



“The impact of this paper is that it will be exceptionally important to reach out to primary-care doctors, to rheumatologists, and to fibromyalgia centers to present this information and experience and encourage them to do a screening. It’s not widely appreciated.” Dr. Mira Milas
The Vague Definition Syndromes
Symptom-based definitions involving pain and fatigue have a problem: they can fit a lot of people, and that means subsets abound.
If you have them and don’t get a thorough workup at your doctor’s office something could be missed. According to a recent conference report from Medscape News that something in Fibromyalgia includes a very treatable condition called hyperparathyroidism.

Sometimes doctors just don;t know. Most doctors do not screen for hyperparathyroidism in Fibromyalgia
As with orthostatic intolerance, thyroid and adrenal problems, small fiber neuropathy, and other disorders, the symptom overlap between FM and hyperparathyroidism is huge. People with either disorder commonly experience fatigue, musculoskeletal pain, headache, cognitive dysfunction, and mood disturbance. Both disorders are more common in women, and both increase with age.
A large study of over 2,000 people found that 4% of people diagnosed with primary hyperparathyroidism or PHP also had been diagnosed with Fibromyalgia. Since many FM diagnoses are probably missed that percentage is probably low.
Another smaller study found that 10% of FM patients had hyperparathyroidism. With the average incidence of hyperparathyroidism in the general population of .5%, it appears that hyperparathyroidism is greatly over-represented in FM patients.
If these numbers are correct, from 240,000 to 600,000 people with FM in the U.S. could have a treatable condition, and treatment could decrease their symptoms or, in some cases, eliminate them.
An FM and ME/CFS Rule of Thumb
Because Fibromyalgia gets a lot more attention than Chronic Fatigue Syndrome, ME/CFS probably gets lost in the mix. The large symptom overlap between Fibromyalgia and ME/CFS and the tendency of some doctors to call all pain and fatigue disorders “Fibromyalgia” means any factor in FM may apply to a significant number of people with Chronic Fatigue Syndrome (ME/CFS) and vice versa.
Hyperparathyroidism
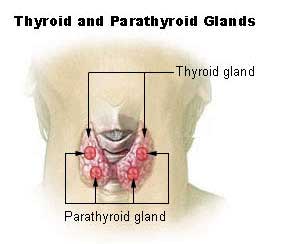
The parathyroid glands are small endocrine glands found in the neck on the back of the thyroid gland, and their purpose is to regulate the amount of calcium and phosphate found in the blood and the body. A hormone they release called parathyroid hormone (PTH) breaks down bone to release calcium. Too much calcium release can cause fragile bones and a variety of other problems. The parathyroid also regulates calcium absorption in the gut by activating Vitamin D.
Besides the role it plays in strengthening bones, calcium also aids in the transmission of signals in nerve cells and in muscle contraction.
Hyperparathyroid symptoms are rather general, involve pain, and could easily lead to a misdiagnosis of Fibromyalgia. Note that FM patients also appear to have an increased incidence of hyperparathyroidism, and this may further confuse the diagnosis. Symptoms include excessive urination, abdominal pain, bone and joint pain, tiring easily, weakness, forgetfulness, depression, kidney stones, easily fractured bones, and nausea/vomiting.
Screening For PHP
“Look for PHP before diagnosing FM” Dr. McCoy
The symptoms in the FM patients with PHP were similar but a bit different from those found in people with PHP and no FM. People with FM had more musculoskeletal symptoms (100% vs 54%), fatigue (96% vs 57%), cognitive decline/memory loss (62% vs 31%), and headache (19% vs 10%). Thirty-one percent were taking FM drugs, 35% were on narcotic pain relievers, and 28% were on antidepressants.
Screening for PHP involves obtaining an initial serum calcium level. If the level is high, the patient has further lab work, including serum calcium, parathyroid hormone, vitamin D, and possibly a 24-hour urine calcium level.
People at higher risk include women past the age of menopause and people who’ve had prolonged, severe reductions in vitamin D.
