

Small Fiber Neuropathy
In the last year or so we’ve seen four studies published (1,2,3,4) that have found objective evidence of small fiber polyneuropathy in FM patients suggesting that the ‘central sensitization’ theory of FM may be at best incomplete. In fact peripheral nerve damage may be driving pain in FM – but what’s causing the nerve damage?
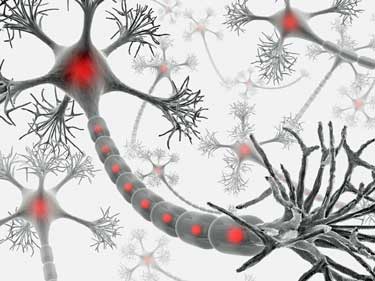
Small fiber neuropathy refers to damage to small myelinated or unmyelinated peripheral nerve fibers found in the skin, peripheral nerves and organs. Damage to these fibers can cause sensory changes (numbness, cold, prickling, pins and needles, enhanced pain, abnormal responses to touch, or loss of sensation). Small fiber neuropathy can also cause enteric (digestive) and autonomic dysfunction (5).
“Patients often do not identify the relationship of these symptoms to their sensory complaints; however, when asked, they may report dry eyes, dry mouth, postural lightheadedness, presyncope, syncope, abnormal sweating, erectile dysfunction, nausea, vomiting, diarrhea, constipation, early satiety, difficulty with urinary frequency, nocturia, and/or voiding.”
As far as I know ME/CFS patients have yet to be tested for small fiber neuropathy, but many patients complain of widespread pain and allodynia. Several studies have now confirmed autonomic dysfunction in ME/CFS patients, and this may well play a central role in the condition.
Small fiber neuropathy isn’t exactly rare, nor is the cause easily identified (5) :
“Peripheral neuropathy is an expanding public health problem, seen in nearly 40 million individuals in the United States. Many of these individuals will have specific damage to small myelinated and unmyelinated nerve fibers, either in isolation or in combination with injury to larger myelinated nerve fibers.
There are a variety of diseases that may result in a small fiber neuropathy, including diabetes and other glucose dysregulation syndromes (e.g., impaired glucose tolerance and metabolic syndrome), thyroid dysfunction, sarcoidosis, vitamin B12 deficiency, HIV, neurotoxic medications (including many chemotherapeutic agents and antiretroviral agents), celiac disease, paraneoplastic syndromes, and paraproteinemias.
We can now add Gulf War Illness to the above list. GWI is another ‘chronic multi-symptom syndrome’ with symptoms that overlap extensively with (or may be considered co-morbid with) ME/CFS and FM. In a recent small study, a disproportionate number of GWI patients, when tested, had either small fiber neuropathy or various autonomic dysfunctions such as orthostatic hypotension or POTS in addition to self reported ‘post-exertional fatigue’ (6)
“Despite extensive diagnostic evaluation, up to 50% of individuals with small fiber neuropathy ultimately may be given a diagnosis of “idiopathic”. Regardless of the underlying etiology, pain is a common and often problematic feature of small fiber neuropathies. Therefore, therapy is tailored toward identification and treatment of the underlying cause of the neuropathy, when possible, while simultaneously managing symptoms of pain.”
The Diabetes Connection
Beriberi
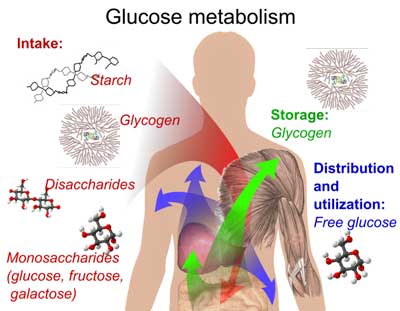
One of the diseases most associated with neuropathies is beriberi which results from a deficiency of the B1 vitamin (thiamine) which is involved in a wide variety of glucose metabolism-related and neurological functions. Excessive urination means that diabetics excrete vitamin B1 in such high amounts that their B1 levels are 75% lower than normal.
Benfotiamine (a fat-soluble thiamine analog) is commonly used to counter peripheral neuropathy in Germany (7). The ME/CFS and FM patients reporting improved symptoms using high-dose B1 supplements were improving their glucose (as well as fat) metabolism and neurological functioning.
Diabetes and Related Disorders – The High Sugar/Low Energy Connection: a Short Primer
As stated above, small fiber neuropathy is a frequent additional problem in diabetes and other disorders of glucose regulation including metabolic syndrome (which one CDC ‘community’ study has linked with ME/CFS).
In essence, diabetes is a disorder of energy metabolism. The body (including the brain uses up about 25% of the total energy when the body is at rest) relies on blood sugar (glucose) to provide cellular energy. The insulin hormone transports glucose from the bloodstream into the cells. When insulin is impaired, as in diabetes, blood sugar (glucose) levels become too high.
Most of the attention in diabetes is focused (and rightly so) on the devastating effects that high blood sugar can cause, but what is often missed is the fact that untreated diabetes is a state of energy deficiency. After all, if insulin does not move glucose into the cells, the cells lack the energy they need to function properly.
A Spectrum Disorder
Diabetes is not just one disorder but a ‘spectrum’ of disorders involving glucose regulation including:
- Type I is perhaps most familiar to the layman as an autoimmune disease that attacks insulin-producing pancreatic islet beta cells, with patients requiring regular insulin injections to regulate blood glucose levels.
- Type II diabetes (T2D) is often seen as a ‘lifestyle’ related form of diabetes where factors including obesity and lack of exercise lead not to a shortage of insulin but to insulin resistance that interferes with signaling; i.e., the insulin is present but the body is not responding to it.
