



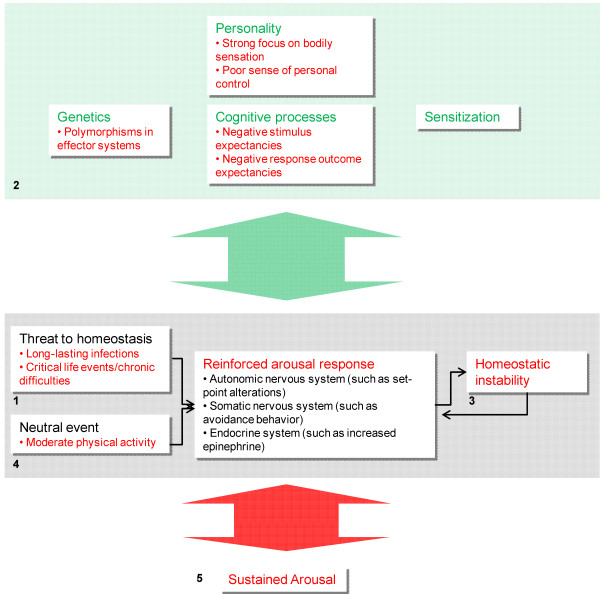
Specifically, we suggest that CFS is caused by sustained arousal. Wyller
Brun Wyller’s drug/behavioral approach to chronic fatigue has been controversial in Norway. Embraced by many in the medical community there it’s emphasis on psychological factors has dismayed many in the ME/CFS community.
We suggest that sustained arousal can originate from different precipitating factors (infections, psychosocial challenges) interacting with predisposing factors (genetic traits, personality) and learned expectancies (classical and operant conditioning). Wyller
While Wyller cites ‘firm evidence’ that long-lasting infections could initiate the SNS arousal in ME/CFS, his model of sustained arousal relies heavily on psychological factors (illness perceptions, poor control over symptoms), ‘personality’ issues (strong focus on bodily symptoms, poor sense of personal control), and maladaptive cognitive processes’ (negative stimulus expectancies and ‘inappropriate learning processes’) to perpetuate the illness.
While psychological factors are embedded in Wyller’s theory, he also believes physiological factors will help explain the fatigue, muscle and even some of the ‘behavioral problems’ present. If it’s true that sympathetic nervous system activation is a prominent feature of ME/CFS, then Clonidine, a sympathetic nervous system inhibiting drug should clear up a variety of problems.
In this Clonidine study of adolescents with ME/CFS Wyller put his ‘sustained arousal’ hypothesis to the test.
Big Trial
Wyller has gotten a lot of support in Norway, and the study, containing 120 people with chronic fatigue syndrome and 69 controls, was a large one.As usual, Wyller used his own case definition of chronic fatigue – severe fatigue over the last three months – to delineate ‘chronic fatigue syndrome’ patients. Seventy-three percent ended up meeting the Fukuda criteria. Forty-one percent had ‘depressive symptoms’.
Because Clonidine can lower blood pressure, which could have negative effects on people with orthostatic intolerance, low doses designed not to affect blood pressure were used. To his credit Wyller used a fairly rigorous primary endpoint to measure effectiveness: the number of steps the adolescents took during the day. If that number increased significantly, the trial would be considered a success. Numerous secondary measures were also taken.
SNS Arousal Hypothesis …Not Sustained
“The results were both interesting and somewhat depressing” Wyller
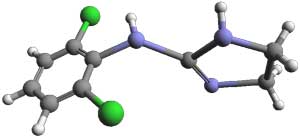
Clonidines SNS antagonism,neuroprotective and anti-inflammatory properties suggested it might work in ME/CFS
Much seemed to line up for Clonidine. It inhibits SNS (fight/flight) activity and enhances PNS (rest/digest) activity and it has anti-inflammatory properties. The receptors it affects were identified in the Light gene expression studies as possibly contributing to ME/CFS. It is used to inhibit anxiety, treat ADHD, migraines and sleep disorders, and even reduce stress – a key component of Wyller’s understanding of chronic fatigue.
Arousal responses also include behavioral changes, which seem to be mediated – at least in part – by catecholaminergic neurotransmission to brain motor areas. Wyller
Given Wyller’s belief that some of the behaviors in ME/CFS are driven by catecholamines such as norepinephrine, Clonidine should have even changed the participants behaviors as well. Reducing sympathetic nervous system activity should also be able to enhance natural killer cell functioning, increase anti-inflammatory activity and reduce pro-inflammatory activity.
