



![]()
Taking the Next, er, Step

Exercise physiologists are becoming more engaged in finding the cause for the exercise intolerance in ME/CFS
First you document the problem, then you try to figure out what’s causing it. At least three research groups have decided it’s time to move past documenting a messed up energy production system in ME/CFS and to begin figuring what’s causing it. Over the next couple of months we’re going to see reports on cytokines and exercise, on lung issues and exercise and, in this study, on oxygen uptake and exercise.
Decreased oxygen extraction during cardiopulmonary exercise test in patients with chronic fatigue syndrome.Vermeulen RC, Vermeulen van Eck IW. J Transl Med. 2014 Jan 23;12(1):20. doi: 10.1186/1479-5876-12-20.
Follow the Oxygen Molecule
Maximal oxygen consumption reflects the aerobic and physical fitness of the individual. Wikipedia
Past studies from Dr. Newton and others have been zeroing in on poor oxygen uptake by the muscles. Let’s take a quick look at oxygen and energy production.
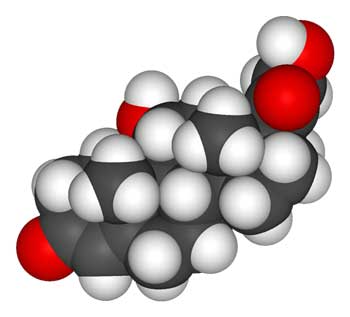
Oxygen means everything for exertion in humans. If you want to be able exercise vigorously you’ve got to get oxygen (and lots of it) into the mitochondria of your muscles. We get more oxygen into our blood by breathing more deeply and quickly, and then our hearts whip it to our muscles more quickly by beating faster and pumping out more blood. If it all works right we’re pounding the pavement for our morning jog or hitting the tennis courts for our afternoon sets.
Something obviously has gone very wrong when simply a walk around the block wipes people with ME/CFS out.
Big Study
Over the course of five years Vermeulen’s clinic collected exercise data on 203 people with CFS (Fukuda) and 223 other fatigued (did not meet Fukuda) patients (called Chronic Fatigue Idiopathic). Everyone with CFS (Fukuda) or severe fatigue (CFI) in this Dutch ME/CFS clinic got to do one exercise test to exhaustion. (Lucky them:) ). That made this study easily the biggest exercise study ever done in chronic fatigue syndrome.
The small control group (n= 18) included men and women who were ‘physically active’ less than an hour a week. (Somebody better acquainted with statistics and study design would know better how the small control group vs the large patient group affects the rigor of the results.)
Results
Seventy percent of the CFS and the CFI patients had significantly lower maximal oxygen uptake (VO2 max) at anaerobic threshold than the controls. ‘Significantly lower’ did not mean a bit lower; the high probability scores (P<.008) indicated that oxygen uptake into the muscles was much lower in the fatigued group.

Oxygen uptake by the muscles at anaerobic threshold was greatly reduced in about 2/3rds of the ‘chronic fatigue’ patients
For example, the lowest muscle oxygen uptake achieved by the healthy controls at maximal workload was a very low 10 ml/100 mls, a value Vermoulen reported is found in heart failure..
The lowest O2 uptake by the CFI patients was almost half that (5.4 ml/100 mls), while the lowest oxygen uptake by the ‘CFS’ (Fukuda) patients was less than half that of the worst off control (4.4 ml/100 mls.) or similar to that found in (asymptomatic) HIV patients. That means that the muscles of that patient was receiving about 44% of the oxygen that the poorly functioning healthy control was.
The fact that the patients who met the Fukuda definition and who did not had similar VO2 max levels at anaerobic threshold suggested that simply being very fatigued was enough to result in low VO2 max scores.
The ME/CFS group, had a higher cardiac output relative to oxygen uptake, than the idiopathic CFS group appeared to suggest that their hearts were working harder in an attempt to compensate for the reduced oxygen uptake.
The Normal VO2 Max ME/CFS and CFI Group
About 30 percent of ME/CFS and the CFI had VO2 max results similar to those found in the healthy controls. (Oddly enough more ME/CFS patients (73.203 – 35%) than CFI (59/223 – 26%) did not have reduced VO2 max values. The source of their fatigue lay elsewhere. (But would their normal VO2 max levels remained normal in a second , repeat exercise test.)
Cause of the Cause?
