



We report here a surprisingly high prevalence of clinical and electrodiagnostic (EDX) abnormalities implying a demyelinating polyneuropathy, suggestive of chronic inflammatory demyelinating polyneuropathy (CIDP), in FMS. Caro et. al 2008
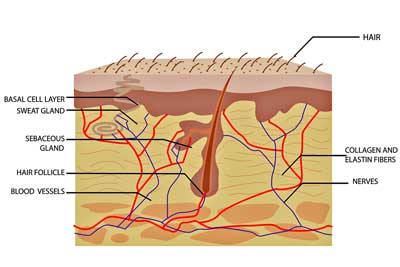
Interest in the skin 30 years ago in FM lead to the nerves and findings of small nerve fiber neuropathy
With three studies finding evidence of small fiber neuropathy in significant numbers of people with Fibromyalgia, the skin has become of increasing interest. (Small fiber neuropathy refers to damage to the small nerve fibers in the skin. Skin biopsies are used to determine if SFN is present).
Caro was the latest researcher to find evidence of nerve problems in FM and it turns out he was the first as well.
From Immune Problems in the Skin
Science often moves slowly and it has in this case as well. Thirty years ago in 1984 Caro found evidence of an autoimmune process – IgG antibodies in the dermal-epidermal junction – in the skin of people with FM. Two years later he validated his findings in a blinded study. That same year Dineman found increased prevalence of Raynaud’s phenomenom, dry mouth, low complement, ANA and IgG antibodies in the skin as well. Something unusual appeared to be occurring in the skin of people with FM but progress defining it was slow.
To the Nerves….
In 1988 Sim’s study “Symptoms mimicking neurological disorders in Fibromyalgia” put a focus on the nerves. Caro reported on nerve conduction tests in FM in 2005 and then in 2008 provided the first evidence of peripheral neuropathy.
Small fiber neuropathy is kind of the rage in FM right now, but Caro’s 2008 study suggested that larger nerve neuropathy (demyelination) was also present. In this blog we take a look at that 2008 study containing 58 Fibromyalgia patients.
The Study
X. J. Caro, E. F. Winter and A. J. Dumas. A subset of fibromyalgia patients have findings suggestive of chronic inflammatory demyelinating polyneuropathy and appear to respond to IVIg. Rheumatology 2008; 47;208–211
A ‘demyelinating polyneuropathy’ was reported present when EMG and nerve conduction studies revealed nerve conduction speeds two (and often three) standard deviations below normal in two or more nerves. (Nerve signals travel more slowly in demyelinated nerves.). Caro et. al followed standards proposed by the Inflammatory Neuropathy Cause and Treatment (INCAT) group for demyelinating polyneuropathy.
The Findings
With 76% of patients reporting paresthesias (tingling), 88% percent reporting hypaesthesia (loss of sensation – with increased loss in the lower extremities) and 90% reporting weakness, the symptom presentation in FM suggested nerve damage was present. (The ‘stocking distribution’ of nerve symptoms which involves worsening symptoms the further down the limbs one goes is highly emblematic of peripheral nerve disorders.)
Greatly increased rates of nerve symptoms as well as muscle weakness in people with FM (90%) compared to people with rheumatoid arthritis (13%) suggested FM was a far different type of disease than it’s rheumatological counterpart. (Martinez-Lavin found that 95% of FM patients as opposed to 30% of RA patients reported sensory symptoms as well).
Nerve conduction studies revealed a polyneuropathy was present in almost 50% of their FM patients. Seventy percent of the FM patients with polyneuropathy had evidence of demyelination. (Note that demyelination refers to large nerve fibers; small nerve fibers are not myelinated.) Sural nerve biopsies suggested myelin injury (segmental de and re-myelination and/or myelinated nerve fiber dropout) had occurred in the majority of those tested. (They revealed no vasculitis or amyloidosis and provided little evidence of what was causing the demyelination.)
Chronic Inflammatory Demyelinating Polyneuropathy
Comparing FM to chronic inflammatory demyelinating polyneuropathy (CIDP), Caro put FM squarely in the realm of an immune mediated neurological disorder.
CIDP is an inflammatory disorder affecting the peripheral (as opposed to the central) nervous system. Considered a chronic form of Guillain-Barre disease, CIDP is characterized by the loss of the myelin sheath in the larger nerves in the body.
The symptom presentation is quite heterogeneous and includes weakness, fatigue, numbness, tingling, pain, difficulty in walking, burning pain in the extremities, sudden onset back or neck pain radiating down to the arms and /or legs. Loss of deep tendon reflexes (rarely increased or normal), loss of muscle mass and fasciculations (twitching) may be present. Autonomic dysfunction can cause problems standing (orthostatic intolerance, bladder, bowel and/or cardiac problems).