Unfortunately, not only did Clonidine not make the adolescents with ME/CFS better, it actually made them worse.
Reduced levels of norepinephrine in the ME/CFS patient’s blood stream indicated that Clonidine was indeed reducing sympathetic nervous system activity, but instead of increasing activity levels and reducing fatigue, it significantly reduced physical activity and significantly increased fatigue scores. By the end of the trial the ‘CFS’ patients on Clonidine were significantly worse off, leaving Wyller’s hypothesis of “sustained arousal’ in shambles.

Clonidine effects – increased fatigue and reduced activity – suggested the sustained arousal might be there for a reason.
Some basic characteristics of Wyller’s model (the SNS arousal, the parasympathetic nervous system inhibition, and the state of low-grade inflammation) were validated, but the study results suggest these factors may be an attempt by the body to improve health – not a bar to it.
Stating that he still believes his ‘sustained arousal’ theory is sound Wyller wouldn’t go that far, but it’s hard to know how else to interpret this study. If Clonidine had had no effect that would have been one thing, but making chronically fatigued patients significantly worse is another.
The findings suggest, at least to me, a laymen, that the ‘arousal’ and activation of the fight/flight system, the increased heart rates during rest, the inability to relax, even maybe those rushing thoughts – are there for a reason. Far from causing ME/CFS, the fact that Wyller’s patients got worse when the arousal was tamped down, suggested it might actually be helping.
That leaves the question what an aroused fight or flight system might be trying to fix? We know continuous SNS activation is not good. It doesn’t give the body any time to ‘rest and digest’ or relax and repair itself; i.e. some fuses are going to blow over time. SNS activation also accentuates the Th2 side of the immune system while reducing the Th1 (antiviral) part of the immune system that fights pathogens in cells.
We do know several things Clonidine does. Because it decreases vascular resistance (opens blood vessels) it should increase blood flows, which would seem like a good thing. Those constricted blood vessels may be constricted, however, to raise blood pressure. (Do people with ME/CFS have both low blood volume and low blood pressure?).
Clonidine also decreases gut motility and inhibits insulin release. Insulin carries glucose to the cells. (Could clonidine have interfered with energy metabolism?)
Deconditioning – Not ‘It’ in ME/CFS
As the results undermined Wyller’s hypothesis they also demolished the idea that deconditioning is a factor in ME/CFS. Some researchers have believed that the higher heart rates and the SNS activation indicated by increased norepinephrine (NE) levels found in ME/CFS could reflect deconditioning, but Wyller’s inability to find a link between blood NE and activity levels suggested the increased SNS activity was not being driven by deconditioning.
Inflammation – Not ‘It’ Either?
The fact that both NE and C-reactive protein (CRP) levels fell together suggested that SNS activation was indeed driving inflammation. (The sympathetic nervous system is an important immune regulator.)
Inflammation has long been proposed as a key factor in ME/CFS, and inflammation was present in Wyller’s patients, but Clonidine’s reduction of a broad inflammation factor (CRP) had no effect on symptoms or physical functioning. That was surprising.
The Autoimmune Connection
One blog listed autoimmunity as an alternate theory to Wyller’s stress response hypothesis, but my understanding is that the stress response issues could help prepare the ground for it. Chronic activation of the sympathetic nervous system and low cortisol levels from the HPA axis both upregulate the humoral (antibody driven) side of the immune response. Since cortisol is an anti-inflammatory, the low cortisol levels in ME/CFS should increase inflammation. Both would seem to help set the stage for autoimmunity.
Conclusion
We still believe that it’s about a sustained stress response in the patient. We have much evidence of this phenomenon in those who are chronically fatigued. But there is no direct correlation between the stress response and the patient’s ailments. Wyller

Something is keeping ME/CFS patients systems on edge. At least in this case, removing that edge didn’t work. Finding out what’s putting them on edge sounds like the next step.






