



The Future of Pain Relief in Fibromyalgia (and ME/CFS)?
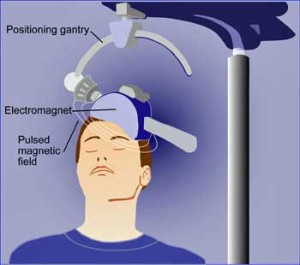
Someone sits in a chair with a coil pressed against the side of their head. Aside from odd tapping sounds they feel nothing. Sometimes they fall asleep. After about 30 minutes, they get up and resume their day; their pain much diminished. No drugs are needed. Could this be the future of pain relief in fibromyalgia?
A powerful magnetic field has been changing the electrical currents in their brain. If everything has gone as planned, the activity in parts of their brains that have been causing pain have been turned down (or parts of the brain that reduce pain have been turned on).
That is the idea behind the use of repetitive transcranial magnetic stimulation (rTMS), a magnetic therapy being pursued in disorders ranging from fibromyalgia to Alzheimer’s to multiple sclerosis to schizophrenia.
Prior fibromyalgia rTMS studies have had some success, but this one is different. Earlier rTMS studies affected the superficial parts of the brain, but this one – using new equipment able to reach deeper in the brain – attempted to increase the activity of a part of the deep brain (anterior cingulate cortex) that has been implicated in fibromyalgia (and chronic fatigue syndrome). Reduced activity in the anterior cingulate cortex correlates with reduced activity in the nervous system circuits that inhibit the production of pain.
Working out of their ‘Brain Stimulation Laboratory’, these South Carolina researchers tried to turn those pain inhibiting circuits back on.
The Study
First healthy volunteers and fibromyalgia patients were put in acute pain (using capsaicin solution), and ‘zapped’ with low frequency rTMS’ (I HZ) to see if rTMS reduced acute, short term pain. Then the FM patients were zapped with higher frequency (10 HZ) rTMS for 30 minutes a day for 20 sessions over a month to determine rTMS effectiveness at reducing chronic pain.
Results
“In addition, the effect on fibromyalgia pain was persistent for at least 4 weeks following treatment, indicating the induction of a neuroplastic, and potentially disease modifying, event.” Tzabazis et. al.
The milder TMS (1 Hz) temporarily cut out the pain in the healthy controls, but the FM patients needed something stronger. Cranking the rTMS unit up to 10 HZ and then ‘zapping’ them 20 days over 3 month resulted, according to one self-report measure, with a sixty percent reduction in pain. Significant improvements in Fibromyalgia Impact Scores, however, were not reported.
Rather astonishingly, the pain reductions remained strong four weeks after the study ended with the FM patients still reporting almost 60% reductions in pain.
While longer-follow ups in FM have not been done, the effects may be lasting for some. In some depression trials rTMS series repeats occurred every 6-12 months. The duration of response to rTMS is highly variable, however, and other patients require more frequent repeats.
Shake Out Period
“The capacity to differentially target specific structures deep within the brain may suggest numerous additional applications for this relatively new but fast evolving treatment approach of rTMS” Tzabazis et. al.
The high frequency rTMS we saw in the study increases brain activity, but low frequency rTMS can depress brain activity. Two earlier TMS studies suggested that turning down prefrontal cortex activity could reduce pain and improve mood in FM, as well.
Animal experiments in the 1970’s indicating that repetitive stimulation of neurons could change their long-term functioning set the stage for rTMS. The ability to change neuronal is called ‘neuroplasticity’; in effect rTMS is trying to reverse negative neuroplastic changes and induce new ones

As researchers better delineate which parts of the brain are under or over-activated in FM/ME/CFS, rTMS effectiveness should improve.
With the advent of deeper reaching rTMS machines, much of the brain appears open for tweaking. Any under or overactivated part of the brain could potentially be reset by rTMS. Clinician target areas of the prefrontal cortex with reduced activity in depression, for instance . Thus far, the machine has helped Parkinson’s patients move better, people with depression elevate their mood and people with stroke recover better. rTMS machines have been able to restore working memory – a key problem in ME/CFS – to normal levels in bipolar patients.
