



September 2013
“We conquer not in any brilliant fashion – we conquer by continuing” – author unknown
Current Medication Protocol:

(Medication Changes: Since testing began after an inflammatory lesion was found on my cervical spinal cord on an MRI in February of 2013, I have been off IVIG (Gamunex). With all of the testing that followed and the time and energy required to complete them, I discontinued my trips to my local doctor’s office for the IV amino acids (Aminosyn). I was able to continue, and in fact, increase my intake of IV saline through my home health nurse, which I found to be helpful. I switched my epoetin alfa injection from Procrit to Epogen only because the latter is less expensive and this is one drug I must pay out-of-pocket.)
Background
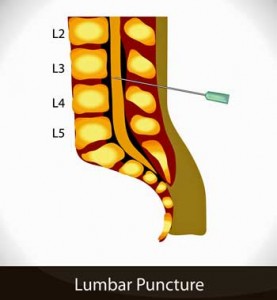
In this blog, I will update you on the travels and investigations that continue on. To summarize my last blog: I saw a neurologist, Dr. G, at the University of San Francisco, to whom I was referred by Dr. P. After completing the long list of scans and other tests ordered by Dr. G, all of which returned “non-definitive,” Dr. P and I decided that I should return to Incline Village to have another lumbar puncture (LP), #3 to be exact, hoping that since I’d been off IVIG for five months, we would have a better chance of finding something.
My last LP was February 2013 while I was on regular IVIG infusions. The theory is that the IVIG could have masked something as the expected inflammatory properties were not seen in my last spinal fluid test.
In Dr. G’s opinion, the very mildly hypermetabolic lymph nodes in my chest area – not at all enlarged and non-specific in nature – are what he wants to go after next, suspecting neurosarcoidosis and suggesting a biopsy of those nodes. Relative to the tests I’ve done so far, this one would be much more invasive. I chose instead to take my chances of finding something in my cerebrospinal fluid (CSF).
Visit #11
My first LP was done at my very first visit to Dr. P in June of 2009. It was a breeze. My second was in February of 2013, the day after the cervical spinal cord lesion was discovered. It too was uneventful. As a result, I have no trepidation in doing a third.
My travel choice is the two day car trip, as flying alone always seems to be so much more taxing. Like always, I commence a search for assistance. Having been blessed by so many helpful angels in the past, this time is no exception. Suellen (spelled like Suellen in Gone With The Wind), a volunteer at my church and a friend who conveniently lives two blocks away, offers to take me. Locked and loaded, off we go on another of the only road trips I ever get to take – to a doctor’s appointment!
Day One/Two (Saturday and Sunday)
The company is great and thus, time flies. Suellen is a gem of a companion, so helpful and empathetic. She gets it! Most everything goes smoothly except for the fact that my neurological symptoms have unknowingly worsened to the point that it has become uncomfortable for me to sit in a car seat that is far from being as soft and cushy as my recliner at home. I find myself shifting my weight often, trying to find a position I can tolerate for a period of time. Things ache, hurt and burn and are perhaps an omen of what is to come. But I manage well enough and we make it safely to Lake Tahoe by Sunday afternoon.
Day Three (Monday)
The LP is scheduled early at 7:00 a.m., even before I visit with Dr. P. Since it must be followed with 48-hours of lying flat, it’s best to get it done ASAP. This also increases the chances of getting lab results back by the end of the week.
Nurse C whisks me off to the exam room where she gently places me in a fetal position on the exam table, prepared for Dr. P’s grand entrance. I know that my most recent health issues have been a challenging mystery to all so as he walks in I remark, “You must be frustrated to see me again.” “Don’t be silly” he says with a smile. “You were invited to come back.”
Dr. P proceeds to inject Lidocaine into the skin area to be punctured. I experience a dull, aching, nauseating pain down my leg. I’ve never had pain during this procedure before, so I am wondering if something may be wrong. I express my discomfort “Ouch!”
He tries again….”Ouch… OUCH!”
As I start to sweat, Nurse C wets a paper towel and applies it to my forehead. Obviously I am looking pale and faint. Dr. P seems surprised as he tells me he is only administering the numbing agent with a small needle into the skin. He hasn’t even started the lumbar puncture! He expresses concern that this must be a result of the disease process – this hypersensitivity. I take some deep breaths in an attempt to relax. Thankfully, the actual needle puncture into the spinal column is not anywhere near as painful as the skin sensations, and soon Nurse C is saying “we’re in.”