ebv..ebv”’ebv I am an electrician but 2 hours a day for 26 years on the computer trying to make sense of this bug that has ruined my life and my wife’s it screams at me ebv
I have a big white blob on my brain[infection damage ]
I have a new aorta valve in my heart[the old one was in pristine condition except it hade large infection burn holes in the leafs
…..AND I…. still say EBV IMPLICATION some how someway
cheers geoffrey
:)… We have a really interesting EBV blog coming up. I think you’re going to like it 🙂
I wish that our country would examine the shape of red blood cells in ppl with ME/CFS/Fibromyalgia
They would see that a high percentage of the cells reproduce in an un-natural shape
When these cells try to pass through the smaller capillaries they have trouble – this is why Fibromyalgia has distinctive tender point areas. As the shape of the cells is not right it does not carry as much oxygen – hence the muscle cramps fatigue etc
The body keeps reproducing faulty red blood cells, at some stage a person contracted a bacteria/virus/pollutant and their immunity was lowered prime then for a trigger to overwhelm the body (an accident a trauma ) and allow any bacterium/virus/pollutant to mutate, we are not getting rid of this and our red blood cells reproduce in a faulty way, I think they are trying not to pick up the contaminant or the contaminant is causing the faulty red blood cells.
Accept the red blood cells examination challenge! then find out why they reproduce that way I think try an anti-inflammatory with an antiviral with antibiotic for 3 months then re test. By getting the red blood cells normal – you have a cure.
Your theory would seem to fit the not getting enough oxygen to the muscles problem. I thought though this was studied and it didn’t pan out (????) but maybe I’m wrong.
How about the idea that the capillaries are too small to get many red blood cells through? Is that possible?
There is a possible issue with to low levels of Vascular endothelial growth factor (VEGF). Hypotetical speaking: Can’t rule this out as a potential cause or contributing factor. (might or might not?)
i.e. how to do?: Quest-labs or labs that is certified as performing test for analysis.
—
Thanks Cort for your blogpost. Wyllers name is by the way: Vegard Bruun Wyller. We say it short VB Wyller (his brother TB Wyller).
Do you still thinks Norway is a patiens paradise for PWME??
😉 so long folks, and there is comming more publications from the NorCapital-study (2 allready out)
‘Like this. ‘Reminds me of the low sed rate (0-2ish); Dr. Hyde said that’s seldom seen except in sickle-cell anemia. So, to what extent are our cells mis-shapen? ‘Shouldn’t take a whole heck of a lot of money to start doing. Dr. Kl should snag a grad student; just make sure they’re getting THEIR sleep and don’t prick themselves!
‘Also believe, like Cort suggested, that the capillaries may be too small. Whether this is because of NO and all that, I don’t know. But to this layman, it makes sense as to why it would be harder to warm up, cool down, and sweat.
Cort, it seems that an active autonomic nervous system is an adaptation rather than the cause. This would be a meaningful conclusion. But is this conclusion justified?
I don’t know It’s an idea – and Wyller does not seem to subscribe to it and he knows a lot more about this stuff than I do.
Clonidine knocked down the norepinephrine levels in the blood, but I imagine there’s a lot more to the SNS arousal than NE. It’s a very complex subject that I can’t begin to understand.
I wonder what Gupta’s reaction to this is…
The excessive sympathetic nervous system activation is most definitely a symptom of underlying dysfunction and/or infection rather than an adaption or a causative factor.
I’ve seen this activation completely erased (temporarily) by antibiotics in the past and increased significantly by food and chemical reactions. I’ve even seen significant and immediate decreases in this activation purely from having an enema to relieve effects of dysbiosis and leaky gut. Also glutathione has in the paste helped (but this no longer does).
An over-reactive SNS system – that makes sense. Calming it down, though, didn’t help and, in fact, the kids got worse. It’s very puzzling…Dysbiosis and infection appears to get it going in your case (and in some of his patients).
Maybe it’s not the SNS; it’s the PNS that’s the problem. The SNS may be both helping and hurting but unless you fix the PNS it’s not going to work, and turning the SNS down with a drug is not enough.
We really need a dysautonomia expert. 🙂
Fatigue is a very common side effect of Clonidine (>10% of patients according to Wikipedia)…
It seems to me part of the problem for some of us is that SNS stays in high gear because many of us are stuck in a cycle of ‘we got sick’ -> ‘we couldn’t work’ -> ‘we can’t afford treatment or a healing environment to live in’ – > ‘we are financially and environmentally stressed’ -> ‘we stay sick because our bodies can’t heal from underlying causes (infections, detox problems, and nutritional deficiencies, etc.) while under severe stress’.
Wyller should do a study where he asks patients what is their needs are and cater to that for a year and see how they do. Give them enough money for food and housing of their choice, access to doctors and treatments of their choice, and basically listen to their needs. While this wouldn’t solve CFS/ME for everyone (certainly a some patients are well taken care of by their families and they do not improve) it seems to me many who have improved or ‘recovered’ generally do not have financial issues and have solid social and medical support.