If low oxygen uptake is responsible for the reduced exercise performance what is causing the low oxygen uptake?
The oxygen carrying capacity of the hemoglobin in the red blood cells that carries oxygen could be reduced. The lungs might not be pumping hard enough to get the oxygen into the blood in the first place. The heart might not be pumping fast enough and hard enough to get the blood to the muscles. The blood and oxygen might be getting to the muscles, but the muscles might not be picking it up. Lastly, deconditioning or lack of effort could be a factor.
This study found no reason to suspect that lung or heart problems or deconditioning or lack of effort played a role in the inability of many people with CFS or CFI.
Instead the authors proposed that mitochondrial problems or immune issues were responsible and pointed to reduced VO2 max levels found in people with lupus in 1995. Three followup studies found that reduced aerobic metabolism was common on SLE.
The Autoimmune Connection
Several studies suggest reduced cortisol during exercise could play a role in similar exercise problems in some autoimmune disorders
Since cortisol plays a significant role in releasing energy for exercise, the authors of a 2004 study examined the effects of maximal exercise on cortisol production in rheumatoid arthritis and lupus. Cortisol levels should rise in response to exercise, but they in both disorders they immediately fell 10% during exercise and over 20% an hour later. A later study suggested that low cortisol in combination with increased cytotoxic T-cells helped set the stage for RA. (Soon we’re going to review an ME/CFS paper suggesting that low cortisol in combination with immune factors could set the stage for many disorders including ME/CFS).
Unexpected decreases in cortisol (and IL-8 and heat shock proteins) in fibromyalgia during moderate exercise suggested a similar pattern may prevail there.
At one time cortisol was the most researched topic in chronic fatigue syndrome. Studies linking low cortisol output to reduced exercise capacity and altered immune functioning in these disorders suggest reviving it again might be a good idea. (Cortisol levels were not reduced during a standardized exercise test in one study, but ACTH responsive was. )
Conclusion
The sheer size of this study would, one would think, effectively end the question whether metabolic abnormalities thwart energy production during exercise in ME/CFS, or whether deconditioning is a significant factor. (Wyller’s recent study also suggested deconditioning was not a factor. In fact, it’s hard to think of any physiological study – although many have tried – which has suggested that deconditioning is a significant factor in chronic fatigue syndrome.)
Vermeulen’s findings fit a series of research results that are more and more fingering reduced oxygen uptake as a cause of the exercise problems in ME/CFS. (He noted that Newton’s recent pH findings may fit his findings.) While people with autoimmune disorders and fibromyalgia do not typically experience the degree of exercise incapacity as ME/CFS (and light exercise is often recommended), similar reductions in VO2 max have been found, and may be tied to cortisol and immune abnormalities.
Satisfied that metabolic impairment is present, exercise physiologists are moving forward to try and discern its cause. At the March IACFS/ME conference Workwell’s exercise findings will focus on reduced ventilation and cytokines will be the focus of another exercise study. We seem to be getting closer.






I have been telling Dr.s for years that every time I have been given Oxygen in hospital my pain levels have dropped to ZERO! Definitely on the right track I am certain of it. Fibro friends have also reported the same thing to me. Unfortunatly nobody ever listened except one Physiotherapist. Bless her. We know our bodies better than anyone else and I am certain this is the problem in my case. Thank you and good wishes from a chronic pain sufferer for 60 years.
Now got heart problems…no wonder x
.
I like this. Could explain a lot of things. Reduced oxygen uptake would necessarily be the beginning of …an avalanche of problems. Oxygen is life itself. ( ‘Closer’ is very very good.)
It could explain the breathlessness
Hi Cort,
Thanks so much for breaking the research down for us yet again. This is the first time in many years that I feel a little more aware of why I feel so rotten after the mildest of exercise. It’s always been something that has confused and frustrated me over the last years.
It’s really interesting but I can’t help feeling I’d love to know if there’s something us sufferers of post exertional malaise can DO about it NOW that these results have been found…. I know, I know, getting greedy 😉
All the best,
Jo
I will ask Vermoulen what the next step for him is. Wouldn’t it be interesting if the immune and endocrine findings in ME/CFS came together with the exercise problems. That would be really something. It could be that the different groups are converging on each other.
