



(Ken Lassesen has recovered three times from chronic fatigue syndrome (ME/CFS). In his gut series on ME/CFS/FM he provides his personal prescription for better health through gut flora manipulation. Please note that Ken is a patient, not a doctor; these blogs are for informational purposes only. Please consult with your physician before making changes to your treatment regimen.)
Before we look at correcting the microbiome, we should understand better what we are striving to do and why.
Microbiome is the fancy new name for the gut and other bacterial systems that keeps us alive. All microbiomes are not the same — in fact, the microbiome you have is connected strongly with your DNA and is actually more unique than your DNA. A recent study of identical twins found that they can be told apart by their microbiome and not by their DNA.
You have around 100 trillion bacteria according to a recent New York Times article which states:
Our resident microbes also appear to play a critical role in training and modulating our immune system, helping it to accurately distinguish between friend and foe and not go nuts on, well, nuts and all sorts of other potential allergens. Some researchers believe that the alarming increase in autoimmune diseases in the West may owe to a disruption in the ancient relationship between our bodies and their “old friends” — the microbial symbionts with whom we coevolved.
Microbiome Under Attack?

Modern times with our poor diets, low use of fermented foods and high antibiotic use have not been good for our gut flora
Modern times have not been good for our gut flora. Our modern high carbohydrate and fat diets have been shown to negatively effect the gut microbiome but for increasing numbers of us the negative impact to our gut flora began long before junior had his first french fries. Research indicates mothers actually pass important parts of their microbiome to their children as they move through the birth canal. Some researchers believe the higher rates of C-sections in the modern era maybe inadvertently contributing to the higher rates of allergy, asthma and autoimmune problems present.
Frequent antibiotic use may have snuffed out some good gut flora in many of us. Nor do we eat the array of probiotic saturated fermented foods our ancestors did. Given all that it’s no surprise that the diversity of our gut flora compares poorly with those living in more traditional societies with their healthier, more varied diets and reduced C-section and antibiotic use rates.
Shifts Confirmed in a June, 2013 Study
Marc Frémont, Danny Coomans, Sebastien Massart, Kenny De Meirleir just published a study (full text free) which found
“A highly significant separation could be achieved between Norwegian controls and Norwegian patients: patients presented increased proportions of Lactonifactor and Alistipes, as well as a decrease in several Firmicutes populations.”
and
“129 Different bacterial genera could be identified from the 79 samples included in the study. A majority of these however were present only in a few samples (sometimes just one or two subjects, in a very small proportion).”
Micro in Name Only: Little Bugs With Big Impact
There is already abundant evidence that microflora can have system-wide effects and influence immune responses, brain development and behavior. Williams, Hornig and Lipkin et. al.
Researchers are still figuring out how important gut flora is our health but studies suggest the state of our gut can impact many areas, some of which are listed below.
- inflammatory gastrointestinal disease – reduced levels of a helpful bacteria appear to set the stage for Crohn’s disease
- cognition – specific bacterial families are associated with poor cognition and inflammation
- obesity – certain bacteria that metabolize food more completely may increase the risk of obesity/weight)
- B12 levels (Lactobacillus Reuteri produces most of it)
- autism – people with autism appear to have a unique gastrointestinal flora that has less variety than healthy individuals.
Autism provides an intriguing example of a dysfunctional gut (increased intestinal permeability, aberrant immune profiles, etc.) possibly contributing to severe cognitive and emotional dysfunction. Hornig and Lipkin’s Center for Infection and Immunity recently published a study suggesting reduced levels of carbohydrate digesting enzymes may lead to high carbohydrate levels that foster the growth of unhealthy bacteria. Indeed, RNA sequencing indicated an abnormal gut flora was present (decreased levels of Bacteroidetes, increased Firmicute/Bacteroidete ratio, Firmicutes and Proteobacteria, and increased Betaproteobacteria.)
A CFIDS Association of America pilot study recently found greatly increased ratios of Firmicute/Bacteriodetes bacteria before and after exercise in ME/CFS. People with ME/CFS also may have deficits in the bacteria that produce B-vitamins in our guts.)
