

From Top Down to Bottoms Up In Fibromyalgia
For the past decade or so research evidence has suggested that fibromyalgia is more a brain disorder than a body disorder. Studies indicating increased substance P levels, increased activity in the pain sensing and decreased activity of the pain inhibitory sections of the central nervous system suggest people with FM have a nervous system primed to produce pain. The central sensitization theory suggests FM is a ‘top-down’ disorder that starts in messed up circuits in the brain and goes down from there.
Recent studies taking a close look at the muscles and skin, particularly the stunning small fiber neuropathy findings, suggest it’s far too early to dismiss the body in FM. In fact, some researchers are suggesting that the ‘central sensitization’ present may be driven by problems in the body – a stunning turnaround from a decade or so when the body was more less, excluded from the conversation.
This may not be just about fibromyalgia. If this theory is right the pain and fatigue in ME/CFS and FM my very well come down to two common denominators in both diseases; the sympathetic nervous system and the blood.
Some Background
Let’s back up and look at some recent things we’ve learned regarding the SNS/blood interaction.
- Allodynia may be caused by an inflammatory cascade (ischemia) produced by low blood flows to the tissues.
- Low blood flows to the muscles are present in both fibromyalgia and chronic fatigue syndrome.
- ME/CFS patients appear to have such reduced aerobic functioning that they begin producing energy anaerobically very early in an exercise period. Anaerobic energy production produces toxic metabolites that cause pain and inflammation.
Now a theory posits that anaerobic metabolites and inflammatory cytokines caused by low blood flows are driving the central nervous system sensitization present in fibromyalgia. This theory suggests that small blood vessel constriction caused by an overactive sympathetic nervous system is the problem.
In this study, researchers looked for evidence of sympathetic nervous system/blood vessel problems in one of the most blood and blood vessel-rich areas of the body – the hands.
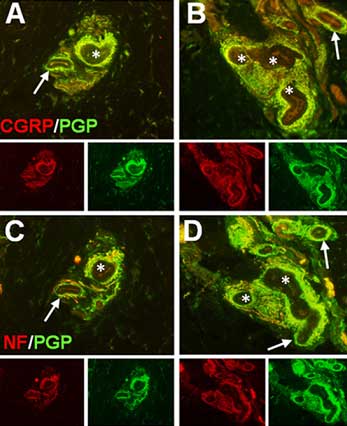
- Pain Med. 2013 May 20. doi: 10.1111/pme.12139. Excessive Peptidergic Sensory Innervation of Cutaneous Arteriole-Venule Shunts (AVS) in the Palmar Glabrous Skin of Fibromyalgia Patients: Implications for Widespread Deep Tissue Pain and Fatigue. Albrecht PJ, Hou Q, Argoff CE, Storey JR, Wymer JP, Rice FL.
Small Caliber Nerves – Big Caliber Effects?
Our hands are more than just tools. It turns out that sensory and autonomic nervous system nerve fibers permeate the small blood vessels in our skin. When we get too hot these small ‘caliber’ blood vessels dilate, bringing blood to our surface to cool us. When we get too cold they help us retain heat by constricting and sending blood to our interior organs.
These researchers biopsied small pieces of skin in the hands of people with fibromyalgia to see what was going on in this area of intense nervous system and cardiovascular activity. If the sympathetic nervous system was messed up it should definitely show up there… and it did.
Results
Taken together, these data indicate that FM patients have a neurovascular pathology in the palms of the hands predominantly increasing the peptidergic sensory innervation of the AVS.
Sensory nerves that relayed pain and other sensory signals and dilated the blood vessels abundance were highly abundant in the small shunts between the arteries and veins in the hands of the FM patients.
Loaded with small capillaries, the hands of humans are not only important thermoregulatory’ devices but they’re also important reservoirs of blood.
It turns out that the blood flows to our hands far exceeds their metabolic demands. Our hands are essentially used as blood storage sites the body can access to quickly shunt blood to areas in need. Studies indicate that as soon as you start to exercise, for instance, blood flows out of your hands and into your muscles.
The high levels of sensory nerves found in the FM group suggested why some FM patients experience pain in their hands, particularly when it’s cold.
