



“In conclusion, these data support the addition of POTS to a growing number of cardiovascular entities with an autoimmune pathophysiology.” Authors
The Rituximab findings, the female predominance, the increasing evidence of heritability, the inflammatory component, and the common infectious trigger all suggest that at least some people with Chronic Fatigue Syndrome (ME/CFS) may have an autoimmune/autoinflammatory disorder. While these findings point to an autoimmune basis for ME/CFS, no studies have incontrovertibly demonstrated that ME/CFS or some subset of ME/CFS is an ‘autoimmune’ disorder.
A new study on a closely allied illness, postural orthostatic tachycardia syndrome (POTS), however, strongly suggests that POTS is a autoimmune disorder and points to possibilities that could apply to ME/CFS.
If you have POTS, the findings of this study – if validated – could open exciting new treatment possibilities for you. If you ME/CFS and don’t have POTS, I believe this line of inquiry could ultimately provide some answers as well.
Postural Orthostatic Tachycardia Syndrome (POTS)
People with POTS experience high heart rates, fatigue, dizziness, and light-headedness while standing or even at times while sitting. One of the striking things about POTS is how commonly, like Chronic Fatigue Syndrome, infections precede it.
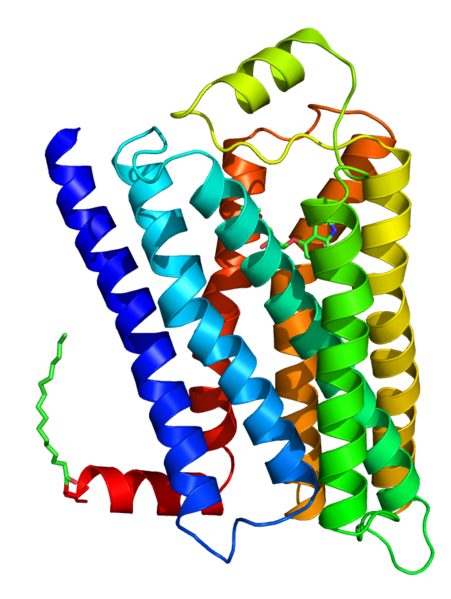
This study looked at autoantibodies to adrenergic (autonomic nervous system) receptors found on the blood vessels and in the heart which control heart rate and blood flow across the body. Two main types of adrenergic receptors, alpha-adrenergic receptors and beta-adrenergic receptors, exist and many subtypes are present (alpha-1, alpha-2A, alpha-2B, alpha-2C, beta-1, beta-2, etc.).
The researchers believed that autoantibodies to the a1 adrenergic receptors (AR-1) responsible for vasoconstriction would prevent blood vessels from squeezing tightly enough to prevent blood from pooling in the legs when POTS patients stood. Other autoantibodies would be implicated in the unusually high heart rates.
They took sera from the patients and controls and then added it to various preparations to see if it triggered cAMP activity, that is, to see if it vasodilated or constricted arterioles. Check this sentence – I changed it a bit.
They found greatly increased levels of autoantibodies to AR-1 receptors in ALL the POTS patients they studied. The consistent findings were remarkable given the heterogeneity believed present in POTS.
With the autoantibodies putting those receptors out of commission, their blood vessels weren’t tightening as they should. As their blood began pooling in their legs, their sympathetic nervous system kicked into gear and produced the racing heart rates characteristic of POTS. A second type of autoantibody appears to produce this result in some patients.
Treatment Implications
The great thing about these findings is that if they’re validated there is the potential of a clear fix: develop a drug to latch onto and block the autoantibodies. In fact, such drugs are under development now.
A POTS Patient in the News
We hope to eventually develop treatments to block these autoantibodies, without blocking the target receptor proteins at the cell surface at the same time. Such agents are in development and within a few years may be applicable in POTS. This approach may prove useful in several other diseases which are caused by similar autoantibodies.
Chronic Fatigue Syndrome Connection?
