

Tomorrow in a webinar the CFIDS Association of America will provide the results of Shukla’s study looking at the effects of exercise on gut flora and gut permeability in chronic fatigue syndrome (ME/CFS).
Could leaky gut be contributing to post-exertional malaise?
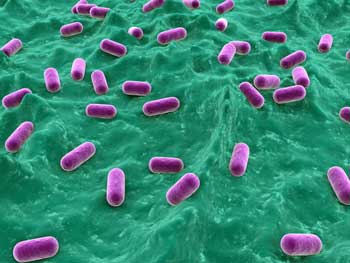
We know the gut is affected in ME/CFS; we just don’t know how much and what role it plays. Low levels of good gut bacteria, leaky gut, high rates of enterovirus infection (stomach), and gastrointestinal complaints have all been found in ME/CFS. Now, not only is Shukla going to give us a really comprehensive look at the gut flora in ME/CFS but we’re going to see how much exercise, the big bug-a-boo in this disorder, affects it.
If it does then a new treatment avenue and a new understanding of this disorder opens up. This is a small study – a pilot study – but the word thus far has been that the findings are ‘significant’.
- Register for the Gut Microbiome and Exercise Webinar at 1pm EST May 2nd
Exercise and the Gut
Exercise was a key part of the Shukla study so let’s take at look at what happens to th gut when we exercise.

Reduced blood flows and gut lining problems after exercise can take their toll – even in some healthy people
Exercise, even in healthy people, puts a lot of strain on the gut because of the need to direct blood to the muscles and away from the gut. In healthy people this isn’t a problem; in fact, the gut uses only about half of the oxygen available to it, so it’s easily able to shunt oxygen-rich blood to the muscles when asked to. That doesn’t mean there are no effects, though; blood flows to the gut drops dramatically during exercise and digestion and the passage of foods through the gut slows.
This is all made possible through our old friend, the always-activated sympathetic nervous system. We might expect problems to occur in a system that’s already beat up in ME/CFS but gut problems can occur even in healthy people with fine autonomic nervous systems during exercise.
Fifty percent reductions in gut blood flows during even moderate (submaximal) exercise commonly occur and can reach 80% during maximal exercise. These drops in oxygen levels can damage the tips of the villi that transport nutrients into the blood. If blood flows are reduced significantly enough an ‘ischemic state’ producing high levels of oxidative stress and inflammation could harm the lining of the gut.
Bacterial Toxins

Bacterial toxins leaking into the bloodstream from the gut could produce fatigue, pain, and other symptoms
Either way, a messed up gut lining can allow bad actors such as endotoxins and inadequately digested proteins to gain entry to the bloodstream where they’ll be met by a nice strong immune response; i.e. the inflammation some researchers believe is so damaging in this disorder. Some endotoxin leakage may be common and is usually easily dealt but prolonged, vigorous exercise can produce ‘endotoxemia’ even in healthy people.
Increased levels of bacterial endotoxins called lipopolysaccharides (LPS) can occur after even short bouts of ‘exhaustional exercise’ in healthy people. Increased antibody levels to LPS that were associated with markers of immune activation (ie inflammation) have been found in ME/CFS – during rest.
The fatigue, autonomic nervous system symptoms, flu-like symptoms, sadness, and irritability Maes found associated with those antibody levels suggested the escaped gut bacteria might be having a significant immune impact.
Low Blood Volume
Given the low blood volume endemic in ME/CFS and several studies suggesting low oxygen states may occur in the muscles during exercise, we can probably take for granted that gut oxygen levels are not optimum in ME/CFS even before exercise. The big question – soon to be answered by the CAA’s webinar – is how much even small amounts of vigorous exercise can knock the gut around in people with ME/CFS.
Dr. Shukla compared the entire gut microbiome after exercise in people with ME/CFS compared to controls. A few studies suggest the gut flora in ME/CFS may be dominated by unhealthy bacteria.
Treatment
Diet
One way to counteract the low blood flows to the gut during exercise may be to eat small, probably liquid meals before you ‘exercise’. Eating will increase blood flows to the gut but it may also reduce blood flows to the muscles – probably not a good thing given they may already be in a low oxygen state.
Eating directly after activity could help restore blood flows to the gut more quickly….but if, as has been proposed, an ischemic state is causing problems in the muscles after exercise, doing so may interfere with muscle repair. The best dietary advice might be to take blood volume enhancers (salt loading, NUUN, electrolyte drinks) before and after exercise.
Gut Enhancing Substances
Maes found that gut-enhancing substances such as glutamine, N-acetyl cysteine, and zinc in combination with a leaky gut diet were helpful in ME/CFS. One review article suggested that glutamine, arginine, citrulline, nitrate, and nitrite (green leafy vegetables) supplementation may help. Since NSAIDs can decrease blood flow and cause bleeding in the upper gut they should be avoided.