The Fix
The fix is an outpatient surgical procedure under local anesthetic which entails removing the glands that have become enlarged.
Results of the Study
“The key take-home message is that all patients who are potentially diagnosed with FM or carry that diagnosis, wherever they are in their course of treatment, should be screened for parathyroid disease. These patients are labeled as sick, and they may have something that we can fix. I think it’s really crucial to do a bigger study so we can get this out there.” Dr. McCoy
A followup questionnaire 14 months after the surgery found that about 90% of the parathyroid/FM patients reported improvement in at least one symptom, but that 25% reported improvement in cognitive functioning (80%), fatigue (71%), pain (55%), and mood (39%). Over 80% percent stopped taking at least one medication.
The medication most commonly dropped after the surgery were anti-inflammatories, followed by opioid pain drugs, anti-depressants, and FM-specific drugs.
That was pretty good, but the stunning statistic was that about 20% of the group were able to stop taking all their medications. These were the PHP patients misdiagnosed with FM. (Wouldn’t it be lovely to have your diagnosis switched from a chronic, difficult-to-treat illness to a treatable one?)
A Very Successful Surgical Procedure
If you simply associated success with a return to normal serum calcium levels, the surgery was stunningly successful with 97% of the patients’ calcium levels returning to normal. If you associate success with a dramatic reduction in prescription drug use then the surgery was a major success for about 20% of the FM patients. Most of the others had improvement in one or more symptoms and dropped one or more medications.
Anti-inflammatories were the most commonly dropped class of drugs, followed by narcotics, antidepressants, and FM-specific drugs.
These researchers may be coming to your clinic. Multi-center FM and PHP trials are planned.
Conclusion
A small but significant percentage of people with Fibromyalgia may also have a condition called hyperparathyroidism. This condition, which causes increased serum calcium levels, can produce symptoms similar to FM and is easily treated with outpatient surgery. This study found that 20% of FM patients with PHP were able to stop all their prescription drugs after surgery.
Thanks to Steve for the tip.







While hyperparathyroidism is indeed easy to diagnose, it does take a thorough diagnostician which I think is someone that is becoming more and more rare these days. I can’t tell you how many times my wife, self, mother, etc.,. have abnormal (often greatly so) blood values that are just ignored by doctors these days! My mother had a TSH of 11 (n=1-5.4) and that was “normal” even though she was sleeping all the time- off to the endocrinologist!
Also to call this a simple out patient surgery is erroneous, in the wrong hands you can have a disaster! Vocal cord paralysis etc.,. -please make sure you see someone really qualified for surgery!
Greg
I think you are confusing hyperthyroidism and hyperparathyroidism. TSH (Thyroid Stimulating Hormone) relates to hyperthyroidism (and hypothyroidism) as far as I know.
This is EXACTLY what I feel is wrong with me. Calcium numbers, etc. not to mention family history. Now on med. Can’t test pth numbers. Just had thyroid scanned, mentioned parathyroid to ultrasound tech. She checked them out. 8 days, tests are in but Dr. hasn’t read them yet. On thyroid med. Said I am normal now. No, sure don’t feel normal. Where does muscle vibrations and shaking figure into FM? That’s why I think it’s hyperparathyroidism.
Deanna, me too. I have recently developed a tremor and when I saw that could be caused by excess calcium in the brain I thought what are the odds this isn’t related. Wish we could talk and compare stories.
I have low calcium levels, something my gp didn’t think they needed to treat.
You can have hyoparathyroidism as well. 🙂
After having hight pth but low calcium levels an adena has now been found. So will have surgery to remove it. Goes to show one does not have to have a high serum calcium to have an adenoma on parathyroid gland.
I went to an endocrinologist 12 years ago looking for something else and my parathyroid level was high. I was losing too much calcium from my urine so he put me on a diuretic. ( don’t understand how that works.). Took it a few years and then stopped. Have had it checked a few times since, latest being 6 months ago, and it’s remained normal. Interesting it’s more common in those with FM.
