after using Amydgala Retraining or LP or whatever I’m for it. If it means people getting better using Rituximab or Valtrex or Xafaxin or Klonopin or Propanolol or whate ver, I’m for that too. I personally know of people who’ve gotten results from everyone of those treatment modalities.
What I’m irretrievably opposed to is anyone on either side cutting off the other. That means if Wyller is trying to cut off funding for Rituximab studies I’m absolutely opposed to that. If you’re going to automatically negate Amygdala then I’m opposed to that.
This is a very big community with all sorts of degrees of sickness and probably quite a few subsets. It’s going to take awhile for everything to settle; what works for who and what doesn’t work for who. I certainly can’t figure it out and that’s what you’re going to see blogs on all sorts of treatments on this website.
So, if Wyller is trashing Rituximab then I think he’s probably a rather small-minded individual who’s too focused on his own thing…as many researchers are…They think they’ve got the answer but I believe, in fact, I know – there are many answers to ME/CFS…
When you say better with Gupta, is that better as in improved or fully well? Thanks.
One person almost fully well, several people much better and some with not much success :). It’s like with almost every treatment…there’s quite a mixture…but that’s what you would expect in a diverse illness. Even as well characterized disorders like cancer feature several different options…it depends on the patient.
Same with pain medication – its amazing how differently people with react to the same pain medication. This mix of results is what is to be expected, I believe.
I think the problem and fundamental difference between us is that you describe various fprms of Chronic Fatigue and ME/CFS as if they were the same. That is exactly what the biopsychosocial school wants people to believe, and they are using unethical and, in some instances, borderline criminal methods to keep it that way. To me, ME/CFS as described by the CCC is one unique disorder.
Ignore Lars – he is just a troll and it’s abundantly clear that he doesn’t really know what he is talking about. Unfortunately the CFS world is full of people like him. Keep up the good work, Cort.
Well I don’t mean to imply that…Actually I really don’t know.l just talked to somebody who’s had a remarkable near recovery probably from near death – by going on Valcyte. He had a huge pathogen problem…I don’t know if I do or not…but we did have symptoms in common.
Is it all one disorder with all sorts of branches? I think it’s possible and I think its possible that its a number of very separate disorders that all look similar. It makes my brain hurt to think about it to tell you the truth. 🙂
I, like you, was very taken by the Rituximab results…I cherish the thought of being able to exercise regularly and being well – and it’s clear that Rituximab can achieve that in some people, so I very much oppose anyone who would try and stop further investigations – particularly in Norway where it seems the federal government will (in contrast to here) fund those types of studies. If Wyller is doing that then he’s doing, in my opinion, a very negative thing.
Thank you for this article. Unfortunately I have not managed to read through all the comments so please forgive me if I am repeating what has already been said.
What I read here fits with my experience. I have had an added experience that may shed some light on the noradrenaline connection, so I wanted to add it in case it switches on any lights for researchers.
6 or so years ago I started taking edronax to help with ADD. It is a noradrenaline re-uptake inhibitor. I have been in pain with fibromyalgia since age 4, so it came as a shock to me a few days after starting to realise I was not. This state lasted about 6 months, without pain to guide me I may have been overdoing things, but the downfall came after a series of stresses, both emotionally from my family and physically after moving into a house that’s situation allowed it to reach 50 degrees Celsius inside during a heatwave while I was recovering from the move.
I still take the edronax as my ability to focus is noticeably better on it, and my pain level is lower when on it, but I believe that during that time my CNS reset and adapted to the new level of noradrenaline. I have gradually declined and developed all the ME criteria since then and, after pushing my boundaries too far once again 18 months ago, I am housebound unless I have significant help to go out.
How interesting, Julia and thanks for the tip on a drug I had never heard of. Good luck with everything.