I’m sure that would help James.
It’s a great start..but if fibromyalgia originates from a dysfunctional hypothalamic/pituitary axis due to cortisol levels being chronically high…why not call fibromyalgia by a more probable name of ” Thyromylgia”…I’m a believer that if thyroid dysfunction is not treated correctly you have a downfall in all the rest of the hormones, muscles and organs in your body because of dysfunctional immunity! There are not enough doctor’s knowledge of all about how important thyroid function is to our bodies…what will it take toget our Drs more zoned in…and to consider all this put together for them. It is such a disservice to us all! Time to zero in on causes..not more new drugs as a bandaid! As a research nurse and a fibromyalgia patient myself, it really upsets me to see the endocrinologistignore major blood test and to stick by the pristine test of the TSH… people need to move outside the box and expand their minds and not practiced medicine from what they learned 20 years ago I see it all the time and it makes me so angry but they are not willing to expand their thought process 2 more possibilities of the causes of our immunity diseases!
Marilyn, you are right, many patients with FM and ME/CFS for that matter, have thyroid issues of some sort explaining many of Wolfe’s polysymptoms…. urgh. However, not all patient do, though I suspect thyroid resistance, which is NOT considered because so few really know what it is our how to assess for it, play a key role. For sure, something in the HPA is affecting other body systems, though some are moving away from the HPA hypothesis, for which I am gravely concerned.
Cort, Wyller’s name is not Bernard. His full name is Vegard Bruun Wyller, with Vegard being the first name and Bruun Wyller the family name. His brother, Torgeir Bruun Wyller, is also a doctor, working not with kids and youths as Vegard does, but with the elderly. FYI.
I cant find the study published but Im not that surprised if you artificially dampen the SNS then people feel more tired. What was the time lengths they worked on? I know in my case when I have relaxed my system (using techniques) I feel more tired. But often that tiredness is restorative and feels like a ‘good’ tired – if that makes sense…and my system being more relaxed allows it to actually rest and recover a bit…IMO there could be a long healing time needed even with the SNS activity reduced – to actually have the body starting to feel ‘more’ energetic and to rebalance the multiple endocrine systems that will be depleted after chronic over stimulation-could take several months Id think…thats not to mention – we are tampering with a homeostatic system here with an exogenous drug – the SNS might indeed be hyper aroused for a reason. Just drugging someone doesnt really attend to the root cause…and the list and instance of adverse effects isnt exactly encouraging…
This subject is very interesting to me. I developed CFS after nearly 10 years of experiencing complex post traumatic stress disorder. My gut feeling is there is definitely a connection. I’d just love to understand better what that is. Not surprisingly, when triggers increase my PTSD symptoms, my CFS goes through the roof. What to do though? I’d be interested to hear if anyone has heard of any link between the two.
Klimas and her gulf war syndrome patients are a group of people PTSD that developed CFS symptoms.
Sharon,
Dr Martin Pall, has a hypothesis which links CFS, PTSD,MCS, GWS,FM through the nitric oxide vicious cycle. It is quite complex and he quotes evidence for parts of it.
Martin Pall; Explaining “Unexplained Illnesses”’ Disease Paradigm for Chronic Fatigue Syndrome, Multiple Chemical Sensitivity, Fibromyalgia, Post-Traumatic Stress Disorder, Gulf War Syndrome, and Others (Haworth Press, 2007).
I wish this hypothesis was researched more broadly.
The whole ‘sustained arousal’, ‘dysfunctional stress response’, ‘HPA-axis dysfunction’ etc. theories are based on the assumption that there’s nothing physically wrong with ME/CFS patients. The problem is that even if ME/CFS patients’ ‘stress response’ was activated, it may not be ‘dysfunctional’ at all, but rather entirely functional. If ME/CFS patients’ bodies have problems producing sufficient energy to get through the day, then there are probably backup redundancy-type systems in the body and this might be what is causing the activation. If regular oxygen metabolism isn’t getting it done then patients might have to rely on adrenal activation or similar, which would cause the ‘HPA-axis activation’ or whatever, but as stated above, this in itself is not a ‘dysfunctional’ response, but rather it is an entirely functional response to a truly dysfunctional energy metabolism system. If you took a healthy person and tied huge weights around their arms, legs, head, neck, chest, etc. and told them to go about their business, then don’t you think that that person’s ‘stress response’ would be through the roof?
