



(The text is by Dr. Rosamund Vallings of New Zealand. I added the commentary (in brackets) and headings.)
December 2013, Gold Coast, Australia.

The programme for the day began at Griffith University with the Opening Ceremony for the National Centre for Neuroimmunology and Emerging Diseases (NCNED). We were welcomed by Professor Sonya Marshall-Gradisnik, Co-director. She then introduced Professor Allan Cripps, Pro Vice Chancellor Health, Griffith University, who welcomed us, and he then introduced Dr. Elizabeth Unger (USA), who gave a brief opening address before they both unveiled the plaque.
Hugh Perry (Southampton, UK) – Alison Hunter Memorial Foundation address
Hugh Perry (Southampton, UK) gave the inaugural Alison Hunter Memorial Foundation address. However he began his address pointing out that neuro-immunology has a large role to play in the understanding and research associated with ME/CFS. He reiterated how much Christine Hunter (AMHF) had raised so much the awareness of the illness.
The first part of his talk explained the Medical Research Council (MRC) mission. The MRC has been established for 100 years. The mission is to encourage research, produce skilled researchers, disseminate knowledge and bring dialogue to the table. ME/CFS research has been supported since 2003. A strategy document was produced in 2008 – leading to an expert group incorporating external researchers for collaboration. The idea was to bring in new people, new research and new technologies.
One of the big challenges was the unmet clinical need (up to 600,000 sufferers in the UK). Grants were initially low as there was no clear pathology and no targeted therapies. Treatment has been geared towards support and symptom control. There is need to define phenotypes and sub-phenotypes and embrace new technology.
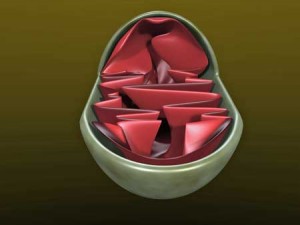
He then outlined a prioritization of topics for research: Autonomic dysfunction, cognitive symptoms, fatigue, immune dysregulation, pain and sleep. There is a need to bring in external expertise. In the medium term there is need to encompass comorbidity and chronicity, susceptibility and resilience, mitochondrial function, use of well characterized cohorts and development of intervention (e.g., cytokine inhibition). In the long term there should be development of imaging technologies, assessment of genetic risk and review of neurobiological changes (e.g., cerebral activity).
The MRC is currently funding new research looking into the mechanism of ME/CFS (1.6 million pounds). There needs to be partnership with new researchers to qualify for grants, and a focus on one of the 6 topics listed above.
So far the following awards have been made:
- Mitochondrial function
- Autonomic dysfunction
- Biological fingerprints of fatigue
- Slow-wave sleep and daytime function
- persistent fatigue induced by interferonα (a new model for ME/CFS).
The MRC role is to support excellent and innovative research. There is increased emphasis on translation, and increased commitment to develop research for application to new therapies. This needs a “bottom-up” researcher –led approach which led to the establishment of the UK ME/CFS Research collaborative launched in April 2013, associated with Dr Stephen Holgate.
This brings together funders and ME Charities. The MRC acts as an observer. The aim is to collaborate the ME charities and to increase awareness with the research community. The key to success is that research should drive the agenda, the “bottom-up” approach and the engagement of researchers outside the field. This has led to the First UK CMRC Research conference to be held in Bristol in September 2014.
[CJ – Check out the MRC rewards here. Prior to their more recent emphasis on physiology, the MRC focused on behavioral (e.g., PACE trial) and epidemiological studies.
The MRC’s research docket is not large, but it contains some fascinating studies. Below are overviews of a few of them.
The McCardle Mitochondria Study
“This … will lead to a definitive answer regarding a mitochondrial defect in muscles of patients with CFS.” McCardle
McCardle’s mitochondrial and cytokine skeletal muscle study is using techniques developed in her lab to test the hypothesis that mitochondrial abnormalities produce free radicals that initiate a state of low-level inflammation in ME/CFS. Free radical activation of the inflammatory mediator NF-kB produces pro-inflammatory cytokines that further dysregulate the mitochondria resulting in a vicious circle of more free radicals, more cytokines, etc. McCardle is very confident of her new approach, stating it will provide a ‘definitive answer’ (!) to the mitochondrial question that’s been dogging researchers for years in ME/CFS.
Dr. Julia Newton and the Autonomic Nervous System
“This programme will lay a foundation … that will enable a future set of diagnostic tools, system based explanations of dysfunction, a new generation of therapies and ultimately clinical protocols that will counter the biological processes that underpin fatigue in a range of diseases.” Dr. Newton
Dr. Newton’s study is equally exciting. Stating that it will also use ‘novel technologies’, Newton’s study will attempt to determine whether the autonomic nervous system issues in ME/CFS are driven by problems in the brain or the periphery. (Newton’s most recently published study suggested that pH handling problems in the muscle could be causing the reduced cerebral blood flow.)