Dr. P is perplexed but actually this is consistent with what I’ve been experiencing. Slight brushes against my feet or legs can cause my legs to jump – but if my legs are firmly grabbed, I am not as sensitive. No longer in pain, it is just a matter of now waiting the ten minutes or so for the three tubes to fill with my CSF.
When the procedure is done, I am wheeled into the room that I call the “rest and recovery room.” In the past, I have been able to relax, nap and infuse fluids for the entire day that I am required to remain there. So, thinking the worse is over, I let out a sigh of relief. But this is not the case today. The misnamed “rest and recovery room” becomes Grand Central Station! It is important to receive my IV saline as the fluids help me replenish my CSF, but I am not allowed it until my blood draws are complete. First comes the many vials drawn for Lab Corp – this is usual for every visit.
But this is followed after several minutes by another needle poke in order to draw blood for the Cleveland Clinic and other faraway places. Just when I thought my blood donation was complete, Dr. P’s research coordinator, Gunnar, apologizes for needing to poke me yet again to draw blood for the CDC Study. Nurse J sums it up perfectly when she says “Corinne, look at it this way. Your body fluids are going on vacation all over the country, but you’re staying right here.” J
Now that my IV saline is finally set up, I mistakenly think I can now rest but the staff continue to come in and out with form after form to be signed – papers that will accompany my blood and CSF to the many labs, as well as for insurance. By now it is well past noon and I’m starving.
This time I did not prepare a filling meal to bring along. Instead, I munch on some almonds, yogurt and a banana. The room is cold and because I am infusing room temperature saline, I’m shivering. What I really crave is a steaming bowl of soup. Though I know that I can give Suellen a call if I need anything, I give up on that idea when I decide that I’m actually more exhausted than hungry. I decide to try to rest, but it isn’t long before the saline does its thing – trigger the urgent need to empty my bladder!
Having to remain with my head at or below heart level for at least 48 hours, I go through that always awkward effort to slide off the table and onto my feet. As I use my arms to lift my body into a semi-pushup position, I feel an excruciating pain in my left chest muscle, as if someone stabbed me with a knife. It’s painful enough for the thought to cross my mind…have I dislocated a rib?!
I continue to the nearby bathroom and awkwardly climb back onto the table. The pain is gone but the muscle feels sore. I am wondering if it has something to do with the nerves coming from the spinal cord lesion or if I’ve strained a muscle. Considering all that I’ve been through today, I am feeling akin to a human punching bag – not only tired, cold and hungry, but just plain ol’ beat up!
It is now 2:00 p.m. and I haven’t had a chance to rest at all. It isn’t long before I have to make another awkward trip to the restroom, getting tangled up in my IV tubing during the process. Each effort is difficult and painful. This is by far the toughest time I’ve experienced while having an LP. So far the third time has not been a charm.
I am told not to leave the building until Dr. P sees me. That turns out to be after his last patient, at 5:15 p.m. I’ve been here over ten hours and I’m pooped. Suellen has been waiting in the lobby since 3:00 after spending some of the day exploring Lake Tahoe, but never wanting to be too far should I need her. When Dr. P walks in, he takes a seat and to be honest, he doesn’t look much better than I do. Yawning, he puts his head in his hands, appearing exhausted. How can I not feel empathy for this man’s hard work and dedication?
Dr. P asks how I am feeling and I confess that this time has been tougher than the other two. He tells me where by CSF and blood have been sent (Lipkin for studies, Cleveland and Mayo Clinics, University of Miami, etc.) and remarks that he feels that this time we will find something. He wants to see me again before I return home. Since I have to lie flat another 36 hours and he will be out of the office for a couple of days, our appointment will have to wait until Friday morning.
After asking who I came with, he graciously goes out to the waiting room to introduce himself to Suellen and to thank her for accompanying me on this trip. I am then wheel- chaired out to the car and trying to remain as flat as possible in the passenger seat but in a boatload of pain from the contorted position, I grit my teeth during the 25 minutes back to the hotel, where I plop myself into bed to stay.