Cort writes- “The ME/CFS group, had a higher cardiac output relative to oxygen uptake, than the idiopathic CFS group appeared to suggest (?) that their hearts were working harder in an attempt to compensate for the reduced oxygen uptake.”
I’m not sure if it’s the same thing, but after I exert myself too much one of the things that happens is that my heart will go on pounding all night long even into the next day instead of just going back to normal in like 10-15 minutes like what happens in a healthy person. Pisses me off.
Well done to the authors for making such a valuable contribution to the research literature.
One of the things I’ve seen in exercise and other studies are difficulties in systems turning themselves off. Your heart seems to think you still need it to pound as if you were still exercising. A upcoming blog will reference these reactions that don’t turn themselves off as they should.
Do you know if Kogelnik’s ‘everything’ study has an exercise component? Would be interesting to see how the things he’s looking at (ie ‘everything’) react to being hit w/ exercise.
With a Level 2 or 3 CFS Energy Point Score* and a bad knee, when I first started bicycling 10-12mph to the park or friend’s house 2 miles down the flat street, that happened to me too. HR would be 160 for 20-30 min after getting there, and stayed elevated (>110) for a very long time. Resting rate was 70-80.
Since bicycling was easier than walking, I continued to bike 2x/wk, adding on a little more distance each time (usually to various coffee shops!), and taking 3 days to recover. After about 6 months, I could bike 25-32 flat miles r/t and my heart would recover in minutes.
3 years later, any hills >4% grade are still VERY difficult (HR=165-183, at age 60), but I can do them. However, I am gasping for air like a fish out of water, and my companions are asking me if I am OK! Anything over 32 miles is still difficult. Snack every 15 min. vs no food makes no difference.
Iron levels, ferritin, etc. are all slightly high, so no anemia and all signs of high altitude training >7000′,but I am at 200′. So body thinks it is starved for oxygen.
Resting HR is now 62-65, and 52 while sleeping; Means heart is stronger. 🙂
Measuring HRV every morning can tell you your heart health. Scale is 0-100. Takes $50 bluetooth chest strap and a free EliteHRV (or similar) App. 60-80 is normal. Mine was usually 36-42, which implies Vagus nerve viral infection.
Note:
Dr. Martin Lerner’s Protocol of 5 supplements + Iodoral + Selenium + Zinc got me to Level 3 from semi-bedridden (Level 1).
*CFS Energy Index is 0-10. Bedridden =0, Normal =10.
(Google for .pdf chart).
Yeah, I hate the phrase ‘post-exertional malaise’. lol It doesn’t come close to expressing what I experience from just walking around. It is more like ‘prolonged near death experience’. Looking forward to the ‘upcoming blog’.
Prolonged near death experience – I can see that. 🙂
You’re right – it’s a horrible term that obscures what’s really going on! I thought it referred to an exacerbation of symptoms but now I think the medical definition for is much the same as our ordinary conception of it. (blah!)
Post-Exertional Malaise (PEM), Myalgic Encephalomyelitis (ME), Systemic Exercise Intolerance Disease (SEID), and any other long and complicated names are way too difficult for anyone with CFS.
It is just another way doctors f#%& with us.
Traditionally, low V02 is caused by either your lungs not being able to get oxygen into your blood, or your heart not being able to pump the oxygen saturated blood. This is what happens in more “common” pulmonary disease or heart failure.
In our case, it appears to be neither of these. We can be fully oxygen saturated at the periphery meaning that our lungs are heart are working (as evidenced by a %95-%100 reading on a pules oxymeter), yet our bodies are somehow not able to use this oxygen to make energy. Its either not diffusing correctly from the capillaries into the cells, or the cells/mitochondria aren’t using it to make energy. I sure hope they figure this out.
Well said!
Workwell has some evidence suggesting the muscles that move the lungs are not doing well. I wonder if the microvascular problems are causing the blood not to get out all the way out to the muscles. It’s also possible, I believe that the brain is not activating the muscles like it should. There’s some evidence for that in ME/CFS. I’m not sure how that works in this scenario but it must fit in there somewhere.
I think we are getting closer and I hope this study sparks more studies! I think this is where we need to go 🙂
One study Cort posted awhile back showed CFS people’s low ATP-energy producing cells produced double the normal amount when in the blood serum from Normal people, making up for lost time.
Many CFS people are ex super athletes, myself (a champion ‘all-natural’ powerlifter, training & competing on & off until age 52) included. Some were in the middle of training for the Olympics when hit by CFS.
