



(Ken Lassesen’s focus on the gut enabled him to recover from chronic fatigue syndrome. Over the next couple of months he’ll be exploring his understanding of the role the gut played for him on Health Rising. Check out his website CFSRemission here. Please welcome Ken Lassesen to Health Rising. )
In 2012, while experiencing significant work stress from a new job at Amazon, I got a flu that sent me to the hospital. The result was the start of my third onset of ME/CFS. Yes, third. You may say — no one recovers, so how can you have recovered three times? You must have something else!
A short description of the symptoms (and tests results of each) may help
Onset #1 1972-73

Ken’s first bout with chronic fatigue syndrome occurred over 40 years. Two more followed several decades later. Ken fully recovered from all his bouts with ME/CFS.
Doing triple honors at University, working full time and family stress resulted in a sudden collapse of cognitive ability, tiredness and a persistent cough after a mild flu. This was before CFS or Lyme existed as a condition. The family MD (in his 60’s then) happened to have also treated my parents and grandparents and recognized some characteristics of my grandfather. The official diagnosis was “Antibiotic resistant walking pneumonia” which resulted in different antibiotics in high dosages for several months.
I also changed diet to lose weight, a high protein – no carbohydrates diet (which was effectively a gluten free diet before it was invented!). He advised me that stress is a real contributor and to minimize it. It took almost 4-5 years before cognitive ability returned fully. IMHO (in hindsight), I was lucky — the treatment was likely ideal.
Onset #2 2000-2001
I was working at Microsoft with a 90 minute commute each way and long days. The work situation had become very high stress (the boss causing it was later “asked” to leave Microsoft). Driving home, I fell asleep driving at a stop light and never went back to work. I was being treated by a Family Practice MD and had just done a regular checkout two weeks earlier that had zero problems. I had cognitive collapse, physical fatigue, body pains, “stress cough”, low blood pressure, low body temperature, gray skin, etc
I had the full range of conventional medical testing done with nothing apparent. The MD was honest and said that she did not know what to do and literally asked me to research options. I found some very recently published works by Cecile Jadin and David Berg as the two most probable treatments given that both were reporting 70-80% remission. There was no clue as to how they could relate to the same condition! Without testing for infections, she agreed to put me on the same dosage of a tetracycline that she would prescribe for Acne. I improved and she became more willing to follow Jadin’s protocol.
I was a bad patient — I did not mention to her until 6 months later that I was badly herxing from the tetracycline (from readings, I knew what it was and knew that she may panic if I reported it to her… at times you need to control information flow to medical professionals.
(A Herxheimer effect or herx refers to a ‘healing crisis’ usually caused by the release of bacterial endotoxins during bacterial die-off. The symptoms, which resemble those of sepsis, where first characterized in syphilis patients undergoing treatment.)
My blood was sent to Hemex labs for testing and I was indeed hyper-coagulated. Genetic testing confirmed that I had a genetic factor common to a population that my father’s family had come from. He had passed away from a stroke.
My treatment consisted of multiple antibiotics rotated monthly (using herx to determine if it was an effective one; a herx suggested it was) plus heparin and a variety of non-prescription anticoagulants. This time my recovery took a year.
Onset #3 2012
Similar situation as Onset #2: High stress company with dysfunctional management (my direct manager left Amazon about the same time I got the flu). Reduced blood pressure and body temperature, cognitive issues and cough were a few of the 40 symptoms I have listed in my notes. When the symptoms first showed up I continuously increased anti-coagulants (which kept me work-functional) until I started to bruise easy.
I stopped the anticoagulants because of the very easy bruising and rapidly collapsed over the next week. MRI results showed no problems (which is typical for CFS), however SPECT result matched those seen from Chronic Lyme and CFS (the radiologist described it as early (under-65) Alzheimer’s Disease). I was having severe memory issues which many readers are likely familiar with. My conventional MD referred me to NDs, she did not want to/felt incapable of dealing with me.
I went to Dr. Kim Iller, who was familiar with Jadin’s work and willing to follow her protocol. She was working Dr. Marty Ross at that time. I tested positive for Chronic Lyme. As with the 2000 onset, I proceeded to read over 3000 pub med articles to make sure that there was not a better (more effective) treatment available. I discovered some serious studies on gut bacteria and CFS and with Dr.Iller’s consent, went on to Mutaflor. A probiotic, Mutaflor caused the worst herx that I ever had in my life… but also rapid decrease of symptoms. It does not just kick-ass, it kicks-head; the worst headaches that I have ever had in my life…. Mutaflor is non-prescription in Canada and thus was easy to obtain crossing the border. Recovery time was just 6 months until I was authorized to return to work.
Was This a Remission?
As described above I’ve actually recovered from chronic fatigue syndrome three times, when most people never recover once. Besides having a classic symptoms presentation, two objective measurements suggested that, once again, I did have CFS:
- My SPECT scan was abnormal in the same way that is commonly reported for CFS and for Chronic Lyme in PubMed articles. Later neuro-psychological testing found that I was in the outstanding range in most areas, but just “normal” for memory. Memory issues continue to improve but are still present.
- My vitamin 1,25D values were extremely high — the lab report actually stated that the measurements was done twice to be sure. This extreme 1,25D is seen with autoimmune diseases and with CFS.
With remission, my 1,25D levels dropped down to the normal range — suggesting that it was indeed a remission!
Each time there was a remission, it became faster, and I understood better the probable mechanisms involved.
Several apparently random observations lead me to focus on the gut
- Fecal transplants produced an immediate remission from CFS that lasted for at least a few months.
- I’d corresponded with a patient that experienced this twice in Australia before this onset.
- Long term antibiotics result in remission for a significant percentage of patients (but don’t work for others)
- Each antibiotics impacts different gut flora, thus the randomness of results made sense.
