



![]()
More Medical Maneuvers
Even after the not-so-successful chronic fatigue doctors, alternative doctors, and Lyme Literate doctors, and as other health issues arose, my Odyssey continued.
Dr. Beatrix Roemheld-Hamm, internist in a family practice associated with Robert Wood Johnson Hospital in New Brunswick, NJ
For a long time I refused to seek any more weird and wondrous treatments
My friend Rona raved about Dr. Hamm, the mother of two of my former students, and since I needed a good ol’ regular local doctor, I paid her a visit. A tall, beautiful woman with long dark hair, pink lipstick, and a hint of a Germanic accent, she understands holistic medicine and sometimes prescribes herbal supplements, communicating by email and web conferences with other similar practitioners.

I think she also teaches at the University of Medicine and Dentistry of New Jersey.
For a long time I refused to seek any more weird and wondrous treatments. I had improved enough to enjoy a life of sorts: movies, plays, book club, a Rutgers football game, restaurants, very light housework, carefully managed cooking (It took me all day to make a turkey loaf: dice and sauté onions in morning; mince and add garlic after lunch; assemble other ingredients after nap; mix all together and bake around 5pm.) But even with that nap after lunch I too frequently had to push through an impending crash or just stop dead in my tracks and collapse. Sometimes, however, I would actually recover from a crash if I rested and ate something, so that instead of sprawling on the couch in bone-crushing pain and fatigue, I’d just feel more normally tired, and even bounce back the next day.
Clearly, however, I was still a sick person, and Dr. Hamm suggested I might consider that I had a “leaky gut”, a “syndrome” that even has its own website (leakygut.co.uk) which says:

Dr. Hamm suggested that Carol’s gut, by leaking substances in her blood, might be sparking sparking inflammation and causing fatigue.
“The official definition of Leaky Gut Syndrome is an increase in permeability of the intestinal mucosa to luminal macromolecules, antigens, and toxins associated with inflammatory degenerative and/ or atrophic mucosa or lining.Put more simply, large spaces develop between the cells of the gut wall allowing bacteria, toxins and food to leak into the bloodstream.”
On his website, Dr. Andrew Weil agrees:
“Leaky gut syndrome is not generally recognized by conventional physicians, but evidence is accumulating that it is a real condition that affects the lining of the intestines. The theory is that leaky gut syndrome (also called increased intestinal permeability), is the result of damage to the intestinal lining, making it less able to protect the internal environment as well as to filter needed nutrients and other biological substances. As a consequence, some bacteria and their toxins, incompletely digested proteins and fats, and waste not normally absorbed may “leak” out of the intestines into the blood stream.”
Dr. Hamm suggested that I might improve if my body were absorbing more necessary nutrients, and recommended her colleague from med school, Dr. Kate Thomsen, who focuses on women’s health, including nutritional and digestive issues. She is board certified in Family Medicine, has a Masters in Public Health, and is an assistant clinical professor at Robert Wood Johnson Medical School. She runs clinics, publishes newsletters, and gives presentations. She spends a lot of time with each patient. She is very expensive. She does not take Medicare.
At the time of Dr. Hamm’s recommendation, however, I wanted NO treatment, NO new doctors, NO new pills. Time off. I let the information settle for a few months, and by the end of 2008 I was ready to investigate.
***
Dr. Kathleen Thomsen, Pennington, NJ, “Integrative & Holistic Health and Wellness” for Women
So down Route 1 I drove for almost an hour, to the office of Dr. Thomsen, which was attached to her ranch-style home and contained large, soft, cozy brown leather chairs and sofa, two very friendly staff members, one efficient and competent nurse, and Dr. Thomsen’s beloved dog Silky. This adorable silver terrier yaps at new arrivals and then scurries around the waiting room. Then she sits at your feet in the doctor’s office.
Dr. Kate, as her staff calls her, looks late-fortyish. Attractive with short brown hair, friendly eyes and a beautiful smile, she seems to come from sturdy Scandanavian stock, but that’s just my guess. When I conjure her face I see dimples, but maybe because her personality has dimples. She is good humored, knowledgeable, willing to explain anything, and thorough. She schedules a big block of time for each patient, listens carefully to your history and symptoms and takes notes on her computer of everything a patient says. And then at the end of each session, she gives you a printed list of her diagnoses and recommendations and a big hug.