“the excess sensory innervation may itself explain why fibromyalgia patients typically have especially tender and painful hands….But, in addition, since the sensory fibers are responsible for opening the shunts, they would become particularly active under cold conditions, which are generally very bothersome to fibromyalgia patients.“ The authors
Blood In…..Not Blood Out
The researchers found that the shunts between the arterioles and veins in the hands were highly innervated with blood vessel-dilating nerves suggesting that blood was able to easily find its way into the hands but not out of them.
Given the role the hands play as storage reservoirs for blood not being able to move that blood around could be a problem if you want to exercise, think hard or sleep. The authors suggested that fatigue during exercise, cognitive problems during thinking, and problems sleeping could all be a function of these dilated small blood vessels in FM patients’ hands.
With the blood stuck in the hands, the SNS could be tightening blood vessels down elsewhere in an effort to squeeze what it has available out to the muscles and the brain.
Interestingly, given the gender imbalance in this disease, estrogen is a huge player in sensory nerve production in the hands and females typically, have twice the sensory innervation in their hands than men.
It seems a bit much to say FM is all in the hands but throw in problems with blood volume, dilated arteries elsewhere and issues with the mitochondrial uptake of oxygen, etc. with shunts that appear to be chronically open in one of the most blood-rich areas of the body, and maybe you really have something.
Perhaps the blood really will out in ME/CFS and fibromyalgia.
The authors are examining male FM patients to see if the same pattern applies.
New Treatments Possibly on Tap
They noted that SNRI drugs that act on the brain also act on the nerve endings in the skin and may be helpful in FM and assert the finding opens the door for new therapeutics.
“This discovery provides concrete evidence of a fibromyalgia-specific pathology which can now be used for diagnosing the disease, and as a novel starting point for developing more effective therapeutics.”
Senior Research Chair of the Alan Edwards Center for Pain Research at McGill University, Dr. Gary Bennett felt so, as well, stating
“It is exciting that something has finally been found. We can hope that this new finding will lead to new treatments for fibromyalgia patients who now receive little or no relief from any medicine.”
- Check out an excellent reader-friendly explanation of all this by the authors of the study.
- Coming up soon: bottoms up indeed for FM; the stunning small nerve fiber neuropathy findings suggest fibromyalgia should perhaps be called fibroneuralgia….







Interesting, but it brings up a question….& I may just not be understanding something, but I know that a lot of people with fibro (& maybe with ME/CFS as well) have Reynauld’s Syndrome, which is actually caused by the blood vessels in the hands (& often the feet, too) overreacting & pretty much shutting down blood flow to the hands, fingers (& toes)….that seems to be the complete opposite of this, so it seems odd that Reynauld’s would be so common in Fibro if the cause of Fibro is too much blood in the hands
After years of CFS I only recently began to for relate my bad days with swelling and stiffness in my hands. On these days not only does my coordination seem affected but my mental processes are significantly slower
I agree with Tammie – I have terrible blood flow to my hands and feet and while I do experience deep, sore pain in my hands and feet at times, it’s my neck, shoulders and back that cause the worse and more consistent pain for me. Also, while i can see how this could come into play with muscular pain, how does this relate to joint pain?
katesw…..Have you seen a Neurologist who is easy to get along with, but more important than anything else specializes in diseases such as SM (Syringomyelia). The pain around your neck, shoulders and back make me wonder if you have a neurological illness causing at least some of your symptoms. By the way, I wholeheartedly believe that you can be suffering from ME. Still, I’d like to see SM ruled out and its often present cousin, Arnold-Chiari Malformation. I’ve noticed that as I age, joint and hand pain is quite painful. Of course a broken arm, etc., may do that for you, too. I’m 73 and have had ME for at least 45 yrs.
I agree with Tammie – I have terrible blood flow to my hands and feet and while I do experience deep, sore pain in my hands and feet at times, it’s my neck, shoulders and back that cause the worse and more consistent pain for me. Maybe having Reynaulds makes no difference or could it possibly be a response TO and a way of the body coping with what would otherwise be blood-filled hands?
Also, while i can see how this could come into play with muscular pain, how does this relate to joint pain?