- At the start of this onset, I recognized, after clearing up other symptoms, that many of my core symptoms were gastrointestinal. These symptoms were “below” the radar on other onsets.
Once I was on sick leave I started reading every article on PubMed dealing with CFS, in particular, when remission was reported for some. Two interesting and seemingly disconnected cases occurred; some people, oddly enough, recovered through the use of 85% chocolate and others from the use of licorice. Obviously, this is not the way out for most people with ME/CFS but something did happen. My question then became what was in common with these observations???? My academic training is in modelling.
The conclusion was simple: all of these items result in changes of the gastrointestinal bacteria. Given that we all have different bacterial mixes I wondered if it was possible that these two people just happened to hit on the food that righted their bacterial flora.
The next step was to see if anyone has reported changes in the gastrointestinal bacteria on a sample of CFS patients. A paper presented in 1998 in Australia and available [here] had. The study deal with only 6 family of bacteria, but the pattern was clear; the bacterial flora in this group of ME/CFS patients was profoundly disturbed.
Gut Flora in ME/CFS from an Australian Study
| Family | Controls | CFS Patients |
|---|---|---|
| E.coli | 92.3% | 49% |
| Klebsiella/Enterobacter | 0% | 3% |
| Enterococcus spp. | < 1% | 24% |
| Bacteroides spp | 92.8% | 91% |
| Bifidobacterium spp, | 7.1% | 2% |
| Lactobacillus spp. | < 1% | 0% |
My conclusion was that if you could change these bacteria back to the ranges seen with controls, CFS may disappear but how to do that?
Diet
I believe that a part of my first remission from CFS was going on a high protein, low/no carbohydrate diet for almost two years. This change was not as a treatment for CFS, but I believe that it helped correct my gut flora dysfunction. In animal studies, we find that it does alter gut bacteria[1] as well as human studies[2]. Even Dr. Mercola is in agreement[3].
I recently read “The Lure of the Stone Age” by Marlene Zuk, an evolutionary biologist, in New Scientist. She is the author of a recent book, Paleofantasy: What Evolution Really Tells Us about Sex, Diet, and How We Live. Sometimes CFS patients will ascribe the cause of their condition to GMO foods, chemical additives, and many other aspects of modern life. In her book Zuk discusses how advances in technology (pre-GMO, pre-chemical revolution) such as breeding techniques developed specialized strains (of plants) or breed (of animals) that may no longer provide the nutrition their predecessors did. The key may not be the nutrition that our human body needs, rather the nutrition that our gut bacteria needs to keep a healthy balance!
For example Holstein cattle were breed to be the world’s best milk producers over the last 1000 years. The goal was volume of milk, not the content of the milk. If the milk had 50% more of certain (potentially unhealthy) fat types than low producing cattle species, no one knew it. The same happens with plants. In recent times, commercial plant species have been breed for characteristics such as shelf-life; again, the impact of slight shifts of composition are unknown. Is it possible some people with ME/CFS simply aren’t suited to some of the dietary changes of modern life (or for that matter the chemicals)?
Take our ability to eat the same fresh fruit and vegetables all year round — instead of just a few months of the year.
Conceptually, the general population believes all of this to be good. But looking at the role of gut flora in health, I find many questions are unanswered. If you have a fresh apple a day, you are supposed to be keeping the doctor away! But some families of bacteria will find themselves very happy from the sugar and malic acid in apples,while others will not be happy; by eating an apple a day you may have actually upset the microbiome apple cart!
Studies have shown that the modern, high fat, high carbohydrate diet is hard on the gut flora. Even after raw food has made its way through the acid bath of the stomach it still retains about 35% of it’s lactobacillus bacteria. What we eat makes a difference but now instead of seasonal variations in gut flora (due to changes of diet), we end up with a single monotonic gut flora for the entire year. If this gut flora goes bad (as I believe is the case for CFS, IBS, Crohn’s and many other autoimmune conditions) then the historical mechanism that constrained this, goes away; ie we’re stuck with the bad flora.
A Change of Flora
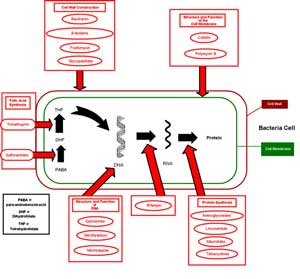
So what is the bottom line? If a stable dysfunction of gut bacteria (microbiome) is the root cause of CFS (my working hypothesis), then fixing it is the way to remission. At present, I know of several ways:
- Severe change of diet (likely the slowest)
- The use of the right antibiotics (likely several families on antibiotics needed)
- The use of the right probiotics (Mutaflor and Prescript Assist appears to be the best, any probiotic containing Lactobacillus Acidophilus is NOT the right probiotic IMHO)
- The use of the right herbs (the herbs are natural antibiotics to certain species), the best ones appears to be Neem, Haritaki and Tulsi.
We’ll be getting into more on antibiotics, herbs/spices, diet and probiotics in future blogs. For now, the take away story is that the situation is more complex than one would think.
(The term right is very important for probiotics, for example, CFS patients are low in all E.Coli species. Lactobacillus Acidophilus is usually deemed good, especially when dealing with bad E.Coli — unfortunately it does not know the difference between good and bad E.Coli.. On the other hand, Mutaflor is a probiotic composed of E.Coli Nissle 1917; this is the right probiotic (IMHO).)