Even patients with treatment resistant depression can respond well. One study suggested 50% respond well and 1/3rd fully recover. One person with 30 years of depression reported :”I feel like the person I used to be 30 years ago! I’ve got my brain back”.
With the rTMS field expanding rapidly, it will take some time to understand the limits of this technology. A recent review of five rTMS FM studies found different parts of the brain (prefrontal cortex, motor cortex, now anterior cingulate) being targeted . In general rTMS appears to be at least as effective as opioids at relieving pain, has fewer side effects and is considerably more expensive.
Cost and Time
rTMS is not cheap. According to one source a typical session is about $300 and the recommended series of sessions topping of between 6-$10,000. Dr. Clauw, however, reported at the Ottawa IACFS/ME Conference that the rTMS machine is not particularly expensive ($25K) and suggested a series of sessions would run about 2K.
A newer technology called transcranial brain stimulation (TBS) that takes 1-7 minutes to work instead of the 20-40 minutes rTMS could reduce costs significantly.
Conclusions
rTMS appears to be effective at reducing pain for some people with FM, and, since some of the same brain regions are affected in ME/CFS, it may be effective there as well. (Check out Jess’s blog to see how painful ME/CFS can be.)
As brain imaging studies produce a clearer picture of which parts of the brain are over or under-activated in FM/ME/CFS, rTMS should become more effective at reducing pain and fatigue. Newer technologies that work more quickly may reduce costs. New approaches such as doing multiple sessions in a day may be able to improve effectiveness and drive down costs.
We know FM drugs often have underwhelming results, that mind/body therapies are a help but not cure, and that many people with FM/ME/CFS have exhausted their treatment options. Approved for treatment resistant depression, rTMS may be, if you can afford it, a good option for treatment resistant fibromyalgia and perhaps ME/CFS as well.






Excellent reporting Cort. So great that new methods of treatment are on the horizon….
Interesting . . . .
I just read Jess blog too. He summed it up nicely. I do have FMS and EDS (Ehlers Danlos). The FMS DX came first – so I question whether it is FMS or if EDS has been the problem the whole time. Or maybe it’s both. 🙂 But, pain is something that I know well. When a person has EDS and laxity of connective tissue – they have to contract their muscles pretty much all the time to keep themselves held together and upright. Because of this, it is causes a lot of muscle fatigue and pain. EDS people get osteoarthritis at a very young age.
I have always been one to try to find more natural, alternative type things to address whatever I’m dealing with and there have been some herbals that I use daily that greatly have helped. (Turmeric, Ginger, Astaxanthin) But, I have to use a pain med and muscle relaxer at night in order to get out of pain enough to sleep. (Tramadol, Bentyl) (I’ve talked about this before and how I’m able to keep my amounts low and not build a tolerance.)
But, this would be something nice – if it would help with pain signaling. I wonder if lying on a magnetic pad would do the same thing? I know of people that lie on magnetic sheets and say that it helps their pain. I’ve tried that and it overstimulated my sympathetic system. Was too energizing and I couldn’t tolerate it. But, when I broke my back – one of the things my osteopath used was a magnet over the area to bring more blood to it and to help with pain —and it for sure made a difference. So, would lying daily, on something with magnets in it – on our head, help? I think I’ll try it and find out. Now you’ve got my wheels turning. Something else to experiment with.
Thanks Cort!
Issie
What is the test that can tell you if you have EDS? I’m thin, have hypermobility and several other of the symptoms and just curious what the test is called.
Also, TMS seems to be a good option. Dr. Bradstreet uses it now as well.
You have to find a rheumatologist that is familiar with EDS – they are hard to find. First they need to determine the amount of flexibility that you have and then determine if they think you are just Hypermobile or have EDS. (There is question as to whether Hypermobile and EDS III is the same thing. Since this is the only form of EDS that can not be tested with genetics.) A lot will depend on what your presentation is. Then, depending on the type of EDS that they think you have, they will send you for genetic testing. Really, the only type of EDS that you need to know for definite sure that you have is the vascular type – as there can be aneurysms that could rupture and be deadly. Since there really is nothing that can be done for it, and it is genetically inherited —question is —do you need to have the genetic testing to know for sure. Would that make a difference in the scheme of things? If you haven’t had children yet – might be something good to know for sure. If you think there is the type that can cause rupture of vessels and/or organs – would be a good thing to know. Otherwise, it’s addressed with PT – keeping muscles as strong as possible to hold joints in place – bracing, if needed – and pain maskers. I find that keeping inflammation down is a big help too.