Day Four (Tuesday)
I had a rough night. Turning is difficult as that stabbing pain in my left chest has become a very sore muscle, not at all conducive to bearing weight. The soreness reminds me of my pre-illness workout days when I would do too many pushups.
Today I am allowed to use a small pillow but I still have to remain relatively flat, hopefully to prevent the dreaded post-LP headache that can occur. The hotel staff brings me my early breakfast while Suellen furnishes me with a nourishing lunch.
I can’t say that I am comfortable in any position. I try my best to rest in between efforts to fill out the many pages of the CDC Study questionnaire for this year. I have little desire to watch TV or make phone calls – I just feel sick and hurt everywhere. Oh well, maybe it’ll be better tomorrow when I’m finally allowed to sit up.
Day Five (Wednesday)
This morning I was hoping to be able to get out of bed and walk down the hall to the hotel’s breakfast. Not a chance. I didn’t sleep well again and I just feel so ME/CFS sick. I am able to sit up, walk to the restroom and get dressed, but that’s the extent of it. Suellen brings me breakfast as I spend the day finishing the CDC questionnaire and resting.

Getting comfortable has become more and more of a challenge since the appearance of her spinal cord lesion 8 months prior
I continue to be uncomfortable in most positions, making it apparent to me the effects this inflammatory spinal cord lesion has had on my overall condition – especially my tolerance and resiliency.
I’m disappointed that this LP was so much more difficult than the previous two. It’s always disheartening when you realize that you’ve declined. Maybe it’s a good thing that I’m feeling this ill while answering these questions for the CDC. Perhaps my misery will somehow be conveyed to them in my answers.
The good news for today, as I spent it upright – no post-LP headache! J
Day Six (Thursday)
Today I am feeling a little better – well enough to walk down to breakfast and then tackle that always daunting task of showering and washing my hair. Suellen has been waiting and staying close by should I need anything, but I assure her that I will be fine and encourage her to go out and enjoy the beautiful day. After providing me with a lunch I can eat later, off she goes.
Why is it that I always have such high expectations prior to each trip here? “Maybe this time I can go on a drive around the lake”, or “maybe this time I’ll go on that long-wished for sleigh ride”…”maybe this time”, I always seem to tell myself. But “this time” never happens. Being ill for 23 years I am not surprised at the inability to accomplish these goals. I think what surprises me the most is the fact that I keep on setting them. It’s amazing that there remains a resiliency of spirit, if not of body.
After Suellen leaves alone and I nestle back into bed, I think once again…”Maybe next time.”
Day Seven (Friday)
Dr. P wants to see me before we head for home. Some of my labs have returned but there is nothing of significance. He discusses what I’ll do next, depending on the rest of the results. He lets me know that if I end up doing the mediastinoscopy (thoracic lymph node biopsy) that it is an easy procedure, rather routine. He relays to me the fact that Dr. G is very concerned about me, in a good way, and explains how pleased he is that Dr. G has been aggressive and remains very interested.
Even with all this positive talk, I think Dr. P can sense that I’m frustrated. I will be completing another trip, another appointment, another bunch of tests without any treatment for a condition that was considered serious and urgent when it was discovered seven months ago – and with symptoms that have slowly worsened. It is here that he reassures me that these type of neurological issues are slow to progress – one or two more months won’t matter much (to who!?).
Apparently, I must appear somewhat disheartened because suddenly the image on his face changes from logical doctor to compassionate friend….”but in the meantime you are suffering, right?” I nod my head. “When I first met you, I told myself if I could not help you, I would find someone who could.” As he holds up my file he adds “This has really become quite a challenge and I love a challenge. I’m in this for the long haul. I will not give up on you.”
Teary eyed, we exchange hugs as he reminds me he will be in touch. Sitting alone, I reflect on how many years and how many doctors I have had to go through to get this kind of support.
When Nurse D comes in, she tells me the doctor wants me to have a bag of saline and Depo-medrol and Toradol injections for the road. Apparently the “in the meantime you are suffering” comment was not for show. He is making sure I have something to help with the inflammation and pain on the way home, along with the boost in blood volume the saline gives me.
