

Pretty Graphs
Dr. Susan Vernon and Dr. Lucinda Bateman spoke in Denver on Saturday, June 28. Dr. Bateman gave a presentation on research out of the University of Utah she co-authored in her talk, “Treatment Options for ME/CFS and Fibromyalgia patients
I took two main points from her presentation. The first was her strong emphasis on using “pacing” to mitigate the “crash and burn cycle” which can be so damaging to ME/CFS patients (and a cycle that I cannot seem to avoid.) The second point I took regards gene expression studies that incorporate exercise to dramatically highlight subsets….which I am going to explore in this blog.
In her talk Dr. Bateman presented PowerPoint slides from the paper, “Gene expression alterations at baseline and following moderate exercise in patients with Chronic Fatigue Syndrome and Fibromyalgia Syndrome” that she co- authored with Dr. Light of the University of Utah, and can be found here.
This is not “new” research; this blog is a look back at a piece of research that affected me powerfully.
Dr. Bateman supplied the patients for this study. Dr. Light had them do moderate exercise on a stationary bike and then compared their gene expression profiles before, during and after exercise to those of healthy controls. They concentrated on three groups; people with fibromyalgia, people with fibromyalgia and ME/CFS, and a control group of healthy people.
An Orthostatically Intolerant Group Stands Out
They started with three groups but the results allowed them to separate the fibromyalgia and ME/CFS patient group into two additional subgroups. This blog is about one of those subgroups which had two unusual characteristics; the activity of one specific gene was decreased and 2/3rds of this group had orthostatic intolerance (POTS).
Kim McCleary, the former President of the CFIDS Association of America’ posted an excellent summary of this research. Here is Kim’s summary of that subgroup (emphasis added by me):
α-2A Decrease Subgroup (14/48 CFS subjects): The majority of this group (71%) also had clinical orthostatic intolerance (which) “suggests that different mechanisms cause the debilitating fatigue in this subgroup. The large decreases in α-2A may reflect a particular type of dysregulation of the sympathetic nervous system.” The researchers suggest that an effect of this dysregulation would be the “inadequate blood flow to the working muscles and the brain” that has been reported by other groups in some CFS subgroups. They state, “The relationship between α-2A decrease CFS patients and postural orthostatic tachycardia syndrome and the degree and type of autonomic disturbances needs further study.”
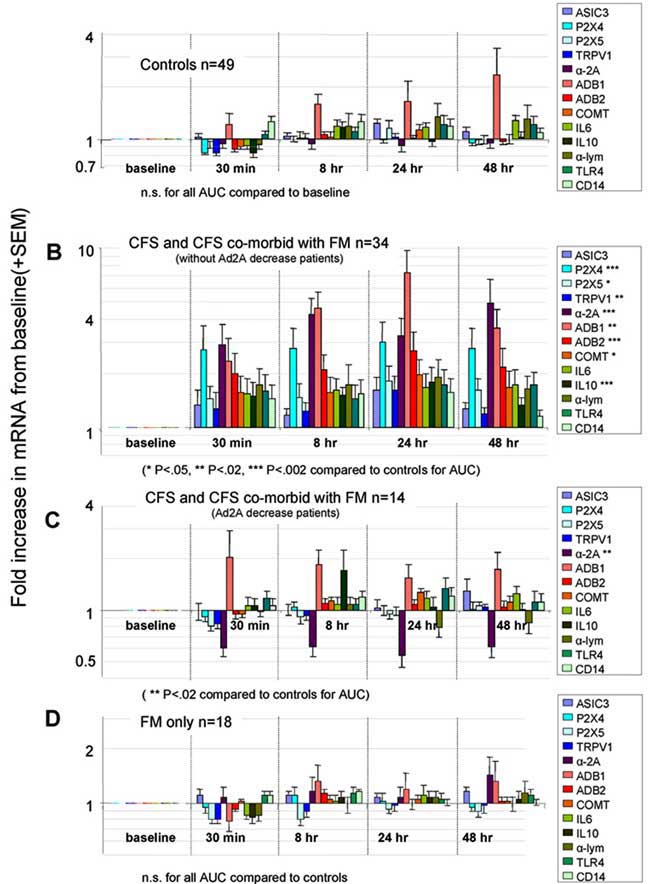
The radical difference in the gene expression results from the “orthostatic Intolerance” subgroup and the others can be seen in this stunning set of graphs below (The “orthostatic Intolerance” patient subgroup is set “C“).
Note how similar all the groups looked prior to exercise. During and after exercise gene expression skyrocketed in the biggest CFS/FM group, but only two genes really went out of whack after exercise in Group C. Decreased expression of the alpha-2a receptor gene (note the descending purple bars) during exercise was found in this group and only this group. That gene definitely did not kick in for that group during exercise.
I’ve always been fascinated by colorful charts and graphs maps, but this dramatic visual display of what may be going on in our bodies really stunned me. When this study was published I put a copy of the graph showing patient group A and B on my refrigerator.