These researchers believe changes like these could effect immune functioning, brain development and behavior.
The Infection Connection
It turns out that most infections do temporarily change the microbiome which usually reverts to normal after the infection has passed. In approximately 4-8% of cases, though, this fails to happen and the microbiome remains in a new stable state.
That percentage is pretty close to the percentage of people who come down with a CFS-like state after flu-like infections. Researchers have examined immune, autonomic, endocrine functioning in people with ME/CFS at the start of infection and afterwards with marginal success. Thus far, immune up regulation and increased symptoms during the early course of an infection and autonomic variables later on are the only unique factors found in people with infections who come down with ME/CFS.
No one yet,however, has examined the most immune-rich substrate of all – the gut. I propose that an infection induced change of gut microflora – which do not revert to normal – plays a key role in chronic fatigue syndrome.
A Historical Analogy
Think of your gut (an ecosystem or biome, if there ever was one) as a land; in fact, think of your original gut (hopefully fully populated with your mothers microbiome) as Newfoundland in Canada prior to the entrance of the Vikings. The Native Americans living there, the Beothuk, flourished until an invading species (an infection) arrived called Lief Eriksen and the Vikings. The Vikings lived there for a few seasons but the native species eventually pushed them out, just as your body does to an infection. The next time around, the Boethuks met a more difficult match in English settlers and the settlers eventually pushed the Beothuk out.
Has our original microbiome been altered by unwanted invaders? I believe it has.
Your Microbiome is Unique to you — and So May Be Your ME/CFS/FM
If my hypothesis on the cause of ME/CFS/FM is correct (a stable dysfunction of your microbiome) then every patient will have a different variations of their unique microbiome! This means that your symptoms will be slightly different because your dysfunctional bacteria are slightly different. This actually goes one step further, the signaling chemicals from these bacteria interact uniquely with your DNA.
Getting a good idea of your gut composition, however, is difficult. Unfortunately currently available medical tests only characterize a small percentage of the species in our gut. Tests done at academic centers (not available at commercial labs) using PCR and DNA fragments are more accurate. Furthermore, many species(~ 80%) cannot be kept alive outside of the body which makes study very difficult.