- Metabolic Syndrome (or pre-diabetes) is a disorder affecting glucose use and storage associated with abdominal obesity, elevated blood pressure, elevated fasting plasma glucose, high serum triglycerides, and low high-density (‘good’) cholesterol (HDL) levels. Neither T2D nor Metabolic Syndrome initially require insulin supplementation and are usually managed by lifestyle changes.
- ‘Type III diabetes’ – “Diabetes of the Brain” – is not yet universally accepted by the wider medical community, but some evidence suggests that Alzheimer’s disease may result from a similar problem with glucose metabolism in the brain causing oxidative stress, mitochondrial dysfunction, and neuroinflammation. A ‘diabetes of the brain’ condition involving insulin deficiency or insulin resistance may be a risk factor for developing a variety of neurodegenerative diseases.
- LADA (Latent Autoimmune Diabetes of Adults) or Type 1.5 diabetes. Also referred to as slow onset type I diabetes, it shares a similar autoimmune etiology to type I diabetes, but first appears in older adults rather than in juveniles or young adults. Insulin treatment is eventually necessary, but due to the age of onset it may be misdiagnosed as T2D (even though many with LADA are slim and/or of normal weight). There is often a family history of autoimmune diseases including Hashimoto’s Disease (autoimmune hypothyroidism) and Celiac Disease.
- ‘Type IV diabetes’ — One author has proposed a ‘Type 4 diabetes’ as underlying a range of chronic conditions including FM in which either insulin insufficiency or insulin resistance may result in high blood sugar levels but low cell sugar levels (glucose energy not getting to where it’s needed, including the brain, which he terms ‘hypoglycellia’) with the implication that higher blood glucose levels may be needed to compensate. This is a highly speculative concept with little or no current scientific support
Diabetes and ME/CFS or FM?
Common Symptoms
Why discuss diabetes in the context of ME/CFS or FM (or other ‘chronic multi-symptom syndromes’ for that matter)? We don’t normally think of these as metabolic diseases. Anecdotally we do seem to have problems with blood sugar regulation, share some early symptoms of diabetes (dry eyes and mouth, frequent urination), plus physical and mental fatigue and exercise problems in ME/CFS and FM suggest some (unidentified) problem with energy metabolism. One theory suggests that an altered metabolic stress response in ME/CFS patients results in the ‘selfish brain’ starving the peripheral organs and muscles of glucose. Again anecdotally, one prominent ME/CFS physician has mentioned a high frequency of diabetes in his patients.
Avoiding the immediate and long-term consequences of poor glucose management is a priority in diabetes, with treatment centered on maintaining a delicate blood/sugar balance. There are serious medical issues facing diabetics from mismanagement of their blood sugar levels. In the short term, missing medication can result in diabetic ketoacidosis or diabetic coma, while over-medication can result in hypoglycaemia. The longer term consequences of poor glucose control (diabetic neuropathy, retinopathy, low grade systemic inflammation, cardiovascular problems etc) can be severe.
What may be discussed less often are the daily consequences of the inability to efficiently extract sufficient energy from blood glucose, such as fatigue and exercise intolerance.
Fatigue and Exercise Intolerance
Chronic fatigue levels are high in Type I diabetics, but surprisingly (according to one recent study) not necessarily associated with blood glucose levels. Patients with ‘co-morbidities’ such as neuropathy, nephropathy, pain, and cardiovascular disease reported higher levels of fatigue (8).
Type II diabetes patients also suffer from fatigue, early onset of muscle pain, exercise intolerance, and delayed recovery. Similar problems of reduced oxygen uptake during exercise have been found in ME/CFS patients and in Type II diabetics. In Type II diabetes, oxygen uptake is delayed in response to exercise and prolonged after exercise, and this may depend on vascular/endothelial function in skeletal muscle (which appears to be impaired in T2D) (9)
Other studies (10) have found exercise intolerance was linked to variables such as impaired heart rate recovery (where the heart rate does not slow as expected after exercise – a sign of autonomic dysfunction). Vigorous exercise can result in either hypo or hyperglycemia in an individual depending on medication status, type of exercise (aerobic or anaerobic) and type of diabetes (11).
Hormone Connection
Leptin, one of the hormones implicated in diabetes, is involved in appetite regulation and fat storage. Increased leptin levels tell the body that you’re fully fuelled allowing you to increase your energy level, metabolism, and mental sharpness. Low leptin levels tell the brain that you need to eat, slow your metabolism, and reduce your mental sharpness. Leptin is also an anti-depressant that reduces neuronal excitation.
Just as you can have insulin resistance, chronically high leptin levels can result in leptin resistance. Women generally tend to have two to three times the level of men, and leptin levels are very high in obese women. High leptin levels that were correlated with fatigue days suggested leptin could be playing a role in ME/CFS. Chronically elevated leptin levels are a marker of inflammation.
Low leptin levels, on the other hand, were associated with a wide and impressive list of self-reported symptoms and disease severity in Fibromyalgia in one study. Another FM study found reduced leptin levels in FM that were not associated with disease severity. A third study found no difference in leptin levels.
Low levels of leptin have been found to correlate with mental decline in Alzheimer’s disease.
It now appears that leptin may be closely tied to energy metabolism, and may even reverse diabetes in the absence of insulin (12).
Autonomic Nervous and Immune Systems
Fibromyalgia, chronic fatigue syndrome, and diabetes are all associated with low heart rate variability (HRV) (enhanced sympathetic nervous system activity). Low HRV in diabetes is believed to originate in damage to parasympathetic nerve fibers in the vagus nerve. Low HRV in diabetes has long been thought to be an early marker of later autonomic neuropathy and is associated with both large and small-fiber neuropathy (34).