Left untreated about 30% of CIPD patients will end up in a wheelchair.
FM patients were determined to have a CIDP-like illness when they exhibited lower extremity stocking hypaesthesia (loss of sensation), muscle weakness in at least two extremities, and evidence of a demyelinating polyneuropathy.
Following Latov’s proposal that “most acquired demyelinating neuropathies of otherwise unknown etiology are considered to be a form of CIDP’, Caro and Winter proposed that a significant subset of FM patients have a form of CIDP.
CIDP is another disorder with decided overlaps with ME/CFS and FM. As with ME/CFS, the lack of agreed upon clinical criteria have thwarted clinical trials. It’s widely acknowledged that the criteria often used to diagnose CIDP misses many leaving many untreated (including ME/CFS and FM patients????)
Treatment
Treatments include steroids, IVIG and immunosuppressive drugs such as Rituximab. Suspecting that an immune mediated nervous system disorder similar to CIPD was present Caro started IVIG treatment in 15 patients. A ‘large percentage’ reported significant improvements in pain, tender points and strength.
Update
Since Caro’s 2008 report indicating reduced nerve conduction and possibly demyelination of the large nerves in the body, Nacir. et. al found widespread evidence of decreased nerve conduction velocity in the upper bodies of FM patients.
Conclusion
This study and others suggest that some people with FM could have both small and large fiber neuropathies. If you have symptoms similar to those described above nerve conduction tests (for the large fiber neuropathy) and skin biopsies (for the small) may be warranted.
Caro and others propose that the neuropathies in Fibromyalgia are probably immune mediated and proposes immune therapies for them.
.









Great article… If ONLY more doctors would learn about Buprenophine for neuropathic issues. I have SUFFERED for over 35 years with debilitating pain…and NEVER got a GOOD DEEP sleep in all those years… I didn’t think I was long for this world.
Was taking 10 Norco a day…for the pain…then traveled to see Dr. Madill in N. Calif and he told me he wanted me off of the opiates right away… I said “gladly” but then I would have to resort to a GUN!
He explained how Bup is used widely in Europe for Neuropathic issues…yet only used here in the US for Addiction issues…
I have now been OFF of all opiates for almost 10 months…and have not slept better since I was a child…..
I take 1/2 to 1 pill a day…and the only side effect is some constipation!
Someone needs to get the word out on this MIRACLE substance and how it can really alleviate nerve pain!!!
Hope you all check it out!
Jacque
Congratulations Jacque – didn’t know buprenophine was used for nerve pain. What a difference it made! Thanks for passing the word along. It’s nice to find new wine in old bottles.
Where is Dr.Madrill in Northern California? I live in Brookings Oregon on the Oregon coast. My pain is bad getting worse. I have been tested for neuropathy and have both small and large nerve damage. I desperately need a physician. Thank you.
Thanks, Cort, for reporting on this very helpful study. I am certain I have the large nerve problem as well as the small nerve kind.
Cecelia
Big talk among some that have POTS and are finding SFN to be something we also have. As you know, I have FMS too. (I question whether or not EDSIII and /or FMS as being the same thing. But that’s a whole other topic.) I also wonder if there is a genetic component too. I do believe there is autoimmune issues and inflammation would go hand in hand with this.
I did an experiment recently on myself, with a bad outcome. Here’s what I tried and the results. Gabapention is a med used for neuropathy. It ups Gaba and lowers glutamate. One thing it helps is neuropathy pain and sleep. It increases Gaba and would increase the parasympathic nervous system. In HyperPOTS we are more in a sympathetic mode – our bodies hype up that response – probably as a compensatory response. Lowering that response threw me into all the nastiness that POTS has to bring. I had near passing out, hot flashes, dizziness, naseau, headaches and some pretty bad tremors. It did help the pain and also sleep was much better. But the other things were just not tolerable. Sooooooo, could the increase of glutamate and decrease of Gaba be what is increasing that response and actually be a good thing, but maybe could be increasing our pain?We know that with HyperPOTS there is a big increase of NE with standing, therefore an increase in the sympathetic nervous system.. This also can cause an increase in heart rate and contribute to the tachycardia we experience to get our blood to go where it needs to be – our heart and our brain. But maybe there is an increase of glutamate as a compensatory thing too? Changing that with meds was not a good thing for me with POTS. But the neuropathy and body pain is not good either.