Wyller is (rightfully, IMO) getting a lot of flak in his homeland due to the fact that before the study began, he was very vocal about how if Clonidine worked, then this would provide strong evidence that his ‘sustained arousal’ theory was accurate. However when the Clonidine trial produces a big goose egg it somehow doesn’t take anything away from the theory at all. Successful trial= theory all but proven, unsuccessful trial= doesn’t damage theory at all. Sorry but that’s the religion of psychiatry, not science. Whatever.
I agree. The stressrespons can be due to low o2 levels and energy. Compensation.
We all (at least in Norway) knew the outcome of the conclution in this trial, even before he began.
John you’re right: “…he (Wyller) was very vocal about how if Clonidine worked, then this would provide strong evidence that his ‘sustained arousal’ theory was accurate”
The medisin failed and he still is stubborn and say: “We still believe that it’s about a sustained stress response in the patient.”
Wyller even say: “…But there is no direct correlation between the stress response and the patient’s ailments”
How perfect to say when you failed to prove.
Wyller is just presenting a hypotese. But it is a dangerous hypotese for many of the patients!
Why does so many patients protest, and saying the treatment does not work, or the patients really get worse?
Question:
Do we talk about / study different diseases?
I do have dysautonomia. In the summer, I have rapid pulse, BP>, faint, GI system spasms causing simultaneous vomiting/evacuation standing upright < 5 minutes or being In the heat. In the winter, I have high BP 260/160. (Had stroke in December) increased pulse, both very intractable to treatment. Team of doctors didn't know how to treat the OI in the summer so went to ER most every week all summer. My autonomic NS is broken. I will have to go off all my BP medicines come summer then back on them in the winter. The only behavior change I have to make is… Quit working, quit driving, stay home in air conditioning all summer, never ever stand in line at the store. That's all. His theory is an attempt to explain the "psychology" of CFS/ME.
That’s really something Linz!
There is a physical cause. Science is just not that interested. No one wants to spend a lot of money and fail, look stupid. ( Too late on the ‘don’t look stupid’ tact.. tsk. .) And too, the environmental insults/possibilities are immense Science has huge political/monetary incentives to skip this disease, and just chemically lobotomize everyone.
Well Kudos to Bruun Wyller for putting his theory to the test and while his blank conclusions that Clonidine doesn’t work sounds a little self flagellating its the only conclusion that can be drawn from the data at present. It doesn’t however disprove his sustained arousal hypothesis and I’d be happy to see him pursue this line of reasoning given that autonomic dysfunction does seem to be a key part of the problem. Even negative findings are useful and we can at least infer from this that it isn’t as simple as blocking sympathetic over-activation.
I did wonder if it might be a dosage issue – I had a similar (but more extreme) reaction to a standard adult dose of a beta blocker but they did use a low dose of Clonadine.
Perhaps part of the problem is an assumption that the sympathetic and parasympathetic arms act like a see-saw and dampening down one automatically lifts the other side? In diabetic autonomic neuropathy though individuals can show mixed patterns with both arms over or under activated.
Alzheimer’s patients apparently have parasympathetic dysfunction associated with acetylcholine deficiency and this causes cerebral hypoperfusion and hence cognitive problems. I don’t know what exactly Clonidine does to acetylcholine or where but there’s some suggestion that it may inhibit brain acetylcholine biosynthesis and some evidence of an association between autoantibodies to ganglionic acetylcholine receptors and severity of autonomic dysfunction .
It could well be that sympathetic overactivation is a compensatory reaction to impaired para function. I certainly wouldn’t throw the baby out with the bathwater just because this particular approach didn’t work.
As always Marco – very interesting. I just heard that a Mayo doctor said that poor blood pressure regulation in orthostatic intolerance causes the ANS to go jhaywire. The problem apparently is that the fluctuating BP confuses it. I’ve heard something similar from Staci Stevens – that it’s not that the SNS is over-activated and that the PNS is under-activated but that the whole system is not responding correctly. I wouldn’t be surprised if your diabetic neuropathy analogy fits.
MERUK’s earlier reesearch showed acetylcholine problems in the skin but I guess it didn’t pan out as they didn’t continue with it.
Thanks : )
I can’t remember all the details but one guide to treating diabetic neuropathy stated not just that early and regular screening was necessary (due to possible implications for morbidity/mortality) but that each individual’s pattern of autonomic dysfunction needed to be characterised and treated appropriately.