The fact that low HRV often predates diabetes and is commonly found in ME/CFS and FM suggests ME/CFS and FM patients should take care with their diet and, to the extent they can maintain some sort of mild exercise regimen. (34)
Lower HRV in diabetes is associated with the pro-inflammatory cytokine IL-6. Insulin resistance is associated with increased levels of IL-6, TNF-a and c-reactive protein. It’s not clear if this low-grade inflammatory state contributes to insulin resistance or vice versa, but the fact that all three inflammatory markers have been found in some ME/CFS studies suggests a similar type of inflammation could be occurring.
Higher IL-6 levels appear to increase the risk of coming down with ME/CFS after infectious mononucleosis and to higher fatigue and emotional distress. Lastly, recent research suggests natural killer cell functioning including reduced cytotoxicity is impaired in diabetes. Impaired NK cell cytotoxicity is common in ME/CFS.
The findings underscore the multidimensional impact a low-grade systemic inflammatory state involving the innate immune system may have in various diseases.
Cognitive Deficits
One review (13) of cognitive deficits in Type I diabetes identified the following:
“In patients with type 1 diabetes, cognitive dysfunction is characterized by a slowing of mental speed and a diminished mental flexibility, whereas learning and memory are spared. The magnitude of the cognitive deficit is mild to moderate, but even mild forms of cognitive dysfunction might hamper everyday activities since they can be expected to present problems in more demanding situations.”
The slowed thinking and problems with ‘mental flexibility’ found in ME/CFS and FM appear to mirror both research findings and subjective experiences in ME/CFS. As with patients with diabetes, memory is not the issue. (‘Memory problems’ in ME/CFS generally reflect difficulties processing information; if the information was processed correctly in the first place, people with ME/CFS would probably be able to remember it.)
Another type I diabetes study (14), however, also suggests “impairments in executive function, language, general intelligence, perceptual organization, and memory.”
A recent study of cognitive decline in Type II diabetes patients (15) suggests this decline may be due to brain atrophy of the type usually seen in Alzheimer’s Disease (rather than vascular lesions) apparently supporting the concept of ‘Type III’ diabetes discussed above.
Interestingly, ‘major’ changes in glucose regulation may not be necessary to cause brain damage and cognitive decline. Frequent spells of mild hypoglycemia may be all that’s needed to induce microglial activation and neurodegeneration in diabetics (16).
Depression and Anxiety
High levels of distress, anxiety, and depression have been found in type I and II diabetics (17) and some report rates of depression 3 times higher in Type I and twice as high in Type II diabetes compared to the general population.
“The connection between metabolic disturbances and neuropsychiatric disorders has been strengthened by recent and ongoing human clinical studies, which document numerous and complex interactions between metabolism and the brain. For example, individuals with depression have an approximately 60 percent higher risk of developing Type II diabetes. Conversely, individuals with diabetes are at an elevated risk of developing depression.” (18)
In the context of diabetes related cognitive and mood problems and the possibility that neurodegenerative conditions such as Alzheimer’s and Parkinson’s may be ‘Type 3 diabetes’, a number of diabetes drugs that improve insulin signalling can cross the blood-brain barrier and may be effective in treating these conditions (19).
More directly, researchers have recently been awarded $1.7 million for a clinical trial to see if intranasal insulin (nicely non-invasive) might help with cognitive and other ‘multi-symptom’ problems in Gulf War Illness (20).
“Previous studies of other cognitive disorders, led by researcher Suzanne Craft of the Seattle VA, have found that intranasal insulin improves memory, attention and mood, reduces neuroinflammation, and modulates cortisol levels. Intranasal administration has the advantage of direct access to the brain through the nasal cavity and avoids problems associated with orally administered medications that require higher dosages to cross the blood-brain barrier, making it a potentially effective and safe treatment option.”
Fibromyalgia or ‘fibromyalgia-ness’ in diabetes
Fibromyalgia appears to be a frequent ‘co-morbidity’ in type I and type II diabetes (21) while a large scale comparison of the symptoms of peripheral neuropathy and fibromyalgia concluded that, while both conditions have a specific character, there is considerable (20-30%) overlap (22).
Long-term Consequences
Systemic inflammation
Returning to long-term consequences, chronic elevation of glucose levels can result in a familiar mix of systemic low-grade inflammation, oxidative stress, and mitochondrial dysfunction impacting on endothelial function and arterial stiffness with increased risk for cardiovascular problems.
Arterial stiffness has been found in both chronic fatigue syndrome and fibromyalgia.
Despite obvious cellular stress, the usually mitochondria-protecting heat shock protein response is compromised in diabetes (23) and appears to be the case in ME/CFS. Heat shock protein production appears to be very low in newly diagnosed T1 Diabetes.
Pain
A chronic inflammatory state appears to be the cause of the peripheral neuropathy in diabetes and the resulting neuropathic pain and could underpin widespread pain in FM and ME/CFS.

Some types of pain in fibromyalgia and diabetes are similar and some are different, but the dorsal root ganglia may be involved in both
Interestingly, the experience of pain varies widely in diabetics, with some barely troubled while in others it may be ‘devastating’. One study of Type II diabetes suggests that a toxic byproduct of glucose metabolism – methylglyoxal – may mediate pain. Methylglyoxal levels were higher in T2D patients compared to healthy controls (as would be expected) but also higher again in those patients with pain compared to those patients without pain, despite the two groups having similar neuropathic deficits. This suggests that methylglyoxal was
“not a general marker of diabetic neuropathy, but was specifically associated with pain.”
Methylglyoxal appears to increase the excitability of spinal dorsal root ganglia (DRG) sensory neurons, which could cause ‘central sensitization’ of the higher central nervous system (24). Dorsal root ganglia excitation appears to play a role in the increased pain in Fibromyalgia.
Diabetic and Cardiovascular Neuropathy
In addition to peripheral neuropathy, autonomic neuropathy (diabetic autonomic neuropathy – DAN and cardiovascular autonomic neuropathy – CAN) may develop with again familiar physiological findings (increased sympathetic nervous system activity, reduced heart rate variability, POTS, etc.) (25). Due to the risk of sudden death (eek!) the potentially beneficial effects of exercise must be carefully weighed against the risks in patients with CAN and any exercise program must be individually tailored and carefully monitored (26).