Having an illness like ME/CFS where it is not often one is offered by the medical community even a small possibility of hope or promise for relief of the constant suffering one endures, I am most thankful for this gift. Perhaps this gesture will actually help make my trip home semi-enjoyable even though I am well aware that steroids such as depo-medrol are not to be taken lightly and are not something that I could use on a regular basis.
By 10:00 a.m., Suellen and I are on the road for the first half of the drive home. By mid-afternoon I feel the steroid kick in as I become a bit energized and the edge has been taken off the pain. The side effect, however, is that I cannot fall asleep until midnight. Oh well, can’t win them all. J
Day Eight (Saturday)
Despite the lack of sleep, I do well during the six hour ride which flies by with music, prayer, laughter and loads of talking. Suellen has been a wonderful “Visit to Dr. P” companion – a true blessing. It never ceases to amaze me how I can get through these trips in spite of being so ill – accomplishing not just another doctor visit but another lumbar puncture to top it off! However, it is clear that none of it would be possible without the help of so many. Thank you angels!
CONCLUSION
Recovery from the trip went well. I felt pretty good for two weeks, perhaps due to the Depo-medrol and Toradol injections. The other good news is, nothing unusual showed up in my test results. The bad news is, nothing unusual showed up in my test results. Same old song, just another verse. Here is a partial list of the extensive things I was tested for:
In my CSF: Mycoplasma, Chlamydia, Oligoclonal bands, Lyme, West Nile, Herpes Viruses (HSV,EBV,CMV,HHV-6&7), Measles Rubeola, Mumps, Varicella Zoster, California Encephalitis, St. Louis Encephalitis, Eastern and Western Encephalitis, LCM Virus, fungus, Angiotensin Converting Enzyme (ACE), cell count, lactic acid, acid fast bacilli, malignant cells, glucose and amino acids.
In my Blood: All the conventional stuff in addition to IgG subclasses 1-4, T&B cell gene rearrangement, NK cell numbers and function, ACE, C-reactive protein, Toll 3 Receptors, cytokines, and a lymphoma panel.
The only abnormalities in my CSF were elevated HSV antibodies and a slightly elevated ACE. Not even the expected inflammatory properties in the cell count that the neurologist expected would appear now that I had been off IVIG, showed up, which makes me quite an anomaly in anyone’s book! An inflammatory lesion with no obvious “inflammation” – go figure!
My blood exhibited the usual elevated herpes virus antibodies (EBV, CMV, HSV) and slightly elevated ANA and high CD4/CD8 ratio – all which can suggest autoimmunity. But at the same time, I lack the more common signs of AI – high SED rate, C-react, protein, WBC’s etc. My NK cell function was low/normal.

Once again the tests reveal nothing definitive; the cause of Corinne’s spinal lesion remains unclear
So, with nothing definitive revealed, Dr. P suggested I proceed with the mediastinoscopy which Dr. G (the neurologist) was hoping would confirm his suspicion of neurosarcoid. In his words a diagnosis would lead to a more targeted treatment of Remicade (a TNF-alpha blocker) and methotrexate (an immune suppressor) which he says he has good results with in his NS patients and would be preferred to treating me empirically with a wide spectrum immune-suppressor such as high dose IV steroids.
(His view is strictly one of autoimmunity, whereas Dr. P has to take into consideration what he firmly believes as critical – the immuno-suppressed component of ME/CFS – in fact at one point stating that he could not consider treating me with high dose steroids as he would be afraid of hurting me.)
Meanwhile, however, Dr. G’s consultation with his colleagues at UCSF determined that the biopsy of those mediastinal lymph nodes that were mildly hypermetabolic on the PET scan, could not be done easily with a scope down the throat/airway. Because the nodes are too small, it would have to be done in a more invasive way – from the outside in, and thus becomes a minor surgery involving general anesthesia and an overnight stay in a hospital L.
When I suggested possibly doing it somewhere closer to my home, both doctors agreed. Not sure what the procedure entailed, with a referral from Dr. P, I made an October appointment with a thoracic surgeon at the Mayo Clinic. In doing so, I was hoping to get more details that would help me decide on whether to proceed or not – knowing that this would probably be the most invasive testing I’ve done so far and no matter how minor, it would not be easy on me.
In the interim, I noticed that each flare-up brought me to a new level of worsened neurological symptoms to which I did not recover. Thus continued the slow but steady progression of this disease process – whatever its name might be.