Carol new diet restricted what she could eat, and the rotation diet didn’t work out but, at the end, she felt better.
So. Back to lab work: very expensive food allergy blood tests, a comprehensive digestive stool analysis, celiac disease tests, hepatic function tests, Vitamin D tests, breath tests for bacterial overgrowth.
Like many chronic fatigue sufferers and antibiotic guzzlers I had leaky gut and yeast all over the place.
Treatment: Nystatin and certain herbs for yeast, very expensive supplements, probiotics, and a diet that was as difficult to execute as the Marshall Protocol or Dr. Gonzalez’s’ brutal regimens. No bread. No sugar. No fruit juice, coffee, tea, melons, mushrooms, cheese, processed food, peanuts and pistachios, alcohol, ketchup, mustard, soy sauce, pickles, vinegar, mayonnaise, smoked meat, dried fruit.
I also had to avoid various foods to which test showed I was allergic: eggs, milk, almonds, lentils, avocado, asparagus, soybeans, tomatoes, lettuce, pumpkins, garlic, and even peas. PEAS?
But it got worse. Because the strong recommendation is to maintain a 4-day rotation diet which means you should not eat any particular food any more often than every 4 days! Can you imagine? I went bonkers for about a week, trying to find foods I could eat and arrange menus, churning inside from all this decision making with a foggy brain.
Then I pulled in the reins. No way. I will just do what I can. Which meant scrapping the whole rotation thing and avoiding as much as I could the forbidden foods. That was sorta manageable.
I saw Dr. Kate for about 3 years. My last visit was about a year ago. I still take probiotics, some of the supplements, and try to avoid many of the proscribed foods, though I cheat more than initially. At book club meetings I put lox on my bagel; in a restaurant I’ll eat the mushrooms in the sauce.

Carol did pretty well on her diet..until the breads of France proved to be a temptation she couldn’t resist…and was happy not to..
The baddest I’ve been was during that trip to France for the wedding of the son of good friends (who was also a beloved former student of mine). I totally flipped and threw all my former caution into the French wind, tearing thick pieces off crusty loaves and stuffing them into my mouth, along with slabs of all kinds of cheeses. Every day. Many times a day.
When I took my little stool sample in my little plastic bag to Dr. Thomsen on my next visit, it was swarming with yeast. But I hereby declare IT WAS TOTALLY WORTH IT. I am unrepentant and would do it again.
Did the treatment help? I felt stronger. I went to France. We’ve spent five winters in Tucson, Arizona and just bought our own home there. I’ve visited my sons who’ve moved to Los Angeles and went on an Elder Hostel trip to the Berkshires with friends. And as I said, for a long time I engaged in more activities during the day. I slept better. I rebounded from crashes more readily.
***
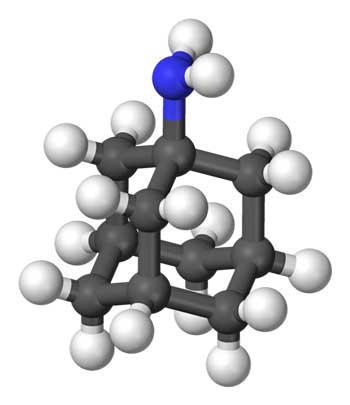
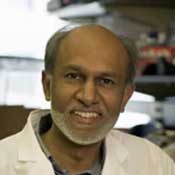
Enter Dr. Avindra Nath, Professor of Neurology and Neuroscience Director, Division of Neuroimmunology and Neurological Infections, Johns Hopkins Medical School, Baltimore, Maryland
Then he asked how I was doing on Amantadine. I told him why I wasn’t taking it. Oops.
One day in 2009, Alexandra, another beloved former student, visited with her husband, Dan, and adorable toddler Sam. Dan was a doctor/researcher who worked at Johns Hopkins in neurology. In the course of our conversation, Dan mentioned Dr. Nath and his expertise. Since other doctors had called my CFS symptoms neurological, since the Lyme Disease diagnosis and high HHV-6 titers indicated an infection, and since, as is clear from these pages, I leave no stone unturned, I thought a trip to Johns Hopkins was warranted. Maybe this man would offer an important perspective.