So even in a disease as well understood as diabetes drug treatment of autonomic dysfunction will be highly individualised using different drugs and dosages which will probably also need to change over time.
Little wonder that a one size fits all drug regime didn’t help.
Elegantly put John – From what I have read Adrenaline is indeed released as a last resort when the body has exhausted other supplies of energy. I think our bodies get used to using the adrenaline response all the time, so we hardly even notice it, but the long term effects then cause other problems such as heightened anxiety, wired brain, poor sleep etc. Damping down our last resort for energy is going to = no energy.
There might be a role for that type of drug if there was a question of the system being stuck in an “on” position but for it to be effective the underlying energy production problem must be resolved.or managed.
HA! This will be a big blow to Gupta, Phil Parker’s LP and Alex Howard’s Optimum Health clinic psychological therapy, as well as Mickel and Reverse Therapy. Also, some theories delivered in the NHS’s CFS/ME clinics, based on biopsychosocial rubbish. Will they all now give it a rest and actually listen properly to what patients tell them, or still have a skewed theory based on what they think we’re suffering from? No, I don’t think so, but at least patients, advocates and those doctors and scientists on our side, have the science to prove that this theory is what I always knew and that the treatment delivered by the psychobabble peddlars, is just snake oil.
You certainly have a point; they do tend to target an overactive stress response. As long as they’re getting results, though, and at least according to some patients they are getting results, I imagine they will continue. It’s definitely a complex subject that’s difficult to figure out.
As many, perhaps all people with Ramsay defined ME have orthostatic tachycardia and/or orthostatic hypotension/intolerance, then even low doses of Clonidine aren’t going to help. Getting people to increase activity, doesn’t help. There are some good avenues of research, into 2/3 day PEM (bad term), mitochondrial dysfunction and immunology, we don’t need this, but I’m glad it’s been done, as it proves it’s rubbish, just as the underlying theory behind PACE and FINE, is also rubbish. Mood-*feeling smug*
John and MsJustice are right. Wyller started with an erroneous belief — that “strong focus on bodily sensation and poor sense of personal control” describe the typical ME patient. Or was it just people with 3 months of “fatigue”?
If he had bothered to acquaint himself with some real patients he might have instantly seen that his “personality”-as-cause theory is just stupid, stupid, stupid! I remember when we were told we got this because we were “Type A” workaholics with a strong sense of controling our destiny. Was that before or after we were told we were fakers, lazy, malingerers?
Only researchers who actually listen, observe and test real-life patients should have anything to say about mecfs.
Wyller should sit down and shut up, after he admits that his theory has been proven wrong by his own study.
“If he had bothered to acquaint himself with some real patients he might have instantly seen that his “personality”-as-cause theory is just stupid, stupid, stupid! I remember when we were told we got this because we were “Type A” workaholics with a strong sense of controling our destiny. Was that before or after we were told we were fakers, lazy, malingerers?”
Love this!
I don’t believe I have a personality pre-destined to get sick with ME/CFS. Still I did get sick. I think it’s silly to try to put all sufferers of this heterogeneous disease under one description, such as “Type A” personality.
At the same time, addressing my sympathetic nervous system arousal by using mind/body techniques makes a huge impact on my everyday functioning.
This study shows that sympathetic arousal correlates with level of fatigue in ME/CFS:
http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0049518
I agree with one of the comments further down this page that just because this study failed, sympathetic hyper-arousal should not be ruled out as a major contributor to symptoms. In many cases it may not be the root cause, but I still believe that addressing it through mind/body techniques is an important aspect of treating the condition. One of the side-effects of the drug used in this study is fatigue, so I interpret the results of this study as, “due to the drug’s side-effects addressing the sympathetic hyper-arousal through this drug did not help,” and not as “sympathetic hyper-arousal is not an issue.”
I still believe that addressing the hyper-arousal through mind/body techniques is a very important part of treating the condition. I see the big difference it makes every day in myself and my coaching clients.
I can tell from knowing Johannes that of all the people I know, he does NOT have a personality that lends itself to hyperarousal :)…..
Neither do I really 🙂
And if anyone thinks Toni Bernhardt does they’re definitely loo loo.
Damage to the cranial nerves should be looked into .