The first part of the study will use “ground breaking dynamic magnetic resonance (MR) modalities” to examine brain functioning. The second part will determine how much cardiovascular dysfunction in the periphery contributes to the blood flow problems in the brain.
Using the Fatigue in Sjogren’s Syndrome to Understand the Immune Problems in ME/CFS – Ng
“By uncovering the abnormalities of the immune system in CFS in detail, it will help make the diagnosis of CFS easier and more accurate as well as give us clues to develop effective treatment of this condition.” Ng
Ng believes the fatigue in disease is primarily immune mediated and is driven by the same immune processes in different disorders. Since the definition of chronic fatigue syndrome is so nebulous and the patients so heterogeneous, he chose to use Sjogren’s Syndrome to get at the heart of immune mediated fatigue in chronic illness. Ng will use gene expression and markers of immune dysregulation from a group of 550 Sjogren’s Syndrome patients to produce a biological profile of immune induced fatigue. He will then look for that ‘biological signature’ or biomarker in people with ME/CFS.]
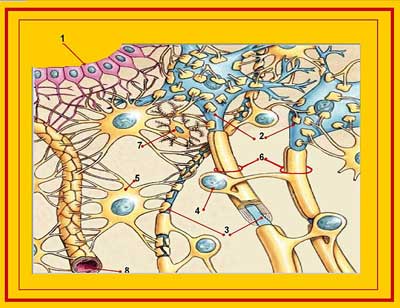
Perry Part II: Impact of Systemic Inflammation on the Brain
The second part of the address focused on the Impact of Systemic Inflammation on the Brain. He described how diseases “talk” to the brain, and how infection makes you feel “sick”. Inflammation changes behavior. These symptoms can be the same as those experienced by those with ME/CFS.
This highly organized strategy is critical to survival if living in the wild. Systemic inflammation activates selective brain regions. Infection causes a localized inflammatory response, with release of pro-inflammatory cytokines, which then communicate with the brain.
The cytokines act on the endothelial cells, which in turn affect the macrophages in the brain (microglia) – and microglia play a key role in immune/brain communication. This is tightly regulated by the brain/micro-environment.
The microglia may become dysregulated, escaping from CNS control, and this leads to massive pathology and symptoms equivalent to microglial activation. The activated microglia may proliferate, leading to neuro-degeneration. The microglia may be primed by decline (e.g., Alzheimer’s disease).
Macrophages are primed by exposure to ɣinterferon and then triggered by infection, which is the secondary stimulus. In a younger population the microglia can be primed by the environment – living in dirty conditions (animal model) predisposes the brain to give a more robust response to infection, which can lead to microglial activation for months.
Smoking and obesity lead to higher levels of cytokines and this in turn leads to more activation of the microglia as if a peripheral disease exists. Lifestyle, systemic infection and genetics all prime the microglia.
The final conclusion/hypothesis was that systemic infection and inflammation, that normally leads to sickness behavior in an individual with a healthy brain, is a homeostatic mechanism with no long term consequences, is distorted and maladaptive in an individual with primed microglia. The question is to find “inhibitors” to penetrate the brain and downregulate the microglia.
[CJ -The Japanese have presented two findings in conferences indicating microglial activation occurs in the thalamus of chronic fatigue syndrome patients. Perched on top of the brainstem deep inside the brain, the thalamus is the switchboard for sensory signals entering the brain. Every sensory signal (except for smell) is routed through the thalamus to different parts of the brain. A major regulator of sleep, awareness, arousal and wakefulness as well, the thalamus could certainly play a major role in ME/CFS. The Japanese findings suggest inflammation in present in the thalamus of people with ME/CFS.]Elena Gonzalez-Rey (Granada, Spain) – Cortostatin – A Possible Future Therapy for Chronic Fatigue Syndrome
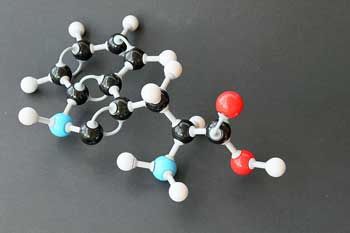
Elena Gonzalez-Rey (Granada, Spain) was the next presenter who addressed the issue of therapeutic and physiological relevance of cortistatin as a key molecule in the development and progression of inflammatory and autoimmune diseases. Cortistatin is a cyclic-neuropeptide produced by the brain cortex and immune cells, with unique function, that shows potent anti-inflammatory activity.
She reiterated that homeostasis leads to survival, and that immune homeostasis is protective. The immune system “talks” to the neuroendocrine system via cytokines and neuropeptides. The therapeutic effect of cortistatin gives a good response. She had looked at mouse models and found a good response in MS (EAE).
Cortistatin improves symptoms, reduces inflammatory response, inhibits demyelination, inhibits Th1/Th17 responses and induces regulatory T cells. It also induces the production of trophic factors, modulates the immune response of resident cells and protects against oxidative stress. Severe disease leads to decrease in cortistatin levels. Low cortistatin leads to anxiety and fear behaviours, affects neurogenic processes and induces cognitive problems. (article published in Arthritis and Rheumatism May 2013). This is a potential treatment for ME/CFS.