It is amazing the number of abnormal results on “routine” blood tests that are never mentioned much less discussed with the patient. Makes one wonder if the doctor doing the tests really understands what these results mean. I am of the opinion that all FM patients should be screened by an Endocrinologist to begin with. But then, what do I know, I am only “the patient”.
I feel the same way
Drs don’t listen to patients
I have severe bone pain, extreme fatigue, my hands do not do what I want them to do I can barely walk … I’m 42
I have had 2 parathyroid tumors removed
I now have kidney stones, uncontrolled hbp, a high pth level but no tumor is seen
So they dismiss me
in it something is I will know, many thanks for the help in this question Orthomol B 17 vitamin
I would appreciate your correcting the places in your article where you called Hyperparathyroidism “parahyperthyroidism”….this caused me some confusion as I was reading your article….the correct acronym is HPP or HPT, NOT PHP…while I think your article makes some good points, I admit to being put off by your putting “(yawn)” at the end of certain sentences…what exactly did THAT mean? If you meant going off antiinflammatories, like NSAIDS is small potatoes, I most definitely would disagree…a significant number of people who take longterm NSAIDS will develop significant side effects…some which can be quite serious (heart, liver or kidney damage). I also think it may not be quite as easy for someone diagnosed with FM to have undiagnosed hyperparathyroidism…the reason is that hyperparathyroidism will typically cause increased serum calcium levels. Since people with FM usually see doctors regularly, they are likely to have health profile blood work done as part of the diagnostic process…I would doubt that many people are ever diagnosed with FM without having had a workup at some point which included a serum health profile, a cbc, and usually also thyroid testing. If calcium comes back elevated in a blood profile, doctors know to repeat the result for accuracy and then to look further into possible causes if the calcium really is elevated. That said, from what you are saying, there is some small percentage of people who might have hyperparathyroidism which is getting missed. For that reason I am glad you brought this up, but I think the details I am stating are important so people don’t jump to the conclusion that they must have this. I also agree with the person who commented suggesting you should be careful about saying how correcting hyperparathyoidism is just an outpatient procedure…It never was outpt until managed care came on the scene, and yes,there is a possibility of significant complications from this surgery. Overall, thanks for this information but I would appreciate it if you would work on your accuracy and details, and would prefer you leave out what appears to be sarcasm (or something)–I mean that (yawn) thing.
Lorrie
Retired RN
Amherst, VA
To answer some of your concerns
The outpatient procedure information I got from the Mayo Clinic website – It says this “Surgery may be done as an outpatient procedure, allowing you to go home the same day. In such cases, the surgery is done through very small incisions in the neck, and you receive only local anesthetics.
Complications from surgery aren’t common. Risks include:
Damage to nerves controlling the vocal cords
Long-term low calcium levels requiring the use of calcium and vitamin D supplements”
Now that I know better I would not have described the operation as simple in the email for the blog.
The PHP reference was taken directly from a quote from a doctor. It refers to primary hyperparathyroidism – http://endocrinediseases.org/parathyroid/parathyroid_php.shtml
Your comment regarding the blood tests makes sense and I wondered about that as well. The authors of the study, however, and some doctors in the Medscape article do believe that a significant number of FM patients who have hyperparathyroidism have not been diagnosed with it. They’re apparently confident enough about this to plan a multicenter trial focusing on FM clinics to ferret out more FM patients with hyperparathyroidism or PHP.
While I agree that getting NSAIDS is a good thing, NSAIDS are quite far down the list of effective drugs in FM, probably because a different kind of inflammation is present.. Because of that my guess is that the symptom reduction associated with getting off of them is probably not that significant. I was looking at it from that end, but I didn’t think about the harmful effects of staying on NSAIDS. I thought that was a good point.
Spine-health reports that “Unfortunately, despite their widespread use, NSAID’s have not been shown to be very effective in relieving the painful symptoms of fibromyalgia. There is no documented evidence of inflammatory changes associated with this syndrome.
In a study of 46 fibromyalgia patients that compared Ibuprofen to placebo, both groups reported interval improvement in fatigue, pain, tender points, and subjective swelling and there was no significant difference between the two groups 44.”