Issie
Something else great for pain is taking enzymes between meals. Here’s an article that tells why this is of benefit. If you look up enzymes – there are many different kinds and each type is used for breaking down different things – when they are used for digestion. When used between meals – things that cause inflammation are “eaten up” and eliminated.
http://doctorvolpe.com/chronic-fatigue/systemic-enzymes/
I thought about this tonight when I ate something that disagreed with me and also remembered this blog.
Breaking down fibrin is also one of the things done for protozoa problems – you try to get the immune system to work better and that is one of the things done. I use several types of enzymes. I’m to take lumbrokinase a few hours before I take either my antibiotic or anti-malarial herb. If you break down the bio-films then the enzymes can go in and destroy the pathogens, virus etc. that lives in the bio-films. Some people use serrapeptase or natokinase that is spoken of in this article – but, lumbrokinase is more potent.
Depending on what you’re trying to do with the enzymes is how you use them. I also have another one that has more types of enzymes that helps me more with pain. The one I use is by Integrative Therapeutics called Similase. I found that one doesn’t make my stomach burn and has all the things that will break down most types of food.
In Europe and also now in the USA Wobenzyme is one that is well known for inflammation.
http://www.wobenzymps.net/
Issie
Thanks Issie….its been a long, long time since I tried enzymes; it sounds like I should try them again 🙂
I’m definitely hypermobile, thin, stretchy skin etc but can’t touch my nose with my tongue which I here is a pretty definitive marker. Luckily I don’t have any joint pain.
I can’t do that!!!! There are so many different kinds of EDS and different things that can present for each kind.
Issie
you’re right. well i’m going for genetic testing in November so that should help clear up if I’m EDS or just hypermobile.
Dr. Teitelbaum suggested this cheaper alternative to rTMS
Jacob Teitelbaum, M.D. wrote: “TMS is promising for FMS pain , and also for depression. It is a bit pricier than it needs to be though. An option that it currently available, lower cost and perhaps even more effective for many kinds of pain seen in FMS, including severe neuropathic pain is Frequency Specific Microcurrent. See http://www.frequencyspecific.com/ for more info and for practitioners”
I have regular treatments of cranial osteopathy which i would imagine is similar although maybe not so deep into the brain but very effective. One treatment lasts about two weeks.
I hadn’t heard of rTMS treatment for ME. But my adult daughterhas had extraordinary success with it treating severe depression (which she has had for more than 20 years and it didn’t respond reliably to medication). After 6 weeks of rTMS at MacLean Hosptal in Boston, she is a new person…rational, resilient and equanimous even during a very challenging time. I can’t tell you what a huge difference it has made…and the recovery results are still striping now, 4 months after treatment stopped. The efficacy has me want to ask the doctors there if they’ve had any success with ME patients.
Hello I am just starting to look into rTMS. May I ask how the longer term results are with your daughter? I pray that she is doing well. Has she had any follow up sessions? Has her remission lasted? Any info you can provide would be so appreciated!!
Lisa
I just finished a series of 36 TMS treatments over 6 weeks for major depression disorder. Much to my surprise and delight, the depression is in remission (3 mos)! I also have fibro/ME. I can’t say it did anything for fibro/ME, but don’t know that the area of the brain that was stimulated was relevant for fibro/ME. But I’d sure like to see more research in this area. For me, the pain is mostly manageable with Cymbalta, lidocaine patches, & Gabapentin. However, I’m nearly bedridden & house bound due to the fatigue. Since TMS worked so well for a lifetime of depression with generally low side effects & cost (my copays were $50, total of $1,800) this area definitely needs more research & funding. If you’re suffering from depression, I highly recommend it!!!
Congratulations Carol and thanks for passing that on 🙂
Carol,
Congratulations on those results. May I ask how you are today? Are you still seeing results? Have you had any follow up treatments? I’m just learning about this and am so excited to hear more.
Lisa