For the next six months whenever somebody new came in my house and commented “What is this colorful graph?” I would take it and say, “Look! This is what is wrong with me when I exercise or perform some muscular exertion. This is why I feel like crap and crash for the next couple of days. Finally some researchers have shown why!” Of course, they would not really understand what is going on in these studies; hell, I barely comprehend it, but they can see the control group and they can see the patient group, and they can see the huge difference between normal people and the patient group.
The POTS Group?
This group was called the orthostatic intolerant group, but in fact they were really POTS patients. Dr. Bateman explained that their heart beat increased about 28 bpm when they stood up which is just under the accepted medical definition for POTS of a 30 beat per minute elevation, thus their use of the term, “orthostatic intolerance”.
The Adrenergic Alpha 2A Receptor
Before we get going on what the alpha 2A receptor does, we should understand what receptors do. Think of cells as listening devices primed to respond to changes in their environment and receptors as being their ‘antennae’. Once the receptor is triggered by a substance the cell goes into action…pumping out cytokines or hormones or whatever that receptor tells the cell to do.These researchers picked receptors they knew played a role in the exercise response.
In this case, the adrenergic alpha 2A receptor is being under-expressed; ie when the call came to assist in exercise the AA2a receptors did not pick it up.
A part of the alpha adrenergic 2A receptor that is under-activated in the orthostatically intolerant group
Found in both the central nervous system (including the brain) and the peripheral nervous system in the body, the adrenergic receptors and the neurons they’re associated with, impact many areas of the body. The alpha 2A receptors decrease sympathetic outflow and blood pressure, whereas the alpha 2B subtype increases blood pressure. Also, they regulate the inhibitory presynaptic feedback loop that controls neurotransmitter release from adrenergic nerves. The key point is that activation of these receptors inhibits the release of norepinephrine.
Since norepinephrine activates the sympathetic nervous system, the reduced alpha 2a receptor expression in the subgroup suggests norepinephrine levels and sympathetic nervous system activity are increased in the POTS group. Let’s see what effect that might have. From Wikipedia:
Norepinephrine is also used as a vasopressor medication (for example, brand name Levophed) for patients with critical hypotension. It is given intravenously and acts on both α1 and α2 adrenergic receptors to cause vasoconstriction. Its effects are often limited to the increasing of blood pressure through agonist activity on α1 and α2 receptors, and causing a resultant increase in peripheral vascular resistance.
They’re saying that norepinephrine can be given intravenously (with great care) to patients that have life-threatening low blood pressure to constrict the peripheral vascular system in order to increase the blood pressure in the arteries.
If you look on YouTube and find the video where Dr. Kenny De Meirleir talks about blood circulation and ME/CFS, you will hear him say that some of his patients have constriction of the peripheral vascular system because the larger blood vessels are dilated too much, or you can read Cort’s summary here.
Dr. DeMeirleir appears to suggest that blood vessels elsewhere are tightening up furiously in order to get blood to the brain. That scenario fits this subgroup of POTS patients with an over active sympathetic nervous system who are unable to stand without symptoms.
Here There and Everywhere
The sympathetic nervous system appears to be involved in multiple ways in ME/CFS. Try reading Cort’s blog suggesting that an overactive sympathetic system and peripheral system vascular dysfunction may be causing pain, or my recent blog on allodynia (a common symptom in fibromyalgia) which suggests that vasospasms in capillaries due to a dysfunctional autonomic system result in ischemia, reperfusion, and pain issues including allodynia.
A Clinically Definable Subgroup
So, we have a ME/CFS subgroup, some mounting research evidence, and two experienced clinicians, Dr. Bateman and Dr. Kenny De Meirleir, who appear to be finding the same issue in a subgroup of their patients. This is a subgroup of patients that any clinician can easily diagnose. The subgroup has three easily diagnosable characteristics;
- postexertional malaise
- muscular pain (perhaps allodynia)
- orthostatic intolerance.
Perhaps the most intriguing thing about this group is that it’s primarily defined right now by the declines in the expression of just one gene. That means this group, which may very well be the most debilitated one, is potentially the simplest to understand and the easiest to treat. It’s possible that a drug manufactured to target just that gene could pop that group right out of their exercise intolerance. Much more study, of course, is needed to validate that finding and check if other genes are involved. Another study is underway to do just that (see below.)
An Easily Diagnosable Patient Group. Is This Not What We Are Looking For?
This is not rocket science; we just need more experienced and educated clinicians. Orthostatic intolerance, after all, can be pretty easily measured with a simple heart monitor and doing a poor man’s tilt table test. Muscular pain and postexertional malaise can be easily determined from a quick patient interview and history.
Good luck on finding that medical doctor who will do this, though. Climb a mountain top and proclaim to all when you do find one.
The Clinician Deficit
I asked my “CFS/FM specialist” to distribute the notice of the presentation by Dr. Vernon and Dr. Bateman to her associates in the University of Colorado Healthcare system, which consists of hundreds, if not thousands of doctors and medical researchers. Did any of them show up? No. The room was full of families of patients and patients, and not a medical doctor to be seen anywhere, except for Dr. Bateman.
