
Your book “Reviving the Broken Marionette: Treatments for CFS/ME and Fibromyalgia” provided an overview of over 250 ME/CFS and FM treatments six years ago. How have your views of ME/CFS and FM treatments changed in the past six years?
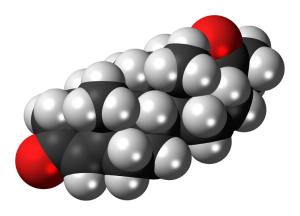
I am even more convinced now that low dose naltrexone (LDN) is “the” CFS/ME drug. Hundreds of Finns have now been using it and 2/3 have a positive experience. Some get minor benefit, others have life-changing experiences. I’m a bit less impressed by antivirals now, but more enthusiastic about beta blockers.
- Check out Health Rising’s Low Dose Naltrexone Fibromyalgia and Chronic Fatigue Syndrome Resource Center

Maija pegged ‘missed diagnoses’ such as Sjogren’s Syndrome, lupus, B-12 deficiency and mold as a major problem
Besides rituximab and GC-maf I don’t think there have been any major new treatments. Had Ampligen been approved the landscape might be very different now. My doctor in Finland is trialing some interesting new treatments that regulate the sympathetic nervous system.
I would say the biggest change in treatment is personalized medicine, like 23andMe, which has increased the importance of non-pharmaceutical treatments, like the various methylation protocol.
I’ve been hoping to update the book, but sadly it hasn’t fit my schedule and finances – I can only afford to write in Finnish now.
But should I update it, I will include a new chapter about verifying your diagnosis is correct. It is so common for people to get a CFS/ME diagnosis when they really have something else – sometimes several illnesses at once. Whether it’s Sjögren’s, Lyme, B12 deficiency, mold illness, adrenal insufficiency or something rarer.
Rituximab wasn’t even a blip on the screen six years ago when you published your book. Now it’s a major interest. What do you think about rituximab?
I included rituximab in the Finnish version of the book which came out in 2010, soon after the first Norwegian study, but I’m not enthusiastic about it, to put it mildly. I think CFS/ME should always be treated with immunostimulants – as pretty much all of the other major CFS/ME treatments are – never immunosuppressants.
The same goes for autoimmune diseases, as well. It goes against the dogma , but then again, first there was a dogma that autoimmune diseases could not even exist (horror autotoxicus) and for a long time the dogma was that they were extremely rare. My most recent medical book (published in Finnish last year) was about the treatment of autoimmune diseases and it presents a lot of evidence to support this idea.

Maija, who wrote a book on autoimmune disorders, believes ME/CFS is generally better treated with immunostimulants than immunosuppressants
I’m often asked whether I think CFS/ME is an autoimmune disease. Perhaps surprisingly, I don’t have a clear answer for this, but I usually say that treatment-wise, it doesn’t matter. Both are diseases of low immune function, which may in some ways manifest as “overactive immune system”, but it’s really just immune system that doesn’t work right.
Politically, having conclusive proof of autoimmune origin would be helpful, but contrary to what some think, rituximab “working” doesn’t prove CFS/ME is a physical illness – obviously we already have proof of that. Biological immunosuppressants are also being studied in psychiatric illnesses.
What do you think about microglial inhibitors?
It’s a highly promising area, but needs more research to ascertain how promising. Naltrexone is a microglial inhibitor among its other modes of action. There is constant disagreement whether large or small LDN doses are more effective and some have suggested only using the enantiomer D-naltrexone (which is a microglial inhibitor with no opioid blocking effects) or using a heterochiral mixture (more D-naltrexone than L-naltrexone). Then people could take large amounts of the microglial inhibiting isomer and smaller amounts (or none) of the opioid blocker. But this is something the pharmaceutical industry must do, you can’t have your pharmacy compound it.
Most drugs and supplements that inhibit microglial activation also have other potentially useful modes of action.
Your knowledge of pharmaceutical drugs in ME/CFS is incredible. Tell me one drug that you suspect is underused in ME/CFS and FM.