(The information on Health Rising is produced by laymen and should not be construed as medical advice. Please consult with your doctor before making any changes to your treatment plan)
Support Health Rising







Millions have high stress jobs, lousy diets, use tobacco and alcohol and do not get CFS! Yes, there is most likely a genetic component about the gut/immune system. If the gut is infected, or overloaded with pathogens, in many, it will harm the immune system, therein. If you look at the symptoms of Enterovirus, they match ME/CFS! Diet and probiotics over time will reduce the burden on the gut/immune system and recover to a degree but I believe if the tough primary pathogen is eliminated, recovery will be much faster. RP
Symptoms of CFS vary greatly and match many viral and non-viral infections. 10 years ago I was a believer in the single-pathogen cause. Today, my thinking is different…. many infections can cause the gut alteration…. and that infection may be eliminated/defated but the gut alteration remains…
Thus you may have PCR testing for every proposed pathogen and be negative for all of them. On the flip side, the gut alteration will frequently “farm” passing infections that helps it survive. By farm, I mean producing chemicals that the infection will thrive on – because the infection will produce chemicals that the microbiome will thrive on. Mutual support.
There is no way to “prove” either way. There are several studies of different acute infections that resulted in a 4-8% of those infected not recovering after the infection is defeated. Post-Infection Fatigue Syndrome is sometimes applied to this condition.
I tried multiflor: several bottles and no difference 🙁
What is the anti-coagulant you use and where do you acquire it?
I will give a list of them in a future post, as well as explanation of what the issues in selecting them are.
The one’s that I use (because I have a Prothrombin 20210 A/G defect) are turmeric (the kitchen spice) 2-4 gms/day, piracetam (2-4 gm), nattokinenase, lumbrokinease — to break down fibrin.
80-90% of CFS patients have inherited/genetic coagulation defects. Which defect determines what type of treatment is needed….
“80-90% of CFS patients have inherited/genetic coagulation defects. Which defect determines what type of treatment is needed….”
That strikes me as a very significant statement, if true, given that many PWME have high readings such a mean corpuscular volume and very low to non-existent SED rates.
Do you have a source for this?
Yes, the articles of David Berg/hemex labs plus several conversations with him.
Some of the conversations are at http://cfsremission.wordpress.com/?s=berg
The articles
http://www.ahmf.org/99access/99berg.html
Berg D, Berg LH, Couvaras J, Harrison H. Chronic fatigue syndrome and/or fibromyalgia as a variation of antiphospholipid antibody syndrome: an explanatory model and approach to laboratory diagnosis. Blood Coagul Fibrinolysis. 1999 Oct;10(7):435-8.
http://www.ncbi.nlm.nih.gov/pubmed/10695770
Harrison H, et al. Procoagulant genetic factor in a pooled cohort of 582 chronic fatigue syndrome, fibromyalgia and related chornic illnesses, AACFS, Oct 2004
Hannan KL, Berg E, et al. Activation of the coagulation system in Gulf War Illness: a potential pathophysiologic link with chronic fatigue syndrome: a laboratory approach to diagnosis. Blood Coag Fibrinolysis 2000, 11:7
I am planning to a post shortly on coagulation since I talked extensively with Berg (who is now retired), had positive results, and spent a lot of time understanding the complexities.
Thanks
I was aware of hypercoagulation in GWI but hadn’t seen anything in print for ME/CFS.
I’ll check out the links.
I did a fecal transplant from a fully healthy and screened donor. It didnt result in a recovery, only made me worse. In fact, i am considering going on 3 days on vancomycin to destroy whatever it did to me and try and reverse the procedure.
Thomas, the literature states that best results are obtained from blood relatives, the closer the better. DNA and gut bacteria are closely connected. A non-blood related donor may create the same situation that “non-matched organ transplants” have — rejection, open warfare between two populations of microbiome.
I know someone that would love to try a fecal transplant — but the closest “healthy” family member is just 1/16th of the same DNA. Everyone closer have autoimmune or digestive issues.
Hi Ken, thanks for the reply. I wish I knew that before, or that my doctor told me that before suggesting I do one. Do you think a short course of vancomycin might be able to reverse the effects and bet things back to the way they were before the FT??
Would love to know what you think i might be able to do about it…
Not medical advice, but assuming you are living in the US, not close to the Canadian Border, I would suggest a bottle of Prescript Assist as a starting point. See
http://cfsremission.wordpress.com/2013/01/07/508/
for a list of the species in it.
Start with 1/day and work up the dosage.
Expect radical changes of stools and some possible discomfort.
IMHO, it is more likely to be successful then a course of any single antibiotic, and likely healthier (adding good microbiome instead of flattening all microbiome: reminds me of the story Jesus told of tossing out a demon from a house, and then seven worst demons came to occupy it…. ).
Pulse … i.e. no more than 10-14 days on and then take a 2-4 week break.
Thanks Ken. I live in Canada but apparently there are some websites that will ship it within Canada. I will give it a shot as per your pulsing recommendation. I still might do the 3 day course of vancomycin first then start on the prescript assist probiotic. I had IBS long before i ever had MECFS so hopefully this will help!
Also, perhaps another FT (from my very healthy brother) would be a good choice to reverse the bad one if all else fails. What do you think?
Again, i appreciate the responses. Thank you, kindly.
Thomas, our experience is that often doing two things at the same time do not result in each re-enforcing each other, rather, they partially neutralized each other.
My thinking is that it better to dislodge the bad microbiome by good microbiome (“pro-biotics”) then to kill all of the microbiome. Thus, if I was in this situation I would talk with my health professional about:
1) Two weeks of Prescript Assist (increasing dosage slowly)
2) 1 week break
3) Two weeks of Mutaflor (increasing dosage slowly)
4) 1 week break
Then re-evaluate — if significant improvement, repeat, otherwise….
Base on degree of my own response, I would consider a course of Haritaki and Neem (Indian spices) after that (slowly increase dosage to a max of 5 gm/day) before going to conventional antibiotics (I have done lots of antibiotics — so it is not a bias against them, just the degree of response that I have seen from each).