In response to Sunshine, the hypothesis that these disorders are one and the same is certainly not random. As far as I see it, an over activation of the sympathetic nervous system could easily account for all these similar disorders and I include PTSD and Gulf War Syndrome amongst them, and that what caused the over activation would be the more appropriate question to ask. How this over activation manifests in each case would depend on what time of life it occurred, what severe stress to the body proceeded it, what one’s nutritional status and toxic load are and what single nucleotide polymorphisms you have that have been associated with one or more of these disorders. In other words, there are many factors, including genetic, that can determine how your body will respond to an over activation of the sympathetic nervous system. Everyone will be slightly different. IBS, though, can be regarded as just a symptom of this over activation as it is known that high levels of cortisol cause a serum alkalinity and the body will take acid from the stomach to rectify this situation. Once the pH levels of the digestive tract become unbalanced, digestion is affected and toxic substances and candida overgrowth can occur causing symptoms of IBS.
As well as a demand for cortisol, an over activation of the sympathetic nervous system will create a high demand for adrenalin and NE from which it is produced. Dopamine stays on a par with cortisol and so more demand on the catecholamines as less dopamine available for production of NE. A high level of nutrition is necessary to keep up with all these demands. Cortisol is anti-inflammatory and high levels will suppress the immune system creating cytokine changes and leaving one open to increased viral counts and any infection happening along. As the demand for cortisol and NE becomes chronic, the ability of the body to keep producing these hormones diminishes, especially in women at the menopause as the demand for oestrogen compromises the production of cortisol even further. This creates a move towards acidity and an over active immune system, possibly increasing one’s susceptibility to autoimmune disorders. Still the same illness, just a different part of the process.
As for pain, I believe it is caused by trigger points or knots that are created in all the muscles due to continual fight/flight responses, during which muscles tense up. An imbalance of hormones will maintain these trigger points which early on only manifest as overall weakness and then later start to refer pain which over time gradually increases in intensity, especially during a flare-up of illness. Manual de-activation of these trigger points and supplementation with hormones can do a lot to reduce central sensitisation and overall hypersensitivity as I have found from my own experience.
I think it is an excelent biomedical description of symptoms, but the cause may be diverse. If this vicious circle would be last by incentives patients without these incentives must become better again. That is not the case. So there is something terribly wrong with the fight / flight system and autonomic nervous system. What causes this abnormal response? Or is this a compensatory response? This is essential to know. I agree with Lars that Wyller is thinking the other way around i.e. mental stress etc… is the cause… i do not agree but i think that the mechanisme Wyller descripes is broken and explain our symptoms.
I strongly agree with the points brought up by Humphrey, especially the ones below! Thanks, Humphrey!
Humphrey says:
“Also, implicit in this paper is the assumption that fatigue severity among a group of fatigued adolescents is a basis upon which to rely in seeking to identify the defining characterists of ME/CFS. There is no logical reason to make this assumption.
Two independent papers are cited as the pretext for the employment of such a loosely characterised cohort. These are papers from journals of psychological and psychosomatic medicine. One of the two was a 2004 CDC paper for which Bill Reeves was the senior author (J Psychosom Res 2004, 56:171–178). This was a preliminary paper to the CDC’s empirical case definition. It is interesting that the data mining approach of Reeves and colleagues in that paper is conceptually analogous to the approach employed in Wyller’s paper. This quote from the Reeves study illustrates this point by explaining that his study:
“measured the occurrence of 21 symptoms in 1391 chronically fatigued subjects who did not report fatigue-associated medical or psychiatric conditions. We used factor analyses to identify symptom dimensions of fatigue and cluster analysis to assign subjects to subgroups.”
That is to say, both the Reeves and Wyller papers used data mining to try to hone in on the nature of the illness, and both started with loosely characterised fatigue cohorts. Such approaches are prone to unreliable findings. Reeves’ findings are now widely understood to have proved unreliable.
In general, the research tactic of employing a loosely characterised cohort is undesirable, because it decreases the probability of reliable findings. Rationalisation of this approach in the case of ME/CFS invariably comes from the psychological and psychiatric literature. It is impossible to ignore the elephant in the room in relation to this approach in ME/CFS research, namely that encouraging the use of this approach is one of the main tactics employed by the Wessely School in their attempts to reconceptualise ME/CFS as a psychosomatic condition. Aside from such agendas, it is puzzling why any researcher would choose to use a loosely characterised cohort.”