The idea that Reynauld’s could be a response to blood filled hands might be true of some people with Fibro and Reynauld’s, but I had Reynauld’s LONG before I got Fibro and ME/CFS.
Perhaps the pain from what is thought to be Reynaulds syndrome is actually from the problem described here? Just a thought, since I’ve never had a formal diagnosis of Reynaulds syndrome so I don’t know what goes into testing for and diagnosing it.
Hey. That makes sense, and finally something about this disease that talks about hands—always one of my primary sources of pain. My hands are almost always hot and they burn. My patients like it; not too many health care practitioners have warm hands, especially in the icy environment of the OR! Strangely, however, my feet, which also hurt (but only after standing) tend to get cold easily.
As I noted in another comment, the authors in the study specifically referred to painful hands; I don’t think I referred to that in the blog but it sure sounds like its present in FM/CFS…
Everyone I’ve spoken to (who’s been diagnosed with CFS/ME) has problems with their hands, not so many have problems with their feet. But my feet are as problematic as my hands, it feels as if they boil when I’m tired, even if they feel cold to the touch to other people.
What interests me most about the above though is whether there might be any link to sensory processing disorder. I conceived my son, who has severe sensory problems (and probably ASD), at the same time that I went down with the shingles that triggered this nasty condition – I’ve often wondered whether my illness caused his problems.
Really interesting Rachel. Boy those sensory and autonomic nerves are closely related; in fact I believe that the same nerves can relay both sensory and autonomic nervous system information. We’re going to see this in the small fiber neuropathy blog coming up.
What kind of issues does your son have, if you don’t mind my asking.
He has a mix of hyper and hypo sensitivities. The primary problems are his hyposensitivities which leads him to bang and crash a lot, he’ll climb up high and deliberately fall off which gives him both the vestibular (movement) and the proprioceptive (pressure) stimulation that he needs. He doesn’t get dizzy, he can swing and spin for ages. (I’m the opposite to him on these senses and so is my older son, we both get very dizzy very easily and hate banging into things – it hurts!)
His main trigger is his head – we solved the sleep problem overnight by using a tight hat, instead of 12 nights a year he now sleeps through unless he’s actually throwing up. Once he was able to sleep and we found strategies to give him the stimulation he needs (and changed school to one which was prepared to use them) he started catching up really quickly; he still has language problems and is emotionally immature but the speed at which he is learning is incredible.
I’ve learned a lot through my youngest’s problems and I now understand a lot more about myself. Which is another reason why I wonder about a link. I’ve often pointed out to my doctor that the symptoms I have had nearly all occurred before I technically fell ill, it’s just that they are now magnified to the nth.
My dad says I’ve always pushed myself to my limits and then as far past as possible – that’s a common feature with people I know with ME/CFS, they were ‘always busy’ before they fell ill, always multitasking – the kind who watch tv, hold a conversation, do the accounts and knit all at once. And not necessarily sporty but very active. Those I know who have claimed to recover through what I consider ‘think yourself better’ techniques were invariably not ‘always busy’, high achievers maybe but not compulsive multitaskers.
These highly nerve packed ‘shunts’ in question are found in three places; the hands, the feet and the lungs – so it sounds like its very possible for this problem to show up in the feed as well. (Now what about the lungs???)
Hi Rachel
Did you read my ‘blog’ on sensory gating problems in ME/CFS?
http://www.cortjohnson.org/blog/2013/01/17/not-fatigue-after-all-new-model-suggests-other-symptoms-explain-chronic-fatigue-syndrome-mecfs-better/
This series of blogs started from discussions on Phoenix Rising where many of us reported various sensory processing or sensory defensiveness issues (involving, light, sound, touch sensitivity or just general ‘overload’) as well as certain traits such as social problems and face recognition issues that are more associated with ASD.
This led me to identify a range of neurological, psychiatric and neurodegenerative conditions (including ASD and ADHD) where researchers has found sensory processing issues as measures by various sensory gating deficits. I also found that common to these conditions were similar physiological findings to ME/CFS – immune dysfunction, oxidative stress and mitochondrial dysfunction.