Twice Steve drove me to and from Baltimore.
The first time, we sat in the waiting room for over 45 minutes. Finally the very distinguished Dr. Nath, gray haired and darkly handsome, appeared and called us into his office. He listened and took notes on his computer.
First, he prescribed Amantadine, a drug more commonly used to treat symptoms of Parkinson’s Disease, but found to improve fatigue and muscle stiffness in Chronic Fatigue. He also wanted me to have another (#4) brain MRI and (#3) Spect Scan of the brain. I hated those tests because of the accompanying injections of gadolinium, a heavy metal contrast dye, for the MRI, and a small amount of a radioisotope for the spect scan.
Coaxing a vein in my arm to cooperate and lie still is always difficult and frequently quite painful, and the possibility of a bad reaction always frightens me. But what’s the point in seeing this exquisitely trained doctor if I’m not going to do what he needs in order to help me?
He wrote in a report that my symptoms might be due to an autoimmune response in reaction to the flu shot, and recommended getting “ANA titers, rheumatoid factor, anti-Ro, anti-La, anti-thyroglobulin and anti-peroxidase antibodies. . .In addition, if not already done, she should also have a serum protein electrophoresis and immune electrophoresis.”
More medical terms that make me cross-eyed.
First thing I googled amantadine, and found that “common serious side effects” can include dizziness, trouble sleeping, nausea, depression, anxiety, hallucinations, low blood pressure, and agitation (http://parkinsons-disease.emedtv.com/amantadine/amantadine-side-effects.html).
With Amantadine’s side-effects mirroring many of Carol’s symptoms, Amantadine did not appear to be a good option
About.com says: “anecdotal success in ME/CFS is not supported by studies.” I’d struggled for years to overcome depression and anxiety; I have chronic low blood pressure; I finally don’t have sleeping problems; I’m already dizzy when I crash; and there’s no scientific support. Why, oh why, would I take this medicine? So I never filled the prescription.
I suppose I had all the blood work; I don’t recall. The imaging tests were typically dreadful, with the arm poking and pinching, and the banging noise of the MRI and the long wait after the radioactive injection. Whatever. I did what I was told.
Six months later I returned to Johns Hopkins and the eminent Dr. Nath. This time we waited over an hour. When Dr. Nath appeared, he was followed by three or four groupies, young residents lapping up his every word.
Dr. Nath reviewed his computer notes. He asked for the MRI and Spect Scan results, since they weren’t there. I explained that the imaging centers had sent them to him. He denied it. Then he said, “Where are the pictures? I want to see the pictures.”
No one, nowhere, had ever suggested that I needed to bring him the actual pictures. Wouldn’t it be reasonable to expect to be told something as important as that. . . . especially when I’m driving over 3 hours each way to see this specialist? So he was perturbed at me about that.

Adolph Bunswanger actually wrote about neurasthenia in the 1800’s but Dr. Nath’s assertion, based on her MRI, that Carol had Bunswangers’s disease did not pan out.
Then he asked how I was doing on Amantadine. I told him why I wasn’t taking it. Oops. Again he seemed annoyed. He abruptly stood up and walked out to another office, where, apparently, he found the MRI report from University Radiology and the Spect Scan report from Columbia Presbyterian Medical Center. Here’s pretty much what he said to me, in a mechanical, unemotional voice, as the young residents simultaneously nodded like bobbleheads:
“According to the MRI, you have white matter lesions on your brain. This indicates you probably have serious cholesterol problems. You should check your cholesterol with your doctor and probably take a statin. As a result of the white matter, I’d say you have Binswanger’s Disease, which can cause memory loss and symptoms like Alzheimers. You can see your internist about these issues. One doctor you don’t have to see anymore is me.”
I looked and him; I looked at Steve; I looked at the smiling young residents. “I don’t know what to say. I don’t know what to ask,” I mumbled. I think I asked if he were positive, if it were as serious as it sounded. Steve too stood dumbfounded, not only by the content of his words but also by his dismissive, who-cares tone.
We left.