Why Wyller would choose to go out on his own and create a new definition that is bound, particularly in this disorder, to raise questions is a good question. He must feel he gets something out of that and he must realize that he loses alot as well; people are less likely to accept his findings, for one thing. It would be interesting to find out.
Cort, I have criticed you heavily for this article, maybe using too harsh words, but I think Anne and Humphrey have said the same as I me, but in more academic terms. It boils down to what researchers want to do with their research, and Wyller has a clear agenda with his, which you don´t seem to see or acknowledge. We in Norway live with this everyday, where desperate patients are being preyed on by profit seeking LP-coaches supported by Wyller. If they get worse after these 3-day miracle cures, its their own fault….the Lp course in itself is fine, its the unethical marketing and outright lies about its risks that are the point to me.
It is difficult for me to reconcile pleading for international support for Bob Miller on Ampligen one day, and praise the work and drawing erroneous conclusions from a study written by Wyller the next day, knowing the damage and grief he gives patients in my country. The reality gap is just too big.
It seems to me that I may have misunderstood what your blog was about and what your aim is with it. I apologize if I have offended you, not my intention! Maybe we have both learned something from this.
Or maybe people like me are just trolls who really don´t understand what is going on in his own country and with a disease that he has had for decades.
I’m not very well informed on Wyller’s work really, but I have seen in different contexts that he seems to be quite steadily rooted in the framework of Bodily Distress Syndrome (BDS)/Bodily Distress Disorder (which also is called ”functional somatic syndrome”.
http://funktionellelidelser.dk/en/about/bds/
Bodily Distress Syndrome is a more modern version of somatization disorders. The researchers and clinicians do acknowledge that there are somatic dysfunctions causing patient to suffer, but the thinking seems quite focused on explaining the syndrome as a consequence from prolonged exposure of different types of stress (not only psychological). What’s central is that they think that different syndromes like FM, ME/CFS, IBS, chronic pain etc are really just different manifestations of the same type of ”functional somatic syndrome”. There you see a plausible explanation for his disinterest in sharp diagnostic criteria. CBT, GET and other psychological treatment methods are seen as the main solution to the problem.
That doesn’t mean that Wyller is inherently evil in any way, although I think his opposing of biomedical explanations for ME/CFS has been harmful for the ME/CFS research. His influence is being linked by the ME community to how ME patients are being denied the kind of care they are looking for, and a disinterest in the massive physical pathology in severe ME cases. I agree with Cort that we shouldn’t automatically trash his research, but some of the quirks of the article is easier to understand if one knows what research tradition he is rooted in. Even the functional somatic syndrome approach might yield important research results though.
As has been noted already in the discussion there’s nothing that says that the pathology of the most severely affected *necessarily* says anything about what mechanisms are at the core of the development of the pathology. It might be that what causes the severe symptoms are a core mechanism, but it might as well be some problem that for some reasons follows as a secondary problems in some subset of patients.
This is not really a new idea, given what myalgic encephalomyelitis means. However, it makes a lot of sense compared to my symptomology (it is assumed that my first episode was at 6 years old,and I am now 60). I would like to see further research done on Wyller’s ideas, in sync with other similar research being done. And let’s hope that more research — and well researched testing — will be done in Canada.