Probiotics
Probiotics may play a key role in replenishing the gut flora in ME/CFS; figuring how the best way to do that will be important
If the Shukla study finds abnormal gut flora either before or after exercise probiotics and antibiotics are going to get a lot of interest. Logan took some pains to point out in his review article that a lot remains to be learned about probiotic supplementation and health. Studies examining probiotic effects in athletes are becoming fairly common.
Giving trained athletes probiotics appeared to decrease intestinal permeability and had some effect on oxidative stress and cytokine levels in one study. Probiotics strongly reduced oxidative stress levels in another study. Daily administration of probiotics reduced the incidence of infection in one study but not another.
The variable results may reflect the different strains of probiotics used. The field is still early in the game of determining which probiotics work best for different conditions. The CAA’s study should give us a much finer-tuned idea of which bacteria to supplement/experiment but the study was small and may not reflect what’s going on in the community at large.






It’s seems like the basis of the message of day 2 of the FDA meeting was to get to the CAUSE of ME/CFS yet here we go again looking at an effect.
I remember when we were kids and we would as why the sky is blue? We need to get back to the basics and concentrate on the cause of our disease and stop being distracted by all the effects of the disease or no big pharma is going to get involved with our plight.
These are all interesting but if you look at MS, or ALS, or CF, they’re not working on all the side effects of the disease they’re looking for the cause.
Greg
It may depend on who are. I do know of a couple of people who’ve had fantastic results from dietary changes, probiotics and antibiotics and of course people who have not. Getting rid of gut misery, which I think I’m on the road to, will be only be helpful.
We don’t know the cause of MS or ALS or any chronic illness yet, as far as I know. That means that all of the treatments for chronic illnesses are based on symptoms downstream of the root cause, and many of those treatments greatly increase quality of life. So I am happy that researchers are looking at important systems that are broken and could be improved with treatment. Also, understanding what’s not working in the gut and nervous system can help researchers work backward to figure out what the likely culprits are (i.e. specific pathogens and/or toxins.)
That said, we obviously need researchers trying to figure out the root cause but in the meantime we can still get treatments that allow us to live closer to normal lives.
Actually the Cystic Fibrosis Foundation with private/public funding of some 60 million over the last 7 years developed a drug that cures one form of their disease and is hopefully leading to an understanding of future drugs for other forms.
I think this is the kind of thing we need, not say with CF a better drug for treating their GI problems but the actual disease and therefore ALL the problems!
To clarify, we don’t know the root cause of most non-genetic chronic illnesses. It’s a lot easier to find the root cause of diseases with genetic origins because you can actually determine the specific protein that is not working correctly and create a treatment/cure based on that. We have hundreds of genes that are not being expressed appropriately and it’s much harder to find the root cause (assuming there is just one) than it is in a genetic or typical infection disease. So there’s a good chance that treatments for neuroimmune diseases will be based on downstream mechanisms for quite a while, although I hope that we get to the root soon.
Even if I had MS I would rather use Terry Wahls’ treatment (diet and electrical muscle stimulation) than most of the other treatments out there so nutrition and potentially gut bacteria appear to be big players in MS too.
I had been a clinician in primary care for decades (Physician Assistant) until I started to get sick 5 years ago after a severe viral infection (but who knows how much of a contributing factor my lifelong undiagnosed celiac disease may have set me up.) My “gut,” (pun intended,) told me I should avoid antibiotics to prevent healthy microbiome disruption. I got a true bacterial sinusitis and was forced to take a round of broad-spectrum antibiotic for two weeks to clear it up. (This was two years in to my illness. I was still working full time.)
I was completely well for six weeks. This has been such a mystery to me, and in hindsight, to Dr Bateman.
Then, after six weeks of feeling healthy, I got sicker than I had ever been, overnight, with new and rather startling gastrointestinal symptoms. Managed to work another year; but now on disability for 2.
Boggled! This article perhaps sheds a ray of light to explain this.
I agree. Getting to the core reason for the problems will bring possible better results, Instead of using bandaids to mask the problem. I think that the underlying problem with ME/CFS, POTS, MCAS and all the related autonomic nervous system issues – is an underlying autoimmune dysfunction, inflammation and genetics.
My doctor has me on a low-fat, vegan diet. I’ve been on it for 4 months now and am starting to have some outstanding results with it. Not only do I hardly ever have any gut related issues, but most everything related to my illness seems to be getting better.