LDN is still underused, but at least now most people have heard about it.

She believes that nootropics such as Nimodipine and Piracetum are among the most underutilized drugs in the ME/CFS and FM communities
I’d say nootropics (cognition enhancing drugs) are very underused. Most people, including many doctors, haven’t even heard of them! Piracetam is very well-tolerated and even OTC in some countries.
- Better Thinking for Chronic Fatigue Syndrome and Fibromyalgia: the Nootropics
- Piractem For Chronic Fatigue Syndrome and Fibromyalgia
Another class is NMDA antagonists. I hope to see proper studies on this front soon.
Medical marijuana is probably very underused, sadly we all know why.
I believe we probably have many great underused drugs, but even I don’t know they’re underused! There are several medications in my book that I believe would work well, but the data is still missing.
We hardly ever hear about nimodopine but it plays a key role in a Dr. Downing-Orr’s book and treatment protocol. How helpful was nimodopine for you?
It was very helpful from the first dose. It wiped off that “foggy” feeling and it helped with language problems in particular, but in a different way from piracetam, which also helped on that front. It didn’t help my fatigue or any other symptom except for orthostatic hypotension, which was always mild for me. The best part was that after half a year of taking it at half a tablet a day I was able to retain all the cognitive benefits even though I stopped taking it.
Several people on my forum have had the same experience of lasting benefits. One person found nimodipine very helpful for fatigue and blurry vision. Another woman found it made it easier for her to walk.
- Learn more about Nimodine – Nimodipine for Chronic Fatigue Syndrome and Fibromyalgia
What’s going on with your health? You benefited greatly from low dose naltrexone (LDN). Are you still using LDN? Has anything else significantly helped?
I’ve been using LDN for over seven years now. It was almost like a miracle, stopping my rapid disease progression, pretty much completely eliminating PEM (!) and increasing my ability to walk from some 50 meters to 5 km or more. I wasn’t cured but I’d sometimes work 15-hour days writing my medical books. I’ve also benefited significantly from nootropics. After starting nimodipine and piracetam I’ve written six novels, four non-fiction books, three plays and a screenplay.
Unfortunately in November 2011 acute stress destroyed most of my pituitary. The result was a nearly narcolepsy-like condition, apparently from growth hormone deficiency. Some people interpreted this to mean that LDN no longer works for me. I could still walk a lot, no PEM, but my ability to work was reduced to 0.5-1 hours on most days, often zero.
Now I’m finally getting treatment for the GH deficiency. On my own expense – not cheap, by the way. It’s too early to say whether it will fix the problem. I’m also taking most other pituitary and related hormones except for testosterone – glucocorticoids, mineralocorticoids, estrogen, progesterone, DHEA, desmopressin, T3 and T4. I might start oxytocin, too.
It has turned out that I’m helped a lot by progesterone. It’s quite a surprise, as I was hoping to
improve on estrogen, but didn’t really expect anything fromprogesterone – it’s just “something that has to be taken if you take estrogen” (which doesn’t seem to do anything). But progesterone helps my hypoglycemia and makes my breathing easier and physical stamina better. Sadly, it’s supposed to be taken cyclically. I’m on a break after 11 days and my blood sugar just won’t stay up at all.
Dozens of supplements have helped me over the years, but those that help my fatigue/functionality always stop working, I don’t know why. I’m still experimenting with new supplements despite having tried over 100 already. I just don’t expect them to help more than a month.
For sleep I use a combination of melatonin, baclofen and Sophora flavescens. B12 and methylfolate help that too. But the most important thing for my sleep is adequate hormones. For example, low cortisol used to mean not sleeping more than one hour a night.
I know of another person with ME/CFS who did very well on progesterone (but not on estrogen). She found out about progesterone by visiting forums for another disease group. How did you find out about progesterone?