It’s exciting to see a potentially clear pathway emerge for some people with POTS, but my guess is that these results and these types of studies will also ultimately pay dividends for people with ME/CFS. The disorders may be closer cousins than we think. An identical pattern of altered pH and cerebral blood flow showed up in two separate studies on POTS and ME/CFS patients. When I pressed the ME/CFS researcher on whether she was inadvertently studying people with POTS, she made it clear that she was not. However, the two groups of patients appear to share some striking physiological abnormalities.
An abstract presented at an 2014 autonomic disorders conference indicating that a second tilt table test greatly increases the number of people who meet the criteria for POTS suggests many people are unaware that they have POTS.
My guess is that many people with ME/CFS who don’t meet the criteria for POTS or other forms of orthostatic intolerance still have an undiagnosed form of orthostatic intolerance. These are people who have trouble standing up for long periods, who tolerate exercise much better if it’s done while lying down, who generally think and talk better while sitting or lying down, and who don’t tolerate repeated up and down movements well.
I ‘passed’ a tilt table test with flying colors except for the fact that symptomatically I crashed badly during the test and afterwards, while my twin had no problems. I had to quickly quit a job at a bookstore because the up and down motions produced while returning books to the shelves was too much for my system to handle.
This is still a new field and there’s a lot to learn. One example of that are two studies that found autoantibodies to different adrenergic receptors in another form of orthostatic intolerance.
Orthostatic Hypotension Also Associated with Increased Levels of Autoantibodies
The POTS study was not the first to look for autoantibodies in orthostatic intolerance. Two earlier studies found autoantibodies to adrenergic blood vessel receptors (B2AR and M3R) in orthostatic hypotension.
Your blood vessels should tighten when you stand to counter gravitational blood flow to your legs. In people with orthostatic hypotension, however, inappropriately dilated blood vessels cause their blood pressure to drop when they stand. (The good part of this is that it’s a simple, non-invasive way to diagnose POTS.)
The earlier autoantibody study of orthostatic hypotension found three different patterns of autoantibody activity in six patients, and these three patterns produced three different clinical outcomes. All patients, for instance, demonstrated problems with tightening their blood vessels when they stood, but some also had a blunted cardiac response. This simply suggests that very complex patterns of autoantibodies and functioning are present in these disorders.
It bears noting that increased levels of autoantibodies to autonomic receptors are now associated with a variety of cardiovascular disorders which cause problems with standing, such as hypertension, heart rhythm problems, and heart disease.
The big question now is how much of orthostatic intolerance is autoimmune mediated?
That’s why, even though this research is on POTS patients, I think of it as ME/CFS research; the more attention drawn to the blood vessels and cardiovascular system in POTS and ME/CFS and other orthostatically challenging disorders the better.
Crowdfunding Effort Underway

Help Dysautonomia International crack cause and provide tests and treatments for POTS and other forms of orthostatic intolerance
Dysautonomia International (DI) has launched a crowdfunding effort to take this research to the next level. Their ambitious research agenda includes examining autoantibodies in more POTS patients, developing a commercially available blood test, and, if the findings are validated, they’ll be working to develop new drugs to suppress those autoantibodies that are knocking the blood vessels for a loop.
The DI crowdfunding effort (which was inspired by the Rituximab effort in ME/CFS) is about halfway to its goal of $50,000. Donate during April and your contribution will be doubled due to a matching grant (up to $10,000) from an anonymous donor. DI is over half-way there, and you can make a difference with your donation!








As usual, Cort, a very good blog. I didn’t know much about POTS before, and you made it more clear than other blogs and reports I’ve read.
I just wish you wouldn’t use the term “Chronic Fatigue Syndrome” so much. The sufferers of ME are trying to downplay the name CFS. CFS really isn’t a disease. ME is. I call CFS a misnomer, and so do many ME patients. What are your thoughts on this?
Thanks.