[CJ –Cortistatin is a relatively new discovery, and the first research papers on cortistatin date back only to 1999. Cortistatin is receiving a lot of interest, but animal studies dominate at this point and I was unable to find any cortistatin drugs trials listed in the clinicaltrials.gov database. Cortistatin is one of several neuropeptides being investigated as anti-inflammatories. These include substances such as vasoactive intestinal peptide, pituitary adenylate cyclase-activating polypeptide, alpha-melanocyte-stimulating hormone, urocortin, adrenomedullin, somatostatin, cortistatin, ghrelin, galanin and opioid peptides.]
Mario Delgado (Granada,Spain) – Vasoactive Intestinal Peptide – A Potential Therapy for ME/CFS?
The therapeutic potential of Vasoactive Intestinal Peptide (in auto-immunology) was discussed by Mario Delgado (Granada, Spain). VIP is widely distributed in the body, produced from many organs. It has a plethora of functions. It has been found to be a pleiotropic immunomodulatory factor with potential for use in inflammatory and auto-immune disorders. It is a key factor. Various auto-immune diseases have been studied. It has been found to reduce experimental auto-immune endocarditis in mice, decreases severity of EAE and restores immune tolerance. Questions asked were: Is VIP needed for a healthy immune system, is it ready for clinical use and could it play a role in ME/CFS?
Endogenous VIP and its signalling are critically involved in maintenance of immune tolerance. Clinical use of VIP (Aviptadil) includes treatment of erectile dysfunction, idiopathic pulmonary hypertension and acute systemic respiratory disease. Inhaled Aviptadil is used for alleviation of lung inflammation in sarcoidosis (Treg cells increase). A published article on ciguatera poisoning (Shoemaker May 2010) found that VIP was decreased leading to many symptoms. In another open label study, patients exposed to contaminated buildings had reduced symptoms with inhaled VIP treatment. Inflammation was corrected, Treg cells were normalized and there was enhanced quality of life in all patients. We need to look to see if VIP is decreased in ME/CFS and also whether a VIP infusion could be helpful.
[CJ – VIP is getting a lot of study everywhere (RA, IBS, epilepsy, high blood pressure, etc.) it seems, but not in ME/CFS. The NCNED did, however, present findings on VIP at a conference this year. Mast cell activation that triggered VIP (and Substance P) in a recent study of women with IBS was intriguing given the possibility that mast cells play a role in ME/CFS. The greatly increased level of the ciguatera epitope found in ME/CFS several years ago indicates a possible tie-in with VIP.]
Gilles Guillemin (Sydney, Australia) – Tryptophan Metabolism
Gilles Guillemin (Sydney, Australia) presented his work looking at the involvement of the tryptophan mechanism in neuro-inflammation. He explained that the kynurenine pathway is a major route of tryptophan catabolism resulting in the production of several neuro-active intermediates. Tryptophan is one of 20 amino acids and is diet sourced. It is a “calming” neurotransmitter and a sleep inducing hormone. The kynurenine pathway is induced during inflammatory brain diseases leading to tryptophan catabolism, and then production of various neuroactive metabolites , including quinolinic acid (QUIN.) This field of research is growing and there is now a Journal of Tryptophan Research. The foetus protects itself against rejection via this pathway.
An overactivated kyneurine pathway in the brain could result in neuroinflammation and an central nervous system excitation in fibromyalgia and ME/CFS
Human microglia and macrophages produce QUIN, which acutely can lead to neuronal death and chronically to neuronal dysfunction and neurotoxicity. Neuroinflammation can lead to suicidal ideology, (there may be an imbalance with elevated QUIN). QUIN can induce apoptosis in human primary astrocytes. It also induces oligodendrite apoptosis, and affects chemokine production and expression by astrocytes. It is not specific for any particular neurological diseases. The kynurenine pathway is activated and QUIN rises in neuroinflammation. QUIN also rises in various neurological diseases. This pathway is potentially modifiable, and may be a therapeutic option.
Richard Kwiatek (Adelaide, Australia) – Neuroimaging, Chronic Fatigue Syndrome, Depression and Anxiety: Similarities and Differences
Richard Kwiatek (Adelaide, Australia) has looked closely at neuroimaging to differentiate ME/CFS from anxiety and depression. He explained initially how ME/CFS still has not been scientifically validated, and appears to be a multi-system disorder. There has been hot debate over psychological issues. ME/CFS and fibromyalgia models are closely linked to those of regional pain syndrome and a number of psychiatric disorders.