A good review is at Aging of the human metaorganism: the microbial counterpart from which the diagram below comes from.
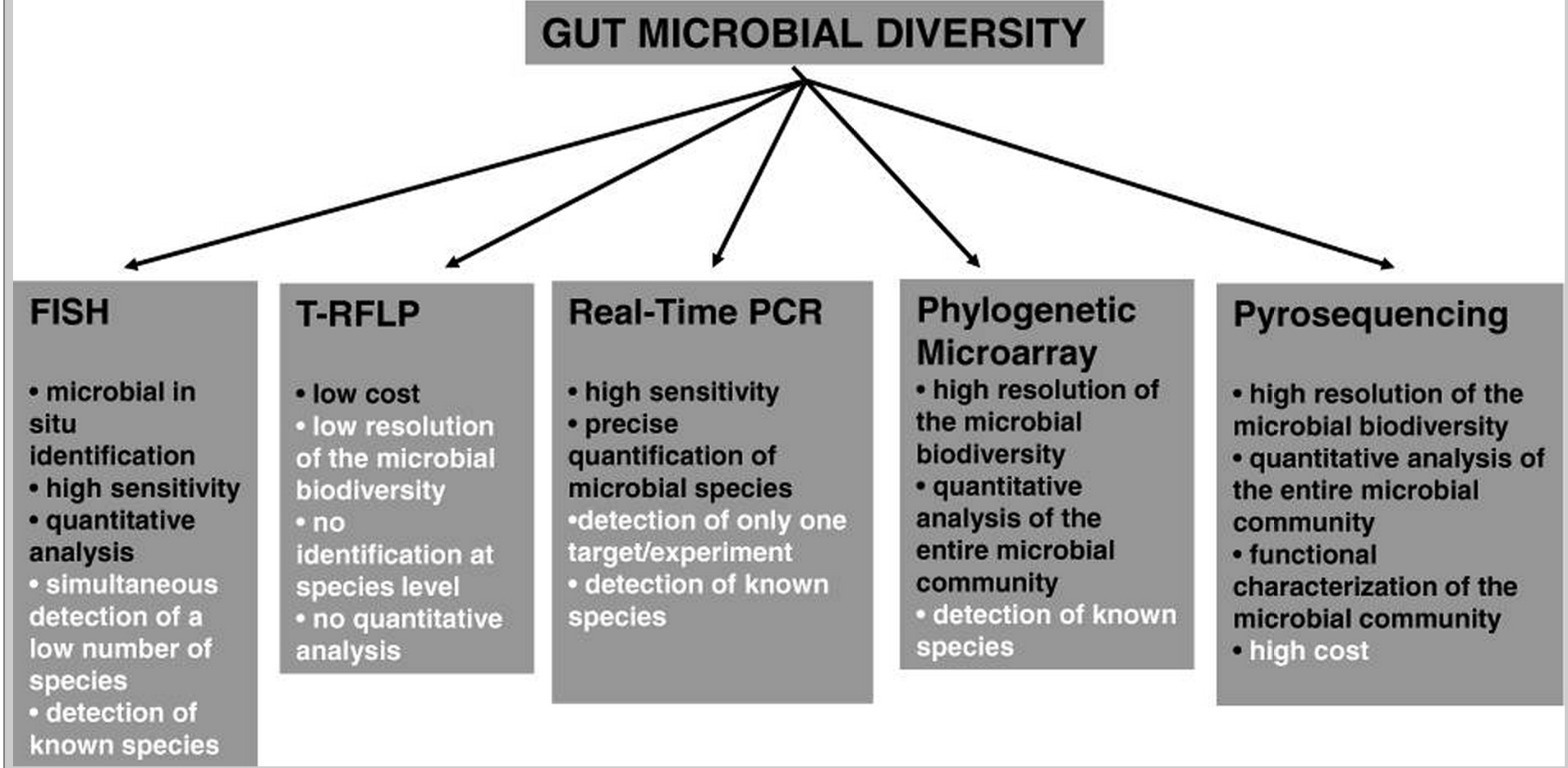
Commercial labs test for less than 2% of the bacterial strains present in our gut.
Altering Gut Flora: More Art Than Science
That means there’s more art to changing the gut flora than science.
On the plus side, it appears very possible – by effectively declaring war against the offending bacteria – and then aggressively repopulating it with good ones, to alter the gut flora. The disruption is not easy — before the arrival of antibiotics- a reset of the gut flora often began by inducing a gut infection (often cholera) to clear the slate, so to speak. Asking a MD to infect you with cholera to treat CFS today , of course, would be met with complete disbelief ; at one time, it was conventional medical practice and was reportedly successful. (Then again who would have thought we’d be talking about fecal transplants or using worms to alter gut flora….)
In following posts, I will share my current understanding and experience in being an anarchist against this dysfunctional microbiome. To me, any change is better than resignation to the current state of health in CFS.
The key items are:
- Killing off bad species (may have collateral damage on the good species) – antibiotics, herbs, spices
- Feeding the good species (so they start to dominate) – prebiotics, often FOS, but there are other things
- Disruption of the new stability (so the old ones have a fighting chance)
- Importing good species (a.k.a. probiotics of the appropriate type, fermented foods, raw milk and fecal transplants)
- Starving the bad species (so there are less of them) – no gluten and no sugar diets are likely doing this
I believe the following approaches have the right general approach but may lack the fine-tuning needed for ME/CFS and other disorders. Early reports suggest that ME/CFS patients, for instance, may have a major drop in all E.Coli species but in Crohn’s Disease over 95% of the invasive species are E.Coli. With one, you want to encourage (healthy) E.Coli; with the other, you want to kill off (unhealthy) E.Coli — one treatment plan does not suit all conditions.
These approaches below are correct, I believe, that we should attempt to enhance our gut flora — but they have not evolved enough to address specific gut dysfunctions.