Here’s what The Cleveland Clinic’s website says about Binswanger’s Disease:
Binswanger’s disease (BD), also called subcortical vascular dementia, is a type of dementia caused by widespread, microscopic areas of damage to the deep layers of white matter in the brain. . . The symptoms associated with BD are related to the disruption of subcortical neural circuits that control what neuroscientists call executive cognitive functioning: short-term memory, organization, mood, the regulation of attention, the ability to act or make decisions, and appropriate behavior. . .Other symptoms include forgetfulness (but not as severe as the forgetfulness of Alzheimer’s disease), changes in speech, an unsteady gait, clumsiness or frequent falls, changes in personality or mood (most likely in the form of apathy, irritability, and depression), and urinary symptoms that aren’t caused by urological disease.
What the fuck?
I had hoped for some new and possibly fruitful perspective on my illness and had no clue what to do with this information except worry. I had never come across anything mentioning Binswanger’s Disease in all the material I’d read about CFS/ME. Was this another instance proving my doctor-phobic mother-in-law’s theory that the more medical tests you have, the more they’ll find, results that probably mean nothing and that you would have been much better off not knowing about?
Of course, I took this to Dr. Hamm, my internist. Blood tests showed good cholesterol levels. She, along with other doctors, have totally pooh-poohed the diagnosis. Yet, when I find myself standing in front of the refrigerator wondering what I’m looking for, and when I can’t remember the name of the Netflix movie I watched the night before, and when I find my keys in the front door lock, I quickly subdue that momentary flash of panic. I suppose I should see another neurologist, but who knows on what kind of journey that would lead me?
***
The Unexpected Aftermath of a Colonoscopy by Dr. Debra R. Goldstein, Division of Gastroenterology and Hepatology, Saint Peter’s University Hospital, New Brunswick, NJ.
Just a routine procedure I’ve had at least 5 times before. We of a certain age know how the colonoscopy itself is a breeze, while the prep the night before is gross and sickening, whether you have to drink the gallons of battery acid or just take a few Ducolax pills and drink some fizzy stuff. You’re sitting on the toilet all night. For past colonoscopies, I’ve had to throw out a few pajama bottoms when I didn’t make it to the bathroom in time.
The latest preparation, however, resulted in massive cramps, for which Dr. Goldstein, my new gastroenterolgist, had to prescribe special pills after I called her office in agony, as well as a few periods of wild nausea and dizziness. By the next morning I was completely drained.
That was a Monday night. The procedure itself went fine and I had no polyps to be removed. By Tuesday night, however, I was back in bed, in the midst of as bad a crash as I’d ever experienced in the past few years of my illness. Weakness, muscle pains, headaches, brain fog, even some nausea. After a few weeks, I began to wonder if this long downturn heralded the beginning of a serious relapse, one that would erase the progress I’d made over the last few years of semi-recovery, and I went back to Dr. Hamm.

After a colonoscopy provokes a severe relapse, Carol goes back on her gluten and other food restricted diet
She blamed the preparation for the colonoscopy. “When you clear out all fecal matter from the intestines, you also rid your body of all bacteria, good and bad. I’ve seen this happen pretty frequently with my patients and it takes a long time for them to recover.”
“Yeah,” I said. “But I’ve had colonoscopies before, even after I got sick, and never had this happen afterwards.”
“I don’t know why it happened now and not before. But your immune system is weak to begin with, and there’s a strong link between your gut and your immune system. When the prep destroys your bacterial flora, your immune system is weakened even further.”
Dr. Hamm seemed pretty confident with this diagnosis, and recommended I take certain supplements to restore the balance to my gut flora: probiotics, kombucha, glutamine, zinc and a bunch of pre-biotics (aka Fructo-oligosaccharides). Also, I should maintain a gluten and dairy free diet until I improved. So off I went again, into the wild blue yonder, with yet another restrictive diet and unpronounceable pills and powders. And yes, after a few weeks, my system seemed to re-balance and return to its normal-abnormal state.
In December, 2011, after the whole XMRV uproar, I decided that I really should see someone else with CFS/ME expertise and so I chose the clinic in Miami, where the prominent researcher Dr. Nancy Klimas sees patients. And so, she and now Dr. Irma Rey are the latest and, so far, the last on this doctor list.
They’re up next…
Find more of Carol’s blogs on her search for health with chronic fatigue syndrome here.