I went to a Belgian clinic after I asked my Dutch CFS/ME doctor if he could prescribe me growth hormone and he said he wouldn’t, but the clinic probably would. Which they did – they use it quite often. I was already taking various hormones, but based on my symptoms, lab tests and a physical exam they added estrogen, progesterone, the GH (and changed some of my existing hormone prescriptions).
They said estrogen deficiency is one of my main problems and behind my severe hair loss (I had figured out I was deficient in estrogen, but didn’t connect it to the hair loss – time will tell whether they’re right), but they didn’t really mention anything about progesterone.
I don’t really view myself as taking it for CFS/ME (but progesterone deficiency from hypopituitarism), but of course it’s hard to say for sure which symptom comes from which problem. But I doubt I’d have never specifically asked for progesterone.
I’ll have to ask if there’s any chance I could take progesterone all the time. After all with the mini pill women are taking only (synthetic) progestagens without any breaks.
After you discovered LDN and nootropics such as nimodopine and piracetam your productivity increased greatly. You were able to put in 15 hour days but then you experienced a sudden acute stress that wiped your pituitary out and your ability to work – not to exercise – but to do the kind of mental work you were so good at before plummeted. Did you have any indication prior to that that your system was weakening or was your collapse an out-of-the blue type thing?
No, I was doing just fine. Though I’ve had minor instances of worsening hypopit, e.g. in March 2009 (I’ve been dependent on corticosteroids since), June 2012 and August 2012, where I’ve had some preliminary symptoms. For the first two there was no obvious serious stressor, the last one followed a trip to Berlin with temperatures reaching 37C.
In the first and last instance I had a sudden sensation of feeling inexplicably good for a few hours the day before the problem got worse. In the second instance I suddenly started feeling extremely thirsty, like I could drink an ocean. I wasn’t very surprised when my diabetes insipidus got permanently worse after that. (Normally diabetes insipidus does not make me thirsty.)
Do you know what happened to your pituitary? Was it your immune system? I know that car accidents can shear off the pituitary…
I have no idea. Some people have suggested it might be autoimmunity, but I’m not convinced. I’m on LDN after all, I have no evidence of any autoimmunity (which of course doesn’t exclude it; I haven’t had pituitary autoantibodies tested) and it seems strange to me that autoimmunity could destroy something so quickly, just hours from the acute stressor. I’ve only had a pituitary MRI in late 2010, before the worst problems started, which showed nothing unusual.
You wrote ‘Don’t go chasing expensive fad treatments”. Is there anything in particular you want to put in that category?
I feel that applies for most areas of medicine. Not just CFS/ME but e.g. autoimmune diseases. People think that if a new super expensive biological drug is approved, it must be the best treatment. Some new biologics do work well, others don’t. Just because something is a biologic doesn’t mean it works better than a pill. Targeted drugs aren’t automatically more effective (or safer) than non-targeted ones and new meds don’t always beat the old.

The large and varied range of treatments that dramatically help some people with ME/CFS speaks to how heterogeneous this disorder is.
Things that have had dramatic beneficial effects on at least one person on my forum, besides the LDN, include e.g. L-carnitine, D-ribose, methylfolate, wild vegetables, gluten-free diet, ozone therapy, oral saline, beta blockers, sumatriptan (for all symptoms), tramadol (similarly), modafinil, hydrocortisone, amitriptyline, fluoxetine, clonazepam, prednisone, testosterone, IVIG, nimodipine, antibiotics. Some of these are common CFS/ME treatments, some are not.
My Finnish doctor has started treating people with saline solution (normal salt + water), usually just orally, and a few people have benefited a lot. It shows that even though this is avery serious illness, sometimes simple things can help a lot.
Many people don’t even want to try any treatments because they are just waiting for Ampligen and rituximab.
It’s not so much which is the best treatment but what is the right fit for you.
What role do you think supplements and non-pharmaceutical treatments play in ME/CFS and FM treatment?