Dr. Bateman gave an enlightening presentation in Denver. I interrupted her at one point and asked her how many medical doctors had she given this presentation to? She squirmed and looked uncomfortable, but eventually said that she had not given this presentation to any medical doctors, yet. I understand that this is a new presentation and it was only the second time she had given it, but I got a strong feeling she was planning to give this presentation to only patient groups, not clinicians. As much as I loved learning what she had to present, you and I both know that the patients are probably far more educated about ME/CFS/FMS treatment as a group than clinicians.
My Recent Experience as Example
My symptoms meet the definition of the orthostatic intolerance subgroup Dr. Bateman’s study delineated. After searching and going through doctor after doctor for years (sound familiar?) I finally stumbled upon an experienced cardiologist who seemed worth a shot.
The cardiologist walked in, I told him about my orthostatic intolerance, cold extremities and showed him some heart monitor graphs. He listened carefully. He put a stethoscope to my heart and said that I had a mitral valve prolapse, which is commonly found people with low blood volume. He examined my medical chart and history, scratched his head in confusion at my medical history and then said this:
“You most likely have low blood volume, and possibly your large blood vessels are vasodilating causing your peripheral vessels to vasoconstrict. The first thing we will try to do is to raise your blood volume then once it appears to be near proper, we will see if we can try to get more blood to your peripheral vascular system.”
No fancy tests, no blood draws, no rocket science, just an experienced and caring physician.
We Need Clinicians Now
We need an ongoing system to develop knowledgeable and competent clinicians. I’ve heard Dr. Klimas and Dr. Bateman both state that they can significantly improve the quality of life of many of their patients. What if we had a system that multiplied the number of experienced clinicians by a few thousand?
Let’s suppose that all that orthostatically intolerant group identified in this study really needs is a drug targeting the activity of that one gene. If networks of ME/CFS knowledgeable physicians were available not only would patients would be more functional the day that drug became available, but a way of getting the word quickly out to them would already be in place. Otherwise, you are going to be back in that medical doctor’s office with a stack of papers about the Holy Grail Cure and trying to negotiate with him (or her) to take a look at this new information within the allocated 10-15 minutes you have with him.
We need one of the national organizations to put the time and money into educating clinicians now, not later.
Ongoing Research
The Lights are engaged in two studies that will further their findings. One expanded version of the study under discussion study will add 140 subjects to the 170 person database they already have. This study will involve full genomic arrays plus targeted genes (including some new ones) to see if ME/CFS patients can be differentiated from healthy controls, people with depression and cancer patients with fatigue during and exercise challenge. It’s due to end in August of next year.
Another study seeks to uncover how neurons on muscles detect and transmit signs of muscle fatigue to the central nervous system and how abnormalities in that system can produce excessive fatigue.









I still remember the uh’s and ah’s the audience emitted when Dr. Light presented his work at one of the IACFS/ME conferences.
Perhaps the most intriguing thing about Tim’s group is that it’s primarily defined right now by the declines in the expression of just one gene That means this group, which may very well be the most debilitated one, is potentially the simplest to understand, and the easiest to treat.. It’s possible that a drug manufactured to target just that gene could pop that group right out of their exercise intolerance. Much more study, of course, is needed to validate that finding and check if other genes are involved. Another study is underway to do just that.
This group may be the first one to find really effective treatments; to be really ‘treatable’. Time will tell. I’ve asked Dr. Light if he can give us an update on the study.
Please, how is this cardiologist expanding your blood volume?
My CFS “expert” didn’t even know about Phoenix Rising or Health Rising….my feeling is that they all should look for new jobs….I was always told that the 7 or 8 hours at work got you a “C” grade. It’s the extra hours you put in that makes you a standout….there should be a credential of sorts that requires all these people who say they have expertise to prove it….I know more about more of the recent research than every single doctor I’ve seen but one
Yes…I’m burnt out on all of them….
At the Simmmaron Roundtable Dr. Klimas proposed that a certificate in ME/CFS treatment be created. She now believes it would be better to try to extensively train some doctors (at least one in every community) instead to trying to educate the mass of doctors about how to treat this disorders. It’s just too complex a disorder.
There’s a CFS doc in Denver as well who, I’ve been told, has very limited knowledge…
Hey, y’all! Marcie Myers here. This issue is exactly what I directed my CFSAC phone testimony toward this past May when I discovered that not one single MD in the Primary Practice Clinic at the Medical College of Georgia Teaching Hospital and Clinics knew anything about CFS/ME. Furthermore, because it doesn’t fall under “scope of any specialty’s practice”, not a single specialist knew anything either. So my presumption that one would receive the correct diagnosis at MCG was totally incorrect and, though I am not able to access how many patients have received the ICD code for ME/CFS as a new diagnosis, I suspect the answer would be ZERO.