I agree that all this is nothing new. Issues with cortisol, NE and dopamine in these disorders have been known about for a long time. It is a known fact that lack of dopamine causes cognitive problems and that a fight/flight response entails hypersensitivity to one’s surroundings. However, just because Wyller recommends or recommended in the past treatments that are not effective does not mean that his explanation of the processes of the disease are wrong, just that he is going about treatment in the wrong way. Frankly, I think he needs to do a lot more study in the area of neuroendocrinology before he rushes in where angels fear to tread. And what does it really matter if the cause is mental or physical, the evidence pretty obviously shows that something has gone physically wrong with the brain and that it most likely happened in very early life, perhaps even in utero; most probably in people with a genetic susceptibility though the most common polymorphisms associated with these disorders are variations to help compensate for the dysfunctional neurotransmitter systems rather than causing them. The only difference in these people being how far along in their life when the crunch finally came and I have noticed that it seems to be happening earlier and earlier. I have FM which used to be called rheumatism and used to be something only our old grandmothers had but which now children are getting. It is not something I believe that can be easily cured though there have been recent claims of repairing damaged brains through mental exercises. Neuroplasticiity can be a bad thing but can also be a good thing as it means the brain can heal itself, given the right conditions. CBT may teach one how to cope with the symptoms of these disorders but it is definitely not a cure and some may benefit from GET if you catch them early enough in the process but it can do a lot of damage in most cases. I see so many studies claiming that FM can be improved with exercise but have not heard personally from anyone who has. I was diagnosed with FM and have no fevers or swollen lymph nodes, but any exercise will put me in bed and in pain for days at a time. I have trigger points in every muscle of my body which will never completely go away due to the disarray in my endocrine system and it is known that trigger points can spread to the skin, ligaments and smooth muscle, even the heart, which could be a contributer to the post-exertional malaise. This huge peripheral input is believed by many to contribute greatly to central sensitisation and may be the only cause.
The exchange in the preceding comments raises an interesting question: whether to judge every academic paper on its merits (as Cort suggests) or whether to approach papers with a bias according to the track record of the author/authors (as some of our Scandinavian friends suggest).
There is no correct answer – both contentions have merits and flaws.
If you judge every paper on its merits, you won’t miss anything but you’ll waste a lot of time and take lots of junk seriously.
If you approach papers with a bias, you’ll dismiss some important findings.
A similar question is whether to place more trust in high impact (prestigious) journals than low impact ones.
We’re the last group who should ignore the lessons there are to learn from the history of research into gastric ulcers – an infectious disease long dismissed as a psychosomatic condition, notwithstanding various researchers having published evidence of an etiology of bacterial infection.
On the other hand, if you read a Wessely paper in isolation, or if you listened to Sharpe being interviewed on the radio, and didn’t know the background, you’d could easily come away thinking they are doing useful and compassionate work.
After reading up on Wyller it is crystal clear that he is part of the CDC, Peter White, Simon Wessley et al cabal (in fact his website is chock full of research by the usual suspects) to label ME as a medically unexplained somatization disorder. I cannot fathom how anybody in our situation could look at anything coming from this group as helpful no matter what the content is. Their position is clear: throw all of us with unrelated conditions into a massive group and declare that we are the same. Then do “research” on selected “cohorts” and say that we are somehow the same and that the “solution” is CBT and GET? The Psychs are happy as this is a nice business development project for them and insurance companies and doctors are happy because they don’t have to deal with a difficult to treat population.
Look at what they do/who they hang out with not what they say.
floydguy,
excellent summary of reality, in addition the Psychs also play the “divide and conquer” game successfully with ME/CFS patients, and that breaks my heart more than anything…
Yeah, I wish despite our likely different conditions and viewpoints we could ALL agree on some high level things.
I don’t even think I could agree on “more funding”. If money is going for mind-body research, I’d rather not bother. I actually do qi-gong, mindfulness and other stuff to alleviate symptoms and make me more functional but there is no way this getting at the root cause.
I think some things we might be able to agree on:
– Strict transparency in research – put significant pressure on governments and others to conduct “proper” research studies
– Put pressure on Psychs to replicate their BS studies (where is the outrage over inability to replicate this outside of pre-selected research populations?)
– Strict cohort and subset definitions based on proven lab tests (every day we talk about all the different lab abnormalities we have, why doesn’t research acknowledge this, rather than select based on “fatigue” and stupid questionnaires)
– Pressure on Psychs and others that significant improvement/recovery isn’t taking 3 more steps after their miracle cures (I walk over 10,000 steps a day but still have the VO2 max of somebody in heart failure, what’s up with that??). It doesn’t seem like rocket science to base recovery on something other than interviews and questionnaires.