I think for most of us medications are going to be the most helpful form of treatment (aside from rest/pacing), but that doesn’t mean other treatments are useless. Some people benefit massively from diet changes, others not at all. Mitochondrial nutrients like carnitine, D-ribose, lipoic acid, NADH and PQQ help many of us, and if mitochondrial issues are your main problem, they may help more than anything else.
Less popular supplements that can be helpful include e.g. Epicor, benfotiamine, astragalus, berberine, cat’s claw and inosine. Bromelain is great for post-exertional muscle soreness. As with meds, there are supplements that may carry a lot of promise, but hardly anyone uses them.
My Finnish doctor uses supplemental oxygen, which several of my friends have tried and feel it is very helpful. Ozone therapy may have use in some cases. A friend benefited a lot from neurofeedback. Acupuncture may help some. My Dutch doctor uses intermittent hypoxia.
You lost most of your youth to ME/CFS but you’re not bitter about it. In fact, you say that you’ve probably learned things about yourself and may even be happier than if you’d never gotten sick. What has having ME/CFS had you learn and how might you be happier than if you hadn’t to confront this disorder?
I don’t buy the common inspirational ideas that “illness is a gift” and such. It hasn’t been a path to “spiritual awakening” for me, even though post-LDN I’m grateful of such things as being able to walk. But it got me into medicine, made me realize I didn’t want to live in Finland (and move to the Netherlands) and it has made me appreciate time. I would never waste time.
You also talk about ‘accepting’ ME/CFS and FM and still fighting to get better. Many people think of acceptance as a kind of passive stance that doesn’t include taking action. Can you talk about what you mean by ‘acceptance’ and how that doesn’t mean for you caving in to this illness?

Is ME/CFS/FM treatable? Maija believes yes – many people can improve – if they have the resources and keep looking
A Finnish friend (who used to have severe CFS/ME but is now much better) put it well. To get better you need a positive attitude. The attitude itself isn’t helpful – you just need it to pursue treatment. Of course for many people getting treatment is difficult or impossible, because of finances or lack of local doctors, but others just give up, thinking that CFS/ME isn’t really treatable, or that their own case is too difficult. They already tried several meds. Well, there are 250 meds in my book.
What’s the situation in Finland like for people with ME/CFS?
Bad but slowly improving. When I started CFS/ME advocacy in 2006 there was absolutely nothing. Doctors had never heard of it. One university site and one infectious disease textbook was it.
I was hopeful, but for like five years it seemed like nothing was happening. Then we started getting some magazine and newspaper articles (before that it was less than one article a year) and one important milestone was when me, my doctor and another CFS/ME patient appeared on a well-respected TV talk show.
Now in May we got an article about CFS/ME in the biggest Finnish newspaper, mentioning LDN, hypermobility (which he is researching actively) and other good things. Puzzlingly, the next day they published another article – touting CBT and GET. I guess the insurance doctors weren’t happy. I sent them a letter, not sure yet whether they’ll publish it.
The situation has been very limited in focus. I’m the only visible activist – even though I haven’t even lived there after 2010 – and my doctor is the only visible expert. As a result we’re both overwhelmed. He works from morning late into the night, I get tons of email.
Still, officially this illness does not exist. Recently some lucky people have managed to obtain disability benefits from the public insurance provider, but it’s rare. We are still waiting for the first Finnish medical paper (that isn’t a completely incoherent “review article” written by an insurance doctor). I’m aware of several Finnish celebs with CFS/ME, but no one is willing to speak out.
You’ve been an active advocate and you’re an independent and original thinker so I’m going to ask you a big question- what is missing in advocacy movements the providing of which would make them a lot more effective?
I’m not sure what’s “missing” as much as people are focusing their energy on things that I feel would be better focused on other things. It’s hard to answer in a way which doesn’t feel like I’m blaming someone. As we all know, there is all kinds of division (is CFS the same as ME etc). It seems like people are often reinventing the wheel, setting up new charities and organizations which feel duplicate. There have been at least five international CFS/ME documentaries made or in the making in the past few years.