Got it. I will go by your advice and do that course of action first. What is interesting is that my Genova CDSA looked better after the FT than before as far as healthy bacteria goes, So at least on paper it worked, but i didnt feel any better. Perhaps my decline was completely unrelated. I always had high e coli but i will get some mutaflor anyways. I am more excited by the prescript-assist though and what it can do. Thank you.
Mutaflor currently not available in the US pending some FDA reclassification.
Correct. FDA deems it to be a drug. Even with a US prescription for it, you could not get it. Mutaflor is very temperature sensitive. In Canada they send it express packed in a large foam chest loaded with ice packs. It is always sent directly from the Canadian distributor directly to the shipping address.
On the other hand, Prescript Assist is not temperature sensitive and available in the US — it’s the next best choice for US residents.
Just what I was going to ask. What are the alternatives in the US. How close is Prescript Assist to Mutaflor. I guess we’ll get into his later but what makes up a really good probiotic?
Prescript Assist and Mutaflor have ZERO bacteria families in common. A good probiotics is one that has been repeatedly found to be very effective for IBS in published studies found on PubMed (Prescript Assist has) or other IBD/IDS (Mutaflor has).
With CFS — there is a gotcha, there should be no species known to reduce E.Coli (since we are known to be low in that). In general, (apart from L.Reuteri), I avoid probiotics containing Lactobacillus of any species.
I am constantly looking for additional “unusual” probiotics (may require import from outside of the US — there are some interesting ones in Japan and Korea) that matches that criteria.
I’m curious how you obtained the Mutaflor if you’re a U.S. resident? Do you have cousins or family in Canada?
And what if a stool test has shown good levels of e. coli (metametrix)? Will the Mutalfor make things worse?
Thank you.
My gut was fine until I tried probiotics (have tried them two different times, using different kinds)……going on them was hell & it wasn’t herxing, bc I stayed on them long enough for that to have stopped…..and ever since being on them, my gut has become progressively worse (bad gut reactions are not the only thing that was bad abt being on them, by any means, but they are the only bad reactions that never got better after stopping them)..
…..at this pt there are absolutely ZERO foods that I can eat w/o either throwing up, having diarrhea, and/or having the food just sit in my GI tract & not move and my stomach blow up like I am 6 months pregnant (& my weight also goes up a lot almost immediately when this happens, even if I have only eaten a very small amt of food….I went up 4 clothing sizes in 6 days while throwing up every day & not eating that much food)
I am now starving during the day & then eating the foods that have the least bad reactions when I know that I am not goign to be going anywhere or around anyone (not that I go anywhere much, but if I know I have to, I won’t eat so that I can avoid getting a bad reactions while I am out)
You will note that I state the any probiotics containing Lactobacillus as being the wrong choice for CFS. This has been expressed by a few MD’s at CFS conference is mild terms of “yet to see any benefit”. If you purchase the probiotics in a health food store it is extremely likely they are mainly Lactobacillus.
It sound like you have have UC or Crohn’s Disease or some form of IBD. If it is Crohn’s then studies have > 95% of the invasive species are E.Coli — often antibiotic resistant. Mutaflor has been found effective in Europe for Crohn’s — because it is more robust and out competes most of the bad E.Coli.
I have seen an alternative protocol for Crohn’s have outstanding result over several weeks by rotating thru herbs that have been demonstrated in clinical studies to be effective against some species of E.Coli. These studies were done in India and China and are included on Pub Med.
It was rotating weekly between items such as the following
• Rheum officinale
• Chitosan
• Zingiber officinale
• Punica granatum
• Terminalia chebula
• Withania somnifera
• Epilobium angustifolium
• Salvia Plebeia
• Rosmarinus officinalis
• Scutellaria baicalensis
• Trianthema decandra
• Quercus infectoria
There was one Chinese study that reported that herbs for E.Coli often developed resistance if used too long… hence the need to continuously change the herbs(or antibiotics) being used…
I;m glad there are alternatives because I think I had a bad reactions to probiotics as well. I won’t be able to tell until I try them again…but I had issues with dizziness. I don’t know how probiotics could cause that but I hadn’t started anything else. I always thought of probiotics as being rather mild but judging from some peoples reactions they’re not – which actually speaks to how powerful they can be.
Probiotics are bacteria. Bacteria can produce signaling chemicals that have been documented to alter the mind, re-activate prior virus, and recently have been found to manufacture their own virus. When you introduce foreign bacteria (i.e. probiotic) into your system — you will usually find them greeted as friends, enemies or don’t care.
What the reaction is depends on your current, unique set of microbiome.
Ken,
Thanks for your reply. I did find some w/o Lactobacillus. Those were the ones I tried the second time around & still had really bad reactions. Also, I oddly have no E Coli in my body at all according to stool sample testing, so that’s not it. (Hopefully someone else reading this will be able to use some of your suggestions, though. I do appreciate you taking the time to list them.) Actually, my GI tract is strangely devoid of bad bacteria as well as of many of the good bacteria.
So far, related to the GI system, I have been diagnosed with: eosinophilic esophagitis, gastroparesis, vagus nerve issues, many food and chemical allergies and sensitivities, low digestive enzymes (which I am now taking on and off – can’t take them for too long w/o getting really bad diarrhea), and the Dr was still looking for more answers when he decided to stop being a Dr so I am looking for a new Dr. However, like I said, I had none of these issues until I started trying probiotics, so I still think there has to be some connection and/or something that is getting missed.
I am probably just forgetting thanks to brain fog, but what is UC?
Hi Tammie,
I think you may have solved your own issue – inadvertently
You are without ALL E. Coli – good and bad.
That means you don’t have any of the good E. Coli. Not all E. Coli are bad – in fact, according to Ken’s article, the composition and proportion of species is important – to replicate the controls or normal gut bacteria.