Andrew
I certainly don’t think that wasting time arguing over definitions and politicking is getting anyone anywhere. If the world is flooded with studies from people with vested interests, then why don’t we as individuals flood the internet with our own ideas. This is the best way for ideas to take hold and become reality. Rumours and myths become more valid in society than obscure studies that promote yet another drug or put money into the pockets of psychs. What made me think of this was Humphrey mentioning the fact that gastritis and peptic ulcers were once dismissed as phychosomatic disorders, in other words, due to stress. This notion came about as rumours and myth became rife that stress was only a mental disorder whereas the fact is that environmental stress has the same effect on the body. Extremes of environment, poisoning, poor nutrition, overcrowding, elevated noise levels, excess lighting, etc, all take their toll. There are also two types of stress, negative (distress) and positive (eustress) but with CBT and GET, the psychs are only treating mental causes and eustress. When the body is “distressed”, exercise will only create a bigger demand on the stress system, thereby making the situation worse. I love the explanation given by Hans Selye in 1926 as to the ambiguity of the term stress when he said that stress “in addition to being itself, was also the cause of itself, and the result of itself.”
I agree with Floydguy to forget more funding – there are too few genuine researchers in this field. We need to do our own research into the working of the stress system and spread the word to make the world more familiar with the fact that stress is not just mental and cannot necessarily be corrected by exercise.
By the way, the Nobel prize was awarded to the two scientists for their discovery of helicobacter pylori which they proved caused gastritis by one of them infecting himself but they did not actually prove that this gastritis continued on to form ulcers but common rumour and myth would have you believe otherwise. These two guys are actually from the city I come from in Australia and I have worked in both hospitals they have done research in which is why I have taken an interest. Despite their discovery, they have been unable to give an explanation as to why this bacteria overgrows in some people whereas it is known to be present in the stomach of over 50% of the world population and believed now to be part of the normal flora of the stomach and involved in regulation of acid production. Just goes to show that the cause could still be put down to stress as stress causes alterations in the acid/base balances of the digestive system which could favour overgrowth of this bacteria.
There are good valid points being made in all of this discussion here. However, I just want to comment that I have thought for a long time that autonomic dysfunction and CFS are likely part of the same thing – at least in some cases. Both of my kids, now young adults, were initially diagnosed as POTS, though they both clearly meet criteria for CFS as well and CFS was also officially added as a dx for my son. I have long ago come to the conclusion that its all part of the same thing. I also believe that there are likely various forms of CFS as to cause but I do believe that when autonomic function and CFS are seen in a patient that there is a central cause regardless of what name(s) we give it. I also believe that because all of this is clearly still a mystery and that there are likely various causes that it is important to look at all research
As to hypersensitivity, that has definitely been a part of our picture but in various areas. Sensitivity to smell and to crowds are biggies in our case as well. The light and sound issues have improved over time but were a huge issue in the early stages.
Wyller’s thoughts that possibly things like fibro and IBS may also be part of the same is also interesting to me. My Mom also has fibro and has had mild autonomic issues through the years. We also have IBS in our family including myself and I have also had intermittent mild autonomic issues through the years. It’s also interesting that in chatting with others over recent years that fibro and similar are commonly present in family members of those with CFS/autonomic issues. Given all of this, I have long had a hard time believing that there is not at the very least a connection of some sort between these. Certainly an autoimmune connection comes to mind as well. Thus I also find the research about possible autoimmune causes very interesting.
While I certainly understand and appreciate some of the concerns raised here about Wyeller, this research is extremely interesting to me because it certainly fits our picture, something I’ve felt for several years now. To bring in the possibility of fibro etc also being related makes it even more interesting because of our family picture. At the same time I am also very interested in the autoimmune research as we have such a strong history of autoimmune issues in our family. I think the bottom line is we have to be open to all research as it will likely be various pieces of research that ultimately hopefully leads to finding some answers and also because there are very likely various causes and subsets in the first place. Cort, thank you for all you do in keeping up with this info, sharing, and for those like me putting in simpler terms. And thanks to all for sharing.