Soooo, I hope that no one is surprised when I tell you that I’ve discovered that CFS/ME has yet to be added to the curriculum for medical students ANYWHERE per Dr. Elizabeth Unger who is over chronic illnesses for the CDC. She stated via email and phone conversations that the CDC is “beta testing” small groups of students and hoped the curriculum would be completed by this fall. However, it must then be approved by the American Association of Medical Universities. Sigh. I met a junior and senior medical student last week and neither had heard of CFS before, much less ME. I gave them a crash course.
My hero is a Rheumatologist at Medical College of GA who is willing to allow me to teach her about CFS/ME. I have HHV6 so now I’ve gotta figure out what was said about having Quest Diagnostics Lab do a PCR test looking for ??ic or ciHHV6 using whole, not serum blood. Because, GOOD NEWS for about 30% of us, it would appear that Valcyte 450mg 2 tabs in am and 2 in pm for 3 weeks and then one tab twice daily for 3 months might just make that subset of patients well(er). Due to Herxheimer’s, or viral die-off with toxins released, you’re gonna feel much worse before you feel better and need liver monitoring. Hell, I could teach this!!!
The CDC does currently have m.e.u.’s for practicing MD’s about CFS/ME available on their website but I would have never known had Dr. Unger not told me directly. I haven’t bothered to see what they amount to either, oh me of such little faith as regards the CDC. I am currently pushing the Director of Quality Management AND the Chief Medical Officer over ALL practioners at Medical College of Georgia to at least mandate that the Primary Care MD’s know enough to consider the diagnosis when a new patient meeting the criteria (I know….whose criteria) would present themselves.
AND I wish that the CDC were not the only ones in charge of devising the curriculum for medical students. That Dr. Unger would turn to Dr. Klimas and the IACFSME and to others for input. People, I am but ONE person trying to change an institution here. I could sure use some help. EVERYBODY TURN TO CORT FOR THE ANSWER!!!!! Love ya, Cort!
Gotta say at this point that I agree with Dr. Nancy Klimas that teaching one MD in each area would be a far more efficient start. Then, each one, teach one.
renio, I agree Completely.. We need a certification program put in place Buy one of these nationwide Nonprofit organizations..
That might would tie the hands of other doctors that could possibly help with things – by only allowing those with the cert. to treat. But, if there was one specialized and could help to give seminars to other docs – that might be beneficial. But, not limit the treatment to just those with cert. It could also make the cost of treatment unaffordable to many, or the wait time could be forever. (Just me thinking out loud. 🙂 )
Issie
I am also interested in the protocol for increasing blood volume.
Thanks!
Sheajuli,
I suggest studying up on the subject by going to the DINET forum , or to The phoenix rising forum, “Autonomic, Cardiovascular, and Respiratory”….. make a post or do some research within the postings.
Finding the appropriate doctor to help so much, but it can be so hard.
INTERESTING!
Dr. Bateman is my sister’s doctor and it’s nice to know that she has found this gene and what it does in regards to exercise. Sadly, this does seem to be a genetic problem in our family. My sister has OI and CFS/FMS. All three of her kids have some form of dysautonomia – they think POTS. One was just DX’d with probable mast cell and celiac. And the doctors think that Ehlers Danlos (EDS) plays a part in it all too. As for me, I have this hard to treat type of Hyperadrenergic POTS with MCAS, EDS and lots of autoimmune problems. It would be nice to think that they could “tweak” this one gene and it make a difference with “all” these problems. But, I’m thinking there is more than one gene. This may affect our exercise intolerance and our getting overly sore and post malaise. But, I think it may be a little too hopeful to think it will affect all the things that this particular subset of POTS people deal with. I hope I’m wrong about that. Because, it would be a “miracle” if there was a “simple” solution. Most doctors consider this subset type of POTS to be the HARDEST to treat. (There’s so many drastic swings in symptoms. It’s hard to regulate low bp when there is also high bp.) There is also a problem with an over expression of noriepi (NE) and that does cause the veins to constrict (probably to try to get blood to where it needs to go), and it also probably has something to do with the tachycardia, that we have, to cause our hearts to desperately beat to try to get the blood to our heart and brain. (That’s why I question the wisdom in trying to supress this function —-when it probably is our bodies way of trying to compensate for dysfunction. Yes, it’s very – uncomfortable —but, is probably more important and necessary, in the long run for us, than trying to feel better because of the intensity this brings. That being said though, you wonder if it may long term hurt our hearts.) There is also a possibility that the NE isn’t being used properly in different areas of the body and there is an over release because of this dysfunction.
I have said for years that I feel overly vasoconstricted. Doctors try to give meds that cause more constriction of the veins. When I do those type meds —I feel a whole lot worse. I feel better with things that vasodilate my veins. But, there is a fine line how much you allow that to happen or there will be pooling. When you already have issues with connective tissue that can affect vascular integrity —you’ve got double problems. And when there is faulty distribution of your blood and you open up the channel – you may have more pooling. (There are lots of thoughts as to the dysfunction involved with this also. Is the blood too thick, are the veins not contracting properly because of dysfunction with them or is there a blockage inside the veins causing dysfunction of their ability to expand and contract. I could keep going with all the different ideas and thoughts as to why.)