Eight months had gone by and still no diagnosis, no treatment, no cause for this spinal cord lesion. With the Holidays right around the corner, I was anxious to move forward. The next step was the Mayo Clinic – two hours rather than a two day drive from home and ironically the first place I turned to seek help when I fell ill in 1990, only to be told there was nothing physically wrong.
Back then, I was sent home with the assumption I was depressed and the suggestion that counseling might help. Funny how life works. I had come full circle. Gee, I wonder if counseling 23 years ago would have prevented this spinal cord lesion (she says with sarcasm). Guess we will never know. J
Til next time…Feel good!
Next stop…Mayo Clinic.









Such a long hard time to endure! We all wish for some relief soon. Interesting to note though that there are many other proven factors that influence the post LP headache however laying down for 48 hr has definitively been proven not to be one of them!
You know what didn’t work for me? Hoisting my heavy travel bag to the overhead luggage rack on the bus to the airport. I was fine until then ….
I think I need to make it clear about the 48 hours. That is not standard protocol for an LP…only for Dr. Peterson because he takes so much fluid… three times as much as anyone else, maybe more. He keeps so much at sub-zero temps that I have been able to be tested for many things even years after the LP…no other doc I know does that. The shock to the brain with that much loss in fluid is therefore different in this case.
well it seems to work. I know others who didn’t follow the protocol and ended up with massive headaches. (Cort are you listening?):-)
Thanks for the well wishes!
Yes, indeed 🙂 That headache I will never forget. Simply lifting my head from the floor was agony. It lasted about five days and the poof! it was gone.
Corinne;
Have you been tested for anticardiolipin antibodies (also know as anti-phospholipid antibodies)?
No.
Corinne,
I’m so sorry to hear of your ordeals, caused by both the spinal tap and by the doctors’ inability to determine a diagnosis. At least some nasty stuff has been (sort of) ruled out.
Three times I had lumbar punctures in Morristown NJ with a pain management doctor. I had been told by my referring doctor that I wouldn’t have any problems, but I’d heard the stories of resulting headaches and was apprehensive the first time. Well, not only did I not have to lie down for the procedure, but afterward, the pain dr told me I could stand up and go home! I never had the slightest suggestion of a headache.
In your case, at least your better previous experiences prevented any anxiety during the trip there.
I hope that the next procedure is uneventful and easy, and that you rally quickly afterwards.
All the best,
Carol
I think I need to make it clear about the 48 hours. That is not standard protocol for an LP…only for Dr. Peterson because he takes so much fluid… three times as much as anyone else, maybe more. He keeps so much at sub-zero temps that I have been able to be tested for many things even years after the LP…no other doc I know does that. The shock to the brain with that much loss in fluid is therefore different in this case.
I went to Cleveland Clinic Difficult Diagnosis Clinic. The first Internest called me basically a liar and the next two had nothing to express. Total waste of time, money, and energy and made me extremely depressed. Asked me to come back in March (1st trip was November). Maybe just me; but not a good experience at all.
Hi Corinne,
I’m so sorry things have been so tough for you. I know with certainty that no other doctor offers the diagnostics abilities and compassion as Dr. Peterson. We all go through so much that this kind of care is a precious gift.
I did have to chuckle at your “maybe this time”, it’s been my mantra for many years. But, to get through all the many challenges and unknowns this disease brings, a positive attitude, a good sense of humor, prayer and knowing there are so many of us who understand are the best tools we can have for the journey.
I wish you the best of all of these as your journey continues,
Lynda
Hi Lynda!
thanks for the well wishes. I think if we didn’t have hope enough to say ‘maybe next time’ we would have given up a long time ago…and that’s just not in our nature 🙂
Best to you also, and hope to see you in Dr. P’s infusion room soon!
God Bless
Corinne
The ME/Cfs Dr’s are doing an Elisa and telling patients they don’t have Lyme. I have been to an ME/CFS Dr in Manhattan, one at Stanford and an ILADS Dr in NY. The most thorough is the ILADS Dr. Tick borne disease testing is so inaccurate. I recommend reading “Why Can’t I Get Better? ” by ILADS physician, Richard Horowitz, MD. Not everyone has tick borne diseases, but his 16 point differential map is quite thorough. The big name at Stanford had 1 tool in the toolbox…antivirals. I was so disappointed.