I count about nine hyperparathyroidism’s in the blog and one mistake – sorry that confused you. I have corrected that mistake
While I am in agreement about a number of RN’s comments–certainly the (yawns), I do however take great exception to:
[…doctors know to repeat the result for accuracy and then to look further into possible causes if the calcium really is elevated], if only from the standpoint the large majority really have no idea whatsoever that a calcium level of even the low 10’s can make one quite symptomatic & is most likely owing to PHPT (Primary Hyperparathyroidism). Yes, a battery of tests may be run over the years, even to the point of suspecting Sarcoidosis, RA, MS, CFS & Fibro; again highly unlikely. A plethora of patients are subjected to years of testing, all the while the even slightly elevated calcium levels coast right under the radar & patients are prescribed a host of medications which simply do not address the underlying illness, PHPT.
There is a very large percentage of people “being missed” and not being properly biochemically tested for PHPT. If there should happen to be any doubt of this, performing a Google / Chrome search for Parathyroid Support and Awareness Groups is confirmatory this particular patient population, sadly, continues to grow by leaps and bounds.
As mentioned, in the hands of a highly experienced parathyroid surgeon such as Dr. Milas & others whose background & contact info can be found on the AAES’s (American Association of Endocrine Surgeons) web site–or in some instances to a lesser degree, a well-trained General Surgeon or ENT–it “can be” a relatively straightforward operation. Even in instances with a minimally invasive (smaller incision) bi-lateral exploration. In experienced hands, great care is taken to identify all four parathyroid glands & to preserve the RLN. And while many centers have abandoned use of the “website touted radioguided probe”, thankfully the experienced surgeon utilizes ioPTH monitoring/testing to help determine biochemical confirmation of a successful procedure, or, whether or not further exploration may be needed (i.e. ectopic adenomas / more than 4 PT glands).
Do I think it should be an overnight stay? Yes, I do.
Do I think the surgeons should offer better follow-up on days 3 to 5 where one is most likely to go in to tetany, if at all? Yes, I do.
Do I think physicians everywhere need to be retrained in how to accurately interpret calcium levels on a BMP, and know when to order both total and ionized calcium & intact PTH all at the same time? Yes…
Do I think all physicians need to also familiarize themselves with the entity of Normocalcemic PHPT? Yes…
Is it our PCP’s and Endos who, unfortunately, are miserably failing their patients in not understanding that all symptomatic patients, with biochemically documented labs for PHPT should undergo surgery as a choice that is theirs to make–most certainly according to the workshop-established guidelines.
You bet it’s lovely “to have your illness switched to one that’s treatable” with surgery…
Thanks for all the info Angelia. I think I’m going to take the ‘yawn’ out. 🙂
I have had the FMS diagnosis since 1986 at age 26 and after all this time a new rheumy decided to do a PTH parathyroid hormone test and it is abnormally high. No doctor including other endocrinologists thought to check it? The sure way to get inadequate health treatment is to tell a doctor you have been diagnosed with FMS. Immediate dismissal is what you’ll get. Your mental health is questionable and you’re drug seeking. I have had 36 years of this.
Actually he’s correct that most doctors do not report to their patients that have high calcium results. Not just a few but a lot !! I’m in a group that is nothing but hyperparathyroidism patients. I would say 99% of us weren’t told of our high calcium results . Doctors aren’t educated about this.
Great article. Diagnosed with fibromyalgia by 11 pt touch only in 2007. Diagnosed with primary hyperparathyroidism last month. I self diagnosed and self referred to endocrinologist after reading Dr Jim Normans site. The problem is the labs, my lab says normal calcium is 8.8 to 10.7. Dr. Norman says if over age 40, should be under 10.0. Mine is 10.5. Has been over 10 for about 15 years. My age is 70.