Autoimmunity
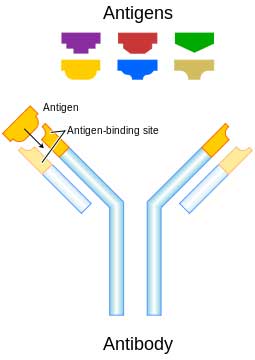
Autoimmune diseases can strike quickly. Autoimmune processes in diabetes can increase glutatmate levels
The autoimmune variants of diabetes (either Type I or LADA) can appear suddenly or insidiously. Both FM and ME/CFS have been tenuously associated with autoimmunity and the evidence thus far is indirect, but autoimmune diabetes tends to cluster with other autoimmune conditions such as lupus, autoimmune thyroiditis, and Sjogren’s, and a similar ‘clustering’ may occur in patients with FM.
Autoantigens in autoimmune diabetes may have intriguing overlaps with FM and ME/CFS. As stated above autoimmune diabetes results in the destruction of insulin-producing pancreatic beta cells. Autoantibodies in both Type I diabetes and LADA increase glutamate levels by attacking the rate-limiting enzyme (glutamic acid decarboxylase – GAD65 or GAD67) that converts glutamate to GABA. Extracellular excitatory glutamate, in turn, has been shown to cause apoptosis of the pancreatic beta cells that produce insulin (27).
Antibodies to GAD would be expected to result in an excess of excitatory glutamate over inhibitory GABA, which may not only impact on insulin production but may also ramp up pain transmission. Some time ago I wrote about the autoimmune disease Stiff Person Syndrome where autoantibodies to GAD65 result in a condition where minor stressors (sudden loud noises, emotional stress, etc.) can trigger severe muscular spasms.
Low serum GABA levels have also been found in FM and various GABAergic or glutamate-blocking drugs have been a mainstay (although not always effective) treatment in FM. Low serum GABA is also found in diabetes and, while exogenous GABA supplementation does not cross the blood brain barrier, serum GABA levels in diabetes do appear to correlate with levels in cerebrospinal fluid. This may explain the high levels of ‘distress’, anxiety, and depression seen in diabetes.
Supplemental GABA has been shown in a rat model (with human trials planned) to prevent and even reverse established diabetes (28).
One intriguing possibility relates to the normally protective heat shock protein (HSP) response that is compromised in both ME/CFS and diabetes. It appears that the anti-GAD65 antibodies found in both Type I diabetes and LADA have a similar amino acid structure to HSP65 and may cross-react with mycobacterial HSP65. This suggests an autoimmune process may affect both GABA and the heat shock protein response (29).
Microbiota – Focusing on the Gut.
While I’m speculating, many of you may already know that the famous ‘virus hunter’ Ian Lipkin seems to feel that the gut microbiome (the billions of resident-commensal, probiotic and pathogenic bacteria in the gut) may be ‘ground zero’ in the inflammatory state of ME/CFS and has just made a public appeal for the ME/CFS community to ‘crowd fund’ a $1 million study.
It increasingly appears that the balance of the microbiome can profoundly affect the body and brain with major implications for human health (30):
“Bidirectional communication between gut microbiota and components of the gut–brain axis influence normal homeostasis and may contribute to risk of disease. Alterations in gastrointestinal (GI), central nervous system (CNS), autonomic nervous system (ANS), and immune systems by microbiota may lead to alterations in (a) fat storage and energy balance; (b) GI barrier function; (c) general low-grade inflammation (GI and systemic); (d) increased stress reactivity; and (e) increased anxiety and depressive-like behaviors.”
Gut Dysbiosis and Diet
Gut dysbiosis causes inflammation and anxiety. The presence of a gut commensal bacteria that produces GABA (31) suggests that an imbalance in gut bacteria might reduce the production of GABA (which as we’ve seen is implicated in diabetes and pain conditions). Could the root of many conditions involving GABA deficiency be located in the gut?
The microbiome may have particular relevance to metabolic problems such as glucose intolerance, metabolic syndrome, and diabetes with diet implicated in gut dysbiosis (32). One animal study suggests that the impact of dietary gluten on the microbiome may increase the incidence of Type I diabetes (33).
Conclusions
Could ME/CFS and FM be unrecognised or atypical forms of diabetes? Normal findings on routine tests such as fasting blood glucose that easily detect ‘diabetes’ suggest not. (Mine tested normal a few weeks ago despite having occasional allodynia plus other suggestive signs of neuropathy). That doesn’t mean a connection is not present.

Diabetes is not ME/CFS or FM and FM or ME/CFS is not diabetes but intriguing similarities are present
Glucose intolerance, ‘pre-diabetes’ (aka metabolic syndrome) may precede a clinical diagnosis of diabetes. Research also suggests that even moderate fluctuations in blood sugar control (frequent moderate hypoglycemia) may cause brain atrophy and cognitive decline in diabetics. Could frequent moderate fluctuations in blood glucose regulation contribute to the symptoms of ME/CFS and FM?
There are the intriguingly similar exercise test findings in ME/CFS and diabetes, and the possibly high rates of small fiber neuropathy in both diabetes and FM. All three disorders feature high rates of oxidative stress, arterial stiffness, and signs of inflammation. Heart rate variability studies suggest sympathetic nervous system activation in all three disorders. Autonomic nervous system issues are rampant in diabetes and may be central to ME/CFS. The leptin findings in FM, ME/CFS, and diabetes indicate another possible sphere of overlap. Underlying all of this potentially is a similar inflammatory milieu.
Practically Speaking ….