If you look at what alternative docs do when they find autoimmune illness one of the first things is take you off dairy and gluten and then with MS put you on a low-fat diet. My addressing this with diet and a few meds —seems to be helping more then any of the other things I’ve done throughout the years.
I’m not saying we shouldn’t use meds – as this may be absolutely necessary in some cases. But, maybe something as a temporary support. I do however, believe that probiotics are essential with the diets that most eat today. Probably meds will improve our quality of life —but, “fixing” the problem – will have to go far deeper.
Issie
Congratulations Issie on your improvement. It’s good to keep in mind that these things can take time (and I wonder if I never allowed enough time) and diet does effect the composition of your gut flora. Definitely keep us posted 🙂
I’ve been taking lots of fermented food, lots of vegies , probiotics and engaging in lots of stress reduction. It’s hard to tell what’s doing what…I can tell my gut is better -probably because of the diet and probiotics – I was starting to have big problems – and I’m definitely doing better overall.
Thanks Cort! It’s taken a whole lot of determination to do this – but, I do feel it is paying off. The more research I do, the more I feel I’m on the right path. As you said, it will take time. It has been a long time since I’ve been “well” – so however long it takes – I’m up for the Journey. 🙂 Since I’m seeing improvements, it makes me more determined to hold the course. The main thing is getting your head around it and being determined to follow through. Educating yourself on the reasons for something – is half the battle. Then, making it a “lifestyle” is the most important part. Some tend to have the head knowledge about things, have good intentions to do something, but then never follow through. It’s when we take control of our own situation and make changes – that changes occur. No changes = NO CHANGE. I’ll keep you posted.
Issie
Lifestyle changes are the hardest! (Particularly when you’re under the weather…)
Hey Issie and Cort. I’m guessing you’ve both seen Dr Terry Wahls work on diet (forgive me Cort if you’ve already written about it) It’s been inspirational for me with my family when I already thought we were eating well…. Glad you are both seeing improvements.
I agree with Greg in that I thought the common goal of the conference was for treatment of the disease, not treatments for the many symptomatic problems. I am pretty certain that the cause for me was retroviral infection of many types which caused dysautonomia, and immune upregulation, which could also switch to down regulation. Inflammation of the brain and spinal cord result and can be found in several ways The effect on the gut is another burdensome result of the disease process and has different causes. Each and every bodily system is affected by neurological and immunological dysfunction. We have plenty of labs, biomarkers, and treatments for these symptoms. Research has to identify how people are vulnerable to the virus population, as they are not well known or understood in mainstream medicine. I have a niece that works for Homeland Security, and several years ago found one of these virus underneath the leaf of an imported orange tree. All were burned. So more evaluation and cleaning of food, more efforts on the parts of patients to learn about supplementation and elimination diets. Oxygen shortage is prevalent everywhere in the body, yet can be supplemented, and as the disease process improves, the oxygenation responds. There are other sources for virii, yet kept to this point. To not be able to exercize was so upsetting to me, as I used to swim three times a week at the YMCA. Yet, I kept trying yoga and gentle stretches and short walks with deep breathing. The results of the Ampligen were amazing, and I am hoping to hear how we can continue trying to get it through their approval process. I hopefully think sometimes we are closer to a cure than we even know! . Thanks…
Oops! Have found an editorial comment that I have already said this? Sorry, friends. I am still sick. Plus this is a blog, not a thesis. MCS
I have found that electrolyte drinks make a significant difference, as does measuring heart rate during any physical or mental exertion. Of course we want to focus on a cure, but many of us are sick NOW and will take any relief we can get – after all, each symptom we suffer taxes our body more so that it is less able to heal itself! I must say that I am annoyed that Nuun keeps being listed separate from electrolyte drinks as if it is something different. I found Nuun to be outrageously expensive and not nearly as helpful as other drinks. I found through my own research that actually, “electrolyte drink” is not a regulated term, and any drink or supplement that has any combination of one or more of at least 6 electrolytes in any amounts can call itself that. I am currently testing on myself how much I need of which elements, in what ratios. I find that making my own drink that is as high in sodium as I can manage taste-wise, with very high potassium, high magnesium, some chloride and calcium, and as many phosphates as I can get in there (many of us are severely deficient in phosphate which may be a significant key to our illness), plus a high antioxidant, makes an astounding difference in how I feel throughout the day, and strongly reduces crash time and severity when taken directly before and after exertion.