Take a look at the table above – it is key. According to the table a normal gut has 93.2% E. Coli – and people with CFS have 49%. In your case 0%. That means something.
Thus, Ken suggests taking Mutaflor – which is a probiotic supplement that is GOOD E. Coli. This may help your gut become normal again.
Also Prescript Assist – is also recommend to help transform the gut into a healthy population of microbes.
I have similar symptoms as you do and have been studying Ken’s article very carefully and am intrigued (THANKS KEN!)
So if you do choose to try these two probiotics – start very slow and low, low dose – like a sprinkle, for a few days and then inch up.
Take Care,
Elisabeth
Thanks for your comments on this……interesting & definitely worth looking further into.
I have similar gut problems. Many are linked to adrenal insufficiency. Are your cortisol levels normal?
In remission, yes — Since the literature (and years of user support group messages) had no progress towards remission looking at the adrenal path, it was skipped for testing. To me, it is a symptom of the gut function with the right approach being to address the cause. Once the cause is addressed, the symptoms will reverse themselves, some quickly, some slowly.
Chem Immunol Allergy. 2012;98:163-75. doi: 10.1159/000336510. Epub 2012 Jun 26.
Role of microbiome in regulating the HPA axis and its relevance to allergy.
Sudo N. http://www.ncbi.nlm.nih.gov/pubmed/22767063
What about heavy metals — they can mess up many organs, mess up the immune system, including the adrenals, can’t they? What would you suggest for someone with a heavy metal issue?
Thank you.
Hi Tammie,
After studying the fascinating article written by Ken Lassesen – I spotted something I think may be important for you (and me). In order for the gut to be healthy (like the controls above) we need to have the same or similar microbes in similar proportions…
Good E. Coli (not bad E. Coli) according to Ken’s table above, is 92.3% of the gut bacteria composition. Hence, he suggests supplementing with Mutaflor (good E-Coli) or Prescript Assist.
Soooooo you may have solved your own issue – you are without ANY E. Coli – so I’d start super slow with the Mutaflor and maybe the Prescript Assist too – very very slow – just sprinkle to start.
Ken – if I’m incorrect here – please jump in…just trying to help and solve my own issues, which like Tammie, include many of the same troubling symptoms.
Take Care,
Elisabeth
just looked into trying Mutaflor & it isn’t available in the US : (
The FDA deems it to be a drug and thus require of any distributor a rather large investment in testing etc. In Canada (where I get mine) and Europe, it is over the counter/internet without prescription.
It is perfectly legal to go to Canada and bring it into the US for your own personal use. Just buy some groceries too and declare to customs “groceries and probiotics” and you will be waved through with no questions. It is not legal to sell it or distribute it in the US.
For those not close to our Northern neighbor, Prescript Assist is the best choice (and usually it is over the internet because it is not stocked by most health food shops).
Hello Ken,
Thank you for an amazing account of your journey to recovery. You sharing this information is so very helpful! I do have a question about the blood coagulation problem. What led you to discovering that this was a problem for you? What were your symptoms? How did you get the proper help? Thanks for sharing. All the best!
Julie Mandli
The testing was NOT due to symptoms but due to Berg articles — at that time I was covered by Microsoft’s (old) Medical Plan with 100% coverage of **everything**. My MD was in a little state of shock that anything could be ordered and there was no insurance hassle!
You can read more detail (month by month of my 2000-2001 recovery in this PDF of my original web site available at: http://lassesen.com/cfids/idefx.pdf I gave month by month reports and lab results. My blood was so thick that it was not unusual for nurses to have to try 4 different spots to get a blood draw done.
On the third go round, the typical symptom was mental fog due, at least in part, to blood that was thick. Because of the anticoagulants that I was taking, there was no problem with blood draws — and my blood still presented in the “normal range”. I say in part, because I am starting to suspect that the microbiome changes result in increased amyloid plaques and neurofibrillary tangles — which reverses slowly with remission.
I was told to take the probiotics with a heavy hard coating called “”Pearl” coating because the stomach juices destroy the probiotic, & this one allows the probiotic to get into the gut/intestine where it is supposed to work. This helped me.
Pearl is actually Primadophilus Reuteri Pearls, that is Lactobacillus Reuteri — which is one of the very few Lactobacillus species I view as good for CFS.
Why? Simple — this is one of two bacteria that processes B-12 in the human gut. Since B-12 is low and total of all Lactobacillus species is low, it is logical to infer that low (or no) level of L.Reuteri is probably a significant contributory cause to low-B12 in CFS.
Rather than take B-12 supplements, taking Pearls and Prescript Assist (which has the other bacteria) maybe a better way of addressing the B-12 deficiency…
I was under tremendous, life changing stress the year prior to having CFS. I caught CMV & a human Parvovirus..Tested active by infectious disease specialist. That was 18 yrs ago. I also developed Fibromyalgia 2 yrs are CFS. I’ve had IBS my entire life. My daughter has been hospitalized many times starting at age 11 for “severe IBS” and colonic inertia.
In 2008 my HHV-6 reactivated while doing very stressful volunteer work as a Court Appointed Special Advocate (CASA). I developed Meningitis & Encephalitis. I was hospitalized for 10 days, having antiviral infusions 3x a day. No lesions were found after recovery. Neurologist told me entero virus , HHV-6, broke through blood-brain barrier due to immune suppression …from stress.
My CFS & Fibro have been worse ever since.
I firmly believe my gut is a culprit in my worsening health. I’ve lost 50 lbs in the last year, without changing my diet or calorie intake. I’ve even been more inactive, homebound, in the last year. My whole body has been scanned, bloodwork all normal. I’m due for a stomach biopsy which I had to postpone due to perpetual headaches in the last 2 months.