What I would suggest is that, regardless of whether peripheral neuropathies point towards a shared pathology with diabetes or that diabetes develops independently, peripheral neuropathies can often be treated effectively and the underlying pathology identified.
Following on from Massachusetts General Hospital researcher Anne Louise Oaklander’s findings of peripheral neuropathy in a high percentage of FM patients, Mass General is now offering FM patients an objective test for peripheral neuropathy with a small skin biopsy taken on site or through your local physician and sent to Mass General for analysis.
“These findings, confirmed by other laboratories, are the first pathological abnormalities found in fibromyalgia patients. Until now fibromyalgia has been a label based on symptoms alone, meaning no possibility of treating the underlying causes. The new findings linking fibromyalgia to SFPN may make that possible since SFPN is caused by underlying medical conditions that can sometimes be identified and treated effectively.”
“What if skin biopsy suggests that you have small-fiber polyneuropathy (SFPN)?
Identifying the cause of SFPN can help doctors and patients choose better treatments, so we recommend that patients with skin biopsies interpreted as SFPN seek advice from nerve specialists to look for its underlying causes.”
If you have some of the symptoms of peripheral neuropathy, objective testing might just confirm this and identify an underlying and treatable condition.
More information can be downloaded from the Mass General Hospital Neurology website:
… under “Neurology News”…. for fibromyalgia patients.
REFERENCES
1. Small fiber pathology in patients with fibromyalgia syndrome. Uçeyler N, Zeller D, Kahn A-K, Kewenig S, Kittel-Schneider S, Schmid A, Casanova-Molla J, Reiners K, Sommer C Brain. 2013 Mar 9. http://www.ncbi.nlm.nih.gov/pubmed/23474848
2. Objective evidence that small-fiber polyneuropathy underlies some illnesses currently labeled as fibromyalgia. Oaklander A L, Herzog Z D, Downs H, Klein MM Pain. 2013 Jun 5. http://www.ncbi.nlm.nih.gov/pubmed/2374811
3. Hyperexcitable C nociceptors in fibromyalgia. Serra J, Collado A, Solà R, Antonelli F, Torres X, Salgueiro M, Quiles C, Bostock H. Ann Neurol. 2013 Nov 16 http://www.ncbi.nlm.nih.gov/pubmed/2424353
4. Update on laser-evoked potential findings in fibromyalgia patients in light of clinical and skin biopsy features.de Tommaso M, Nolano M, Iannone F, Vecchio E, Ricci K, Lorenzo M, Delussi M, Girolamo F, Lavolpe V, Provitera V, Stancanelli A, Lapadula G, Livrea P. J Neurol. 2013 Dec 24. [Epub ahead of print] http://www.ncbi.nlm.nih.gov/pubmed/24366650
5. Diagnosis and Treatment of Pain in Small Fiber Neuropathy Alexandra Hovaguimian and Christopher H. Gibbons http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3086960/
6. Self-reported post-exertional fatigue in Gulf War veterans: roles of autonomic testingMian Li, Changqing Xu, Wenguo Yao, Clare M. Mahan, Han K. Kang, Friedhelm Sandbrink, Ping Zhai and Pamela A. Karasikhttp://www.frontiersin.org/Journal/10.3389/fnins.2013.00269/full
7. Can Benfotiamine Provide Relief For Patients With Painful Peripheral Neuropathy? Podiatry Todayhttp://www.podiatrytoday.com/blogged/can-benfotiamine-provide-relief-patients-painful-peripheral-neuropathy
8. Chronic Fatigue Common in Type 1 Diabetes Medscape News http://www.medscape.com/viewarticle/809663
9. Skeletal Muscle Deoxygenation After the Onset of Moderate Exercise Suggests Slowed Microvascular Blood Flow Kinetics in Type II Diabetes TIMOTHY A. BAUER, PHD, JANE E.B. REUSCH, MD, MOSHE LEVI, MD http://care.diabetesjournals.org/content/30/11/2880.full.pdf
10. Determinants of Exercise Capacity in Patients With Type II Diabetes. Zhi You Fang, MBBS, PHD, James Sharman, PHD, Johannes B. Prins, MBBS, PHD and Thomas H. Marwick, MBBS, PH http://care.diabetesjournals.org/content/28/7/1643.full
11. Type 1 Diabetes and Vigorous Exercise: Applications of Exercise Physiology to Patient Management Michael C. Riddell PhD, Bruce A. Perkins MD MPH http://www.diabetes.ca/files/Riddell–Final.pdf
12. Leptin-controlled gene can reverse diabetes Science Daily http://www.sciencedaily.com/releases/2010/01/100105125836.htm
13. The Effects of Type 1 Diabetes on Cognitive Performance A meta-analysis Augustina M.A. Brands, MSC, Geert Jan Biessels, PHD, MD, Edward H.F. de Haan, P, L. Jaap Kappelle, PHD, MD and Roy P.C. Kessels, PHD http://care.diabetesjournals.org/content/28/3/726.full
14. Cognitive dysfunction associated with anti-glutamic acid decarboxylase autoimmunity: a case-control study Masahito Takagi, Yasushi Ishigaki, Kenji Uno, Shojiro Sawada, Junta Imai, Keizo Kaneko, Yutaka Hasegawa, Tetsuya Yamada, Ai Tokita, Kazumi Iseki, Shigenori Kanno, Yoshiyuki Nishio, Hideki Katagiri and Etsuro Mori http://www.biomedcentral.com/1471-2377/13/76
15. Brain atrophy linked with cognitive decline in diabetes Science Daily http://www.sciencedaily.com/releases/2013/09/130912093807.htm
16. Recurrent/moderate hypoglycemia induces hippocampal dendritic injury, microglial activation, and cognitive impairment in diabetic rats