If you are doing any of the above, I suggest that you keep doing them but consider adding a few modifications that I will be suggesting in my following posts that are specific to the microbiome shift that may be occurring in CFS (which is likely similar to that seen with IBS). I have yet to see any reports of the above consistently resulting in remission of CFS but I have seen reports of symptoms reduction. I believe they are likely part of the solution but are insufficient in themselves.
- Dig Deeper! – find more of Ken’s Gut Flora Manipulation Series on Health Rising’s Chronic Fatigue Syndrome and Fibromyalgia Gut Resource Center








Hi ken,
Always interested in reading your posts. Ive been on the prescript-assist probiotic for a week and a half as you suggested ( i did the fecal transplant last year which i believe made me worse). So far only bery minimal benefit to my IBS and not much with CFS at all. I still may want to try 3 days of vancomycin and then do more prescript-assist. My doc is also suggesting the gcmaf bravo probiotic after the vanco. Any Thoughts on what i just said?
Thomas
Info on the product is at: http://www.gcmaf.eu/ with 40+ PubMed articles (http://www.ncbi.nlm.nih.gov/pubmed/?term=gcmaf ). The site cites “The GcMAF activated macrophages rapidly phagocytize various bacteria (E. coli..” the fancy ph word means “to engulf and destroy bacteria” so we have an E.Coli killer.
So the question to ask your MD, why would you want to kill E.Coli that you are probably already low in?
Ken, Do you have any thoughts or data on MAF314 by Ruggerio. I’m a Cheney patient and did very well on it. But be careful anyone who reads this because there is die-off that happens… that cause intense cytokine storms that can really hit your brain matter so you need OTC meds that protect 3 receptors in the brain… You need testing by someone who is able to monitor http://en.wikipedia.org/wiki/Calcitriol and D as well as Nagalase by a doc who can follow your chemistry as you will crash if your Nagalase goes below 1. Don’t quote me as I don’t remember all the details. Ken any thoughts on MAF314?
My gut is much better. I eat no sugar, fructose, or high glycemic vegies. Mostly raw food…
I think that MAF314 is effective for only certain genotypes Cheney found. some did not do well. Some did well and then crashed.
GcMAF was excellent. Also expect cytokine storms with GcMAF
But my gut is not 100% more like 50% from 0%. Any other ideas besides Mutaflor?
I have a brain injury and so I’d go back on Maf 314 or GcMAF – they are definitely a piece of the puzzle but I dare not to play with my brain right now.
Substances being effective for only certain genotypes is very much in keeping with the microbiome hypothesis. Microbiome and DNA are closely connected, and thus genotypes.
I will be going thru other things in the next posts. As a FYI, the 100% rye german bread (Mestemacher Bread Whole Rye, Feldkamp Whole Rye Bread, 12 loafs for $30 or less on Amazon) appears to make a significant difference. On my own blog, some one reported that first round with mutaflor had little response, but the second round after starting to eat the above breads “hit me like a truck”.
Lactobacillus Reuteri is near the top of my list. The reason is simple, in almost all mammals it is the species that is usually most seen in healthy individuals. Often studies reported something like 55% of the Lactobacillus species are Reuteri. It is NOT in most probiotics. L.Reuteri is by far the Lactobacillus that is most likely to persist in the gut, most Lactobacillus are literally flow-thru, they have an impact, (in fact, one antibiotic (not used much today) is extracted from Lactobacillus Acidopholus), but do not establish a colony. It produces reuterin and cobalamin (B12), which no other Lactobacillus does.
My own practice is to buy as many different strains of L.Reuteri that I can find. For maintenance, I do a week of it every 2-3 months. Glutathione is one of L.Reuteri essential foods (http://www.ncbi.nlm.nih.gov/pubmed/21585317 ) so make sure that you supplement with it (I would suggest taking that 1 hr before the L.Reuteri) . For a more technical description of L.Reuteri, see http://microbewiki.kenyon.edu/index.php/Lactobacillus_reuteri and http://www.plosone.org/article/info:doi/10.1371/journal.pone.0031951
Ken– Thanks so much for this great series of articles. Have you found a product that has lactobacillus reuteri without other lactobacillus strains? It seemed like all the products I saw on amazon and iherb had l reuteri combined with some undesirable strains.