So heart, lungs, diet, and muscle development are above normal. So CFS is obviously not just people being lazy or out of shape.
So it is not the mitochondria that is damaged, but something in the bioslime, serum, and enzyme reactions.
Q: Has anyone EVER tested the Serum of CFS people for unknown strains of HHV-4?
99.99% of adults worldwide carry at least one strain of HHV-4, out of dozens. Just like bacteria, viruses mutate constantly. Some mild strains have zero symptoms for years.
Others make even little children sick and bedridden for months or years.
That seems like the obvious place to start.
When ME patiënts exercise they have difficulties with the system turning the ortho sympathetic nervous system -stress- reaction off. This is an objective point to measure and the hallmark for this illness. I think. The heart pounds (tachycardy) as if you were still exercising even after hours till days. Why don’t this reaction not turn themselve off as it should? The parasympathetic nervous system is not working properly (infection?) or is this reaction to compensate for the reduced oxygen uptake? If this is true then there is nothing wrong with te ANS.
Right – Wyller’s recent study suggest the ANS is trying to correct a bigger problem!
This is why people with ME have breathing problems like hyperventilation. Maybe there is something wrong with handling pH. If pH is a problem infections are born…. pH is in the blood, stomach, salvia, muscle etc… i think infections in ME are secondary…
Hi Cort
Type II diabetes patients also suffer from fatigue, early onset muscle pain and exercise intolerance.
There also appears to be a similar pattern in type II diabetes patients with reduced oxygen uptake and oxygen uptake which is delayed in response to exercise and prolonged after exercise.
Peak oxygen uptake may also depend on vascular/endothelial function at skeletal muscle which appears to be impaired in T2D.
http://care.diabetesjournals.org/content/30/11/2880.full.pdf
http://onlinelibrary.wiley.com/doi/10.1002/clc.4960261107/pdf
Interesting given the recent peripheral neuropathy findings in fibro and endothelial dysfunction and the correlation between leptin levels and fatigue days in ME/CFS.
Its difficult to tell though if the problem is primarily one of tissue metabolism or resulting from, for example, disruption of cerebral blood flow affecting the HPA axis as has been proposed for exercise intolerance in post-concussion syndrome.
Diabetes is in the mix as well. I didn’t know exercise intolerance was found in diabetes and that vascular functioning at skeletal muscle was implicated. So interesting! And then there’s the neuropathy that’s common in diabetes. Oaklander found several undiagnosed diabetes cases in her study as I remember.
So the HPA may be impaired by reduced blood flows as well. I believe Cheney has proposed the same for the gut in ME/CFS.
So much stuff in here. Thanks again, Marco 🙂
You’re welcome.
I think I feel a blog coming on : )
I like that feeling 🙂
Shoemaker’s believes that exercise intolerance in his mold patients is due to low VEGF, which regulates blood flow to the capillaries. Many of Shoemaker’s patients have extremely low VEGF. It would be nice to hear what “CFS” researchers have to say about this…
http://ramblingsearcher.blogspot.com/2012/06/shoemaker-and-improving-vo2.html
Thanks for getting Shoemaker in there Floydguy. I’m looking forward to learning more about his theories.
It is true that when I am around certain kinds of mold toxins, my heart will pound.
Anything that hampers the oxygen level of the body includes the muscles, and research has indicated that conditions such as COPD affect the oxygenation of the muscles. Low oxygen in the muscles predisposes them to develop myofascial trigger points, something that all chronic pain states have as pain generators. Both fibromyalgia and chronic fatigue syndrome patients have trigger points generating pain and dysfunction. They cause microcirculation problems, and stick tissues together, restricting motion. Co-existing conditions such as diabetes or insulin resistance, hypothyroid; toxic exposures; body asymmetry and other perpetuating factors act to keep the trigger points in play, and the spiral continues until something is done to treat the trigger points and control the perpetuating factors. Fortunately, we know what to do. If one can identify the trigger points and the perpetuating factors.
Thanks Devin….Lot’s to learn here 🙂
Some of us, probably were genetically never meant to be long distance (endurance) runners. I developed ME/CFS, while doing strenuous (aerobic) exercise. I just kept pushing myself beyond my (genetically, inborn) mitochondrial limit, even though I knew, that my body was telling me to stop.