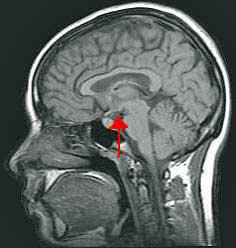
Kwiatek found differences between the brains of people with ME/CFS and people with anxiety and depression
Disturbed immunological, inflammatory, oxidative and stress pathways have overlapping symptoms. Ventricular lactate has been shown to be increased in ME/CFS compared to generalized anxiety disorder. Cortical levels of glutathione compared to ventricular lactate in depression, ME/CFS and controls found that glutathione correlates tightly with ME/CFS. There is a structural peripheral neuropathy in fibromyalgia patients.
He then discussed voxel based imaging, and had studied 25 ME/CFS patients compared to controls. Changes in forebrain white matter were noted in ME/CFS. The analysis was categorical and correlational. When the Bell score was down the disability was greater. When adjustment for depression was included, T1w signals corresponded to severity and T2w did not.
In ME/CFS, myelination in the prefrontal white matter correlated with severity. Kwiatek concluded that ME/CFS may share biological features with anxiety and depression, but present data suggests there appear to be 2 distinct disorders.
[CJ – Expecting there to be a sharp dichotomy between anxiety and depression and ME/CFS is probably unrealistic given the overlap in symptoms and how the body works. Maes has proposed that similar inflammatory factors underlie depression and ME/CFS (and he separates the two as well.). The fact that an ‘antidepressant’ can reduce depression in depressed patients who are not in pain, and pain in chronic pain patients who are not depressed, indicates that similar basic biological processes are in play in these two different disorders. Indeed, Kwiatek observes that “Disturbed immunological, inflammatory, oxidative and stress pathways have overlapping symptoms.”
Given that ME/CFS is, as Kwiatek notes, a multi-system disorder, it can be expected to overlap with many disorders. And, of course, it shares some characteristics with autoimmune disorders and cardiovascular disorders, yet it is distinct from them as well. ]
Sonya Marshall-Gradisnik (Gold Coast,Australia) – NCNED’s Research Direction
Sonya Marshall-Gradisnik (Gold Coast,Australia) opened the afternoon session and explained the current direction of the research at the National Centre for Neuroimmunology and Emerging Diseases (NCNED).
She outlined the research being undertaken by the various members of her team. She explained the importance of looking at the many changes occurring in the immune system and its cells. The NCNED will operate a clinic through which research projects will be undertaken. They will set up a national patient database, which eventually may become international. The search for biomarkers will continue. NK cells are consistantly depleted and cytokine studies are not consistent.
The projects currently undertaken include: looking at: neutrophils, ɣōT cells, Tregs, cytokines (not consistent over time in ME/CFS), CD+8T and microRNA, gene expression, NK receptor/gene (longitudinal – seem consistent over time),(9 different miRNAs found). They are now looking at CD107 as a marker of NK cell lysis – this may not actually be released by the cell, so what is the mechanism?
Plasmacytoid dendritic cells may contribute to the inflammatory response through the release of cytokines and chemokines, and activation of lymphocytes. Important new directions include: Redoing T cell subsets, looking at B cell subsets (immature B cells and memory B cells) and exploring microRNAs in key areas.
[CJ – Cytokines Not the Answer? – Note the two statements emphasizing that cytokine results are not consistent in ME/CFS, and that this research program includes cytokines but is mostly looking elsewhere. The infectious onset and the symptoms present in ME/CFS have suggested for over 30 years that cytokines must play a key role in this disorder, but outside of the Klimas/Fletcher lab the results have been variable. Perhaps the most intriguing cytokine finding came from the Dubbo studies suggesting that high cytokine levels early in an infection (but not later!) predicted who would come down with ME/CFS.
The NCNED group is mostly looking elsewhere and may be looking deeper into the immune system, in particular NK cells, than any other group.]
Several researchers from the department then presented their work.
Ekua Brenu (Gold Coast, Australia) – Immune System Overview
Ekua Brenu (Gold Coast, Australia) discussed the immune system in ME/CFS. Due to inconsistencies the exact immunological mechanism remains unknown.
- Reduced NK cell function worldwide is emerging as an important component. NK function declines further in these patients over time. There are reduced NK lytic proteins in ME/CFS (perforin, granzymeA and significant GranzymeB ). There is increased NK cell fragmentation and increased NK IFNɣ. The percentage of CD56+ and CD16- is down.
- Dendritic cell subsets: MDCs slightly up and PDCs down.
- Neutrophils: phagocytosis normal, but respiratory burst down. HNA’s variable with HNA2 down.
- B cells: Immature down and memory and plasma cells slightly elevated.
- T cell subsets focused on cytokine release. Longitudinal assessment was not consistent. Looking at T cell subsets: FoxP3 Tregs significantly elevated, CD39+T slightly elevated, CD73+T significantly elevated.
With CD8 lysis, NK activity and CD8 activity were significantly decreased. Molecular investigations identified significant decreases in MiRNAs that regulate cellular development and apoptosis.
Her conclusion was that there is reduced cytotoxic activity, compromised neutrophil function, increased T regs, irregular cell distribution and different expression of genes.