My dad had Guillian Barre and did IVIG for it. It did not help, and he has the chronic form of it now. He got it from taking a flu vacinne. It can also happen with pneumonia vaccines. With my having Hypogammaglobulinemia and low IGG levels, they wanted to do a challenge on me. Knowing his experience with the vaccine I wouldnt go there. Of the 26 types of pneumonia they tested me for, I have a very teeny, tiney immunity to only 6 kinds and none to the others. The Mayo docs made sure I was aware that it could kill me if I get it. I have to be super careful where I go and try to be very aware to not get around people who are sick.
Issie
Your family is a case study waiting to happen.
Stay away from sick people!
Sign me up!
My sis, (her kids (we hope) is a patient(s) of Dr. Bateman. I’d gladly go to SLC and let her have some blood or run some test. Both of my sisters twin boys have started passing out from what they think is POTS. One they think has EDS and MCAS (like his Aunt) and the daughter has what appears to be HyperPOTS and, thankfully, she doesnt pass out (like her Aunt). The kids will soon start their testing. Sis has really bad CFS and OI.
There either is a genetic flaw, or we had passed on to us something during pregnancy – and now we have passed it on. It may manifest in different ways, but appears to be all connected. My grandmother, we think, had POTS too. (I have my own theories based on what I’ve learned about myself. And, it can be passed on this way.) I’m getting better with what I’m doing. But, stress makes everything worse.
Yes, our family should be in a study. Any docs want us to be their guinea pigs?
I’m trying to stay away from sick people. But, hard to do with the situation I’m having to try to manage right now. Sad how unaccomadating the ERs are when you have to go there. First thing you do is grab a mask and see if they will let you hide off in another room. (They won’t. ) Seven hours later, you wonder if you signed your own death sentence trying to get someone else seen about. (This is another story for another day. :0 ). I didn’t get sick, thankfully.
Issie
The findings are interesting to me as I have recently developed some transient events of paralysis of specific muscles groups. Duration can be from an hour to a few days. I’ve found no remedy other than totallll bed rest and amelioration through low dose Cortef and /or DHEA. I just lay there and wait to heal. Oddly, before this paralysis bs started, I had taken the Cortef and DHEA for pain only …not to regain feeling or the use of a limb, lol. Augh. This disease is a trip. It would be a better trip if there were an authority figure /physician to ‘trust’. Hard work being sick and getting a lay medical degree at the same time. The docs I can access are not the best. I am in a rural area and pretty much my own doctor. Money walks and money talks. Wait…lol…Sometimes even money can’t walk. I am so sorry everybody. I wish all who suffer a bit of hope and ease.
Great synopsis…….lots of evidence of immune mediated damage in FM in the literature now.
And yet every article I read begins with “the mysterious disease of Fibromyalgia, pain from now where, with no abnormality showing on tests “.
I can just imagine the blank stares I would get asking for IVIG or Rituxmab for my “non-progressive” benign condition.
Dr. Caro is quite a pioneer!
Exactly. Research is one thing and reality another. I get condescending stares from most physicians. I need that to change. Right now my life is like being under shark attack while a few bystanders smile and wave, wish me well.
Well Clauw continues to say apparently that it’s all central sensitization and I just saw on a big FM Facebook saying that FM is all central sensitization. Even the National Fibromyalgia Association mostly says that.
They’re missing the muscle and nerve connections in the body…I am sure that we’ll see many more FM studies on SFN coming out.
I think Dr. Clauw has held on to his central sensitization theory for a little too long. It is important for a clinician to adjust their hypothesis about disease aetiology when new evidence arrives
For those interested, Dr. Caro has some interesting comments on Clauws fibromyalgia paradigm and points out some rather sweeping omissions from his understanding of the pathogenesis of FM. He also indirectly states that rheumatology as a specialty, is not in the best position to discuss FM.
An excerpt from Dr. Caro…
I read Dr. Clauw’s recent review of the pathogenesis and therapy of fibromyalgia (FM) with a good deal of interest.1,2 While his description of FM as an example of “central [nervous system] sensitization (CS)” resulting in pain amplification has appeal on a heuristic basis, I believe that it fails to identify a fundamental pathophysiologic explanation for the initiation and perpetuation of pain in the FM syndrome.
For the full response…..
http://www.the-rheumatologist.org/details/article/865823/Letters_to_the_Editor_Feedback_from_the_Readers.html
Cool – thanks for pointing that out. I heard Clauw a couple of years ago say there was rising evidence for peripheral inputs but they always seem peripheral to his theory. I imagine he’s rethinking as we get more evidence of SFN and peripheral factors.