Majia proposes advocates focus on ROI – what specific returns the investment of their time and energy will bring for ME/CFS
Another thing that feels to me like waste of resources is things like people getting Niagara falls and various towers lit with colored lighting for CFS/ME awareness. Endless retweeting on Twitter doesn’t generate awareness if all your followers are fellow patients. Here is a good recent blog post about the problems with “awareness”.
I think people should focus more old marketing concept of ROI, return of investment. There is one thing the CFS/ME advocacy scene has even less of that money and that’s human resources.
Everyone should ponder whether their activism efforts actually result in something. In the age of social media I still feel like things like paper brochures are often more useful than tweets and videos. Sure, a viral video could really help our cause, but how many have there been?
________________________________________
Maija Haavisto is the author of “Reviving the Broken Marionette: Treatments for CFS/ME and Fibromyalgia” and numerous other books and plays. Check out her website here.








Thanks for the post;I will look for her book but if polypharmacy applies to supplement use, she does it! Perhaps she has kept detailed records of her self trials but many of those substances mentioned are chemicals with, IMO, minimal research base and probably zero research on potential interactions or synergy. I’m not surprised to hear she had a pituitary system collapse. These are same the desperate searches that many intelligent people who have chronic debilitating illness do;I used to try and translate foreign medical journals for arcane and esoteric meds for my son’s Crohn’s. In the end it was Big Pharma that came up with something. I’m sure Maija is quite knowledgeable about these supplments but, personally, I get nervous about ingesting too many fringe chemicals that have no randomized/blinded studies to support them.
unfortunately Big Pharma thinks we’re Big Whinoes and won’t come up with/approve something and we have no other choice than to randomly and blindly test things on ourselves, often 🙁
btw the book-links lead to an empty page
Fixed!
Pretty much everything I take is backed by tons of studies, even if those studies are not for CFS/ME.
What makes you think you have CFS/ME? How do you know it is not Ehlers Dankos Syndrome with possible ‘crossover’ types multiple ones? Anyone I know who is on Naltrexone say it does not do anything for them & are not helped by taking this at all & even say they see no changes with or without its so-called benefits
I agree, Steve. I, also, am “nervous about ingesting too many chemicals that have no randomized/blinded studies to support them”. I ordered Maija’s book a few years ago with hopes it would provide an answer for me. But, I quickly realized the “treatments” described on the book cover were almost all pharmaceuticals. As an extremely chemically-sensitive individual, I was disappointed with my purchase.
During my early years living with ME/FM/MCS, I tried many pharmaceuticals. A few provided increased energy, but only for a few days. The increased activity that resulted from my feeling less ill invariably precipitated a “crash”. I likened my experience to whipping a racehorse. By doing so, you can make the horse run faster, but only for a short period of time. Unless you overcome the horse’s genuine physical limitations, this “treatment” is destined to fail over the long term.
I am sorry my book was disappointing for you! My book covers entirely pharmaceuticals and the descriptions online should make it very clear. It’s NOT that I discount supplements, but I originally wrote a book about meds so that people could take it to their doctors in hopes of getting a prescription. With supplements you could just take what you wanted and there is info about those online. Had I added supplements too, the book would have grown massively.
I was originally supposed to write a second book focusing on non-drug treatments alone. Unfortunately it turned out not to be financially viable.
My experience is the exact opposite of yours: dozens of supplements have helped me for a while but then stopped working, while meds have kept working for me (with the exception of isoprinosine).
Regarding LDN, which is Naltrexone in low dose, what is low dose these days…1 to 3 MG’s?
Naltrexone is available at All Day Chemists on line from India, without a prescription and must be diluted with water to achieve “low dose”. LDN has been tested at Penn State but I don’t believe for CFS. What else is new? RP
Rich,
Earlier this month, I attended an International Awareness Day educational event. Jarred Younger, Assistant Professor of Pain Management at the Stanford School of Medicine was one of the speakers (via web connection). He is an expert on Fibromyalgia.