I’ve improved my diet recently and started taking probiotics. Im feeling a little better, but far from well. Still severe fatigue, malaise, pain etc.
I’m anxious to find out if a virus or bacteria is causing my weight loss.
I’m very pleased to have found this article. Thank you for sharing!
Hi Ken,
What’s your opinion on the relative usefulness of getting coagulation panels and stool bacterial tests done, versus just trying out the Prescript Assist and/or bromelain and seeing whether there’s improvement?
The reason I ask is everyone seems to get ME/CFS through a slightly different route. For me, it was probably a combination of enterovirus + mold exposure + chemical exposure + chronic sinus infections. Given limited time, energy, and money, it’s tricky to know which approach to begin with.
Thanks again for sharing your experiences! It seems like the mindshare in the ME/CFS community has been shifting more towards methylation protocols and antivirals/immunomodulators, but it’s good for us to be reminded every now and again that especially with the multisystem dysfunction seen with ME/CFS, there are many different strategies that might bring about improvement. Stringing enough of those improvements together could push the body back into its former equilibrium.
I’ve a friend in the States who’s mostly recovered from a severe case of M.E. She accomplished this with a stem cell transplant followed by daily dosing with Mutaflor. She says the Mutaflor is what keeps her healthy, that if she goes off it she regresses.
If you do a little research, you will that Dr. Sarah Myhill in Wales, UK (http://www.drmyhill.co.uk/wiki/Growing_Mutaflor) and Dr. Kenny de Meirleir, brussels use Mutaflor with their patients.
I just looked up Mutaflor & it says that it is no longer available in the US. How is your friend getting it?
Hi Ken,
What’s your opinion on a typical ME/CFS sufferer getting the blood and stool culture tests done? Worthwhile, or better to simply start with Prescript Assist / bromelain supplementation and look for improvements?
Thanks for sharing your experiences! It seems like a lot of mindshare in the ME/CFS community has shifted towards methylation supplements, which help some, but not all.
I think for a multifactorial disorder like ME/CFS, there are many routes that can lead to improvements, and if you can string enough of them together it may lead to remission. Thanks for reminding us of alternative treatments that may help.
Blood tests for pathogens and for inherited coagulation conditions are thumbs up with me. The down side is the cost.. Typically they are by PCR or DNA and can run > $2000 which many insurance companies will not cover. The second downside is if you get positive results, it may not result in any MD taking active treatment for it. It may not be because they are not willing, but because there is nothing in their standard treatment book to deal with the results.
Treating non-acute (i.e. obvious stroke, infertility, etc) coagulation issues is not “standard of practice” in many medical systems.
As for stool testing, in general the commercial ones do not provide the fineness of detail to be useful. They may tell you that you are high or low in E.Coli, but they do not list off the amount of each E.Coli species (i.e. the goodies and the baddies). I have seen ideal results in some research papers — and those were done by PCR/DNA and identified several hundred species.
We are, IMHO, in a more “Art of Medicine” instead of “Science of Medicine” for CFS. This leads to trials and recording the precise results and trying to build up a picture of what you are dealing with.
Concerning the methylation “fad”, microbiome and methylation with produce 15+ results on pubmed.
http://www.ncbi.nlm.nih.gov/pubmed/?term=microbiome+methylation, 32 for http://www.ncbi.nlm.nih.gov/pubmed/?term=gut+bacteria+methylation
I thought some of you (and Ken) might be interested in this.
I was part of the citizen science startup uBiome on Indigogo. The project was successfully funded. Their goal was $100,000 but the raised $350,000. uBiome will offer sequencing of the Human microbiome. The kits they offer are already in production and I am eagerly awaiting mine. Because we raised so much more money than expected I could choose 2 other kits. I selected the gut, mouth and nose.
I’m mainly interested in the gut kit sequencing. For those who are wondering what it is, with gut sequencing they can tell you what lives in your gut. I will post the link to the Indigogo page, it answers a lot of questions and the uBiome site itself where you can order kits if wanted to do so.
They ship to 196 countries. I have no financial interest whatsoever in this, I’m just an enthusiastic start-up backer. 🙂 I backer over 100 start-up on Kickstarter and Indigogo.
uBiome is located in San Francisco.
Project: http://www.indiegogo.com/projects/ubiome-sequencing-your-microbiome/x/1574653?c=home
uBiome; http://ubiome.com/
—
Christine
Similar to this, I noticed this article:
http://www.nytimes.com/2013/05/19/magazine/say-hello-to-the-100-trillion-bacteria-that-make-up-your-microbiome.html
It refers to this site:
http://humanfoodproject.com/americangut/
From what I can tell, this particular project is affiliated with the University of Colorado is allowing anyone to “donate” $99 (or more) to participate. In exchange for your donation you get a data detailing your GI microbiome. Perhaps the most interesting “tier” they offer is the $2500 one, in which the characterize not only bacteria, but parasites and viruses that live in your GI system. They appear to offer various more advanced techniques depending on the tier.
Hi Ken-
Thanks for the fascinating write up. I’m looking forward to more. I am unable to swallow any pills so I have to either crush them or use liquid form.
I tried Mutaflor about 3 years ago but had a bad reaction after a couple days. I’m wondering if its because I had to open the capsule, put it in water, and then drink it (ewww).
Do you happen to know of a good probiotic that isn’t in pill form?
So far I’ve been unsuccessful at finding one. I’m on long term antibiotics (Minocyline and pulse Zith two days a week) for c. pneumonia (I had this as a child but it was never treated properly).
Thank you again!
Terri
Because of your pill issue, and assuming that you can stomach blue cheese (Trade Joe’s Crumbs are a fantastic bargin!), then just open the capsule of Prescript Assist or Mutaflor and mix it with the cheese crumbs.