As a child, I never had the endurance it took to be a long distance runner. I enjoyed track and field events, but the activities I excelled at were the ones that required short bursts of energy (anaerobic), the 100 yard dash, standing long jump, or running long jump. I always won the red ribbons in these events. But, as much as I tried I never had the stamina to run long distance. I was always curious, as to why?
I’ve come to understand that slow-twitch muscle fibers like those of the long-distance runner have abundant mitochondria and use large amounts of energy slowly so that you can work out for a long time without getting tired. Slow fibers use oxygen-using (aerobic) pathways for activities that require endurance.
Fast-twitch muscle fibers found in sprinters have less mitochondria and use small amounts of energy quickly. Fast fibers use sugars for fuel (anaerobic) and do not require oxygen. It gives you the ability to run fast, but for short distances. The byproduct of this (anaerobic) energy production is heat and lactic acid. Lactic acid accumulation in the muscle causes fatigue and soreness. The (anaerobic energy) system is a limited system for energy production.
The organization of muscle fibers in each or us is determined by our genes. I now understand, that the endurance of the long-distance runner (aerobic) and the short-burst of energy experienced by the sprinter (anaerobic) are both genetic in nature. If I had known this almost thirty years ago, I may have been able to save myself from developing ME/CFS.
I hear you, Rachael.
One of the interesting things about joining 23andMe is that you can find out if you are a slow twitch or a fast twitch type of person.
I was a fast twitch, too.
It’s good to remember that exercise intolerance is a factor in many diseases, not just ME.
Btw, his name is Ruud Vermeulen, not Vermoulen.
I wonder if they should throw some B1 megadoses into half of the CFS patients – to see if it makes a difference to oxygen uptake (B1 is used in producing energy from carbs, among other things).
And ‘Post Exertional Collapse’ is a much better description. ‘Malaise’ MEANS ‘feels unwell.’ Another trivializing description.
It’s amazing how patronizing all these people are toward those of us who have these symptoms.
Thank you so much for this informative article, Cort!
It reminds me of Dr. Cheney’s lecture where he showed the oxygen level remaining the same in the blood of ME/CFS patients, instead of getting used by the muscles.
I’d be really interested to know if the people in this study with ME/CFS who had normal V02 Max values were in the early years of their illness. I wonder if the researchers could go back and break it down by length of illness.
I’m wondering about this because I could exercise much more in the first three years of illness, before my fever broke.
I have, for years, know that people with fibromyalgia, such as myself, lack the ability to get enough O2 to the heart for healthy cardiac function during exercise. In fact, getting O2 on a regular basis is something a fellow FMS sufferer who lives in Australia no longer has to deal with as she is give O2 for her FMS. She uses it at times with FMS sufferers have the most need for recovering, ie: taking a shower. Everyone in the FMS community uses being able to shower and wash hair as a bar of how well they are doing. My Australian friend simply lays on her bed after a shower and turns on her O2. What I don’t understand is why it is SO difficult to get O2 in the U.S. It is not harmful, not addictive and provides such recovery after taxing activities like grocery shopping or showering or just running errands. I find the inability to get O2 to be very frustrating. In fact beyond frustrating into the stupidity of my current “medical” team. I’m so tired of fighting a very “well patient” HMO for things I need as a sufferer of FMS, Adrenal Fatigue plus a host of other conditons and auto immune diseases. I can understand the recluctance of throwing pain meds around, but O2, really. Who is it hurting?
I’m late reading this article, but so glad to read about it. Thank you, Cort.
I have just a couple of comments.
1. Re: the probability score mentioned under the Results section, “‘Significantly lower’ did not mean a bit lower; the high probability scores (P<.008) indicated that oxygen uptake into the muscles was much lower in the fatigued group." It's a technical point only, given that the study did show that the oxygen uptake was much lower; however, I believe that probability scores only point out how likely it is that the result would have come about by chance. For example, in this study, the probability score indicates that there are only 8 in 1,000 possibilities that this result could be due to chance. So that's a high level of statistical significance. Usually 5 in 100 is sufficient to say that the results are statistically significant or were unlikely to come about due to chance. But that in itself doesn't address the large discrepancy between the oxygen uptake levels. The figures that follow certainly do document the wide discrepancy. (I hope I don't sound like an ass for making this distinction. 🙂
2. I'm wondering why taking cortisol for quite a long time early in my illness didn't seem to help me in any way I could tell.