In his presentation, Dr. Younger divided FM treatments into three categories: green (FDA-approved, but generally not that effective), yellow (medications that may receive FDA approval within the next few years), and red (medications that may be approved in the distant future). The bulk of Dr. Younger’s presentation focussed on “yellow” medications; actually, one medication in particular — LDN.
With an initial disclaimer that he can’t recommend any treatment, and that physicians prescribing medications that are not FDA-approved are taking a risk, Dr. Younger discussed LDN in great detail — in particular, its’ long history, good safety record, and efficacy. In studies with FM patients, 75 percent improved, with 50 percent claiming “much” or “very much” improvement over a 12 – 16 week period. The drug is easily tolerated (as tolerable as placebo), with virtually no side-effects, except more vivid dreams.
The drug used in the study was 4.5 mg of Naltrexone Hydrochloride, custom compounded. Dr. Younger is not in favor of dilution, because it is difficult to obtain a consistent dose. LDN is slow to show results — typically two months.
Dr. Younger mentioned that if 4.5 mg isn’t effective, doses up to 9 mg have been safely used (by a Rheumatologist, David McLean, according to my notes).
Dr. Younger is only authorized to study LDN for FM under his current research grant. He intends to test the drug for CFS patients in the future. Apparently, there is a huge push in Britain to get LDN approved for these conditions.
(My apologies to Dr. Younger, if my notes have caused me to misrepresent him.)
Very helpful info, Karen. As noted, I’m going to try Niagen,( NAD+), soon but LDN is on my next to try list, possibly after a better COQ10 as suggested by Chris.
Pretty soon I’ll be like Maija, but I hope some of the chems I try have been studied a bit more.
LDN caused me to have severe depression and that was on a very low dose. It for sure helped pain and sleep, but the undesirable side effect was not worth it.
Issie
I like this interesting post very much, Cort! Thank you for dedicating yourself to making so many sources of information available to us patients. Though having a limited medical knowledge, I still have enough to know that in time effective treatment and indeed a cure will be accomplished. (I haven’t lost hopes for Ampligen, even if it means going to So America) For me, I suddenly got hit with ME/CFS in 1992 at 39 yrs old starting with Mononucleosis. I was LUCKY to become a patient of a well-known ME/CFS specialist in Utah. However, about 5 years ago a fellow patient I respected very much said, “It won’t be soon enough for me, though”. Being 56 yrs then I guess bought into this idea instead of aggressively pursuing my Dr’s very limited time. I now see that I’ve been stagnant- relying on the medications & supplements that I’ve taken for years without much success. After reading this post and others on your site I realize that I need to start fighting for myself again to gain some ground & improvement.
By the way, Cort: Did this interview effect you personally? What specific things?
The interview opened up some options that I hadn’t thought of in particular the Nootropics. I really like what Nimodipine does and the fact the fact that Dr. Downing-Orr uses it as the basis for her treatments. She uses it at most for 4-5 months..I plan to cover her book in detail.
I was also impressed with the list of supplements Maija pointed. I am one of those who gave up searching really. The interview reminded me of how many options are out there.
I have a friend that had extreme autonomic problems that was cured with the TVAM/CCSVI procedure, and she knows of several others who have benefited from the procedure as well.
How come we never hear about this procedure used for ME/CFS?
Dave
oh, what is this prcedure?
Because people probably dont study it or want to take the chance on the surgery. There have been at least one death from it. My doc feels that CCSVI is very likely a big contribution to POTS. However, he feels we can unblock our veins and arteries with diet and treatment to breakdown biofilm that houses virus, bacteria and protozoa and adheres to the walls and causes the clogging in the first place. He thinks if we can get this under control, maybe we wont need the surgery. Some that he has known to under go the surgery was clogged up again in about 18 months. It requires a lifestyle change.