Hi
something different, but I hope equally worthwhile: migraine sufferers have also hypersensitivity to sound and light and other things.
I developed migraine when I was 11, it got worse over the years and when I had an attack I couldn’t stand light, sounds, smells, food, movement; I had to stay in bed in a cold room and wait patiently till the attack was over and I could drink and eat again. After an attack which could last for 3 days, I would feel this terrible fatigue.
Things got a bit better when I omitted dairy, in terms of severity (no more barfing) but then, five years ago I became ill with CFS and fibro (am 59, Belgian); I had headaches every day and if I didn’t take painkillers they would turn into migraines, so I took a lot of them. I have always felt that there is a connection between migraine and CFS but I do think there is more to it than a disfunctional brain, but if we stick with it for the moment, shouldn’t we also ask : ” What is it that makes the brain disfunctional?”
Six months ago I started a really simple form of Qi Gong (Shibashi) and almost from day one the headaches were gone!!! I only get a headache now when I eat something that has additives in it. Dizziness has also been reduced with 90%. This is so empowering, you only have to do it yoursel^f, preferably daily for 10 to 15 minutes ( you can even do a sitting form) and for those that are housebound, like I am for many days: you can learn it from a video or dvd like I did.
As far as researchers and doctors are concerned, unfortunately I think that many of them are more interested in their own succes than in the welfare of their patients and for many of them it is difficult to remain open minded, they tend to think inside their own box.
Recently I reread “Amalgam Illness” by Andrew Hall Cutler, quite helpful in making me understand why my diet has to be so limited.
Thanks for your site, keep up the good work!
Ria
Amazing Ria and a hearty congratulations! So QiGong helped alot with headaches and migraine and orthostatic intolerance…that is so cool :). I guess its a stress reduction/energy enhancement type of exercise/meditation. I wonder if it evened out your blood flows or reduced some sort of stress chemicals your body was producing??
That’s really something.. How are you doing with fatigue and other symptoms of ME/CFS?
Hi Cort
fatigue, sleeping disorders, IBS, chronic gastritis, shortness of breath still the same.
Qi Gong is also helping to keep an inflammation of a shoulder muscle and thumb tendon in check.
Heart “flutter” has gone, fibro is approx. 20% less.
Doing the exercises calms my body and my mind; I used to feel guilty because I can’t meditate at all (always had trouble but now it simply is impossible), now I don’t anymore!
I expect I’ll reap more benefits the longer I keep doing it.
Maybe I should also mention that one and a half year ago I started taking a good quality reishi and that has helped me a lot, especially with clearing my head. I used to have this tension in my head and that has diminished quite substantially.
So, without meaning to, I stumbled into Chinese traditional medicine.
It is my sincere hope that more people with CFS/ME learn more about Qi Gong and try it; it has not cured me but it sure has alleviated some very bothersome symptoms.
All the best.
Years ago I left work with a horrible headache and went to a free outdoor class in Tai-Chi, (my one and only). By the end of the class my headache was gone. I was totally surprised and happy. I was truly amazing about how much better I felt, from one class.
Recently I decided I wanted to try and learn Tai-Chi, anything to keep my body moving because I’ve have FMS/CFS, and Nueropathy for 13 years, so I did a lot of digging on the Net for an introductory DVD that wouldn’t break the bank. After digging around I found a nice site that teaches Shibashi (QiGong). Lot’s of good info on how to do it for free, or buy a DVD for $50.00.
On the “aside” this is an interesting article, as are the comments. I looked at the list of symptoms and have all but one.
Thank you for this site.
Ugh! I forgot to add the link. 😛
http://www.taichi18.com/
I retired from the Oak Ridge Department of Energy facililities in Tennessee last year. I was diagnosed with CFS and Fibromylgia and severe depression.
I was working when we didn’t take safety precautions working at the 3 Nuclear Sites. I was exposed to many ugly toxins in the early days. Have these two disorders been linked with the Oak Ridge sites?