This I suggest may be underpinned by a ‘neuroinflammatory vicious cycle’, part of which is an imbalance between the neurotransmitters GABA and glutamate where elevated extracellular glutamate is neurotoxic.
This mechanism may cause the neurological problems found in ASD etc and can also result in peripheral (and potentially autonomic) neuropathies which Cort will be blogging on soon (the vascular shunt thing is news to me and very interesting as I too have problems with my hands including swelling every time I do anything physical).
Perhaps the same mechanism acting at a different stage of development can lead to different conditions?
You might be interested to know that a company called Seaside Therapeutics are about to trial ARBaclofen (a modified for of the GABA B agonist Baclofen) for ASD. It has already shown that its the first drug to improve social functioning in Fragile X syndrome – a subset of ASD :
http://healthland.time.com/2010/12/01/how-a-new-version-of-an-old-drug-may-someday-help-treat-autism-and-addiction-too/
I’m reading Marco, I’m reading 😀
Raynaud’s is set in many FM patients. Some also have a sign of a sympathetic nervous system gone haywire, levido riticularis causing discoloration. These are relayed to the SNS. However, we must also consider comorbid hypothyroisim and myofascial trigger points. One being endocrine, the later having to do with fine muscles with knots that can compress vessels and nerves. I doubt the SNS connection is coincidental, but more research is needed, which includes screening for comorbid disorders.
Thanks Celeste for your insights. I look forward to learning more about myofascial trigger points.
Cort,
What about the findings of Dr. A Melvin Ramsay, which show that deformation of some of our red blood cells can cause oxygen to fail to pass through our smallest capillaries? Apparently it is an intermittent problem, and only shows if our blood is fixed immediately after being taken.
Dr. Les Simpson describes this in his book new book Ramsay’s Disease. Recently published on Kindle
To Dr. A. Melvin Ramsay. “…The failure to agree on firm diagnostic criteria has distorted the data base for epidemiological and other research, thus denying recognition of the unique epidemiological pattern of myalgic encephalomyelitis.”
Simpson PhD, Leslie O.; Blake BA CQSW, Nancy (2012-05-28). Ramsay’s Disease – Myalgic Encephalomyelitis (ME) and the Unfortunate Creation of ‘CFS’ (Kindle Locations 26-29). . Kindle Edition.
=========
My hands are just now beginning to be painful. I was attributing this to needlework, but maybe other things are exacerbating this.
Thanks for sharing.
I sure remember about red blood cell deformation but I haven’t heard anything about that for years. I don’t if it was looked into and disproved or just not looked into. If its really there it certainly would fit right in with all these blood flow issues. Maybe somebody else knows.
I was extremely interested to read this article. Since the beginning of my illness I have always felt that my hands were a barometer of how well/ill I am. The more disabled I am the redder the palms of my hands. They appear mottled. In fact if I want to try to do something my husband will often ask to look at my hands – if the palms are red he advises against it. Also, the more ill I am feeling, seems to show deeper red points within the mottling. I have mentioned this to doctors on numerous occasions and none of them seem to have any knowledge of it. My hands are also extremely painful and I am unable to complete any fine movements anymore – and even using a keyboard can be excruciatingly painful.
I’ll be very interested to see if this research goes further.
We’re going to get more into small nerve fiber conditions in the small nerve fiber neuropathy blogs coming up…it sounds like this finding fits you though. Even though I didn’t really mention it they specifically talked about painful hands in the study…
As many of you with Fibro, I also have painful hands (symptoms started 4 yrs ago for 3 months then resolved) now back again for past 2 months. But I also have pain in neck, shoulder, ELBOW (cubital tunnel synd??) and hands(Pain mainly at first digital(phalanges) of ALL fingers and all symptoms in BOTH(bilateral) arms!!! Will get results tomorrow from MRI cervical, as I suspect pain, numbness ,tingling bilateral caused by disk compression and/or osteophytes! If negative, then it’s all Fibro. What are your comments about ischemis/oxygen issues not ONLY affecting hand, but also elbow (ulnar, medial, radial nerves)? Thanks Steve
Excellent Article Cort. I have POTS which I believe to be a mild form of Chronic Fatigue. I have noticed that when I have more severe POTS symptoms, when I raise my hands higher than heart level, they go pale and the blood drains from them quickly. I think this action sets off an adrenaline rush to try to get the blood back up to the hands and if I leave them up there I think I’d pass out eventually. I’d love to know the cause, could it be the ‘floppy/stretchy vein’ theory as in EDS, or the veins being dilated by an excess of a ‘toxin’ like histamine. I don’t know. My heart does go out to all those suffering with Fibromyalgia, I’m glad there’s progress in this study.