[CJ – NK cells are surely not the be all and end all of ME/CFS, but note how many different facets of NK cell dysfunction are found: reduced functioning (reduced killing capacity), high levels of ‘broken up’ or fragmented NK cells (because they’ve committed suicide (apoptosis)?), reduced types of NK cells, and, on a rather ominous note, the finding that NK cell functioning tends to decline over time.]
Sharni Hardcastle (Gold Coast, Australia) – Immunological Profile
Sharni Hardcastle (Gold Coast, Australia) outlined the immunological profile of ME/CFS.
She had examined innate immune cells. She explained that NK cells are protective and, in ME/CFS, show decreased cytotoxic activity. Exocytosis of perforin and granzymes leads to cell apoptosis. Studies by their group had studied the illness in severely affected patients, by visiting them in their homes to collect blood.
Using the new flow cytometer, they had been able to look at cell phenotypes and cytotoxic activity. NK cytotoxic activity in the severely ill was markedly down. Follow up with both moderately and severely ill patients showed that the NK activity in the severe remained significantly far worse. There was increase in NK phenotypes, variable KIR receptors, DC and B cell subsets and reduced perforin in CD8+Tcells compared to controls. She stressed the importance of looking at severity both clinically and in the laboratory.
[CJ- Several groups (including the CDC) are now making a special effort to examine the severely ill who are largely unable to make it to doctor’s offices or engage in studies. This is the first report that I know of to come out of those efforts. The KIR receptors problems suggested their immune systems were more severely suppressed, and these patients’ T cells appeared to have the same malfunction that their NK cells did.]
Samantha Johnston (Gold Coast, Australia) – The Definition Question
Samantha Johnston (Gold Coast, Australia) discussed the application of case definitions in ME/CFS research. She described the fact that there had been 8 case definitions used over the years, including 1988 Holmes, 1994 Fukuda and more recently the Canadian and then International criteria (ICC). Differences in symptoms and exclusion criteria lead to significant causes of variability. Prevalence using the Fukuda and Canadian criteria varied from 0.19% to 0.03%. Prevalence using the ICC has yet to be reported.
Initially definitions had emphasized fatigue and associated flu-like symptoms. More recent definitions describe an illness with neurological, immune and metabolic dysfunctions. The ICC is designed to be used in clinical settings, but if used in research, it could enable to identification of specific subgroups of the illness. Sensitivity and specificity, in relation to the 2011 International criteria has yet to be established.
[CJ – A recent study by the NCNED found more immune abnormalities, in particular those involving immune suppression, in patients meeting the ICC criteria compared to patients meeting the 1994 Fukuda or CDC criteria. About half the chronic fatigue syndrome patients that did not meet the ICC criteria but still had significant immune problems, suggested that both groups should be included in studies. See Definitions Matter blog for more )
Dan Peterson (Simmaron Research Foundation, Nevada, USA) – Diagnosis and Management
Dan Peterson (Simmaron Research Foundation, Nevada, USA) reviewed the diagnostic and management plan for patients with CFS/ME. He acknowledged that there is insufficient home and medical care for these patients. Prevalence worldwide may be as much as 19 million. The illness seems similar worldwide, but therapeutic responses differ widely.
Drug development can take up to 15 years, but a drug can be “repurposed”, and a biomarker is not necessarily required. Drug trials need to be large to be of value. Drugs can be “biomarkers” in themselves. (e.g., responses to cytokine blockers, immune modulators)
He then went on to discuss immune and antiviral therapies. Past trials have included immunoglobulins, Ampligen and Imunovir. Ampligen needs to be taken long term and is very expensive. Data extraction trials are however ongoing. With antivirals, some subsets respond well to Cidofovir. Valtrex (valgancyclovir) has been used for those who are HHV6 or EBV positive and there has been significant improvement. Other interventions include rituximab, cytokine blockers and GcMAF.
[Dr. Peterson’s assertion that a drug can be a ‘biomarker’ refers to the idea of segregating patients according to their response to treatment, and then digging into their physiology to uncover biomarkers that explain why they responded and others did not. Dr. Peterson’s presentation at the recent HHV-6 conference demonstrating that Cidofovir can be effective in some patients is an example of a possible treatment ‘biomarker’ that could be used to find other biomarkers. Dr. Kogelnik at the OMI and Fluge and Mella in Norway are exploring why some patients respond to Rituximab and/or antivirals. )Kathy Rowe (Melbourne, Australia) – Prognosis for Adolescents with Chronic Fatigue Syndrome
Kathy Rowe (Melbourne, Australia) runs a large hospital based clinic in Melbourne and has seen many patients since 1991. She presented her work looking at the long term outcome in young people with ME/CFS. Attempts were made to contact 788 young people who had attended her clinic from 1991-2009. 82% (1200) forms were returned, providing feedback biannually. The questionnaire asked for a functional rating out of 10 and included such things as schooling, tertiary education, level of education, work, marriage, childbirth, etc.