Cort,
Your stuff is great.
Any idea about the link between bain stem dysfunction/overactivity and oxidative stress in ME/CFS sufferers?
ME CFS etc is caused by irregularities of energies..
Healing takes place in mind first then body follows…which explains
Why 1000s ppl who recovered had 1000s different reasons that healed them.
Don’t look for reasons coz you never find it what causes it!
But all I can say all is unseen on subconscious levels, fears energies coz
ME etc.. Even consciously. You are not afraid..
Read bible healing quotes.
Bless you all
Vegard Bruun Wyller is highly criticized by a Norweigan ME association (ME-foreningen). In an interview he makes some statements that supports that he is a problematic figure. He says Wessely is an outstanding researcher.
Vegard Bruun Wyller is also a firm believer that a strict “training program” is very important. He does not seem to understand that patients have ups and downs (relapses) and that it is therefore very difficult to adhere to a strict program where one does not continuously adapt the activity to ones present state. Who would for example prioritize walking 100 m, if one has not showered for a week, or has not had the energy to prepare a proper meal for days? Who would not like to have some variation in its life? I would get crazy if I did not have some variation in what I do. Sometimes I feel a strong urge to do some errand outside my house, but I can only do it when I feel a little stronger and still I have to push myself with a lot of willpower do so.
http://nhi.no/forside/intervju-med-vegard-bruun-wyller-om-kronisk-utmattelse-23728.html?page=5
Wessely er en av mange internasjonale forskere som gjør mye god forskning.
Translated:
Wessely is one of many international researchers that do very good research.
http://nhi.no/forside/intervju-med-vegard-bruun-wyller-om-kronisk-utmattelse-23728.html?page=6
Hvis du bare klarer å gå 100 meter, så skal du aldri gå lenger, men samtidig skal du gå akkurat denne distansen regelmessig.
Translated:
If you can only walk 100 meter, than you shall never walk further, but at the same time you should always walk this distance regularly.
More about Vegard Bruun Wyller below. He is clearly a controversal figure in Norway, and many patients are bothered by him. The adult care unit for ME is good, but the child care unit for ME where Vegard Bruun Wyller Vegard Bruun Wyller works is highly criticized.
http://tidsskriftet.no/article/1561146/
‘Det er usikkert hvilke typer behandling som hjelper, men tidligere studier viser at kognitiv atferdsterapi og gradvis økning i aktivitetsnivå har best effekt.
Translated:
‘It is unclear which type of treatment that is effective, but earlier studies shows CBT and GET have the best effect.’
http://translate.google.com/translate?hl=en&sl=no&tl=en&u=http%3A%2F%2Ftidsskriftet.no%2Farticle%2F1561146%2F
shortlink: http://tiny.cc/glch8w
http://marthashave.wordpress.com/tag/vegard-bruun-wyller/
Here about the different approaches by the adult ME clinic and the child ME clinic in Norway.
http://translate.google.com/translate?hl=en&sl=no&tl=en&u=http%3A%2F%2Fmarthashave.wordpress.com%2Ftag%2Fvegard-bruun-wyller%2F
shortlink: http://tiny.cc/wdch8w
http://www.dagbladet.no/2011/12/01/kultur/debatt/kronikk/helse/me/19240927/
Critics by Annette Gije of the Norwegian ME Association
http://translate.google.com/translate?hl=en&sl=no&tl=en&u=http%3A%2F%2Fwww.dagbladet.no%2F2011%2F12%2F01%2Fkultur%2Fdebatt%2Fkronikk%2Fhelse%2Fme%2F19240927%2F
shortlink: http://tiny.cc/8pch8w
For more results make an internet search with
“Vegard Bruun Wyller kronisk utmattelsessyndrom”
https://www.google.se/search?num=100&newwindow=1&safe=active&site=&source=hp&q=Vegard+Bruun+Wyller+kronisk+utmattelsessyndrom&oq=Vegard+Bruun+Wyller+kronisk+utmattelsessyndrom
shortlink: http://tiny.cc/vvch8w