I am still experimenting to find the right combination, and when I do will test it with others who have the same illness to see if it works better for them than these bought electrolytes (for instance, Gatorade increased blood volume but caused problems due to sensitivity to the dyes), and when I have a good combination I will share it widely. For those interested in trying, though, I am currently mixing 2 tsp Elete electrolyte supplement (found on Amazon), with 1 tbsp dehydrated coconut water (can also find on Amazon), with 2 scoops (10g) magnesium-fortified d-ribose, and 4 oz. pomegranate juice. This works better than anything else I have ever tried, but it is still far more expensive than I intend for the end-product to be. With a lot more testing, I can identify cheaper and more easily available sources of each component that works. But the lack of chemicals and dyes and plastic waste bottles helps me. At 2-3 of these drinks per day, I must say that my bulk purchases of the ingredients are lasting close to 2 months (the dehydrated coconut powder is about 1 pouch a week though – still cheaper than using liquid coconut water), so still doable for now. My experience has been that eliminating any one component made it not work as well, but test for yourself what works, it may not be the same as for me. The point is to get the different electrolytes in a drink with something that has a high antioxidant value (still not sure why, it just works – I have found pomegranate so far to work significantly for me, more than concord grape, for instance) and however you can get them should in theory work fine.
With the drink alone, I have gone from being completely bedridden to being able to leave the house once per week and exercise for 40 min. 3-4 times per week (always with a heart rate monitor, I have to stay below 117 to not cause a crash). It’s not the only thing needed, but it is helping my body fight this much better than most other things I have tried, and I have tried hundreds of things. Also, a note, I’m surprised the article didn’t mention this, but wearing compression stockings also makes a significant difference for those with low blood volume – try 30-40mmhz pressure thigh highs (those at the knee and the waist are more likely to cut off pressure and make the problem worse instead of better), I happen to have had a great experience with Bright Life Direct’s website and customer service [not to push a company, I just liked them], each pair will last you about 6 months and brands like Jobst can be very comfortable – check the reviews before choosing. I also tried Florinef, a Rx to help blood volume, but did not like how it made my face blow up. Some people find licorice tea to work just as well, but be cautious to check your potassium levels occasionally and take extra while using it.
Hope something I posted here will help someone else! We may not have a cure, but we do have methods identified that help our bodies feel much better for large groups of us, that are readily accessible now. So many are desperate for anything that makes one feel better ASAP. Another thing that is making a huge difference for me now is buying a cheap kitchen timer, and setting it for 45 min. all day. At 45 min, I stop what I’m doing, and lay down with my eyes closed for 15 min. Just started this after a break of a year, but wow, what a difference! I hate to slow down, but this actually makes me get far more done in a day than without it.
Thanks for sharing Sunshine! You’ve made great improvement with this change…congratulations.
Congratulations Sunshine! I hope that you keep improving..and thanks for all the information. How much of the drink do you take a day?
Always wondered why my stomach was stone cold ( and when I say cold I mean freezing ) alot of the time even when my body very warm and definately after any exercise just felt like my stomach was shutting down, This new understanding makes good sense to me. Have been suffering with M/E, CFS for around 20 years. Thanks
Did anyone else get scared of exercising after reading this article?
I think it’s important to remember that exercising within their safe limits is still crucial for people with Chronic Fatigue Syndrome. Exercise, if done right, can counteract deconditioning due to inactivity and thus reduce fatigue, pain, and stiffness, and improve mood.
To find out how you can benefit from exercise, have a look at my step-by-step guide on how someone with Chronic Fatigue Syndrome or Fibromyalgia can exercise without worsening their symptoms.
http://cfsrecoveryproject.com/how-to-benefit-from-exercise-even-if-you-have-chronic-fatigue-syndrome/
Warmly,
Johannes
Thank you for this article. It corroborates what I’ve found to be true in my own case. I especially appreciate the videos. Much appreciated!
Thank you for this article. It corroborates what I’ve found to be true in my own case. I especially appreciate the videos.
In the history of medicine finding a treatment that works has often led to greater understanding of the illness and ultimately to better treatment.
Treatments improve – or even save – lives long before the reasons are understood. When doctors first recognised that hand-washing reduced illness it saved lives. It took years before they understood why.
Probiotics have helped me a bit. NAC has helped a lot. That may be it’s effect on biofilms, I’m currently having tests for helicobacter pylori. A gluten-free diet removed a lot of brain fog but oddly after taking NAC a gluten containing diet has less effect (went back on it for a coeliac test).
I’m very interested in this study.
forgot to say – currently trying raw garlic as a treatment and would recommend people consider it. Not easy to get it down but cooking destroys some of the effect.
Perhaps of interest. Have only skimmed it myself.
High-Intensity Exercise, Heat, and Endotoxemia
Published June 3, 2013 | By Ray Medina
http://syontix.com/high-intensity-exercise-heat-and-endotoxemia/
i recall yrs ago in a video Dr. Daniel Peterson stated that no docs or researchers have any interest in this illness because there is no money to be made from us patients
that should be our first red flag