Average duration of illness was 5 years (range 1-16 years) and at 5 years, 60% had recovered, and at 12 years, 88% had recovered. 1/3 said they had to consciously manage their workload. Of those recovered, some only rated their health at 8/10, but were leading relatively normal lives.
There were no differences relating to severity or age. Earlier diagnosis and helpful professionals had positive impact. Only 5% of those recovered were not working or studying, and this was often due to factors other than ME/CFS. 90% had completed their education, and a number were married with children. Rates of depression (usually due to not being well) were comparable to Victorian base rates.
There was a better rate of recovery for those not depressed. Lack of parental bonding was not significant. 58% were EBV positive, and 20% had serological evidence of EBV infection at onset. 25% had significant ANA antibody titres, but this and positive EBV were no predictors of outcome. (10% went on to develop lupus). She questioned the significance of a positive ANA. But overall these results seem very good.
[CJ – Dr. Cheney, in particular, has referred to higher rates of recovery in adolescents than adults (and in a retrospective study dating back decades, Dr. Bell found that treatment made little difference in who recovered and who did not!). Rowe finds high rates of very substantial recovery over a long period of time in this study. The fact that 1/3 of patients (after 12 years?) had to consciously manage their workloads for fear of getting sick again indicated their recoveries were not complete. However, the 88% recovery rate, the very high rates of engagement in work or study, and the ‘relatively normal lives’ they now lead indicated that very substantial recovery had occurred in most people who came down with ME/CFS as adolescents.]
Sarah Knight (Melbourne, Australia) – Children with ME/CFS
Sarah Knight (Melbourne, Australia) – reviewed the state of knowledge about ME/CFS and looked at future directions. She is a paediatric psychologist – part of a large team. She stressed the importance of not seeing children as little adults – there are many differences, including attention to developmental changes. There are more challenges ahead for children with CFS/ME. The illness is more common in females and in children over 10. There is significant school absenteeism. Presentations are often complex and heterogeneous. There is an average delay of 15.5 months from onset until they come to the clinic for diagnosis. Co-morbidities are common. The investigations done by the GPs are variable, but all the usual investigations are undertaken at the clinic. Translational research has led to the development of a clinical programme.
Rosamund Vallings (Auckland, NZ) – Educating Doctors
Rosamund Vallings (Auckland, NZ) gave an overview of the approach she takes to educate GPs further about how to diagnose and manage this illness. She pointed out that the average GP has a minimal grasp of immunology and biochemistry, and with time constraints (usually only 15 minute consultations) also finds this illness seemingly too complex to manage. But a very simplified approach to understanding can be taught in medical schools, to GPs in training and at CME sessions. The doctor may need to approach the illness over several short consultations.
Acknowledgement and then education of the patient and family are important issues once a tentative diagnosis has been established. Attention to symptom management (pain, sleep, orthostatic intolerance) can then follow in much the same way as one would manage any chronic illness. The doctor needs access to suitable handouts. The importance of ongoing surveillance, and referring onto other health professionals were stressed, as well as using on-site other professionals such as practice nurses, physiotherapists and psychologists. This illness should be managed in General Practice, but worldwide there is a shortage of doctors with the requisite knowledge, leading to lack of confidence in tackling this complex area of medicine.
Warren Tate (Dunedin, NZ) – Molecular Pathways in ME/CFS
Warren Tate (Dunedin, NZ) is working to provide understanding of the molecular pathways affected in ME/CFS. He stressed the importance of getting a predictive diagnostic test, and his team is working towards that. He is looking at pPKR and pIFα as potential predictive tests. He has been interested in a study that looked at the molecular changes in one person over 726 days. Following such changes in a ME/CFS patient over time and throughout relapses could be extremely valuable, but could be very expensive. He is also interested in the relationship to other fatigue syndromes and the different subclasses. He will also look at cytokines, microRNAs, DNA polymorphisms, metabolites etc. He has looked at the plasma microRNAs in Alzheimer’s disease, and the individual molecules were combined and analysed to provide a possible predictive model. This technique could be applied to CFS/ME.
The closing addresses then followed.
Ross Humphreys, the chair of the NCNED steering committee spoke briefly and reiterated what a great day it had been, and what a wonderful event we had all witnessed with the opening of the facility.
Dr. Elizabeth Unger – Closing Address
He then introduced Elizabeth Unger (Atlanta, USA) to give the closing address. She said she had learnt a lot that day and had found it very exciting. She acknowledged that ME/CFS is a big public health problem, with epidemiology studies showing great economic impact. Interventions are needed such as education of the public, primary care physicians, nurses etc. Curricula are slowly developing. Many pathways are affected in this illness, and it needs to be dissected apart.
She asked the question as to whether we actually need a case definition, as it does not solve the problem of heterogeneity. We need validated questionnaires. No measures of outcome are readily available. A multisite review of the illness is needed, using a large number of measuring instruments.