I use Chronic Fatigue Syndrome occasionally (and not nearly as much as I use ME/CFS) out of necessity really. I don’t like using it, but search engine results indicate that chronic fatigue syndrome is a much, much, much more searched for term than ME/CFS. That’s why you’ll often see chronic fatigue syndrome in the title and the upper part of the page where search engines search the most. Titles unfortunately are key to search engine results….so up goes CFS into the most visible part of the blog.
I’ve put ME/CFS in titles to find that those blogs don’t get picked up by search engine. It’s frustrating for me as well. I don’t like the term at all.
I, like most (all?) people with this dreaded disease hate the name Chronic Fatigue Syndrome but find I have to use it much more often than ME since most people have no idea what ME is and when I tell them the full name their eyes glaze over and they lose interest. At least Chronic Fatigue Syndrome they have heard of and that then gives me a chance to explain what it is. I have a fear that even once the name is changed we will still have to refer to it often as CFS since that is what is in the all the research done to date, the internet search engines and peoples brains.
Great blog again Cort. Did Dr. Rowe talk about any of this in San Francisco? I missed that session unfortunately.
He didn’t talk about these antibody results that I remember but he did a fantastic session on OI and treatment. A blog will be coming up.
I still run across people and professionals in the medical industry who haven’t a clue what CFS or CFID stands forso they certainly have no clue about ME. I have to say Chronic Fatigue Syndrome or Chronic Fatigue Immune Deficiency for the ears to listen.
it is what it is, call it what you want. Nothing changes the problems assocaited with it
I agree, if I say CFS or ME most people, including doctors haven’t a clue what I mean until I say Chronic Fatigue Syndrome or Chronic Fatigue Immune Deficiency
Is there a link to the study? My apologies if I overlooked it.
There is now :). Thanks for reminding me – http://www.ncbi.nlm.nih.gov/pubmed/24572257
I read this research a while ago and noticed myself the striking relation that this could have with ME/CFS. I think we’re now reaching a point where a autoimmune sub-group of ME/CFS is being narrowed down and the tie between the autonomic nervous system, cardiovascular system and HPA-axis seems to be central to the problem. I’m glad you wrote this article as this sort of research needs much more attention as it is. to my mind, the most promising avenue of research in ME/CFS we have today.
Hi Everyone,
I personally don’t mind to use CFS & Cort is right it is on the top of the search engine.
I have had CFS and fibromyalgia since 1979 almost 35 yrs.
So I am glad to have the name to Chronic Fatigue Syndrome cause at least Dr.’s are aware of this name “NOW”. When I first got this there was NO name for it & Dr’s would tell me it was all in (my head). That I needed a therapist. So for me it’s ok to call it that. It still is what it is folks. Another name is not going to change what we “DEAL WITH” everyday of our lives…..or by changing the name make us better….You see what I am say? We are still in the same boat…with our symptoms everyday for all the days since it started. God Bless you all. Danielle
AMEN!
I BIG thank you so VERY MUCH Mr. Cort Johnson for this blog & ALL you info…God Bless you for that. Danielle
Thanks Danielle – I appreciate that 🙂
When I got ME/CFS around 1980 there was no CFS. Then when CFS appeared I shunned it because it seemed like there was no hope. Now here I am using it :). There is something to be said about continuity in research.
I was surprised at just how much POTS and ME/CFS overlap.
This is a study of 47 POTS patients, 65% of whom met the requirements for Fukuda CFS (others didn’t met the criteria for reasons such as their problems were lifelong and not new onset) and were termed CFS-POTS.
On a wide range of measures CFS-POTS and non-CFS-POTS patients differed only in the severity of symptoms :
“In conclusion, fatigue and CFS-defining symptoms are common in POTS patients.
The majority of them met criteria for CFS.
CFS–POTS patients have higher markers of sympathetic activation, but are part of the spectrum of POTS. Targeting this sympathetic activation should be considered in the treatment of these patients.
These findings suggest that CFS–POTS is not a separate clinical entity distinct from non-CFS–POTS.