First, blue cheese taste will do a good job masking it, but also, some people find that the Penicillin Roquefort in blue cheese improves their gut. 1/2 oz twice a day of blue cheese is worth trying….
Mutaflor package inserts does warn of headaches, etc. and unlike antibiotics where you get hit by them on day 1 — they slowly build for up to a week… and then take a week to quiet down after stopping . Try starting with just 1/4 capsule per day for your first course and see how you do.
My motto is only take as much discomfort as you are comfortable with (not as much as you are willing to tolerate), go slow, go consistent and make sure you understand what you are trying to do so you can tune for your own needs.
I have been making my own fermented vegetables after reading Natasha Campbell McBride. I am on my tenth quart at about 1/4 cup a day. I used cabbage, kale, parsley and carrot. I ordered the culture online and make 6 quarts at a time. Has anyone tried that? I am reading “Nourishing Traditions by Sally Fallon and Mary G Enig a lot of good recipes for fermenting in there. Dr. Weston A Price is a fan of that as well.
Anyone else?
Hi, thanks for the article! I haven’t been able to read all the comments, so please forgive me if this has already been mentioned and discussed. I just wanted to add that research and understanding of the human microbiome seems to really be in an early phase and not much is known – new discoveries appear all the time and turn things around. I think it’s, sadly, too early to say anything about which person needs what probiotic, and which bacterial flora is normal and which is not. We don’t know enough yet! What is abnormal in one person can be normal in another.
Just recently researchers discovered that there may be three main types of gut flora, each with their own dominant strain (Bacteroides, Prevotella, Ruminococcus), see
http://www.nature.com/nature/journal/v473/n7346/abs/nature09944.html
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285216/
I think it’s a little problematic that some (often critizied) doctors, at this stage, claim to know enough about how “normal gut flora” should look. For example, a controversial European ME doctor has told patients that their prevalence of Prevotella is an infection that needs treatment. But in fact maybe they are just a part of the group with the Prevotella enterotype, according to the new research.
We just don’t know enough, so it’s tricky! Probably we have different normal floras and different treatment needs.
“Probably we have different normal floras and different treatment needs.” is actually what I will be examining in the next posts. You have hit the issue on the head.
There are around 1500 known healthy gut flora strains and each of us have between 100 and 150 of these. The number decreases with age. The key is to disrupt the dysfunctional microbiome so an alternative (ideally original) better microbiome replaces it.
Last night I was actually looking at Surströmming, a specialized fermented food available in Sweden which is a rich source of the Haloanaerobium bacteria in it. It meets one of my key criteria: a food with bacteria that is known to be human safe from centuries of use. Another one is Natto, which is a Japanese dessert food. The supplement nattokinease is derived from Bacillus subtilis in it. Since we lack detailed knowledge of the strains, I have often pick up 8-12 packages from different manufacturers at our specialized Asian grocery. My belief is that it is in our best interests to intake as many different strains of different species as possible.
Both Surströmming and Natto are acquired tastes. This is likely true of many non-standard fermented food to dislodge the dysfunctional bacteria. For some people, it will take discipline to intake such on a regular basis.
“Both Surströmming and Natto are acquired tastes.”
IMHO Surströmming makes Natto taste like the finest chocolate. 🙂
Just like cough syrup — it tastes horrible, it is likely good for you! 🙂
Hi Ken, thanks for fantastic blog! I was led to your blog by a friend who is doing his own FMT for various infections with great success.
I have a number of tick borne infections and have been in treatment with antibiotics and herbs for years. The longer I am in treatment the worse I get (cognitive and psych symptoms being the worst, with tremor type activity and muscle pain soon after). The antibiotics used for these infections don’t seem to kill, but are bacteriostatic. I note improvement on a treatment only to slide back within a few days. Why am I still on them? Because off them I am much worse. So in in a no win situation. Bartonella, a gran negative intracellular infection living in the RBC and endothelium, is the likely culprit (but who knows anymore). I have repeatedly tested positive for it after long courses of treatment.
Recently my smart friend focused my attention in my gut. I have not paid much attention to it because other than chronic constipation I’ve not had much trouble … Candida and c. Diff have not shown up. None if my doctors have looked at the gut as a reason why I am not responding to treatment even though reading about it now I am incredulous as to why not. I take VSL3 and s. boulardi, and pretty much don’t think about it.
I wonder if you have any thoughts in why I can’t seem to respond to treatment or clear these infections? I can drink bottles of herbs that put others on the floor, take abx with no reaction, can’t get drunk (I tried as an experiment) and have in digested food in my stool.
I know your dx was CfS (i saw Lyme too) but All these dx seem pathogen related). Any thoughts are appreciated. I know the gut and brain are connected and perhaps inflammation is what is causing the symptoms. I take boluoke and nattokinase (don’t know if they help) and methyl B vitamins for MTHFR defect (haven’t seen much from this either ).
Thank you so much!
Thank you, again, I will be answering using the MODEL that I am working with. Antibiotics and herbs changes gut bacteria — and the hope is that you happen to get the ones that do more good than harm. This means that you (or your care giver) may be faced with the problem of finding something that increases A,B,C without decreasing D,E,F,G,H. Often in my own searches I spent 10-20 hrs on one herb on PubMed by searching for the herb (or antibiotic) and each one of the families of bacteria that I was interested in. I had a “clean slate”, with CFS being less then a few years so assuming the match to Australia reports was reasonable and appeared to work. My wife had IBS for many years, then mild CFS and then remission from CFS (which has persisted) but then Crohn’s showed up complete with fistula 🙁 .
By the Model, this is possible and simply means that while most of the bad bacteria was eliminated, a residue cartel of bad bacteria survived and pushed her symptoms to Crohn’s. She is making excellent progress with items like FireWeed (a bottle a week on occasion), Mutaflor, and other herbs that are effective against E.Coli the dominant family in the Cartel according to PubMed.