Seok Joon Won, Byung Hoon Yoo, Tiina M Kauppinen, Bo Young Choi, Jin Hee Kim, Bong Geom Jang, Min Woo Lee, Min Sohn, Jialing Liu, Raymond A Swanson and Sang Won Suh http://www.jneuroinflammation.com/content/9/1/182
17. Landmark new national study looks at diabetes-related distress, anxiety and depression in Australians with diabetes. Diabetes Australia https://www.diabetesaustralia.com.au/Documents/DA/Media%20Releases/12.05.15%20Diabetes%20MILES%20media%20release.pdf
18. Metabolism and the Brain The Scientist Oksana Kaidanovich-Beilin, Danielle S. Cha, and Roger S. McIntyre http://www.the-scientist.com/?articles.view/articleNo/33338/title/Metabolism-and-the-Brain/
19. Drugs developed to treat diabetes, liraglutide and lixisenatide, cross the blood brain barrier and enhance neurogenesis. Kerry Hunter and Christian Hölscher http://www.biomedcentral.com/1471-2202/13/33
20. BUSPH Researchers Awarded $1.7 million Grant to Test Treatment for Gulf War Veterans’ Illnesses
BU School of Public Health press release. http://www.bu.edu/sph/2012/05/11/busph-researchers-awarded-17m-grant-to-test-treatment-for-gulf-war-veterans-illnesses/
21. Fibromyalgia in diabetes mellitus. Tishler M1, Smorodin T, Vazina-Amit M, Ramot Y, Koffler M, Fishel B. http://www.ncbi.nlm.nih.gov/pubmed/1275649
22. Fibromyalgia and neuropathic pain – differences and similarities. A comparison of 3057 patients with diabetic painful neuropathy and fibromyalgia. Jana Koroschetz, Stefanie E Rehm, Ulrich Gockel, Mathias Brosz, Rainer Freynhagen, Thomas R Tölle and Ralf Baron. http://www.biomedcentral.com/1471-2377/11/55
23. Decreased Expression of Heat Shock Protein 72 In Skeletal Muscle of Patients With Type II Diabetes Correlates With Insulin Resistance. Istvan Kurucz, Ágota Morva, Allan Vaag, Karl-Fredrik Eriksson, Xudong Huang, Leif Groop and Laszlo Koranyi. http://diabetes.diabetesjournals.org/content/51/4/1102.long#aff-1
24. Clues to the Riddle of Pain in Diabetic Neuropathy. Megan Talkington. Pain Research Forum http://www.painresearchforum.org/news/16669-clues-riddle-pain-diabetic-neuropathy
25. Diabetic autonomic neuropathy. Vinik AI, Maser RE, Mitchell BD, Freeman R. http://www.ncbi.nlm.nih.gov/pubmed/12716821
26. Exercise Precautions and Recommendations for Patients With Autonomic Neuropathy Ann L. Albright, PhD, RD. http://journal.diabetes.org/diabetesspectrum/98v11n4/pg231.htm
27. The Glial Glutamate Transporter 1 (GLT1) Is Expressed by Pancreatic β-Cells and Prevents Glutamate-induced β-Cell Death* Eliana S. Di Cairano, Alberto M. Davalli, Lucia Perego, Silvia Sala, V. Franca Sacchi, Stefano La Rosa, Giovanna Finzi, Claudia Placidi, Carlo Capella, Paola Conti, Victoria E. Centonze, Francesca Casiraghi,1, Federico Bertuzzi, Franco Folli and Carla Perego http://www.jbc.org/content/286/16/14007.full
28. Effects Of Gamma Aminobutyric Acid On The Progression Of New Onset Juvenile Type 1 Diabetes. Clinical Trialhttp://clinicaltrials.gov/show/NCT01781884
29. Mycobacterial Hsp65 potentially cross-reacts with autoantibodies of diabetes sera and also induces (in vitro) cytokine responses relevant to diabetes mellitus. Rani PS1, Babajan B, Tulsian NK, Begum M, Kumar A, Ahmed N.http://www.ncbi.nlm.nih.gov/pubmed/24056978
30. Gut–brain axis:how the microbiome influences anxiety and depression Jane A.Foster and Karen-Anne McVeyhttp://fr.scribd.com/doc/155346299/Gut%E2%80%93brain-axis-how-the-microbiome-influences-anxiety-and-depression
31. Intestinal bacteria produce neurotransmitter, could play role in inflammation Science Daily http://www.sciencedaily.com/releases/2012/06/120617142536.htm
32. GenomeWeb Feature: Researchers Scour the Gut Microbiome for Diabetes Associations http://www.genomeweb.com/genomeweb-feature-researchers-scour-gut-microbiome-diabetes-associations
33. Microbiome changed by gluten increases incidences of Type 1 diabetes Science Daily http://www.sciencedaily.com/releases/2013/11/131113182423.htm
34. Heart rate variability and sensorimotor polyneuropathy in Type 1 diabetes. Orlov S1, Bril V, Orszag A, Perkins BA.http://www.ncbi.nlm.nih.gov/pubmed/22357183
35. Lower heart rate variability is associated with higher plasma concentrations of IL-6 in Type 1 diabetes J-M González-Clemente, C Vilardell, M Broch1, et. al. http://eje-online.org/content/157/1/31.long








Hi, neem from India is a good adaptogen that is helpful for many things, including immune system but also regulates blood sugar. I find it helpful as I get low blood sugar issues. It helps both high and low blood sugar.
As is coconut oil too!
I am sure I have seen a study linking Small Fiber Neuropathy also to ME/CFS patients, not just Fibromyalgia and Diabetic patients. I have SFN based on a skin punch test (biopsy) done several years ago. A number of people on Phoenix Rising have shared about having SFN too. There has been research which begins to link factors other than blood sugar levels to this destruction in the nervous system, but I forget the scientific details. Dysautonomia might be the cause or whatever might be causing it.