I stand corrected in having thought that hyperparathyroidism ought to be fairly easily id’d in a population of patients who have reason to see doctors regularly and also to have blood health profiles drawn for diagnostic purposes. I would have thought just about any doctor would pay attention to an elevated calcium level, but apparently this just isn’t so…here is a link to a 2011 article I found where the number of missed cases was actually studied:
http://pubmedcentralcanada.ca/pmcc/articles/PMC3363079/
this study (done in England) reported that 62% of the cases id’d were NOT treated, nor were the patients referred to a specialist…
I found another article which would likely interest you, Cort, since it very much reaches the same conclusions you have reached re: the fact that hyperparathyroidism may be an unrecognized underlying condition in some pts diagnosed with FM and CFS–this was an article written about a yr ago by someone with whom I am not familiar who calls himself the fibro doctor:
http://thefibrodoctor.com/what-is-hyperparathyroidism/
the many potential dangers of untreated hyperparathyroidism are spelled out, including heart and kidney disease and osteoporosis, which can become quite severe. this doctor also agrees that many doctors routinely ignore elevated calcium levels, which is very disturbing.
Lorriel
Amherst, VA
Thanks Lorriel I appreciate it. Didn’t know Dr. Murphee was up on this as well. Hopefully that multi-center study will go through as planned and we’ll have some hard data in a couple of years.
Hi.. Please help me to understand blood results.I have been researching Hyperparathyroidism since seeing a link between it and fibromyalgia a couple of weeks ago. I went to the Gp ( I’m in the UK) just had my blood results back. I will be seeing him on Monday ( 2nd June) and I want to be armed with information! Are the blood measurements different in US than the UK?? My results show PTH 2.32 SERUM…CALCIUM 2.37…THE LEVEL 1.53…T4 13.. Apparently all within ‘normal’ range…I’m so confused…which doesn’t take much with having brain fog!! All the other sites i have been on say that ‘normal’ for my age of 46 should be in the 9’s!! I’m praying that I have a rogue parathyroid gland so I can have it whipped out & cure me from 25 years of he’ll…Thanks in advance
Amended.. THE LEVEL 1.53 Thanks
I have FM & hypothyroidism (had to fight to get those diagnoses). I’ve worked in residential medical schools for MD’s straight out of medical school and drs are not “trained” to look into each patient’s symptoms like you would think they should be. Because I’m not one of those patients who take on every symptom or illness that I read about, my dr will look at any type of lab test or xray seriously that I suggest & this is how I get diagnosed. HE doesn’t have time to look into my case in detail like I do, unfortunately, so this has worked very well for me (of course, everything has been confirmed). I wish EVERYONE had access & understanding of medical science this way!
First of all, you are confusing Hyperparathyroidism & hypothyroidism. There is a HUGE difference. If your doctor doesn’t have time to look into & evaluate your health issues it is time for you to start researching new doctors that will take the time. In the meantime I would read read & read some more about how Fibromyalgia & Hyperparathyroidism overlap in their symptoms. You may very well have been misdiagnosed with Fibromyalgia when in fact you could have a VERY treatable condition (Hyperparathyroidism). It is an outpatient surgery that takes approximately 20 minutes under a local. Do the research & help yourself!! I have a wonderful doctor that has taken the time to put two & two together. Good luck to you!
Would you mind telling me who your doctor is, I am having surgery at the Norman parathyroid clinic in Tampa Florida.
I feel like as soon as I tell a new doctor that I have FM they stop listening. They said to me you do have a appointment with your psychiatrist soon right???
I’ve recently been diagnosed with pHPT & require multiple joint replacements as a result of delayed diagnosis. I’ve suffered years of gaslighting around co-morbid Endometriosis CUTI’s/I/C, sleep issues etc I now learn that orthopedic, MH, sleep & bladder issues are all symptoms associated with pHPT & I had many of the symptoms since age 11 when I first developed issues following a Bornholms like virus followed by Endometriosis later that year.
I was diagnosed with hyperparathyroidism last year after having kidney stones for the hundredth time. My urologist decided to do further testing a found my PHP levels were too high. He sent me to a specialist who then confirmed his diagnosis. I’m have one or more of my parathyroids removed next week. My surgeon has told that several of my FM symptoms should go away after surgery. I was diagnosed with FM over 20 years ago