She discussed the NIH funded PROMIS initiative (Patient Reported Outcomes Measurement Information System). 471 patients have completed questionnaires. There was less diversity than expected, and most respondents have been white upper class, educated people in the higher income bracket. Illness duration is seen as long. There were some symptoms reported by all, but a wide range of diversity. Results need to be combined with biomarkers, and the study is continuing. Results will also be compared with other illnesses such as Chronic Pain.
Christine Hunter then said a few words on behalf of the Alison Hunter Memorial Foundation (AHMF), and reiterated what we had all felt, that this was indeed a wonderful day. The AHMF now feel they have found a “home” and look forward to watching the development of the unit and ongoing research. Their contribution has resulted in installation of the flow cytometer, which will enable much exciting work to be undertaken.
The symposium was closed by Prof Donald Staines (Co-director of the NCNED).










So whats the good news? No treatments. Still much confusion. Who can help us now? What treatments or doctors can help us now not in 15 years?
That’s the hardest part. Unless the Pridgen antiviral study works out – which it very well may, treatment is going to take awhile..There’s always the possibility, though, that some drug that’s already approved will pop up that will work well or something else will pop up.
here here Jimmy. They’ve been talking about natural killer cells for more than 25 years, so what’s new?
Depressing!
I think further immune research is going down the wrong track, it’s been studied to death. The problem is in the brain / nervous system, albeit triggered by an immune assault.
Hi Matthias
On first reading I felt very strongly that a number of these studies were getting very much to the point as to how a peripheral immune reaction can hit the brain.
Slow progress as always but I’m more confident now that they’re looking in the right place.
It’s puzzling to me that the NK cell problems have not really excited the research community outside of ME/CFS. It’s a validated immune abnormality…However, the deeper they dig in NK cells, it seems the more they find. However, I also don’t believe that they’re ‘it’ either.
Yeah….poor natural killer cell function is documented in lots of diseases, I think its a marker for CFS but not that significant
Great article. Thanks for taking the time to share this. I also enjoyed your comments, Cort.
Thanks 🙂
Cort, thanks for this summary. There is amazing information here and I suspect that for some of your readers the reported results are starting to fall into place as part of a larger picture. However, the reports are at such a level that I can’t sort it all out. I try looking up various words on Wikipedia and Google and never get a complete understanding of anything through lack of time and energy. I feel like those of us lacking a medical background who want to actually understand such results should enrol in a summer school or similar set up specifically for our needs.
But this comment is definitely not meant to discourage you! Keep up the good work and I’ll keep trying to build my understanding.
cheers, Lynne
This article was particularly technical..Maybe a highlights section would be a good idea particularly for these types of blogs.
That message I sent was certainly not directed to Cort. He has and is doing much hard work that’s increadiable. Just frustrated today is all with the whole mess. To say that I have gone through hell and back would be an understatement. I’m hoping science will provide some quick answers and treatments but every time we find one part it opens the door to a new part of the body that is not working right. It can be very frustrating for bad cases such as mine. I can’t even get proper medical treatment from docs that specialize in the disease. No one has time or knows enough in cfs medical community yet. If anyone knows of any docs that they are actually getting better with I’m all ears? Where and how to deal with this disease when it gives you cancer as it did me and you can’t support yourself financially for years and years. Oh don’t get me wrong cancer was easy compared to this disease. I’m looking to do spiritual work because my thought is anything can be cured by our own soul and mind. It’s not to rule out hope in docs I think it’s empowering to take control at the seed level like some people do in the field of eppigenetics. Sorry for the rant its been a tough day. p
No problem at all Jimmy. The frustration is understandable. The bottom line is treatments are the key.
Good luck on the spiritual stuff; our mind and the depression and frustration we can control (although it does take perservance). I’m gratified at the results of the mindfulness work I’m doing to reduce stress and feel better. At least for me, this overactive ‘stress response’ is a key part of ME/CFS.
hey Jimmy,
I am only two years in to being ill. Just a baby really. A toxic exposure saw my system crash. So much happened – and in recent times – an extreme low. But I am again improving, improving from the rating of 10% of that previous life. Unfortunately all the improvements vanished, but they were there and if they were rebuilt once they can be again. I now have severe heavy metal issues to resolve. It will certainly complicate things. But great we have now discovered how big a problem this is for me.
I have several interegative medicine practitioners. I only suffered three morons in my saga – thinking an anti-depressent would fix me up. 🙁 The three all contribute in helping me manage this illness, mostly via nutritional supplements, trying to overcome chemical imbalances that are really at the bottom of everything. I recently started hyperthermic treatment, trying to activate my immune system, that seems to have gone AWOL. I guess thats how you developed the cancer 🙁 As if one illness isn’t enough. Reading about the immune system advancements here seems just what is happening for me. Well lets face it, one of the things.
I would encourage you to try spiritual, calm is GOOD for anything. And build that belief that you can overcome this. I now practice Reiki and other things that help me are cranial sacral therapy, far infra red sauna and massage. I have just found that my body can’t convert the B12 so the already converted form (lozenges) is like giving me oxygen in my blood, its amazing. Two years I’ve been saying it’s in my blood, and yes it is. For me. We nailed it – so excited about that. That advancement came about from live blood analysis, which also identified the immune system issue.