When I get muscle cramps at night, I know my magnesium level is way to low. Remember, the cheap magnesium OXIDE will only make you poop, for some not a bad thing, if that’s what you need, but for everything else, you need magnesium ASPARTATE, on a daily basis, 12 to 16 hundred mg per day, divided. We all need magnesium, along with a good multi-mineral supplement. ten four
I read last year that we may have a malic acid defienciency, so started taking Mg Malate. Should I take the Mg Aspartate as well?
Carole- All of this so very close to home.. I had almost the same experience with the Colonoscopy. However I hemmoraged afterward and they had taken out a 18cm Polyp, Sissal
Serrated, Adenoma. Many times Malignant. Said they got everything. Gastro said was one of the largest he had taken out. That was a year ago. I went back in last lweek and he said the the risk now were not worth the benefits as I am having
Heart palpitations. Pathologist said needed to be repeated in a year last time as these are flat tumors. Colon has to be blown up to see all of the Polyp. I also had the cramping and horrible pain. Having Cardiac problem. Better now on CPAP machine and mask.
My main concern now is I just had a very close friend who Emory University here in Atlanta has been seeing for Cardiac problems. She went in for ck up-seeing them all the time
and they found she had Pancreatic Cancer.
She died 28 days later. NO ONE WAS CHECKING HER FOR ANYTHING BUT CARDIAC. THIS COULD HAVE BEEN CAUGHT WITH BLOOD TESTS AND ULTRASOUND.SHE ALSO HAD CFIDS ????
I am very dishear
tened about all of this. To me the CFIDS is TUNNEL VISION and no one is looking for other diseases. I also have White Matter Disease and Ifarcts. These have not changed for 3 years with an MRI. I am not having any dye or fluid put into my brain to ck for anything else. My God -We are allergic to everything anyway. My thinking is fuzzy enough.
My best to you Carol. However I emplore you to ck out other avenues. I have seen the best Chronic Fatigue Dr. I am no better. In fact the last one I saw for cardiac only made me sicker.
SEE AN INFECTIOUS DISEASE DR. I AM. my best Carole
Yes, it’s easy to miss other conditions because we tend to assume their symptoms are from ME/CFS. And it also happens that treatment for those other conditions can make us sicker. Seems like we can’t win.
I have seen a few infectious disease specialists.
I guess it’s a good thing we no longer have health insurance~at least they can’t experiment on me anymore~they want to send you to a specialist for every thing~got tired of having my thyroid poked, and the bad reactions to so many meds.I’m sticking to what my online nutritionist says~which starts with getting the gut healthy…He recommends oxytocin, (for the neurotransmitter issues, I think)~which he says few Dr’s will have heard of as the research is rather new. Has anyone heard of that?
I am also at the point where I am very careful about what tests I will go along with and what specialists I will see. I supplement with quite a few hormones and that has improved my quality of life enough for me, for right now anyway. Oxytocin is one of the hormones I have tried and use occasionally. You are right MK Gilbert when you say most docs will not be aware of the treatment. I find oxytocin to be a “feel good” hormone. It seems to boost endorphins and helps with libido. My doc uses under the tongue troches, but I have been using the injectable liquid I got from another doc. There is a nice book available on Amazon that discusses oxytocin. My current doc uses oxytocin in his fibro patients with success.
But by far the most influential hormone I take is hydrocortisone. Without it, I was cleaning my bathrooms in stages and pushing laundry baskets with my feet. With HC, I can live a reasonable quality of life.
Yes, I first heard of Oxytocin 14 years ago when I first became ill. My doctor prescribed it, I think. Or at least he talked to me about it; I can’t remember, now. Perhaps I took it for awhile, and didn’t notice any significant difference which is why I don’t remember. My doctor at that time was a primary care doctor who focused on Fibromyalgia.
Some of his treatments were pretty radical for that time, but, Oxytocin seems pretty harmless to me. It’s one of the “feel good” and “love” hormones. The body produces it when we feel good, for instance, when we are in love, give or receive a hug, etc. I had very low levels of all hormones which is why it came up in the first place.
I’ve never heard of used for CFS. It’s not like HRT therapy, not at all. In fact I’d take some Oxytocin if someone offered it to me. 🙂
My memory is hazy from 14 years ago, but I’ve heard of Oxytocin recently talked about by people who are quite knowledgeable about how the brain works and what happens when we feel good.