I have been taking prescript-assist for a week and even at 3 pills a day I am not noticing any changes other than a slightly slower digestion time. Any ideas?
Since most of the other L. strains tend to flow thru the gut, I am not that concerned if you are doing 7 days on, 3 weeks off. The L.Reuteri should persist more and more on each cycle.
Probiotics tend to be less dramatic at the start then antibiotics or antibacterial herbs, often their impact will slowly build over 1-2 weeks, especially on the first go-round. On my own blog, someone using Mutaflor mentioned little response on the first cycle, the second cycle (while adding German Rye Bread) he described it as being hit by a truck.
With mutaflor, I was at the point of giving up it’s use when I realized one symptom had totally disappeared. That kept me going on it.
I have used prescript assist on two occasion when unexpected stress started to alter my gut bacteria (i.e. distinctive change of smell and texture). Both times, 3-4 days on prescript assist reversed the undesired shift.
I do not have a protocol, I have a model. The model says that you need to disrupt the stable dysfunction microbiota. This is done by adding in good probiotics of the right nature (ones that will not flow thru) and killing off the bad (and some good) by rotating thru many families of herbs and spices effective against the probable overgrowth. In one way, this is very close to C. Jadin protocol, except, it appears possible to do without needing prescription antibiotics.
Thanks! I am working on creating a protocol based on your model and was wondering if I could pick your brain a little more?
I didn’t notice a big difference with Prescript Assist but seem to be having a great response to just 3 days of Neem (I am up to 1800mg a day.) It’s interesting because I have tried ayurvedic herbs and other gut modulating supplements before but I think the increased dosage may be key. I ordered 1/2 lb of Neem, Haritaki, Tulsi, and Turmeric from Banyan.
1) Do you have an opinion about whether it is fine to just mix the herbs in warm water and skip the capsules? I wa planning on measuring the weight out with a precise scale and take your suggested approach of increasing from 00 (~500mg daily) until I get an obvious response and staying on the specific herb for 7-10 days.
2) Is there a reason that you don’t combine the probiotics on the same day as the herbs? I know with antibiotics the recommendation is often to take the antibiotic in the morning and the probiotic at night. Is it because you think the probiotic will just be wasted due to the inhospitable gut environment or do you think there are potential downsides?
Thanks again for sharing your theories and experience.
Concerning MAF314. My usual first step is to see what has been published on it via PubMed — and there is not a single peer review article or study. There is a summary on non-published studies at http://www.cheneyclinic.com/gcmaf-studies-presented-at-iacfsme-meetings-in-ottawa/833 There are 40+ studies on GcMAF (http://www.ncbi.nlm.nih.gov/pubmed/?term=GcMAF ).
The mechanism is tied to Vitamin D. Vitamin 1,25D goes sky-high with CFS and other auto-immune diseases (regardless of regular Vitamin D levels). A high(top end of the normal range) Vitamin D level has been reported in many studies to reduce the level of symptoms for CFS. Once an effective treatment is started, I expect 1,25D levels to start dropping. My went from over 125 to normal range in 3 months. When it hit normal, I was fully recovered per CDC definition. I was at the high end of the Vitamin D range during this entire period. A certain person’s belief that you should drop Vitamin D levels is not subscribed to by me.
My hypothesis is that MAF314 is likely most effective when Vitamin D levels are at the top of the normal range, and thus getting Vitamin D to that point FIRST is likely the most cost efficient approach. To get there may mean 20,000 IU/day for some people for several months.
In my experience it is possible to take much more IU per day. In the patient information leaflet of dekristol (Germany) is written, you can take up to 200,000 IU on day one.
In my case I took 100,000 IU on the first three days. I survived 🙂
A few years back I read everything about Vitamin D overdosages that I could find and it was actually very hard to do (especially if you are older and thus do not absorb supplements as well). My memory is that it took very large dosages for 9 months…
Good question. Even though i am consistently a 4+ on ecoli via genova cdsa? Or is that a poor illustration of all the species of ecoli?