Low Cortisol, from HPA dysfunction, has been confirmed in many studies of CFS patients. When cortisol is low, adrenaline is secreted to compensate for the low cortisol and the high adrenaline and low cortisol account for most of the symptoms described. Low dose cortisol replacement 5mg-20mg has been found by several researchers to be of benefit to many people with CFS.
It is good to remember that all research has value and many researchers take big risks in credibility when they follow their beliefs instead of at least considering anecdotal evidence before embarking on a research theory. However, I am perswaded by these results that Wyller’s assumptions concerning the cause of Autonomic Dysfuntion are fallacious. He should study the autonomic response in the presence of ischemia. Rule it in or out.
If an underlying cause (or trigger or exacerbating factor or whatever you want to call it) happens to be a toxic exposure, then being motivated to flee from that exposure to somewhere else might have a functional outcome.
http://paradigmchange.me/wp/?p=440
On a side note, I’m really becoming “fatigued” with researchers that claim to be trying to help us but insist on inserting notions of psychological causation into every discussion of this disease.
Despite the many millions of dollars of research money that has been spent trying to prove that this is a psychological illness, all those research studies keep drawing a blank. One after the other.
Maybe it’s time for everyone to put all that psychological stuff aside for a while and start restricting themselves to looking just at possible physical causes.
Since we have some physical possibilities that are seeming increasingly important but haven’t been researched at all yet, I mean.
Best,
Lisa Petrison, Ph.D.
Executive Director
Paradigm Change
http://www.paradigmchange.me
I still believe, based on my own course (hey anecodotal evidence can be the key to any hypothesis!), that it is a prolonged autoimmune reaction that is fed from continued insults to mitochondrial DNA that perpetuate the inflammatory process. The insult might be single (though in most cases I believe it is repetitive stress, i.e. repetitive immunizations like Hep B, MMR, or influenza, or repetitive environmental toxins,inhaled or consumed).
I believe the injuries are multifactorial and dependent on individual predisposition. I believe the “cure” should be directed toward killing the cycle of inflammation→damage→more inflammation.
I believe many of us are affected by nutrient deficiencies not typically sought after by Western medicine.
I believe that symptom-based strategies are just that – they will never target the true etiology of the disease, and even may be harmful in the earlier stages, leading to a false sense of “feeling better” while the damage continues.
I wish there was a study where all of us affected could be whisked away to some “perfect environment” – one devoid of the day to day stresses of life, steady, warm temperatures, no toxins, and pristine nutrition/supplementation.
Such is my humble opinion…
Interesting study.. IMO, coming from someone who has CFS and POTS post EBV being the suspect infection, i do agree with the hypothesis in relation to the body being in a state of over arousal. I know i didn’t solely cause that but i suspect the infectious hit was severe enough on my nervous system to cause the malfunction and symptoms. Also in my opinion just because clonidine’s effects didn’t improve symptoms but made them worse doesn’t debunk the hypothesis in relation to over arousal. Actually i expected that as a result. No surprise.
Clonidine and to mention another, beta blockers, are known to make people more tired. Very tired. Myself included. It put me bedbound for weeks adjusting to a beta blocker in my system for tx of POTS. I believe it takes the edge off but would never solely turn it around. The bodies stress repsonse system, including the adrenals, we know take a long time to rebound, not to mention all the hormones related. I believe no drug will ever turn CFS around. The meds and supplements can only support, take the edge off a body stuck in overdrive. All the hundreds of stories of recovery mention using techniques to retrain the physiology of the body. Like a stroke person learns to walk again, we have to teach our bodies again how to have a balance btw sympathetic and parasympathetic so the ship can sale and all connecting mechansims run smoothely so energy can be restored. Not an easy task being stuck in the dust storm. I don’t take it personal because i see it on an objective level. Lastly, i believe orthostatic intolerance is the result of the ANS stuck in overdrive whether from an infection that cascaded the dynamic or another major trauma to the nervous system. So i take my POTS meds to help me be a tad more comfortable, functional if you will while reworking my physiology back to a healthy state.
Recovery is doable once viewed from an objective viewpoint in retraining our physiology. Everyone has different triggers, sensitvities that keep the dynamic going. If the adrenals are constantly getting punched from innapropriate triggers, then the root cause won’t rebound is how i look at it. Some like myself after the initial insult of infection became very reactive to sound and light so i would be flooded with adrenaline. Some with smells. Some, okay most if not all from the stress of trying to figure out how to feel better and we all strive for results with our efforts. Unfortunately retraining takes time and shooting into the wind blindly until subtle change occurs. That’s why i believe there isn’t a one shoe fits all, but the dynamic malfunctioning is the same.