Symptoms connected with the SFN are not only numbness and shooting pains at times, but also increasing aching brought about through irritating fabrics, elastic, jewelry, etc. When there are fewer and fewer materials you can tolerate wearing, and finally, in some cases, or some areas of the body like the feet, none at all, those are definitely signs of SFN and a proper test is in order. It is true that this particular test is not available everywhere. It is incontestable though (which I like) because it shows a picture of the small nerve fibers in the biopsy, then compares them to a normal level. They literally are dying back, dying out from the ends.
Hi Cecelia
Thanks for mentioning that. All I can find is this paper :
Small Fiber Neuropathy Demonstrated in Pain Syndromes
http://www.painmedicinenews.com/ViewArticle.aspx?d_id=82&a_id=15839
… which includes some ME/CFS patients within the cohort.
It doesn’t seem to have caused much of a stir though as I don’t recall much discussion of peripheral neuropathy in ME/CFS research or clinical circles.
Incidentally I got into this ‘blogging business’ after discussions on PR about various sensitivities (mine is clothes sensitivity) which led to this first blog :
‘Not Fatigue After All’
http://www.cortjohnson.org/blog/2013/01/17/not-fatigue-after-all-new-model-suggests-other-symptoms-explain-chronic-fatigue-syndrome-mecfs-better/
It’s going to be fascinating to see how the SFN thing works out in ME/CFS. I wonder if the burning sensations I feel after exercise could reflect that. We should be hearing from Dr. Teitelbaum and Dr. Sivieri soon about rates in ME/CFS I think.
That sounds promising. Any more details?
Its OK Cort – I see we’ve been down this road before :
http://www.cortjohnson.org/blog/2013/08/06/small-fibe-nerve-study-suggests-new-era-in-fibromyalgia-and-perhaps-chronic-fatigue-syndrome-may-be-at-hand/
Memory issues (sheeesh).
Marco, another good one. You’ve been very busy reading and connecting.
Neuropathy has been a big complaint with many of the POTS people that I talk with. In my family its passed on in the family. Many of us have it. But mine is getting better. I dont have as many issues with it or my POTS. Treating the autoimmune system through different ways (diet, antibiotics, antimalarial herbs, probiotics, and enzymes) is and has made a huge difference with me.
You and I both feel there may be a connection with imbalance between GABA (parasympathetic) vs. Glutamate (sympathetic). One thing I’ve found with myself is anything that ups GABA (Gabapention, nerontin, GABA supplements) makes me feel worse. I’m not sure why this is, since indications are to up it should improve symptoms. Any ideas?
Issie
What seems to be apparent with the rise of many illnesses/conditions is the we are under nourished, overweight and lack excercise. The western diet is malfunctioning and doesn’t help having addictive sugar as a major part of it.
I have to agree. I think diet has a lot to answer for.
Undernourished – from poor diet but also from poor gut functioning, overweight – may be but it wouldn’t be surprising if you can’t exercise. My weight goes up when I overdo it and then eat a lot I guess to reduce the pain, but I wonder about inflammation as well.
Sounds exciting. This link with pre-diabetes feels real. Earlier this year, I switched to a Keto diet which addresses insulin resistance. As a result I experienced significant improvements with my CFS, improved blood test results & improved health in general. I’ve made more progress with my GET regime than expected & continue to loose weight. Metformin has been on my radar for a while. I’d certainly be keen to give it a try.
Very interesting article, Marco!
You mentioned the Lipkin microbiome study – readers might like to know that they can donate to it here:
https://giving.columbia.edu/giveonline/?schoolstyle=5881&alloc=21677
Leave the default choice of ‘Chronic Fatigue Syndrome Gift’ on the drop-down menu and when you get to the next page, put ‘For the microbiome study’ in the message box.
The sooner we donate, the sooner it gets funded and the sooner it starts!
It will only take a year to complete and the scientists are ready to go.
Thanks Sasha and thanks for the link.
I’ve already chipped in for the microbiome study and encourage everyone to do the same.
After all its not every day we can boast a researcher of Lipkin’s calibre and if he feels that the gut is the place to look then I’m willing to back him.
It’s rare to get a scientist of Lipkin’s caliber so interested in ME/CFS. Let’s get this study funded 🙂
Thanks, Sasha – and Marco and Cort
Thanks Issie
I keep chasing this stuff up out personal interest but if I find anything I feel is of more general interest I’ll write it up.
Re the negative effects of GABAergic meds, it does sound counter-intuitive but is this an acute or long lasting reaction?
Despite what I’ve suggested might be contributing to our problems I’ve been personally loathe to tinker with the GABA/glutamate balance. One reason is neuroplasticity. If we do have chronically low GABA levels then its likely that the GABA receptors become exquisitely sensitised and any negative symptoms related to GABAergic drugs may be highly exaggerated . Plus what happens to the sensitivity of GABA receptors and endogenous GABA production over time with exogenous GABA supplementation? What happens when you stop the drugs? Too much uncertainty there for me I’m afraid.
Another issue is whether drugs primarily affect GABA A or GABA B receptors – there are significant differences as I understand it including GABA A having excitatory as well as inhibitory functions (plus faster acting).
For example (again counter intuitively) it appears that GABA A receptors when activated actually inhibit parasympathetic vagal tone and GABA A targeting drugs such as benzos actually reduce heart rate variability and increase resting heart rate :
“A study conducted to evaluate the influence of benzodiazepines on the autonomic neurocardiac regulation in humans found a similar rapid increase in resting heart rate and a concomitant reduction in vagal tone, assessed by changes in heart rate variability.”
http://www.hindawi.com/journals/aps/2011/578273/
In contrast, Gabapentin (where there’s some debate as to its exact mode of action) appears to improve impaired heart rate variability in diabetics :
“Therapeutic doses of gabapentin not only alleviate neuropathic symptoms but also improve cardiac autonomic function in diabetic patients with peripheral neuropathy.”
http://www.ncbi.nlm.nih.gov/pubmed/19195912
In short, its complicated.