The chart above shows the scientist view of what testing can provide. I refrain from recommending commercial tests because they give a very incomplete picture. On the flip side, if the condition has lasted for a long time, the microbiota may have shifted elsewhere. I know of a CFS patient with IBS that end up with a Crohn’s Diagnosis (and symptoms). Crohns is 95% invasive E.Coli. She is recovering well (and fast) from alternating between Mutaflor (E.Coli Nissle 1917) and a rotating assortment of herbs (Fireweed, Ashwanganda, etc) that kills E.Coli. She recently had her first cup of coffee in 2 years.
Thanks Ken, I’m looking forward to future posts.
Re biofilms: What are the protocols for removing them before or during this treatment?
There are two cheap supplements that are both effective against biofilms: NAC and EDTA. A week on one, a week on the other, with anti-bacterial herbs and spices starting in the second week. Neem and Haritaki were very effective in creating a Herx
This study on Pubmed may be of interest. If I recall correctly, Ken has shielded his house against EMFs. And yet I wonder about his exposure while working for Amazon.
Zh Mikrobiol Epidemiol Immunobiol. 2012 Jan-Feb;(1):49-54.
[Study of the state of parietal microflora and wall of the large intestine of mice under the influence of anomalous magnetic field].
[Article in Russian]
Medvedeva OA, Kalutskiĭ PV, Besedin AV, Zhiliaeva LV, Ostap EV, Ivanov AV, Medvedeva SK.
Abstract
AIM:
Study the possible qualitative and quantitative changes of microbial community of the parietal mucin of the large intestine and the state of the wall of the large intestine in experimental animals underbackground and anomalous influence of geomagnetic field.
MATERIALS AND METHODS:
CBA mice were put under the influence of anomalous magnetic field comparable to its intensity in Zheleznogorsk (3 Oe) for 1 and 2 weeks. Quantitative and qualitative study of mucous microflora of the large intestine of the mice was performed by bacteriological method. Identification of the microorganisms was performed by microbiological analyzer “Multiskan-Ascent” and commercial test-systems “Lachema-Czech Republic”: ENTHEROtest-16, STAPHYtest-16, Streptotest-16, En-COCCUStest-16; for lactobacilli and bifidobacteria identification – API 50 CHL (bioMerieux). Bacteria content in 1 g of material was calculated by the number of microorganism colonies grown.
RESULTS:
A pattern of changes of mucous microflora of the intestine and the state of the wall of the large intestine of the experimental animals that had been put under the influence of anomalous magnetic field is shown. During evaluation of qualitative and quantitative diversity of microbial community of parietal mucin of the large intestine of the mice under the influence of magnetic field on the background and anomalous levels changes not only in quantity and frequency of detection of obligate, transitory flora but also cell elements of mucous membrane of the wall of the large intestine were established.
CONCLUSION:
The results of the study allow to make a conclusion about the presence of reactivity of the parietal microflora of the intestine of the mice to the influence of the anomalous magnetic field. This leads to changes in cell elements in the mucous membrane of the wall that manifest by infiltration of the connective tissue stroma by leucocytes and reconstruction of epithelium, that are features of dysbiosis.
PMID: 22442971 [PubMed – indexed for MEDLINE]
http://www.ncbi.nlm.nih.gov/pubmed/22442971
My view is that many things can be part of the regime supporting the dysfunctional microbiome. Most of the items in isolation may not be the cause, rather, it is a combination of several factors. The classic case would be an illness with stress. Per Berg’s research, an additional factor is an inherited or acquired coagulation factor.
Just as several factors must come together to put you into this state, remission may also take several factors to happen at the same time. For example, both appropriate probiotics with the appropriate food for those probiotics to thrive (which may be different than your usual diet). I will be covering some of these factors in posts over the next few weeks.
I’m certainly glad someone in our community is following this and has the brain power to keep up with it. Thank you!