We propose that CFS–POTS is part of the spectrum of this syndrome, associated with greater sympathetic activation and/or a more severe form of this condition.”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3203411/
Boy did that hit the nail on the head! (I wish I’d read it before I wrote the paper – I should have had you proofread it :)). Plus it’s got Biaggioni as the senior author – it doesn’t get much better than that. Who knew? That was three years ago.
Hi Cort and thank you for bringing this research to the attention of the ME/CFS community. I agree with you in that I suspect there are a great many more ME/CFS patients suffering with undiagnosed POTS. My 16 yr old daughter was diagnosed with ME/CFS three years ago and received no treatment other than an appointment every 6 weeks with a psychologist – thankfully there was no CBT or GET on the agenda, just pacing). Last year I pushed and had to fight incredibly hard to have her assessed for POTS and the diagnosis was confirmed following a tilt table test. She has subsequently found benefit from upping her fluid intake, salt loading her diet, using compression stockings and has recently started a trial of fludrocortisone – all, whilst not ‘curing’ her have given her improved functionality, which after three of her teenage years is a really big deal.
Her POTS specialist and neuro now believe the ME/CFS diagnosis should be removed as they believe her symptoms, including PEM, are attributable to POTS. Her ME clinic downplay the POTS and want her to continue attending. So we are left in the position of knowing she had POTS, but unsure if she has ME/CFS or not and no-one seems able to confirm the differentiating symptoms. I always believed Post Exertional Malaise, or worsening of symptoms after physical or mental activity was the unique symptoms associated with ME, but apparently after speaking to lots of POTS patients, this too is experienced by ‘just’ POTS patients and many also refer to it as ‘payback’. If anyone has any thoughts on this, I would be interested in hearing them.
My second point is that whilst infection does commonly precede POTS, so does vaccination. My daughter is one of probably thousands of teenage girls globally who became very ill following their HPV vaccination and many of them are being diagnosed with POTS. Here in the UK, the girls who were lucky enough to escape an outright mental health diagnosis, were often diagnosed with ME/CFS following their HPV vaccination and like my daughter were left to the whims of the ME clinic psychologists, the ‘treatment’ being any permutation of pacing advice, CBT, GET. As we have come together as families of girls injured by the HPV vaccine, we are finding that POTS and autoimmune conditions are a common theme amongst the girls who are lucky enough to have a doctor willing to investigate these areas. Unfortunately, as ME patients in the UK are only too aware, once that label has been applied, trying to get further investigations is near on impossible. My own feeling is that since the HPV vaccination programme was introduced, the incidence of POTS, and particularly autoimmune related POTS will be found to have increased dramatically and I welcome the fantastic initiative Dysautonomia International has shown in taking this research forward.
As a point of note on this, one of the medical advisors to Dysautonomia International, Dr Blitshteyn has published twice regarding her concerns about the development of POTS following HPV vaccination:
http://www.ncbi.nlm.nih.gov/pubmed/24102827
http://www.ncbi.nlm.nih.gov/pubmed/20402758
And a recent paper co authored by Dr Yehuda Shoenfeld, a globally well respected autoimmunity expert, also highlighted concerns about POTS and CFS following HPV vaccination:
http://hic.sagepub.com/content/2/1/2324709614527812.full
Caron, I had a very similar experience as your daughter. I was first diagnosed with CFS, then had to doctor refer me to get a tilt table test and got a POTS diagnosis, which I was told explained the fatigue and replaced CFS. I was skeptical, as I still have a number of symptoms that I didn’t think could be fully explained by POTS, but as I’m learning more about it..I may be wrong. The first few doctors I saw were local cardiologists who seemed to think POTS didn’t cause much more than a fast heartbeat and some lightheadedness, but that’s far from the truth. Even a lot of the more unusual symptoms like food/medication sensitivities, light & sound sensitivities seem to be correlated with POTS as well. I have a specialist now, a neurologist who only treats dysautonomia, and he believes POTS and ME/CFS are part of spectrum of disorders of the autonomic nervous system, which also includes things like interstitial cystitis, IBS, and migraines. Regarding PEM, I’ve wondered about that too, and I’m not sure if anyone really knows. I get PEM too, although it comes and goes. It can definitely be a part of POTS, but not for everyone…so what does that mean? I guess part of the problem is that, like ME/CFS, it’s a syndrome, not a disease, so there are different subsets of patients. If this latest autoimmune research plays out then it may just be an issue of different antibodies for different forms of POTS, and someone’s severity/set of symptoms will depend on which antibodies they have.