…”peripheral to his theory”…… LOL !! That cracks me up 🙂
Thanks for the interesting article, Cort. I have all the symptoms and have attributed them to any number of things. I believe they’ve all come together in a big picture (CIDP) thanks to your article.
I’m with Nina when she says, “I can just imagine the blank stares I would get asking for IVIG or Rituxmab for my “non-progressive” benign condition.” !!
This is how I cope without access to a specialist:
Canes for walking because weak legs and numbness in the lower extremities cause quite a bit of stumbling and bumping into things. Falling is a big and scary issue with me. People rushing to my aid makes me uncomfortable.
The use of a transport wheelchair if you have someone with the time and ability to push.
Power wheelchair for the home on your weakest days. I’ve put laundry baskets on my lap and run them back and forth like a trolley.
Lyrica for pain. This one of the best pain relievers I’ve used. Cymbalta is second.
Very low dose beta-blocker for POTS. This has been working for me for years. Ironically, it’s not the POTS keeping me down these days; it appears to be the CIDP.
For twitching (if it is bothersome), I take a miniscule amount of klonopin.
The sudden deep radiating pains for me are transient, thankfully.
There are times when I am driving to or home from the doctor’s office, I lose all function in my lower legs. I switch to “cruise control” and drive with my thumbs until I can regain enough energy to use the brake and gas pedal.
It was people like you like you I was thinking of as I was doing the blog – people with weakness and motor problems – who may be missing a diagnosis that lots of doctors are apparently not all that aware of.
A very timely article for me, Cort. Particularly this section comparing FM and RA: “Greatly increased rates of nerve symptoms as well as muscle weakness in people with FM (90%) compared to people with rheumatoid arthritis (13%) suggested FM was a far different type of disease than it’s rheumatological counterpart. (Martinez-Lavin found that 95% of FM patients as opposed to 30% of RA patients reported sensory symptoms as well).”
I have become very accustomed to episodes of numb hands. Until this weekend, the problems in my feet/legs have been limited to icy coldness, itching, twitching, and nerve pain. On Saturday, I got up from a seated position to answer the phone, not realizing my right leg and foot were completely numb. My leg collapsed, and in the process I sprained an ankle. This sounds like a mild example of what Polly has described (above).
Since the numbness and other neuropathy symptoms started after my RA diagnosis, I assumed this was the cause. Now I’m not so sure. Thanks for the information.
You know what – I was experiencing pretty dramatic problems with numbness and tingling in my limbs about 15 years. It turned out that the problem was that I was eating a lot of fish – and accumulating mercury in my system. My mercury levels were not high – but they were too much for me.
After stopping eating fish – those symptoms disappeared in about three weeks. Just wanted to pass that on.
Hi All.
As I sit here with my hands shaking and eyes twitching along with being capable of falling off my chair I wonder? Where did the fun go? I am very ill and likely have the neuropathy going on in large and small tissues. My butt is numb and has been for years but only on the left side. A therapist one day asked me what I felt when she did the pin prick thing. Minutes passed as I said I felt zero. She said she had been jabbing a muscle on my butt that had zero response.
Ahh the days of jabbing pins. I found it funny because at least one part of me was without pain. Memory is another thing entirely. Mine is shot full of holes. I tried to post a comment in linkedin and lost it after forgetting to save it or send it. Sigh.
The article you have above Cort is one that is needed to be read in every medical school. I wonder what the authors have studied since. I have POTS and likely POSH as my heart rate has been going wild lately and even with many sleep aids my heart keeps nattering away all night. My cpap machine fails to work with both trial masks so I need to try something different. My breathing is so shallow it fails to push the nose flaps up up and away. So I gag and shove it off. The nose and mouth most often end up pushed into my hair. So my husband tells me and that must be a sight to behold as I snore with that great big thing grasped tight in my long hair.
I need this blog so please sign me up. My website is about the future and what I believe could be the result of what people and the cosmos together do with our galaxy. I am a zoologist and a futurist both by training and love of learning along with being a liberatary learner/teacher when it comes to sharing ideas with communities. I have been too shaky to do much with it for a year or so. The idea is to read and write about books we have today, how we treat ourselves and our planetary system, which leads to 3012 and how our world has changed. It is a continual work in progress. It gives me something to stretch myself as an artist in words and a seeker of knowledge. I am searching for money for a PhD in love, harmony, peace and music so I need a way of recording the songs that seem to burst from me and which I fail to remember along with the poetry my prof used to love to read when I wrote late at night for my thesis.