As for my own experience, I gave up eating sugar years ago. And when I got gluten out of my diet–which was amazingly difficult, given all the things it is hidden in–I had almost a month’s reprieve from symptoms. It was heaven. But then, without reintroducing it, the symptoms came back. I tried a dairy-free diet–a big sacrifice!–for a week, but I didn’t notice any change at all, so I went back to half-and-half in my coffee. I’m still off of gluten, and I know I would be much more ill if I was eating sugar and gluten, but I am still ill enough to have to spend most of each day flat on my back with a heating pad under me. I take PB-8 probiotics, but I can’t say that I notice much difference if I don’t take them.
I’ll be watching for updates. A little hope is a good thing. A necessary thing. Thank you.
So Sarah,, how much of a reprieve did you have when you first got the gluten out of your system?
Its almost like your body shifted to health and then shifted back again. I remember reading that Toni Bernhardt had, I think, 5 successful treatment approaches that worked for a good amount of time (month or so) and then failed…
Some blogs focusing on gluten sensitivity are coming up by the way..There’s more to it than I ever thought.
My observations and experience is that there trend to be such a quickening that you are running up and down the walls. The gotcha is that often this reprise from CFS disappear in a few days or weeks. I believe the reprise ends because other dysfunctional bacteria grows into the vacuum created.
Hence the alteration between killing bacteria and supplementing bacteria. To quote the New Testament, you cast out a demon from the house, the house is empty and seven more demons move in to take it’s place. Matthew 12:45, Luke 11:26 — not preaching, just referring to an applicable piece of our literary heritage.
I’m also glad someone is keeping up with all of this! I feel like the only person here who understands the overall idea but can’t grasp any of the details! I can’t keep up with all the posts and info., although I appreciate what I do read.
Like Sarah, over the years I’ve tried just about every diet there is. I have cut out dairy, meats, egg, you name it. After seeing Dr. Cheney many years ago (can no longer afford him but wonder what he’s up to..) I went on a serious elimination diet. Even 20 years ago he was a proponent of gut permeability and its influence with/on CFS. I felt better when I was on a basically vegan diet. But it didn’t cure me or cause any substantial difference.
I used to have IBS. No more. I don’t know why. I eat very little refined sugar but haven’t given up fruit. As it is, I am so fatigued that I eat whatever I can. Trying to follow anything very complicated is just too difficult. I’ve had brief remissions over the years–once after a series of chiropractic treatments. Once, for an unknown reason.
I’ve taken few antibiotics in my life. I never had the ‘flu until I was 28 and then I never really got over it! That was in 1976. But the symptoms didn’t become disabling until 1992.
I’ve just started the B1 treatment and am taking 600 mg/day. Will up dose tomorrow. No effect yet. (3 days). I tested very low on Vit. D and take supplements. Vit D is now normal. Feel the same. My internist is open to my thoughts/ideas but he knows very little about CFS or fibro.
I can get out of bed and basically take care of myself, which I couldn’t do some years ago so there is hope. I have fewer diverse symptoms, no headaches, overall pain is probably less.
Hi Theresa, first time I’ve visited this web site and I just saw your post of 15th July. This is the first time ever that I have posted or replied on any site. While I was reading your comments it occurred to me something you might not know about. Apparently a fair number of people have what can be a serious issue with folic acid. Blood tests won’t show the problem. Due to a genetic defect in a particular enzyme that converts folic acid to its usable form most of the folic acid that is taken in via the diet or as supplements cannot be used by the body. This for some people has devastating consequences. It’s not a folic acid deficiency problem but rather a conversion problem. Fortunately it is possible to obtain folic acid as a supplement in the form that the body can use directly without needing to be converted. This form of folic acid is methylated folic acid commonly known as methylfolate. If this is something you need to take there is a very good case for taking the methylated form of vitamin b12 along with the methylfolate. If you google MTHFR polymorphisms you can read lots more about the genetic problem. If this is new to you it might be worth investigating.