Rick Hanson is one person who comes to mind who mentions it. He has written many books about how the brain works in relation to being happy. We could all do with higher levels of Oxytocin in my humble opinion.
Good God what a mess the US medical system is in. A lot of these medical practitioners sound like a bunch of quacks, and must be laughing all the way to the bank.
None of this stuff works. Period. I can’t stand any more of these posts and will be unsubscribing to your blog.
Carol your trip to JH confirms why I didn’t take a referral to the “leading” CFS MD at Mass. General. I looked up the man….not one word of encouragement….all “holy speak”.
Your writing is so good!!!
God Bless,
Sara
AND….there are virtual colonoscopies. One clinic is in St. Petersburg, Fla. Even Katie Couric has recommended them. I’m so glad I read Carol’s account…have been feeling guilty that I’ve not had the test in a few years.
God Bless,
Sara
I’ve seen 6 Neurologists, all of them idiots incapable of compassion, much less the ability to come up with a competent differential and diagnostic plan. Haven’t had one actually make a diagnosis that withstood their tests. They all have their own agenda, if you don’t fit in their box, you’re dismissed, usually rudely!
I’ve come to believe there are so many Medical Schools (over 150) vs. Veterinary Schools(25) because they have to make room for all the assholes.
You should ask your primary to have a Board Certified Neurologist review your “Pictures”, with no given history, and get a second opinion.
Greg
Like a genius prof I once had said, many md’s think they’re gods~he was a pathologist and the county coroner. (I don’t know WHY he was teaching Anatomy/Physiology at a Jr College!!!~possibly because he was partially disabled?) A few humble Dr’s did ask him Q’s which he usually knew the answers to, and he was able to make class fun, bringing it down to our level~he exuded joy. I will never forget what he said about the MD’s: “They love to use the nomenclature of the orthography of their discipline to display their arrogant pomposity!” He was one of the best profs I ever had.
Hi Carol,
Thanks for sharing this with us. I really look forward to reading your stories, well written and sometimes funny, glad you still have your sense of humour !
Keep writing,
Lyn
Binswanger’s—never heard of it. My lesions, according to neurologist are due to migraines—-I have to keep reminding him that I’ve never had a migraine in my life. My internist and a new family practitiioner suggested small TIAs, which makes some sense because my father had them.
I was sad to read that someone above had given up. I have been ill for almost 10 years now. Yes sometimes I feel like giving up, but often I feel there’s still a chance because someone writes something that I’ve never heard of and I have another angle to pursue. Thanks, Carol.
Hi Carol,
I just wanted to say I love your blog. I am always awaiting the next installment. It totally speaks to me—we have so many similarities in our stories. I really appreciate that besides writing about all your health adventures you wrote about your marriage/spouse issues. So many people don’t talk about that part of it (if they are lucky enough to have a spouse to fight with and go through all the mayhem with). I’ve had so many treatment travails as well and drug/supplement trials. Some things have helped. My latest is UVB IV therapy. I call it my “get out of jail” treatment because for a week or so…sometimes two weeks … I get to feel like a “normal.” Like I’ve had a body transplant and see what its like to have energy and a brain and actually feel GOOD! That’s the good part, the bad being its expensive and it doesn’t last. But I got to be physically and mentally present for my daughter’s wedding recently and that was worth everything as I’m sure you can imagine.
Anyway please don’t stop writing. You should write a book. I love your humor and candor! I feel your pain. You are such a good writer. I mean you can actually write about this miserable illness and make me laugh. Hard to do–takes talent. Thanks for entertaining me as well as sharing your journey.
Glad you were able to enjoy your daughter’s wedding! I’ll have to look into UVB IV therapy. Never heard of it.