My dad, who has neuropathy and diabetes finds Gabapention to be benefical to him. Interestingly enough though, the docs dont think the neuropathy is caused by the diabetes. His dad also had neuropathy and diabetes. I have/had neuropathy but NO diabetes. At one point I ran a touch high, but not ever considered a diabetic. So there may be another connection.
I have found info on leptin and wonder how big a connection this may be. Here is a very interesting article on a possible connection with us.
http://jackkruse.com/hey-lyme-disease-meet-leptin/
Also, found the info on wiki interesting.
http://en.m.wikipedia.org/wiki/Leptin
We are so sensitive to meds, that’s for sure. But I guess I’m one of the daring ones. You wont know for sure what your reaction will be, unless you try something. My motto is: NO CHANGE = NO CHANGES. You might just hit on the right combination. For me, diet is the biggie, but the other things I’m addressing with the immune system seems to be my right direction.
Issie
I have found the diabetes article very interesting indeed because of our own family history with ME. After 14 years of severe ME and 3 years of some improvement, my daughter had a major relapse in 2005. She was horrendously ill and in 2007 she tried to cure herself by going on a ‘healthy diet’ (bacon and eggs for breakfast, eating whole foods that type of thing). But the advice was that she was not to eat sugar, in the belief that this would stabilise blood sugar levels.
But it didn’t work at all, she steadily declined, till in desperation we were pureeing her food in an attempt to get it into her. Eventually however she had to be admitted as an emergency to hospital in 2008 unable to eat or drink, weighing just 5 stone 5. Straight away they found she was hypoglycaemic and started getting sugar into her. She had also stopped producing insulin.
She had a terrible time in hospital; blood sugar swinging up and down and awful reactions to food, she was often very hyper, distressed and demented. She was tested for Addisons Disease because of the symptoms she was displaying but it came out negative. The doctors were never able to find a diagnosis to fit my daughters symptoms.
We slowly came to realise after the hospital admission, that she was unable to process food no matter what food it was without eating sugar but even with the sugar it was still a hard struggle, she was constantly very ill and losing weight.
We have often thought that she might have something fundamentally wrong that involves sugar. She has recently been diagnosed with Gastroparesis (paralysis of the stomach) but the sugar problem seems to be separate from that. She’s dependent on Ensure Juice (an on prescription sugary replacement food drink) to supplement her food but too much sugar can also seem to act like poison and still today she cannot seem to get sugar naturally out of her food at all.
She has lots of other symptoms that might be connected to this and are part of what she describes as her brain pain; including nightmares, insomnia and naps that are more like passing out, of getting hyper, highly distressed and anxious at the same time. She also loses all judgement and has erratic blood pressure and heart rate.
My son who also has ME has similar symptoms and problems with sugar but less severe.
Wow Eilidh
Thanks for posting this but what a horrendous story. If glucose handling problems are linked to ME/CFS then it sounds as if your daughter is a very extreme case.
Gastroparesis does appear to be a symptom of diabetes but it does beggar belief that they still haven’t identified the root problem.
Best wishes to you all.
I’m so sorry for what you and your children have been through Eilidh. So many who post here have been through such horrible challenges.
Re small fiber neuropathy, does anyone know, would a skin biopsy taken from the lower leg, if positive, lead one to think that chest pain could be micro vessel disease if standard heart tests ( nuclear stress test, echo stress test) are ok? I don’t know that there’s any test for the very tiny capillaries that go into the bigger vessels of the heart and from what I understand MVD, also known as Cardiac X Syndrome is more a diagnosis of exclusion/ history and trying long acting nitro, calcium channel blockers and such. If you can find a cardiologist familiar with it. In reading the cardiac symptoms associated with CFIDS on the blog, I haven’t seen actual pain listed but rather palpitations, irregular heart beats, and high resting heart rate.
I believe chest pain is very common for some people with ME/CFS. I had it in the earlier stages…I wonder about those small capillaries and I believe women are more at risk for microvascular problems
Thanks, Cort and Everyone for this discussion. Something that strikes me and is never mentioned is frequent high levels of insulin in ME/CFS after glucose tolerance test. Dr Lewis of Australia frequently finds this, but I have never seen it mentioned anywhere else.
When I had this test earlier in my illness 11/2 hours after glucose intake my insulin was
4 times the normal limit. The glucose level was normal.
I read that this is supposed to be a prediabetic state. I just wonder what is happening there and why it is never considered. Could the ME/CFS people who develop diabetes have gone through this stage without knowing it? Could there be a pancreatic exhaustion leading to the eventual diabetes?
Good post…….Fibromyalgia is the most common musculoskeletal condition after osteoarthritis. Fibromyalgia is a common and chronic disorder. When a health illness or condition is chronic it means it is long-lasting. visit our site for good tertments for Back Pain, Diabetes, Fibromyalgia, Thyroid. http://www.drbastomski.com/
Sounds exciting. This link with pre-diabetes feels real. Earlier this year, I switched to a Keto diet which addresses insulin resistance. As a result I experienced significant improvements with my CFS, improved blood test results & improved health in general. I’ve made more progress with my GET regime than expected & continue to loose weight. Metformin has been on my radar for a while. I’d certainly be keen to give it a try.
Congrats RobW…and continued good luck with your protocol
Cort, after this article dont place a question mark. Place an exclamation. Because all of my reading has independently led me to the same point about blood sugar.
And when Ischemia happens…. hypoxia happens and brain fog happens.
The other definition of hypoxia is “shock”.
You are referring to heat shock.
Its your own article and I believe you have really nailed it.
Thanks Chris! It’s a very interesting possibility!
Test… my last comment maybe didn’t go through?