Issie
Issie,
What kind of treatment does your Doctor recommend? TY
Breaking down biofilm (with enzymes) which protects and houses virus, protozoa and bacteria. Attacking it with low dose antibiotics and antimalarial herbs. Later taking a good probiotic. Also of more importance a whole food, low fat, vegan diet. Eliminating foods known to cause immune system dysfunction (dairy, gluten). Limiting sugar and trying to be as organic and whole foods and unrefined as possible.
Issie.
I don’t recommend this surgery
It is possible to buy LDN from Israel Pharmacy in Tel Aviv. I did, shipping is very expensive though.
Started 3 weeks ago with 1,5 mg which made me feel verrrryy bad ( stomach and head), cut the pill in half, so that was 0,75 mg. Somehow this medicine is not good for my head, increases the brain fog, maybe I’d have to take an even smaller dose to start with.?
For medicine sensitive people: go easy on this drug.
Hi Ria, If you contact the LDN Research Trust they can put you in touch with a doctor who will prescribe it in Israel as well as the compounding pharmacy, (I say this in figuring Israel is part of the 154 member countries who have LDN available). http://www.ldnresearchtrust.org
Or just ask your doctor – mine gave me a script for 4.5 but I ended up getting it from Rivers pharmacy in Canada because I wanted to dilute and play with the dose. Interesting what Dr. Younger said about dispersion problems doing it this way. I wondered about that but had been told it would disperse evenly.
Betsy,
I don’t recall Dr. Younger mentioning “dispersion problems” as the reason he did not recommend patients diluting the drug to achieve a customized dose. I suspect it is more likely his realization that calculation errors, or inaccurate measurement, may result in some patients taking more, or less, of the drug than intended.
For me, this concern would be justified, considering the way my ME brain sometimes scrambles instructions in cooking recipes!
I misunderstood, thanks for clearing that up Karen.
Dilute a 50mg tablet in 50ml of water. One ml of water bears one mg of medicine! That’s it!
Hi,
I am not sure if this has been posted yet, but there are video on how to take Naltrexone and make it Low Dose. It comes in 50mg tablets which you put in 50 ml of water. Shake and REFRIGERATE. Shake before each dose. Start with .5 or 1ml and work your way up slowly
Here is a place to order
http://www.unitedpharmacies.com/search.html?search_text=naltrexone&searchbutton=Go
You don’t need a prescription when you order in Israel 🙂
What a fantastic and informative interview! As always Cort, great work!
Thanks. I really want to thank Maija for being such a rich source of information 🙂
I agree with the observation that this is an immune deficiency. That’s why I always feel strangely well just before I get a bug – because my system’s defenses are stimulated at that point. I like Pender’s theory that people who get CFS lack the immunity conferred by early exposure to EBV. The fact that killing the B cells with rituximab temporarily helps could indicate that the virus is in those cells, but since the killer T cells are insufficient the virus bounces back.
In any case I want to try the LDN, so I’m looking into getting a prescription. If that works then maybe I could try the nootropics.
LDN looked potentially very promising a few years ago, but seems to have dropped down the radar since then. Trials that were being proposed, if completed / advanced, don’t appear to have produced news-worthy results.
Advocates continue to be positive in their claims, but experience shows that we need to be seeing a range of views and patient reports to venture any sort of useful evaluation on trialling it ourselves, never mind proposing it to others.
Previously, in the UK (& US west coast), there appeared to be a consensus that it was only reliably effective when taken in a prepared solution(?).
Its use in CF has been considered with a view to further differentiation (>CFS > ME?), but the main thrust in relation to roughly similar presentations has appeared to be FM.
Do we have any clear indication where to find the least subjective current information on LDN?
We have previously tended to see roughly as much or more reaction blocking or limiting continued positive effects from types of treatment targetting immunology, virology, etc, so we appear to need to map specifics in individual patients as they progress through such treatments, and see where that leads us(?).