Carol,
I can relate so much to what you have written! I have been sick since 1990. I can’t even write the long hx of diagnosis, , tests, and treatments. I had to stop working as a school psychologist and go on disability. I did some clinical work but the last 2 years I have been very sick. On top of dx of Lyme, fibro, CFS, lupus, Sjogren’s, and who knows what else, I ended up in the hospital and dx with chronic ischemic colitis. I also have autonomic nervous system dysfunction which I truly believe is a big factor in my poor health, plus just dx with sensory ataxia neuropathy and hyperthyroidism. I too have white spots on my brain. Also thromboplihia–blood clotting problems, including factor v. And my neck is a mess with herniated discs and spinal stenosis and the neurosurgeon wants to do a spinal fusion. The pain is very bad in the neck. I am on so many medications and supplements. Been on prednisone for 18 years and can’t go off of it–I now have secondary adrenal insufficiency. I guess I needed to vent tonight! I do look forward to reading what you write!
Carol said:
“I totally flipped and threw all my former caution into the French wind, tearing thick pieces off crusty loaves and stuffing them into my mouth, along with slabs of all kinds of cheeses. Every day. Many times a day. When I took my little stool sample in my little plastic bag to Dr. Thomsen on my next visit, it was swarming with yeast. But I hereby declare IT WAS TOTALLY WORTH IT. I am unrepentant and would do it again.”
And you should. Although Dr. Hamm would probably drop dead at the suggestion, many docs are now realizing that if carbs and even sugar — yes sugar — are restricted too much, then candida or other fungal infections will just go looking elsewhere for ‘fuel’.
In other words, restricting carbs and sugar may actually create the leaky gut that one is trying to avoid in the first place.
Hi Carol,
I so enjoy reading your blog! I too have been fighting this monster for many, many years…since I was 45…just turned 70! I have tried everything you have and more…it all accomplished nothing…but I have to keep going…think if I didn’t I would have to just call it a day, and I can’t do that! I love your use of FUCK…it has become my very favorite expletive…really annoys my family…FUCK them!! Please keep writing…you make me laugh!!
ME/CFS started for me when I was 55 and now I’m 70 also. I wonder how aging alone affects the course of the disease.
Amantadine was first widely used as an antiviral, particularly for Influenza A. The National Health used to give it out before the psychiatrists dominated British thinking; an old colleague of mine was given some by her GP in London and found herself cured of CFS. Of course no proof it wasn’t coincidence. It is used by a lot of MS patients for their fatigue. I took it for a while for mecfs and it was helpful for a while, as for the MS patients. The underlying anti-fatigue mechanism is probably that it is dopaminergic. I have never hear of anyone actually having the listed reactions. I always thought it was pretty harmless. It is long since out of patent and quite cheap.
The multi-colored sea anemones crawling up the wall were kinda cute, but when the Grim Reaper decided to call in the middle of the night I decided that a hallucinogenic med was not my cup of tea.
Tell it like it is, girlfriend! Love it.
Hi Carol
This is a wonderful blog, and so well-written. If you ever get the energy, write the book! Thank you for taking the time to share your journey. In terms of diet, after years of making conditional changes, I think I am finally ready to surrender to necessity and follow the kind of radical exclusions the doc I’m working with has suggested. Your experience helps me see that while there are no absolutes, its got a be worth trying.
I felt very sad reading about the hideous and callous manner in which your brain results were passed on. My beautiful, funny and talented friend Nisha hung herself after a similar failure to pass on the results of while plaques in the brain in any context (the consult with the endo, the mental health team and whoever else she saw in her last weeks didn’t help any either). I think she felt the damage to her system was irreparable now. And the UK, she had plenty of professionals telling her that in effect she was a neurotic. She wasn’t, but the plaque thing really got to her. So glad you managed to survive the stupidity and cruelty of that doctor.
Big hug!
Sian,
I know you’ve seen Dr. Fry and from my own experience, following what he has told me to the tee –is making huge improvements for me. Treating the protozoa and addressing the immune system – with not only antibiotics, herbals and mainly diet —-is causing more improvements than anything I’ve done in years.
The times that I’ve “messed up” with my diet and had more fat than I should —there have been consequences to pay. It does seem to matter. Eliminating animal products has greatly reduced my inflammation and pain.
Issie
Thank You For All The Valuable Info.
I too suffer from CFS-Fibromyalgia. I am a Pharmacist practicing for the last 40+ years. I am still working Full Time.
I see how most MD’s fumble about trying to help. Most only just treat the Symptoms. We have to tell them what tests to run.Most won’t know what to do with the test results.
You have to be your own best MD if you can. I dispense all these Meds on a daily basis and see the results.