Just realized my comment was more of a general rant 😉 So sorry Corrine that you have been through the diagnostic wringer. Soo frustrating. At least it seems that Dr P is quite thorough.
I sure hope you’ll soon get some answers and relief Corinne. Hang in there – you’re a trooper!
We are all troopers!
Thanks for the encouragement.
Just watched a video put out by MEDSCAPE and it indicated that cervical spinal lesions are diagnostic of Multiple Sclerosis. Just thought I’d mention it. marcie
Thanks Marcie, but as I wrote in the blog and in previous ones, the diagnosis of MS was ruled out almost immediately (spinal fluid oligoclonal bands, MRI appearance of the lesion, and the fact that MS c-spine lesions go away in a month or so, etc.). For my case, that would have been way tooo easy! 🙂
So 8 months ago you endured all that, and you are getting worse. I am so sorry for all the hard and painful things you endure.
Especially being near Lake Tahoe and never seeing even a little bit of the spectacular views there, that must sting. I had just one chance in my life to be there, before I got ill, and a two day stay was cut short to overnight by my friend’s illness. I was glad I had walked outside in the dark to see what I could see, and then the little bit as we left in the morning. And recalling the people in the hotel who spent all their time gambling in windowless rooms, as we stated in a hotel on the Nevada side of the lake. I still marvel at their strange ideas of the attractions of Lake Tahoe, those gamblers.
I do hope someone does find out what is making you worse, and that someone has a treatment for it. A 9 day week to be tested, rested, and get home, that is a lot. But more of your story to come.
One question for clarification, what did you mean by AI? Here is the sentence where you used that abbreviation:
common signs of AI – high SED rate, C-react, protein, WBC’s etc
I tried looking it up by putting your phrase into google search, but the top result was this post, so I went full circle.
Thanks.
Sarah
Hi Sarah
Thanks for your comments. Yes, Tahoe is a beautiful place and sad to be stuck in a room. Thank you also for the encouraging words and for reading my story.
AI is auto-immunity. I hope I did mention it in full phrase somewhere earlier. I get anxious to abbreviate whenever I can, being so energy challenged. 🙂
Corinne
Thanks, I figured it was something obvious, but that phrase did not come to my mind.
Hi, Corinne! Respect – you are giving all the help you can to the wonderful doctors who are trying, against all the odds, to figure out ME/CFS.
When I first got sick, 1986, when I finally found out what it was, the received wisdom was that there was no technical medical test, and no technical medical treatment, and what you should do was rest, conserve your physical energy.
Now, as your blog indicates, there are many things which are medically helpful, but still quite a few mysteries, and you still haven’t got a definitive treatment.
Do your doctors ever recommend a break from treatment – a medication-vacation – just to test what your baseline condition may be at the moment, and clarify what your current needs may be? It strikes me that all the trips to the doctor and relatively invasive treatments must be placing great physical demands on your body. You’ll know that right at the beginning, in the 1960’s and onward, Ramsay and Acheson were clear that complete rest, in their view, gave the best prognosis. Would your doctors consider that two or three months without any form of treatment apart from rest and a normal healthy diet, with lots of fluid intake, might be safely undertaken, and provide a means of reviewing your current needs for medication?
I know I’ve been phenomenally fortunate in the course of my own ME/CFS, and my avoidance of medical help might not work for everyone. But it was so sad to read that after all of your medical ordeals, and the most kind and committed doctors helping you, you felt yourself back at the starting post – still ill, still without any advance in your treatment. I really, really wanted you just to give yourself a break – not carry on into ever-more tortuous medical procedures – at least not until just trying out stopping it all for a bit. I wonder what Dr. Peterson’s view would be on this – he has lots of experience, and is passionate and committed to helping…has he ever seen anyone get better by just going into a kind of exertion-hibernation?
Thank you Nancy. I understand completely what you are saying. I have been ill for 23 years and the majority of the time I did exactly what you suggest…rest and no treatment. Most of the time it was through no choice of mine, just simply no doctor nearby who had anything to offer.
I think like most patients who have been ill as long as me, I went through periods where I would try all kinds of things (supplements, meds, etc), and then periods where I would do nothing for years but simply rest. Regardless, it gradually became worse over time.