I’m a bit ashamed to admit this on here, but I generally just claim the POTS diagnosis rather than ME/CFS because it’s much more readily accepted, both by medical professionals and the general public (people rarely know what it is, but at least if they Google it they get info about a nervous system disorder instead of the vague and sketchy controversy on CFS). If POTS is proven to be autoimmune, things will only get better. And I hope that will extend to ME/CFS as well, because there is clearly a strong connection.
Very interesting info on the HPV vaccine as well, and I’m so sorry that happened to your daughter. I’m a bit older than her and got the HPV vaccine the first year it was out. Thankfully, no reaction, but I’ve heard horror stories since then. I guess they’ve started giving it to boys as well – my GP’s nurse’s nephew had a Gullian Barre-like reaction to it and has permanent damage to the nerves in his legs. I’ve heard of lot of bad things about that vaccine, some of it from medical professionals themselves – it’s amazing it’s still so widely used.
What a story Caron. I’ve always been struck by the symptomatic overlap between orthostatic intolerance; it’s almost identical and my guess is that when they get down to it at some point there are going to lots of similar underlying factors. I’ll bet these diseases are all permutations of each other – which is why I find what Dysautonomia International is doing so exciting. I hope they can raise their $50, 000…
“Her POTS specialist and neuro now believe the ME/CFS diagnosis should be removed as they believe her symptoms, including PEM, are attributable to POTS. Her ME clinic downplay the POTS and want her to continue attending. So we are left in the position of knowing she had POTS, but unsure if she has ME/CFS or not and no-one seems able to confirm the differentiating symptoms. I always believed Post Exertional Malaise, or worsening of symptoms after physical or mental activity was the unique symptoms associated with ME, but apparently after speaking to lots of POTS patients, this too is experienced by ‘just’ POTS patients and many also refer to it as ‘payback’. If anyone has any thoughts on this, I would be interested in hearing them.”
Hi Caron, I have both severe ME and severe POTS and do find I can differentiate between crashes between the two. When I crash with POTS, the symptoms build up during the activity and just build up more and more until I go and lay down (or rest legs up). So the POTS crash for me happens during or happens at a point where Im doing the activity and then continues on, how long it continues on depends on how bad Ive POTS crashed eg I can be still sick the next day from the OI incident (obviously in need of a drip!) if I got to the point where I went unconscious due to the POTS or collapsed.
Some may be saying they get post exertional fatigue with their POTS due to the symptoms continuing on long after it takes to recover from normal activities eg bad POTS crash can have one still feeling crap the next day etc so on.
ME/CFS however, thou post exertional symptoms are symptoms which comes in much later eg 18-36hrs later.. its more like one is thier normal sick self and then get a sudden extreme delayed reaction. POTS crashes are far more predictable then ME/CFS crashes (due to build up in symptoms.. where as ME/CFS can just suddenly hit the next day as if out of the blue if one didnt know to relate a sudden crash to the day before).
I too think many who have POTS may in fact have ME/CFS and have POTS as a coexisting condition.. and those of cause would have the delayed post exertional response (of the type it hits the next day).
Thou there is a lot of overlap in symptoms seeing POTS is an autonomic system disorder which hence affects many different body symptoms, I may be wrong but I think there may be some ME symptoms which dont appear in purely POTS people eg swollen glands, sore throats, fevers and things like those may be able to distinguish between those who just have POTS and those who have ME/CFS AND POTS.
Hello Tanya I hope you are ok…I don’t know if you will ever see this and I do wish you all the best…it’s been a long time since we spoke last… David
I was diagnosed with ME/CFS and POTS. About 13% of the people with CFS have also(?) POTS it is a novel subgroup. I think you can have both ME and POTS because there are different immune problems in ME. We must wait till this anti-body test is available.