Then to complicate the matters even more. There is a subset group of us with POTS that have low renin and aldosterone levels. This affects our fluid volume. It is thought that this subset group may have high angiotension II levels. But, if you look at the way this system works —-coming from the kidney level —that could not be possible in the chain of how this breaks down. If this group has high angiotension II levels —it has to be coming from a different place (it can also be from the heart and the liver). Unfortunately, this is only tested in research facilities and is not available for us to even know what our levels are. (At least that’s what my doctors have told me. And I haven’t had my angiotension levels checked.) I do however have low renin and aldosterone levels. What is done for a person with this combination is diuretics. This would be totally unacceptable in a POTS person who already seems to have low blood volume. (So, this wasn’t tried on my behalf.) But, because of the drastic swings in blood pressure that this particular subset type of POTS has – it is very damaging to your kidney function. I went into 3rd stage Chronic Kidney Disease. I’m still considerd hypovolemic by both the kidney doc and my neuro POTS doc. (I have however, reversed my Kidney disease to Stage 1 with my diet and other things I’m now doing with the help of a new doctor.)
Then you have autoimmune problems that a good many in this subset type have. There are autoantibodies to different things that are recently being found, to things connected to ACH (acetylcholine) and now antibodies to something found in the heart. There seems to be autoimmune illness connections. Many have MS type symptoms and some have positive Lupus findings. Yet at the same time –there can be hypogammaglobulinemia – which is a low immune system response to virus etc. So, you have both things going on at the same time.
I wish we would be able to find a doctor that could look at all the information that is out there. And then maybe listen to those of us that are researching and trying to put the puzzle pieces into place by compiling all the information that we gather from this study and that study and have it make sense. I’d be the first one on top of the mountain yelling the answer has been found. And for sure, if I find it —–I’ll be talking about it. I’ve got a whole family that has the problem and I’m the one in the family that enjoys research and TRIES to understands it. So, I’m searching not just for myself —but many others of my immediate family. And over the years, I’ve gotten close to some other lovely people searching for answers and we’ve become a sort of family —all searching for answers with a cause. At least, we’re not alone and we have others that understand. It get frustrating sometimes when we talk and others don’t understand. Even amongst ourselves we get irritated with each other and forget we are in the same boat together. (I’m guilty! And want to just STOP trying sometimes.) But, it’s going to take all of us to have a voice and keep trying to figure it out. The doctors are just too busy and there are not enough of them in this field and the few that are considered POTS doctors are even fewer.
Thanks for bringing this info to us Tim. I really enjoyed reading it. It came on a good day for me, as I over did it yesterday and can barely move today. POTS has come full force today and all the yuck that goes along with it. The exercise intolerance thing would sure be a nice one to sort out —-I think we’d all be happy about that one.
Issie
I agree Issie. It probably is our bodies way of trying to compensate for dysfunction. The evidence for this statement can be found in using Beta-blockers. If it was not compensation then beta-blockers would be more then helpfull but for many patiënts it makes them feel worse. Why we have low bloodvolume? This problem can explain everything. I do not understand why docters don’t search more.
Gigi, they are too busy trying to help those that so desperately need it. They are only able to put on the bandaids – not get to the core. There are so few researchers. We need more researchers and those that will dig deeper. I think those of us that enjoy research – maybe will be able to sort some things out. If we can connect the dots —that will be a big help.
Issie
I agree with you, Issie, that POTS is not easy to treat. I’ve been living with it for about 7 years and in spite of wearing a huge amount of abdominal and leg compression, drinking loads of Gatorade and/or salt water, I still have a great deal of chest pain and shortness of breath on exertion (I will say, though that the compression does help to avoid the very rapid heart rate; but it doesn’t fix the low BP).
I had a lightbulb moment when I watched Dr. Paul cheney’s March 2013 video series, in which he talks about the cardiac problems of ME patients. He is finding that ALL of his severely ill patients are in diastolic heart failure, and he believes that orthostatic intolerance is caused not by autonomic dysfunction, but by diastolic dysfunction. This would certainly make more sense, given how resistant OI is to treatment among those of us with ME/CFS. If we can’t fix the energy deficit that causes the diastolic dysfunction, how can we fix the OI? Perhaps some of the drugs that are out there might help somewhat, but we’re still left with the underlying problem.
One thing that helps me tolerate having to get up to use the commode is taking Sudafed first; it raises my blood pressure a little. I guess with your type of POTs (hi/lo BP) this might not be an option.
All the best to you and your family,
Christine M
Christine, all good questions. I too have diastolic dysfunction and slight valve leakages from all valves. I think part of that could be related to Ehlers Danlos and the laxness of the connective tissue.