I appreciate reading others viewpoints too. Just my take on all i have tried, learned, and seen results slowly.
Garbage in, garbage out. Firm conclusions cannot be made from this study one way or the other because of the fuzzy “definition” of CFS used by Brun Wyller. Definition matters. He wasn’t even using the Fukuda definition, much less the CCC or ICC. Where was the requirement that the “CFS” patients have post-exertional neuroimmune dysfunction (PENE – I do not use PEM because of the word “malaise” which is even worse than “fatigue” for vagueness and inaccuracy)? He speaks of those who are “chronically fatigued.” Stop right there if you are thinking of taking this study seriously.
The hypothesis was neither proven nor disproven with this study.
You definitely have a point but I’m going to wait until we have more data on the differences between definitions. I have no doubt that the CCC does target a sicker patient population, but the Brenu study found similar if lesser immune problems in Fukuda vs CCC and the large Vermoulen study found little difference between exercise capability in the Fukuda vs non-Fukuda patients.
Still I wish that he’d at least done Fukuda! The fact that he didn’t seems to me to reflect a stubbornness that is not helpful.
The juries still out in my opinion, but I think we’re going to learn a lot more about this in the next couple of years.
There is a plausible explanation for the sustained stress response in persons with CFS and FMS that researchers have overlooked. Dr. Farrand Robson has developed a system of oral appliances called Oral Systemic Balance that has successfully treated many persons including myself with these and other chronic conditions. What he discovered over years of research and working with patients is that when a person has trouble maintaining “throat” or ease of breathing this results in agitations of the autonomic nervous system. Robson observes this stress in heart rate variability, EKG and heart ultra sound monitoring and has developed a system of oral appliances that reverses this. In the case of CFS the heart is compensating for restrictions in the air passage by lowering its output of blood flow and volume. As a result of this virtually all enzymatic processes of the body go into low gear. The “worse fate” that the sustained stress response is protecting a person from is heart failure. It makes complete sense to me that a drug that increases flow would worsen the symptoms of CFS. I tried taking Clonidine myself years ago and it worsened the agitation of my sympathetic nervous system.
Cort, a question, grateful for help: Is there any solid proof (repeated in large enough studies with actual ME/CFS patients) that there actually is an aroused fight or flight system in ME/CFS?
I think for sure there are. Any study that’s shown reduced heart rate variability suggests sympathetic nervous system over activation. Increased heart rates at rest during rest have also been found several times by other than Wyller, I believe. I believe the same is found in fibromyalgia.
I sustained stress response actually fits in well with the immune problems found in ME/CFS since it should result in reduced Th1 activity and increased Th2 activity.
Well it seems to me like the increase in adrenaline to compensate for POTS symptoms, low blood volume and BP problems in the upright position is a natural compensatory mechanism.
Also I remember Dr Myhill describing all the muscle problems in ME/CFS and since it is all muscles that includes the heart too of course, so she describes this aspect as a cardiomyopathy. If that is the case then the body spurting out adrenaline to compsensate for poor blood flow would make sense IMHO.
What is the cause of low blood volume or weak muscles though is another matter, and even then these are just symptoms of the whole thing probably.
In me the poor cognitive function also causes a spurt of extra adrenaline to help when I have to speed up my brain enough to understand a conversation for example.
Also if you do too much in the day then later on you are more ill and then it is constant adrenaline to help the system compensate.
On the other hand when resting alot there isn’t an excess adrenaline, not in me anyway, but then I am on cortisol replacement.
I did try taking relatively high doses of fludrocortisone a couple of years back and that did help when in the upright position and I didn’t produce as much if any adrenaline at all then so that did fix the “hyperarousal” but I had high BP problems after a couple of years so had to reduce the fludro and now more adrenalne again in upright position ever since.
No, I don’t think this hyperarousal is a big part of this illness, it is just a compensatory symptom imho. Where hyperousal is big is in the minds of psychiatrists it seems…..
RE: some suggest they didn’t take the clonidine long enough for it to work. If this was the case then why is it that all the people with POTS symptoms that are taking beta blocker long term to manage that symptom don’t get better….
I do wonder if some who are posting on here aren’t lightning process practioners et al. and are trying desperetely to defend the hyperarousal hypothesis. Would be great if people were somehow made to declare their conflicts of interest.
Tim