Hi Cort,
Great article! I have POTS and use my hands as a barometer for how bad it is. If I raise my hand up and it goes pale white vs the red one being held below heart level I know POTS is worse. I’d love to know the cause – if it is vascular stretchiness as in EDS or dilation from a neurotoxin like histamine. I hope research continues!
I personally believe POTS is a mild form of Chronic Fatigue. My heart goes out to those with Fibro, it is so hard to live with and more research is needed. I think the old wastepaper diagnosis labels are becoming less applicable.
Thanks again, Cort, for a great article. I also suffer from very painful hands and feet as well. Sometimes they both are freezingly Cold or really hot or the feet are ice-cold and the hands hot and so on. The pain is in all cases very rough and it is hard to stand on my feet or to do something with my hands.
I have never thought of that to check with my hands and feet how good/bad my daily conditions are. Many thanks fot that tip to you who mentioned that.
I also wonder, there stood something about a SNRI-drug that may help. Do you know what kind of drug is that?
Take care all!
The same arteriole-venule shunts are found in the feet and the lungs. so it makes sense that your feet might be effected. They mentioned SNRI drugs produced by Eli Lily (who funded the study) but didn’t mention what they were. These drugs effect the brain and the nerve endings in the skin.
Thank you – again! I am very excited about these findings!
Interesting stuff. I’ve found the SNRI pristiq (desvenlafaxine) really helps my hand and feet pain…but it might be making the POTS worse. When I tried going off the drug within a day I had much more pain. I think it’s a bit trial and error though as to it working for you and needing to weigh up the other issues of taking an antidepressant.
Good grief -does this explain why when I feel awful i feel the urge to put my hands above my head -i often can’t help myself!
I am ”happy” for FM patiënts with this finding but i do not believe the ”skin” is the problem. FM patiënts have wide spread pain in there muscles.
With fm, if I am typical, one has pain even where there are plainly no muscles. With the skin out of the way, muscles feel very little pain when operated on. I know. Skin is not only practically everywhere, but is also our most sensitive organ. That some perceive fm to be muscle pain is in part a trick of the mind and also the result of having been told that that is what it is, even though the evidence for that assumption has remained poor.
Interesting Kerry…Thanks for your viewpoint.
Good grief, is this why I always feel the urge to put my hands above my head when I’m feeling particularly bad? I often can’t help myself – perhaps it helps to drain the blood towards the brain…
It’s weird but I notice that too, putting my heads above my head helps me to talk better. I have more energy. I notice this just last week when in exclamation I put my hands up and I had more energy…its so bizarre….
It is not so weird because we have bloodcirculation problems in the small bloodvessels. The small vessels are constricted most of the time in whole the body. Also the blood flows to the gut instead of the brain and vice versa etc…
I had to try this and did like you – put my hands and feet up in the air…………..and I never thought that to lie like the letter U should make the pain to decrease, but it did :-).. As soon I took them down the pain came back. Little impractical way to live ones Life though but a relief for the moment, because no pain killers ever help. I shall try this when talking to someone and see what difference it will make. Good tip, many thanks that you wrote this!
I do this as well, and I can’t stand sitting with my hands in my lap, they’re always above my elbows (and usually above my heart) unless I’m doing something.
Thank you Cort for bringing this to us.
This fits my illness and severe chronic pain to a T. When I first became ill with FM & ME it hurt to shake hands with people. I thought it was arthritis in my hands. As a child that had 65 allergies and severe asthma (as many people with FM/ME/CFS have in common) I found the connection to the lungs and inflammation (asthma) quite interesting.
Namaste
I do have a question. When these people were tested, were they on any medications/supplements (whether over-the-counter or prescription) whatsoever? I’ve heard of many varied tests (such as this) proclaiming it’s the cause of FM/CFS due to the high percentages of “their” results.