It is my understanding that POTS has LOW BP when standing – and that is the reason for the dizziness, etc.
I have all the symptoms, but my BP RISES when I stand still, to dangerous levels, and my heartrate goes up. 195/130 with 88 heartrate, just for standing still for 3 min. From completely normal 125/75 when lying down or sitting.
Is there a name for this? I hate to get involved with yet another doctor who doesn’t know anything about CFS – how do I pick a cardiologist?
24 years of this nonsense so far.
Hi, Low BP is not specific for POTS butTachycardia. You can have hyperadrenic POTS.
Actually the standard definition of POTS is that there is no drop in BP, although doctors are now recognizing that someone can have POTS and NCS so it gets a bit more complicated. And as Gijs mentions, there is a form of POTS, hyperadrenergic POTS, that’s almost always accompanied by a rise in blood pressure. I’m not sure if your heart rate is high enough to be POTS-related (unless it continues to rise), but definitely worth looking into, as there are a number of options available for managing dysautonomia. Check out the physician list on http://www.dinet.org/index.php/physician-list for doctors that may be able to help – may be a cardiologist or neurologist.
I don’t what you have Alicia but here you are in what I think of as the ‘cardiovascular subset’ – your autonomic nervous system goes kablooey when you stand. It’s fascinating stuff. I would contact Dysautonomia International and see if they can recommend somebody.
Thanks, Cort! Great blog. This means hope. I’ve realised that fixing POTS takes away about half of my ME/CFS symptoms. It’s hard though to find something that works in the long run so this research is extremely welcome. This could bring relief to many of the most severely ill. Interesting to see that this too seems to be about immunity.
I’m one of the HyperPOTS people. I have a rise in BP with standing and a hike in pulse rate. There is still a drop that happens with bp, but it starts from a higher level. Lots of times it doesnt get caught because it can happen fast and then the tachy kicks in to bring it higher, when it really doesnt need to be higher. Many of us with this form of POTS also have EDS and MCAS. Its a triology that goes together. This is probably a compensatory response and very necessary, but it sure gets tiring and hard to handle.
How longgggggg have I been saying this is autoimmune and inflammation related. Glad more research is going into it. Nice that docs are listening to us. My addressing it from this angle has helped me more than anything else I’ve done.
I also feel a vaccine triggered mine, a polio vaccine, when I was about 8 years old.
But it seemingly has a genectic component with our family. My sis has OI and CFS and all three of her kids have POTS and one has EDS and MCAS. We think my grandmom had POTS too. So that makes me think it could be something passed on even in pregnancy. Lyme disease or co-infections and other protozoa, maybe??? This could still be explained by a faulty immune system, not recognizing what it should, and destroying it. End results, lots of inflammation.
Issie.
They should definitely study your family :). I wonder if you can get into the Dysautonomia study…
Sign me up!!!
Issie.
Thanks Cort for an excellent summary of the Vanderbilt/Oklahoma study. As someone living with POTS and the daily limitations it creates, the progress made by this team is extremely exciting. When looking at the list of diseases caused by autoantibodies – SLE, myasthenia gravis, Hashimoto’s, graves, stiff person syndrome they all can have POTS as a symptom or co-current condition. Hopefully the research will continue to provide answers and help improve the lives of CFS/ME and POTS sufferers. Thank you to all those involved.
Cort, I am interested in the studies you mentioned that assoc autoantibodies with ortho intolerance – that is the prior studies.
Also, any further info you have on the stage of development of specific treatment. – ie that it is only a few years off.
Thanks,
If you look up the same authors on this study on Pubmed the other two studies will pop up. I don’t know about specific treatments, one paper said they are under development in some labs. It sounded like a couple of years but I’m not sure. Getting more studies validated will surely spark more interest. I hope DI can get their study funded. 🙂
This is probably the best summary of the study to date. Great work.