I have found that I do better with abdominal compression than compression on my legs. There appears to be more splanchnic pooling for some of us. (It also helps to keep my ribs and back in place from EDS.) I occasionally wear leg compression – but, find that it will make neuropathy worse. With my blood vessels already appearing to be overly compressed – maybe, that’s why I don’t find the leg compression to be of a whole lot of help. I however, seldom have low blood pressures. If one has lower bp’s I think it might help to bring the bp up.
Believe it or not, some HyperPOTS people are finding Sudafed to be helpful. It wouldn’t make sense for a HyperPOTS person because NE levels are already too high. It increases NE. That brings in the question as to whether or not NE is not being uptaken properly and used in the body correctly. Taking Sudafed would increase the available amount and could lower the body having to supply a surge of an increase. Some of us have tried this and some have continued. Unfortunately, the body adjust to it very quickly. By the third day – many of us don’t get any benefit from it. I continued to take it for a week to just see if it would pick back up the benefits and it didn’t. However, I was pretty clear headed and felt like I could think better – so it maybe was helping with blood flow. The first day felt like a miracle. It was like everything was better. But, because of my weak kidneys – it was hard on them and I couldn’t continue experimenting with it. You can find several discussions on this at DINET.
For those that want a little more info on POTS, there is another blog that Cort has posted about NE. I’ve included some links to some videos that will give you a nice overview of the science involved and what POTS looks like for those that are fainters (we don’t all faint). Please read the comments on the DINET post, as some of the information was omitted from the video and some of it was not exactly correct. Here’s the link:
http://www.cortjohnson.org/blog/2013/07/23/animal-model-breakthrough-increases-our-understanding-of-pots-points-to-new-therapeutic-targets/
Issie
I was on procrit at one time until a black box was put on the medication. I also had to pay out of pocket because my hematocrit was not testing low enough years ago I had a radio active test do and it was able to determine I had low blood volume count
I have POTS too and am now getting treatment for it. The good thing is that there already are treatments available for orthostatic intolerance, so if you can see a doctor who has experience with OI, you can get treatment. Of course it would be perfect to be able to grab the problem by the root, but from what I’ve been told so far POTS can have different causes. So maybe the abnormal expression of that gene is not even the actual cause, but it’s just the body’s reaction to the cause, which might be an infection, autoimmunity or whatever. Or then it’s only one subgroup of POTS patients where that specific gene is the problem.
I think there are different ways to increase blood volume and one probably has to work with one’s doctor to find out what’s best in one’s case. What probably everybody with dysautonomic POTS gets told to do is to increase fluid intake and salt intake. And then POTS doctors also like to prescribe Florinef to increase blood volume. Some doctors also give IV saline.
Good luck with your treatment.
These are the things that most doctors tell POTS people to do. But, I’ve always questioned that as long term treatment. Most cardio docs tell one to not use a lot of salt as does kidney docs. Florinef is an adrenal hormone that causes the kidneys to retain salt. With the retention of salt – it makes the body hold onto fluid.
There is new research showing that too much salt can contribute to autoimmune disorders. If POTS already partially is connected to an autoimmune dysfunction – seems that would make things worse. We may be upping our blood volume – but, what else is it doing —long term?
__________________________________________
http://www.foxnews.com/health/2013/03/07/too-much-salt-may-trigger-autoimmune-diseases-studies-find/
___________________________________________
http://news.yale.edu/2013/03/06/yale-researchers-identify-salt-trigger-autoimmune-diseases
“Today, Western diets all have high salt content and that has led to increase in hypertension and perhaps autoimmune disease as well.”
“Nature did not want immune cells to become turned on in the pipeline, so perhaps blood salt levels are inhibitory.”
Hafler is not waiting with his own patients.
“I already recommend that my patients use a low-salt, low-fat diet,” he said
_________________________________________________________
So, there again —-I question treatments that are used.
Issie
Eric, so true. There are so many possible explanations for POTS. Since it’s a syndrome and so very complex – I’m with you with questioning one gene as the sole cause. Can’t believe that would be possible. But, I look at it as well, if that one gene is causing problems with exercise and there may be a way to affect it’s effects –then we are one step closer to discovering more genes that may be faulty and if we can do something about one gene —that gives more hope that we can do something with the others as they are discovered. I do believe that a lot of the dysfunction is genetic related. We are probably pre-disposed to things and a faulty immune system and inflammation doesn’t help things.
(Are you the Eric that I know from the other forums?)
Issie
I have the high bp POTS. Dr. Klimas is treating it with .02 Clonidine Patch, electrolyte drinks and water. Hydrate, hydrate, hydrate, it helps a lot. Heat still gives me trouble but I am going outside for up to an hour now and it is hot. I hydrate before and during the time I am out.
I have allodynia at times if that is when the skin is sore. It comes and goes, at times I feel perfectly fine and others not. I could never stand to be in a hot tub or whirlpool, now I know why. I mean years before I became sick. I thought that odd since everyone else loved that.