My suggestion would be to join the AmericanGut.org project to get a state of the Art DNA sample of gut bacteria, as well as doing what is available as commercial tests — ideally after two weeks of “washing out” i.e. no antibiotics, herbs or most supplements. That may give you enough information to know which ocean of bacteria you are in… and then proceed from there.
Hi Ken, thanks for fantastic blog! I was led to your blog by a friend who is doing his own FMT for various infections with great success.
I have a number of tick borne infections and have been in treatment with antibiotics and herbs for years. The longer I am in treatment the worse I get (cognitive and psych symptoms being the worst, with tremor type activity and muscle pain soon after). The antibiotics used for these infections don’t seem to kill, but are bacteriostatic. I note improvement on a treatment only to slide back within a few days. Why am I still on them? Because off them I am much worse. So in in a no win situation. Bartonella, a gran negative intracellular infection living in the RBC and endothelium, is the likely culprit (but who knows anymore). I have repeatedly tested positive for it after long courses of treatment.
Recently my smart friend focused my attention in my gut. I have not paid much attention to it because other than chronic constipation I’ve not had much trouble.
I wonder if you have any thoughts in why I can’t seem to respond to treatment or clear these infections? I can drink bottles of herbs that put others on the floor, take abx with no reaction, can’t get drunk (I tried as an experiment) and have in digested food in my stool.
I know your dx was CfS (i saw Lyme too) but All these dx seem pathogen related). Any thoughts are appreciated. I know the gut and brain are connected and perhaps inflammation is what is causing the symptoms. I take boluoke and nattokinase (don’t know if they help) and methyl B vitamins for MTHFR defect (haven’t seen much from this either ).
Thank you so much!
Wow! Thanks so much for writing this, I am 35 and was first diagnosed with CFS at 22, I was treated by Cecile Jadin and changed my diet and life style and experienced a big improvement, but was still not 100%. I fell pregnant with my son in 2008, and felt the best I had felt since childhood, but this quickly changed after birth, and I was diagnosed with pan-hypopituitirism. The main hormone being effected was growth hormone, which I then injected daily, I also have very low cortisol, and have not had a menstrual cycle in 5 yrs since giving birth. I emailed Dr. Jadin, asking if there was a link with the pituitary and her work, which she failed to answer. I have been trying the natural route and have recently become fascinated by probiotics. I would love to hear from you, and if you think there is a link with the gut and pituitary? I don’t really want to do all the anti biotics again, do you think it is possible to heal with just the pro biotics and natural anti biotics you mentioned? Are there any other articles you suggest I read? So excited to read your article!
The frank answer is yes it is possible. My hope is that it is possible for most. For more information, I would suggest hoping over to my own blog, starting at http://cfsremission.wordpress.com/2014/01/28/for-new-readers/ It is more technical (i.e. a lot of pubmed links to articles). On Cort’s blog, we work on keeping it readable for the CFS mind.
There are a few pubmed articles looking at pituitary and probiotics http://www.ncbi.nlm.nih.gov/pubmed/?term=pituitary+probiotics I have not had time to dig into that dimension.
Thanks so much for the prompt reply, I will take a look at those links. I saw you also mentioned to the previous lady about the Americangut.org, is this worth me looking into too? Thanks again
Sorry, one more question! Do you think it’s possible to recover using only the herbs and probiotics without the antibiotics? Could taking the wrong probiotic strain cause problems? Many thanks
Wrong strains can make things worst. My standard example is this: CFSer are low or very low on E.Coli population. Lactobacillus acidophilus kills E.Coli.
You should avoid (as much as is practical) foods containing this species, and especially probiotics containing it.
You want the species that CFSer are reported to be low in OR which has been demonstrated by PubMed papers to be effective for IBS (which is very co-morbid with CFS).
Wow, I just started taking the Mutaflor and am experiencing terrible herx, it says to take 1 a day for 4 days and then move to 2 a day, I am on day 5 and feel like death, can I stay on 1 a day, should I decrease or increase?
My suggestion to discuss with your knowledgable medical practitioner is:
Keep at one until the herx eases or you hit two weeks. Then rotate to Prescript Assist and/or pure bifidobacterium probiotics (Align or any other that consists only of bifidobacterium). Return to it again after 1-2 cycles of other IBS effective probiotics.
As a FYI, when I do a periodic maintenance cycle of Mutaflor — there is now zero herx.
If you look at the lab results for CFS patients that I aggregated at:
http://cfsremission.wordpress.com/2014/03/16/gut-bacteria-testing-part-2-what-cfser-have-gotten-back-from-the-labs/
You will see that very low or non-existence E.Coli is very consistent for CFS patients
Thanks so much Ken!
Thanks for sharing valuable info. I’ve had fibro for approximately 15 years. Have been trying extremely hard to bolster my health before upcoming surgery. I read that 70-80% of immune system is in the gut. I suspected leaky gut, but was not tested for. I did test positive for candida, EBV and Parvovirus.
Began Famvir for viruses, although fibro dr. wants me to take Valcyte. Do you know if these alter the gut environment? What are your thoughts on these antivirals?
Taking vitamin A, zinc, licorice, and Collixen to help heal gut. I began taking Lactobacillus GG (Culterelle) as I read it helps heal leaky gut.
I then began Bio-Kult. I recently began Probiota, because it has strains that are low-histamine causing, because I’ve had issues with hay-fever, and allergies.
I was going to order Prescript-Assist, but then read online a few places that if a person has leaky gut, then these SBO’s can migrate into the blood where it doesn’t belong. It scared me, so I cancelled the order. Can you give me your thoughts on this?
Right now is the year of 2019, I am looking forward to hearing any update from your guys.Thanks!