Yes, the trips are taxing but when a cervical lesion on my spinal cord was found and I was told that the diagnosis and treatment was urgent and there was a distinct possibility of paralysis and incontinence and that I was lucky I was not already so, I felt I had no other choice but to pursue further testing. In fact if you go back two blogs you will find that the first neurologist said I had neuromyelitis optica and that I could become blind. How could I just stay home and rest in the case? For me it wasn’t an option.
My next blog will fill you in on more testing and traveling, but eventually (after a year and a half) I do get a time to rest 🙂
Thank you for your comments and well wishes. Best of health to you.
Corinne
Hi, Corinne, thanks for your reply. I know that both degrees and nature of this illness vary a lot, and that I have been extremely fortunate. Part of that was that I didn’t encounter skepticism, my then husband did all the cooking, and I immediately got a well-paying job which involved going to meetings and writing reports (which I could do at 2 in the morning, if that’s when I felt well enough), I was surrounded by unemployed young men with driving licenses, so I could get chauffeured and wheel-chaired to meetings, the finance office gave me a surplus-to-requirements PC and made me learn to use it —- and and and (my dog even learned to pull me in a wheelchair by grabbing something in his teeth and running backwards – that got me to a meeting in London when there was a tube strike and a 2 hour wait for a taxi!). All of that contributed to managing my life with conservation of energy at the heart of it.
I also took a lot of Vitamin C, deodorised garlic, echinacea, golden seal, probiotics and msm, though that is now not thought to be helpful.
And I came across Les Simpson’s work on blood flow, and now take 6 g of fish oil every day – that makes a significant difference. So rest isn’t the only thing.
But as a determined advocate of rest, as something that first of all the illness forces upon us, and then, unless we have access to medical treatments and can afford them, may be the only thing we’ve got, it is discouraging to know that many people do rest and still get worse. I’ve just written a column for Positive Health magazine (online) in which I write about ethical and unethical uses of NLP – in which I think we need to reframe resting as a way of actively fighting against our illness, rather than, as many people experience it, a form of ‘giving up’. Reading in Health Rising about many people who have benefited from LP, I am having to reconsider viewing that as a harmful use of NLP, though clearly it is dangerous for many. We seem very reluctant, in our culture, to code exercise itself as potentially dangerous, but it does seem to be, for people with ME. Yet the NLP approach, according to many who have commented on it elsewhere, seems to have been helpful to some – even turned their lives around.
I’d be really interested to continue this conversation!
Nancy, I believe your first paragraph says it all. To most patients that will be the defining statement. Most of us have never known the support of family, friends, spouses and medical staff. Most have never NOT experienced skepticism within their own homes.
I truly believe that if ME/CFS had the respect of other illness we would get the support we need from all the above and wellness and recovery would be word that was much more common to our vocabulary.
Stress is a killer when it comes to this illness. I can personally vouch for that. Just knowing one has emotional, physical, spiritual, financial and medical support…or even just two or three of these, would be an enormous contribution to wellness. How wonderful to not have to spend the energy defending one’s reason for needing help, rest, etc.,… and causing anxiety, anger resentment because of it. But in the world of this chronic illness, this is usually not the case.
I have contributed to a book being written by a friend regarding exactly this subject. The lack of support is so crucial to this illness and so widespread, being the rule rather than the exception, that it demanded she write a book about it.
I am so happy for you that you have received such wonderful support and thus wellness. I’m sure you understand and appreciate how blessed you are. I wish you continued good health!
Corinne
Hi Corinne,
Thanks for sharing your story and visit at Dr. Peterson. I do hope that you have recovered from the trip by now.
I am a bit curious about the ACE test (angio tensin converting enzyme). Do you know why this is tested? It is very common among people with ME to have a mutation in the ACE gene that probably causes a lowered enzyme activity.
Dr. Amy Yasko included genotyping of ACE in her first panel, but excluded it later as “all” with ME/CFS had the mutation.
Thanks for your opinion on this.
Helen
Yes, Helen, the ACE test, for me, was to help determine a diagnosis of sarcoidosis, as elevated ACE ( in serum and CSF) is often associated with sarcoid in conjunction with other confirming factors (lung nodules, etc.).