Yes, it sounds reasonable to me to train one doc. My GP is of help but he has other illnesses to treat as well. I am not sure how many ME/CFS people he has but I know he has them and Cort’s blogs are always welcome
Clonidine slows the heart rate down and stops a lot of the tachy. I took it for a few months and hold it in reserve. I needed a break from the constant and my bp was all over the place. It regulated those drastic swings and that hasn’t come back. But, because it slows the heart down – I started having problems with edema. It was hard to determine if it was my kidneys or heart as it appeared similar to congestive heart failure. I got off the clonidine and that got better. For me, it is one that I will cycle – if needed. I got tired of being tired. It made me so lethargic. Sometimes if my bp gets really high – I take 1/4 of one and it will bring things down and I don’t have to take them all the time. Also, this is one med. that is okay for those with mast cell disorders. Beta Blockers cause mast cells to degranulate and will cause an episode.
Issie
I was diagnosed with Orthostatic Intolerance by Dr. Lapp years ago after a long tilt table test, but mine was called Neurally Mediated Hypotension. As I understand it, my BP didn’t shoot up, my heart rate did. Does this gene research only include those with POTS or did it include those with NMH?
If your heart rate shot up it you had POTS; if your blood pressure tanked you had NMH. Both are found in ME/CFS with POTS being more common. I assume some people in the study did have NMH but the POTS group was more prevalent. You may have ended up in group B….
I’m sorry, I remembered it wrong. It was my blood pressure that plummeted. It was in 1998 and I don’t think it’s as bad now. I stopped taking salt tabs years ago. Thanks for the correction.
But what about the non-POTS OI patients? I don’t have POTS but neurally mediated hypotension. My HR doesn’t rise on standing–my systolic BP drops. Did they consider these patients in this study?
For me strattera (a norepinephrine reuptake inhibitor) virtually took care of my OI symptoms. But, I didn’t want to take it long term, my OI improved, so I no longer take it. But strattera has worked for a subset of OI patients. Wonder how this fits in?
sushi,
You can watch her lecture on the Internet, Elsewhere within these comments the link has been posted. I think they only considered patients with heart rate elevation upon standing, and whose blood pressure stays stable.
as Dr. Bateman said, a subgroup.
Strattera upped your NE levels and since NE vasoconstricts your veins it may have helped with your bp because of that. That’s one way to up blood pressure and help with blood flow – to vasoconstrict the veins. That’s why some are using midodrine, it vasoconstricts your veins. But, uses alpha-adrenoreceptors. Sudafed does a similar thing and ups NE. That’s why I wonder if there isn’t some sort of dysfunction in the way our bodies use and regulate NE and if it’s getting to where it needs to in order to help us.
Issie
High doses of propranolol (dr Lights’ ‘less is more’ didn’t work for me), iron supplements and a high daily intake of mineral waters have significantly alleviated my tachycardia, POTS and PEM.
Some people are finding coconut water to be a big help. It will balance out electrolytes without all the salt. It’s high in potassium. Also, since you are saying that iron makes a difference for you. I’ve found that Black Strap Molasses is a big help with tachy. It is high in potassium and iron. It’s amazing how well it works.
My other go to for tachy is Motherwort. Works within about 20 min. and is great for calming that “jump out of your skin” feeling.
Issie
Hi Cort,
Thanks again for an excellent post. I’m in the POTS cohort. No drug treatment just hydration. I have MVP and blood pressure is low normal. I hope that the further studies will lead to epigenetic treatment options. It’s really exciting! I donate to Simmaron, is there anyone else we should be donating to?
Emily, some of us are trying to tweak our genetic dysfunctions and having some good success with what we are doing. Epigenetics is up and coming. Science is advancing. But, for now we can do a lot ourselves to turn things around. (I’ve written about this before and won’t repeat that.) There are some really good blogs here and they point to things that can be done to somewhat correct some things that may be genetic. I know you’re on DINET too and you can do a search over there on the subject – lots has been written on that in relationship to POTS.
MVP is pretty common with POTS. I have it very slight and also have diastolic dysfunction. Have you been checked for EDS? This can go along with EDS.
http://www.ncbi.nlm.nih.gov/pubmed/7237708
http://www.ncbi.nlm.nih.gov/pubmed/901093
Issie
thanks for all the replies. Dr. Bateman’s presentation is a very good start on creating a ME/CFS Certificate as suggested by Dr. Klimas at the Simmmaron Roundtable. When I wrote this, I did not know that Dr. Klimas proposed that a certificate in ME/CFS treatment be created and that she now believes it would be better to try to extensively train some doctors (at least one in every community) instead to trying to educate the mass of doctors about how to treat this disorders. It’s just too complex a disorder. I agree, I suspect most patients who have been around a while to agree with this.
There are certain monied organizations that could do this outside of the federal government route which is fraught with bureaucracy and other inefficiencies. The CAA is one …. They could put a call out for specially allocated donations for this purpose.
Chronic Fatigue Initiative Is another. They are self-funded by a very wealthy gentleman. My guess is they would have to change their mindset as that they are heavily focused on research.
This Simarron foundation would be a interesting one to take it on also. Since it’s driven by Dr. Peterson who appears to be a pretty pragmatic fellow, It might take shape pretty quickly.