For 12 years since my diagnosis at Mayo, along with a ton of reading, I’ve had to “pay attention” to what my body is telling me. What I’ve learned is this…personally, I believe FM is caused by “multiple chemical sensitivities”. This includes medications of any sort along with all the chemicals that are now allowed in not only processed foods (including GMO’s, all forms of hidden MSG, etc.) but chemicals in proteins we eat whether it’s animal or vegetable (soy/corn comes to mind). Add in avoiding plastic products such as bottled water/plastic straws/eating utensils, etc.
When these people were tested, were they properly “prepared”?. In other words, consumed only “true” foods provided by Mother Nature. Were they told not to take any form of medication and/or supplement? Were they told not to use any form of plastic for drinking, eating, cooking (avoiding all petro-chemicals)? If not, then it’s not a “true” study since “chemicals” could be the skewing factor in this test.
In today’s world, it’s almost impossible to avoid most of what I’ve mentioned above. But, I know this. If I control (to the best of my ability) what I consume, I don’t have FM flares. I do well for the most part. I had a pulmonary function test 2 days ago and was given Albuterol for the second 1/2. Since then, I’ve been in a terrible FM flare and know it’s going to take about 3 days to get that medication out of my system.
All this, of course, is just my humble opinion. But, I would like to know how the study patients were “prepared” for this test.
Very interesting. I feel like blood pools in my hands, as the day progresses i feel compelled to raise my arms and stretch my fingers to try to get the blood to flow out of my hands. I am almost bedbound and dont see many people. The few who do see me seem bemused by my strange behaviour. However, if my subconscious wants me to do something i really try to listen these days. The twenty ish years that ive been ill it turns out my subconscious was far more in the ball than the medical professiinals.
I dont believe there is a one size fits all for us. But i do thinkmthis could be a piece in the jigsaw, further research would be interesting
What’s going on in the vasculature of the hands isn’t special, it’s what’s going on
in all 12,000 miles of the microvasculature in the CFS! That’s why people with ME can’t tolerate blood shifts
that go on in mild exercise (skeletal muscle is Chock full of blood flow!)…… and in states of dehydration,
or in simply standing up! OI and all that jazz.
One study by Dr. Spence a number of years ago documented on the response of the CFS skin vasculature
to the vasodilator Acetylcholine to be quite prolonged(~45min.) compared to HC(~5-10min.)
The hands are simply reflecting the broader problem. Which, by the way, does lie in the central nervous
system, which controls autonomic function, or in this case dysfunction, accounting for vasomotor instability,
HPA axis abnormalities, chronically depleted blood volume (BTW, no folks, don’t donate blood, not because
of the ever elusive “stealth pathogen”, but because you will get Much sicker), vertigo, etc…
Barbara Cottone, M.D.
down and out since Apr. ’96
Nice points Barbara…I wouldn’t be surprised at all if you’re right. I kept waiting for MERUK to continue on with acteycholine studies. I wonder if it didn’t pan out. It sure was exciting…
My hands have often hurt quite bad during a bad episode of FM. My new rheumatologist said that if my hands hurt then it can’t be FM. Needless to say I got a new doctor. My palms are mottled most of the time and I can no longer crochet. I’m in the middle of an afghan for my son and can’t seem to finish it.
Kelly
Glad you got a new doctor :)…I hope things turn around for you…
I too have had a lot of pain in my hands over the years with fibromyalgia. At first there was a lot of pain in the wrist area, then it seemed to turn into carpel tunnel syndrome which eventually went away. Strangely, I too have gone through periods of sleeping with my hands above my head,it just seemed to help me get comfortable. I have noticed patches of my body can get very cold,almost icy, as if there is no blood in that area regardless of the weather .I rub them to get the warmth back and relieve the pain. I have noticed these patches on my back ,upper arm and thigh,about the size of the palm of my hand,they are not there all the time. My feet tend to be icy cold at night when I get into bed.I wonder if anyone else has discovered these patches of very cold areas on their body. It seems to me that they could be explained by these findings about blood flow in fibromyalgia.