Actually LDN’s track record in Fibromyalgia has been good. You can find some links to some hopefully pretty objective blogs on it here 🙂
I think it’s the exact opposite. A few years ago LDN was mostly unknown. Now it’s the first line CFS/ME treatment in many countries and gaining ground as a treatment for e.g. autoimmune diseases and cancer. FYI my doctor in Finland has prescribed LDN for hundreds of CFS/ME patients and none of them have taken it as a solution.
In MS the LDN studies seemed to dry out a few years ago. Not sure why, as the preliminary results were good.
I also maintain a page about LDN for all kinds of indications. It’s not 100 % up to date (updated in January, I hope to update it in June), but here you can see pretty much all the research for all conditions. http://www.fiikus.net/?ldnrefs
I tried LDN a few years back, but it disturbed my sleep and I already have terrible insomnia. I stuck with it a couple months…never got past 3mg. I also tried Piracetam for a month with no effect. Not to mention the methylation protocol and a gazillion other things over the last 20 years. I have given up hope 🙁
IMO piracetam should be taken for longer than a month. There are two types of effects, one that appear almost immediately (but not everyone gets them) and those that take months to appear. When I first started piracetam I was slightly disappointed in its efficacy (even though it clearly worked), but three months later things were quite different.
Thank you Cort for publishing Majia’s very fine work. Her mention of ROI with advocacy was perceptive. I plan to try some of her suggestions very soon, especially Nimodipine and LDN.
Good luck, Carol
I saw Maija on Finnish TV (being a Finnish expat myself) so pricked my ears – I am quite impressed by this interview. I don’t suffer from ME but rather FM/CFS, yet hope that good ideas will come my way. She has a lot of typical Finnish common sense. I also read the comments here with interest and agree that polypharmaka and the use of so many supplements can cause severe issues too. I have recently become sensitive to medication, and that’s only from a number of years using rather large doses of Quetiapine and Benzos, and occasionally antidepressants, to treat my insomnia.
The insomnia is the one thing that is bringing me on my knees and would like to hear more about what I can do – going medicine free is simply not an option as I will most likely kill myself from just a couple of nights worth of sleep deprivation (my intolerance to sleep deprivation is extreme).
I recently came to the conclusion with the help of this blog as well as some advice from a homeopath, that LDN and medical marijuana would be worth trying. I tried getting LDN through the NHS here in the UK but failed, as the doctor cannot get hold of small doses (he was quasi-willing to give me a private prescription). It would be free here in Wales. Hearing about dilution was interesting as I live off such a tiny pension that ordering it through the internet would cause financial difficulties – so I might ask again. As for the marijuana, well… It’s very upsetting that they still can’t offer a medical option.
Well, quetiapine and benzos are among the strongest and nastiest medications! Clonazepam in small doses is a good treatment for many CFS/ME/fibro patients, but still benzos have their problems. IMO quetiapine should never be used for insomnia unless all better options have been tried first – and there are probably close to 50 better options.
It’s possible to get a prescription for LDN on the NHS, this PDF explains how: http://ldnresearchtrust.org/sites/default/files/LDN%20Information%20Pack%281%29.pdf
Oh and hair loss!! I have been utterly clueless about my own, and will definitely look into Maija’s suggestions about hormones.
For hair loss, try 5000mg of Biotin, a water soluble B vitamin. Yep, available at Wall-Mart. It works! RP Not the 10,000 size…….5,000.
I’m late reading this, but I wanted to chime in to say that I’m finally trying LDN, and there’s a compounding pharmacy in Florida that makes 1.5 mg, 3 mg and 4.5 mg doses. The costs are: 1.5mg/30-$12.95, 3mg/30=$17.95, and 4.5mg/30=$22.95, plus shipping. My doctor just prescribed some for me, and I’m waiting to have the LDN shipped to me. If anyone is interested, here’s the pharmacy info:
http://www.skipspharmacy.com/wplog/services/low-dose-naltrexone/
Prescriptions can be called, faxed or emailed in as follows:
–800 553 7429,
–fax it 561 218 8873
–email it to info@skipspharmacy.com
I have no financial interest in the pharmacy. (just so you know. 🙂