hope this helps, Sean
Hi Theresa, just noticed your post of 15th July. hope this helps if you don’t already know about it. a fair number of people have what can be a serious problem with folic acid. Not a deficiency issue but more a conversion issue. The folic acid that we take in via our diet or as supplements cannot be used directly by the body but has to be converted to the “body ready” form or usable form by an enzyme in the body. Research in recent years is revealing that quite a few people have a genetic defect with this enzyme and consequently are converting folic acid at a very low level with devastating consequences. If this is something that might help you it is now possible to get folic acid in the form that the body can use directly without needing to be converted. This is the methylated form of folic acid called methylfolate. If this is to help you you would need to take b12 in the methylated form also. Normal blood tests won’t show up this problem. A test for MTHFR Polymorphisms would reveal if there is a problem with this particular enzyme.
hope this helps, good luck, Sean
There is a catch-22 on folate. Microbiome and DNA appear to be both inherited. They is also evidence to suggest that DNA impacts the microbiome that persists. A recent study found:
“bifidobacteria folate content and composition is dynamic, is strain specific and depends on the medium. Suitable selection of the growth conditions can result in high levels of folate per cell unit biomass.”
The potential of bifidobacteria as a source of natural folate. D’Aimmo MR, Mattarelli P, Biavati B, Carlsson NG, Andlid T. J Appl Microbiol. 2012 May;112(5):975-84. Epub 2012 Mar 7.
Another 2012 paper ties folate issues to E.Coli levels. We know from Australian studies that E.Coli is low in CFS patients. “The deficiencies in folate biosynthesis were due to an aroD mutation, or treatment of E. coli with sulfa drugs, which are mimics of the folate precursor para-aminobenzoic acid. This study suggests that pharmacological manipulation of the gut microbiome folate status may be a viable approach to slow animal aging, and raises questions about folate supplementation.” Folate status of gut microbiome affects Caenorhabditis elegans lifespan.
I had been feeling so very defeated physically and when I was put on the gluten and dairy free diet just a couple of weeks ago, not even that long, I am already feeling stronger most of the time. I’m waking up earlier and awakening more refreshed and feeling the need to get up right away. It hasn’t been this way for years. I quit taking sleeping pills four years ago and was just sleeping on my own, but mostly for 10-14 hours a night. Way too much!!!
I needed to lose weight and I am now on these restrictions but my energy levels have increased. I see the doc again next week. She is thinking about doing the b12 injections, perhaps, she also put me on abilify, an antidepressant booster which seems to be working in conjunction with the revised diet.
I am also staying away from sugar a lot. I had a small candy bar one day and for a day afterward quite a bit of sinus drainage in the back of the throat again. I’m hoping my mast cell issues can be resolved soon too. It would be heavenly not having to scratch the itch in twenty places all over my body including my scalp. Still, life is good and I’m thankful for you guys…………..
Hello Mr. Lassesen,
What about heavy metals — they can mess up many organs, mess up the immune system, including the adrenals, can’t they? Can they interfere with the gut flora as well?
Also, I’m curious how you obtained the Mutaflor if you’re a U.S. resident (I’m assuming)? Do you have cousins or family in Canada?
Yes, heavy metals can impact gut flora, however, the odds are against them being the cause because they will likely flow thru. An example on the impact of zinc, http://www.ncbi.nlm.nih.gov/pubmed/22851657
Yes, I am a US Resident and Citizen, however I do have friends and family living in Canada which have been willing to take delivery. I then drive up and pick the shipments up.
Thanks for all this wonderful info!
Can you share a brand or two of L. Rheuteri?
I’ve been looking & can’t find any.
This is so incredible. I am so thankful to have found your site!
I have been finding my way along toward the gut microbiome as being the source of my illness, and with this new information, I have a lot more to look into.
Years ago I had a stool test that showed no detectable e. coli. I knew that couldn’t be good … but I didn’t know what to do about it. I was aware of a specific e. coli strain used in Germany but didn’t know it was available under the name of Mutaflor.
I have been holding out for the fecal transplant once it is made available for CFS/Fibro patients and was dismayed to read the comment here that it made one person worse.
I so appreciate your putting this all together, Ken. It has saved me countless hours and probably many more months of time.
Can I link this page to the Healing Well forum? I’ve been posting there about the gut and its relationship to Fibromyalgia and think there are people who are unaware of your web site but would benefit from this information.
Yes, please link freely to this page, or to my own blog at http://cfsremission.wordpress.com/