I’m not a miracle cure, but it is ANOTHER fragment of the treatment for me.
I think as individuals we are so unique, and then this illness is the same. I don’t imagine it can ever have an easy treatment. It really is cell by cell – but which ones in YOU are the ones we need to target? that is the needle in the haystack.
Sorry for what seems like a long lecture, just wanted to distract you. Feel for you. I sit and wonder ‘why’. Wishing you a 2014 that has significant improvements. 🙂
I think this research could lead somewhere with CFS, Cort is anyone investigating?
http://www.sciencedaily.com/releases/2009/02/090217173034.htm
How interesting…I don’t know if anyone is researching CCL2 in ME/CFS and I know there’s interest in microglial, but I don’t know if anyone is actually studying it in ME/CFS. If they produce a drug that blocks CCL2, though, that’s another possibility for reducing the ‘sickness behavior’ in ME/CFS. Cortistatin and drugs dealing with VIP are others.
I think in the medical community there’s alot of interest in producing new types of anti-inflammatory drugs; particularly drugs that reach the central nervous system.
“Swain and his colleagues found that liver inflammation triggered brain cells called microglia to produce CCL2, a chemical that attracts monocytes. When the researchers blocked CCL2 signaling, monocytes did not enter the brain despite ongoing inflammation in the liver.
When the researchers blocked the signaling of this immune chemical, microglia produced less CCL2, and monocytes stayed out of the brain.
In the mice with inflamed livers, preventing the entry of monocytes into the brain reduced sickness behaviors; mice showed more mobility and social interaction. These findings suggest that people with chronic inflammatory diseases may benefit from treatments that limit monocyte access to the brain.
“Sickness behavior significantly impacts quality of life. Our findings further our understanding and may generate potential new avenues for treatment of these often crippling symptoms,” said Swain.”
Thank you for the comprehensive summary of ongoing research. This is encouraging and even if the ever elusive pharmacological ‘silver bullet’ has not yet been found, the various lines of enquiry will inevitably lead to a better understanding and hopefully practical relief from various debilitating conditions.
I’m waiting for CMX001 to be approved next year for CMV….very closely related to Vistide that Peterson is using with good success, but with fewer side effects. It’s in stage 3 trials right now and if approved could be provided off label (at great expense)
S
Right – let’s not forget about CMX001 :)…That and Pridgen’s results and the CFIDS Associations two drug combo (which will apparently take awhile to get going) are three new possibilities hopefully for next year.
That was a great summary. It feels like pretty fresh information to me coming from another part of the world. It is good for us to realize there is more going on than we realize in North America sometimes.
I would like to reply to Jimmy. I agree with your comments as well. It is very frustrating to realize that we are just now getting on with the research and the class of researchers on board that may actually change the future eventually. It is also discouraging when we do not know what to do to help ourselves in any affordable, accessible way, with such ongoing suffering. I don’t see your comments as a rant but just an honest and common sense response to a almost impossible situation for some. I am a person with ME/CFS for 23 years and I also wish we were further along….so I hear you on all counts. Please be kind to yourself every chance you get and ask for help if there is anyone to ask (I realize there may not be). It is amazing our bodies keep ticking.
All my best to you.
the body’s ability to ‘survive’ is astounding.
I can’t imagine 23 years Valerie 🙁
Cort or Others,
If there is anyway to pull all this research together in a general, more understandable way for those without the technical knowledge, I would appreciate it. Summarizing in a general way is what I wish for, with the caveat, naturally, that this is only your best guess as to what this all means and where it may be going. I am thrilled that researchers are finding and working on understanding specific abnormalities, but can’t myself understand what they are doing at my basic level of knowledge.
For those of us who aren’t M.D.s, where can i find a dictionary of key words involved in ME/CFS research? E.g., the words I pulled out of the above reports to look up are:
Mast cells
Substance P (also relevant to my acne/roseacea issues but I don’t know how, yet)
VIP
Microglia
NK cells
cytokines
cortistatin
ciguatera epitope
glutathione
How to assimilate these definitions relative to each other and in a way that means hope for us?
Thanks.
Hi Cort,
I have a question regarding the Richard Kwiatek neuroimaging bit. If I understand it correctly (and I may not) it says that glutathione levels in ME/CFS match closely with controls, meaning they are the same. Does this mean then that with regards to the methylation protocol that glutathione levels are at healthy levels already? I would really like to know.
The other point I would like to mention RE the MRC in the UK, is that with the rather broad/loose diagnostic criteria used in the UK, however good the research is that they are doing now it will produce inconsistent meaningless results. And as for the £1.6 milliion they are funding it with, why are they contrubuting zero to the most important study in the UK right now- the Invest in Me Rituximab study, we are left to try and raise the funds ourselves. I don’t understand this, do you?
Thanks, Tim