Again, Cort, thanks so much for another excellent review of an important study.
Thank you for such an informative article! I have had CFS for many yrs now and have always been active and i refuse to give in yet some days i have to admit defeat .In my mind i always thought it was something to do with my absorbsion of oxygen as my muscles fatigue quicker than others and i get totally wiped from aerobics classes but still endure them as i love dancing lol.
Im looking forward to learning more as i long to live a somewhat normal life 🙂
Interesting to read someone is actually doing research into M.E. – my pulse is usually between 53 and 64 bpm but when in bigeminy 35. I had to visit my daughter in hospital once and my husband couldnt take me – when I finally arrived in her room she was on oximetry I checked my oxygen as I felt terrible O2 was 79% and pulse 46 – I Had had a long walk and felt almost on collapse – really hoping your work proves +ve .
Interesting stuff.
It has always been one of the most astounding things to me- that I could be healthy and fitter than most people around me for the first 21 years of my life, playing( and loving) a lot of sport…then developing CFS…at which point cardiovascular exercise became utterly destructive. Despite such a fundamentally disabling and clear symptom…there was never any way a clinician could (or would) objectively measure such a thing. Yes- ‘malaise’ doesn’t cut it- I call it post-exertional destruction…and it remains present with the other symptoms 18 years later.
I remember once looking into trying a hyperbaric oxygen chamber…but it seemed too hard to arrange. So- my question is- what’s the easiest way for someone (I’m in Australia) to try some form of oxygen therapy/ get easy access to oxygen. Do I need to get in touch with my nearest scuba centre!!??
I agree that the most astounding thing indeed is the post-exertional destruction (nicely put).
Dr. De Meirleir believes, as I remember, that oxygen therapy might help in the short term but does not get at the core of the problem. Good luck in your search, though.
Anavar (Rx) and Cordyceps Mushrooms have been shown to greatly increase oxygen uptake in Seniors.
Cort: Has anyone done a study using either of these on long-term CFS people?
Readers: Do you have experience using either pre-exercise? (Whatever your ‘exercise’ is).
Me: Sometimes Cordyceps helps, sometimes it doesn’t. I haven’t figured out if it matters what I take it with.
My trim (&chemically sensitve) X-country runner adult son says he feels a positive difference; & says his blood feels ‘fizzy’.
Great article as always, Cort.
Regarding my racing heart at night while trying to go to sleep I’ve recently found homeopathic coffea cruda 30C has helped (Homeopathic nux vomica is another remedy for a racing heart.) I’m also wondering if the Wim Hof breathing method might help push more 02 into the blood? Has anyone tried this?
The article briefly mentioned heat shock proteins are reduced by ME/CFS. I wonder if you might elaborate on this in a future article? Might near-infrared saunas (or steam sauna or far-infrared) help by forcing the production of heat shock proteins? Do you know the effects of taking a regular sauna on ME/CFS?
Another possibility that I’m about to try is the Budwig FOCC protocol (flax oil emulsified into cottage cheese). This protocol is based on the work of Otto Warburg (a Nobel Prize Laureate for the discovery of the nature and action of the respiratory enzyme) who suggested that cancer cells live in hypoxic, very low oxygen (and acidic) conditions.
Dr. Budwig worked under Dr. Warburg in her younger years until his death. According to Budwig, Warburg theorized that cellular respiration, like many chemical reactions, was dependent upon substrate availability, specifically a sulphydryl group and an unknown saturated fatty acid, which he failed to identify. Budwig continued his work and isolated the fatty acid which led to the FOCC protocol of emulsifying flax oil into naturally sulpher-rich cottage cheese. It changes the electrical charge of the fatty acid which allows oxygen to better penetrate the cells. My question is, if this allows 02 to penetrate into the cells well enough to stimulate apoptosis of cancer cells then shouldn’t it also enrich the mitochondria with oxygen and possibly affect the low cellular oxygen levels of ME/CFS sufferers?
Most people think of the Budwig protocol as an effective cancer therapy (and for many it is, it healed my cancer over 20 years ago) but Dr. Budwig later discovered it also cured heart disease, arthritis, and many other conditions. I’ve long wondered if it might be beneficial in ME/CFS or fibro? I’ve never been able to find any information on this. I’ve tried it very short-term, but I’m going to give it a try for at least six months. Fingers crossed!