I guess what I am saying is that I am defined by my action and inaction. I have 22 diagnoses including large neuropathy and hand/arm shaking during research fun at Univ of Calgary. My doctor knew me and he knew I would try anything so his research team did a lot of funny and very odd tests on me which startled all of us sometimes. The Doctor used to laugh out loud when I lost my perscriptions. One day I left and the darn thing went down the elevator shoot with a whoosh. So up I went again and luckily found him and soon as he saw me he began to laugh and so did I as this was the shortest time lost. He also then told me to take the medicine after defending my thesis because it would make me sleepy. So the imps of mischief put things right by swooshing my prescription away so that I would be able to stay awake while defending my thesis.
I am Cindy Birdwise and I love to read and write, to create things like the Canada Trail, a Univ specializing in leadership and sustainability while learning online, engaging communities in building for the future like using old tires turned into thick rubber mats to help protect buildings from the actions of perma frost. I wonder if it worked.
I think that one problem is that fibro is commonly referred to in the ‘mainstream’ medical community as ‘chronic widespread pain’, but there are lots of different kinds of pain. There’s joint pain, muscle pain, nerve pain, etc. and I might be mistaken, but it seems like I’ve heard different patients diagnosed with ‘fibro’ complain of each of these. Exactly what kind of pain is widespread in fibro? I knew a lady who was diagnosed with fibro and she said that it felt like her skin was on fire. To me this is a pretty damn specific kind of pain. It seems by not differentiating different kinds of pain you’re just comparing apples to oranges to grapes to cherries.
John, Fibromyalgia pain must be felt in all four quadrants (including joints) of the body which makes it “widespread.” It frequently moves around and settles in different parts of the body. It used to be diagnosed by having 11 of 18 tender points. It can be an achy feeling combined with jabbing, stabbing, and burning sensations. The pain is thought to derive from the central nervous system.The individual’s perception and descriptive language of what he feels will result in different terminology, so consequently you may hear oranges and apples. Understand that to the sufferer, we hear it as apples and apples.
Cort’s article, however, refers to nerves in the SKIN rather than pain from the central nervous system. “With three studies finding evidence of small fiber neuropathy in significant numbers of people with Fibromyalgia, the skin has become of increasing interest . . .”
In addition, studies have shown large fiber neuropathy is also present. As a ” . . . chronic form of Guillain-Barre disease, CIDP is characterized by the loss of the myelin sheath in the larger nerves in the body. Caro’s 2008 study suggested that larger nerve neuropathy (demyelination) was also present.” Please note the various symptoms and types of pain (in the article above) that accompanies this condition.
When I read the article, I missed the “problem” that you evidently noticed. Rather I related to a startling condition in fibro sufferers to which myself and several others can relate.
(Many apologies if I sound “preachy!”)
Thank you Cort,
You’re website is one of my info lifelines. I too like Nina, live in no man’s land for access to Drs who know what to do w/ ME/CFS/FM. Would a reg family practice Dr be open to having these tests ordered? Can they be done locally by anyone or is the accuracy of the tests dependent on someone very experienced, knowing what specifically they are looking for.
I have been presenting for some time with neurological symptoms. A few yrs ago, an MRI was done. I was certain they would at least find the abnormalities that I’ve read so much about in other ME cases but nothing. I’ve often wondered was it bc they didn’t know what to look for or bc they really weren’t there.
The list of symptoms caught my attention bc I am deteriorating. Severe muscle weakness in my legs & burning pain in my neck radiating down to my arms as well as weakness has made it necessary to purchase wheelchair just to get from my house to the car. I have icy cold hands & feet always while my core & upper thighs are like a furnace. Not so much numbness & tingling, would that in itself rule it out for me? My ND, using Asyra has picked up on peripheral NS problems. But the muscle weakness has become terribly debilitating. It goes from severe weakness to building burning pain on top of that to losing control of the muscles, jerking etc. any ideas anyone?
Maybe MG (Myasthenia Gravis) or maybe Stiffman Syndrome (Jerking Mans Syndrome). Some have found this in connection to autonomic nervous system disorders, (POTS, etc.) Many of us with POTS have what we call tremors and many also have SFN issues.
Issie
Great article Cort! I was recently diagnosed with a small-fiber neuropathy through lab work and a skin biopsy, although I could have told you ten years ago that was the case due to suffering from autonomic symptoms, numbness, and pain. Of course treatment is only palliative.
I know my symptoms go past a small-fiber neuropathy, but it seems a waste of time to pursue further diagnoses because there is no way I’ll be treated with IVIG or immunosuppressive drugs such as Rituximab.