All speculation, but I keep on remembering but Dr. Klimas says that many of her patients can be improved (functionally). It would be great to be able to pass on her knowledge, Dr. Peterson’s knowledge, Dr. Bateman’s knowledge, etc. onto other clinicians through a certification program. This is something that can be done now, it’s not waiting for any researched come in for any federal grants etc. It would improve patients lives. It would bring ME/CFS Much more into mainstream medicine acceptance. Your GPs could refer out to ME/CFS Certified Specialists.
Another note, thanks to Cort for his fine editing and contributions to this blog. The man is one-of-a-kind.
Dr, Bateman’s lecture in Denver can be viewed on the Rocky Mountain CFS/ME and FM Association’s Youtube channel here – http://www.youtube.com/user/RMCFAorg
And an excellent lecture it was. Dr. Bateman was enthusiastic and on the ball. Thanks Mike.
I enjoyed seeing this presentation. Thanks for the link.
Here’s a slide presentations of an earlier presentation that has similar graphs and you can see it closer. You can see the different markers that were tested and the results. (Keep hitting the forward button and the graphs build on themselves. Nice presentation.)
http://www.offerutah.org/Light%20PPT/Offer%20Presentation%202-3-2011.ppt
This is an older presentation but shows some genetic markers for CFS and has some interesting observations.
http://www.hhs.gov/advcomcfs/meetings/presentations/alan_light_20101012.pdf
Issie
mike,
thx!! I did not know it had been posted on the Internet. a must watch, in my book. Thanks to you guys for your work on filming and putting it up on the Internet.
This is an older study, but the problems at hand are as new and real as anything. I appreciate everyone commenting here. Vasoconstriction is an ever present problem in ME/CFS. Fibromyalgia also has an overwhelming co-occurrence of Raynaud’s and hypothyroidism lending to the ice-box body. That’s what I call it anyway. And yes, it isn’t as easy as 1 -2 -3 to treat. What helps one symptoms might cause a kaleidescope of others.
I wish there was a directory of cardiologists that knew how to treat such issues. In my own case, I have a large floppy vein in my left leg that has horrible reflux, but in my right leg the vein is extremely, abnormally tiny yet very efficient. i saw the vein doctor because of the perpetual swelling of my feet. I literally have to keep my legs elevated most of the day in order to be able to walk. I have always thought this were related to my vascular system in general. The evidence is there, I doubt very seriously I am alone in this as a ME/CFS and FM patient, but no one seems to know how to connect the dots.
If we had a registry of cardiologists that understand, those who really want to listen is more like it, many of us could at least have some of our symptoms addressed. I am an RN and still at a loss.
Celeste,
I sympathize with you. the DINET Forum is the closest thing I know to a registry and It is pretty hit or miss. I hit upon my cardiologist via random phone calling. I managed to get a nurse on the phone who had done postgraduate work on dysautonomia. She was into the subject. She gave me a couple good names and at least I have a cardiologist that is not clueless and who cares. Not that this cardiologist knows anything about ME/CFS or Fibromyalgia and the additional complications that that could cause.
I really have a hard time understanding why one of these national organizations does not put their money into training clinicians in “Best practices”.
I asked Dr. Light about the AA2A group and his ongoing work – this is what he wrote
“The larger study will not be finished until next year. We do have a smaller study on the effects of Lyrica on CFS patients with comorbid fibromyalgia that we are finishing the analysis of. Hopefully, we can begin to write the result of this up soon. Unfortunately, it was a small study, and has only a few of the AD2A decreasing patients in it, so we can’t make too much out whatever happened.
Given that these patients decrease their AD2A following exercise inappropriately, any drug targeting this gene would have to increase the expression in order to be effective, unless the lowered levels of expression actually reflect an abnormal increase in the protein for some reason. I know that Dr. Bateman has been treating some of these patients with either beta blockers or midodrine with some success, but these have been prescribed treatments and are not scientific studies that prove the effectiveness.”
Cort, can you find out what the medicine is that the one person with POTS is taking that seemed to “cure” her POTS? Of course, what will work for one may not work for another —so many different subset types. But, that’s got me curious. Is it a medicine that is already released and being used off-label or a new one in trial?
Issie
With all my past 10 years of suffering from cfs and consulting GPs and specialists, I realised that there are a few tests that must be carried out and if diagnosed they should be treated as soon as possible are: hemoglobin, vitamin d, calcium, vitamin b12, thorough hormonal, cortisol, thyroid, blood sugar and insulin resistence. Antidepressants, epileptic medicines (lyrica) better be avoided if possible as they numb nerves and senses but it must be consulted with the doctors first as in some cases Lyrica has helped in some patients.
Along with that, regular stretching, gradual exercises and keeping oneself busy with some possible activity will contribute to the healing process. Healthy diet will help in general well being and will help fight against infectious and life long diseases. In my case herbal treatment, homeopathy, acupuncture, chiropractice, osteopathy nothing worked