A Different Kind of Pain
That the immune system might play a major role in producing pain might seem obvious. Inflammation, swelling, and the symptoms of ‘sickness behavior’ including muscle and joint pains are all produced by the immune system when we catch a cold.
Even in Fibromyalgia – long thought to be a quintessential nervous system pain disorder – immune issues are popping up. The small fiber neuropathy found in that disorder could be caused by an autoimmune response, and recent studies have uncovered immune abnormalities involving cytokines.
Research into the immune and/or autoimmune causes of chronic pain has, however, lagged far, far behind research into the nervous system causes of pain. Recently, though, interest in this area has been picking up and with that interest will come new treatment options for one of the intractable of all symptoms -chronic pain.
Autoimmunity, Pain and Fibromyalgia and Chronic Fatigue Syndrome
The immune system has always been a focus in Chronic Fatigue Syndrome – another pain disorder – but the positive results from the Rituximab studies brought autoimmunity strongly into focus for the first time. With both FM and ME/CFS displaying many factors associated with autoimmune diseases including gender imbalance, increased rates of heritability, age of onset, environmental triggers, and sometimes infectious onset, we now turn to a recent webinar on the Pain Research Forum titled “Autoimmune Causes of Chronic Pain” by Dr. Andreas Goebel to learn how autoimmune processes may be causing pain.
By the end of the webinar not only will we understand how autoantibodies may cause pain, but also we’ll see that there are a variety of different ways they may be doing it.
The autoimmune contribution to pain is a new one – this is cutting edge stuff – but with researchers and clinicians finding that immune treatments can be very effective for some patients, it’s on pretty solid ground.
A recent workshop proposing that immunoglobulins be used to treat a variety of neuropathic pain disorders including diabetes mellitus, Sjögren’s syndrome, fibromyalgia, complex regional pain syndrome, and post-polio syndrome indicates that a major new approach to treating chronic pain is starting to open up, and that is welcome news.
With that, let’s look at how autoimmunity may be causing pain and what some doctors are doing about it. Andreas Goebel’s research is focused on the immune system’s contribution to chronic pain, mostly involving complex regional pain syndrome (CRPS).
Complex Regional Pain Syndrome
CRPS is a fascinating disorder that in its broad outlines may have some relevance for Fibromyalgia and Chronic Fatigue Syndrome. One of the most painful disorders known, people with long term CRPS typically score near the bottom of quality of life tests.
Like ME/CFS and FM, CRPS mostly strikes females in their middle to late years. Both FM and ME/CFS also often occur after an incident (injury/infection) that has outsize consequences and appears to involve some sort of ‘system reset’.
CRPS typically starts with a minor injury to a limb that evokes an immune response causing swelling and pain, which lasts long past the resolution of the initial injury. Both the swelling and the pain usually recede for 85% of CRPS patients over six months to a year, but about 15% of CRPS patients experience severe pain (without swelling) longer than that – and it’s this group we’re mostly interested in.
The Dubbo and other studies suggest a broadly similar pattern to the disorders. Most people with infectious onset Chronic Fatigue Syndrome do recover (or no longer meet the criteria) over the subsequent year or so, but a similar percentage (10-15%) have a long lasting illness. The autonomic and central nervous systems and the immune system are involved in all three disorders. All three disorders appear to be associated with increased gut permeability as well.
The big difference with CRPS is the localized nature of the illness: CRPS is usually confined to the section of the limb where the original injury occurred. At least some of the pain amplification processes in CRPS, however, involve the same nervous structures believed to be involved in FM and ME/CFS – namely the dorsal horn neurons that process pain signals just before they reach the spinal cord.
Autoimmune Causes of Pain in CRPS
In this very difficult to treat disease, Dr. Andreas Goebel was taken by the significant and often very quick pain relief he saw in about 25% of the CRPS patients put on low dose immunoglobulin (IVIG) therapy. (These same patients do not respond to intermediate doses of steroids (while another subset does).
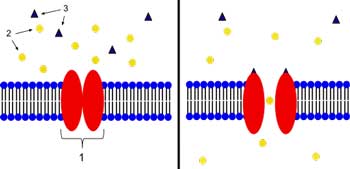
Why IVIG therapy would work at all in these patients isn’t clear. Their IgG levels aren’t low; they tend to be ‘low-normal’, but Goebel believes raising their IgG levels with IVIG may end up blocking autoantibody binding. (Could ME/CFS patients with low normal IgG levels respond to IVIG as well?)
A further study finding increased antibody (serum IgG) binding to sensory and parasympathetic nerves in a mouse model of CRPS suggested the immune system was indeed attacking these nerves.
Next, he looked for autoantibodies that activate autonomic receptors, and he found them. (Recently we saw a similar process involving different autonomic receptors in people with postural orthostatic tachycardia syndrome (POTS), and Dr. Newton is investigating whether the autonomic receptors on muscle cells are damaged in ME/CFS.)
Infection Sets the Stage
Injecting mice with IgG antibodies from CRPS patients and then introducing a mild injury resulted in increased sensitivity to pain in the form greatly increased levels of substance P, a neuropeptide found at high levels in patients with fibromyalgia and CRPS.
The fact that a CRPS-like condition only occurred when the mice were injured and given IgG antibodies from the CRPS patients suggested that an infection occurring shortly before the injury set the stage for CRPS by creating autoantibodies. These autoantibodies then attacked receptors in the nervous system to create the overreaction to the injury. Note that this second step probably only happens when an injury shortly follows an infection and the subsequent temporary production of autoantibodies.
That’s an intriguing model given the frequent instances of infectious onset associated with ME/CFS.
Immune System Fail Safe – Fails
The autoantibody response should get turned off over time, and longitudinal studies suggest that it does for most CRPS patients, but for those with long-term CRPS it remains elevated causing pain and distress.
(Again, this is an intriguing model for ME/CFS and FM, but longitudinal studies tracing the course of post-viral onset ME/CFS have yet to identify a factor that remains stubbornly high (or low) in people with persistent ME/CFS.)
The pain receptors may not be the target in CRPS. In a twist that brings to mind Van Elzakker’s vagus nerve infection hypothesis for ME/CFS, Goebel noted that the autoantibodies doing the damage in CRPS may be binding to immune cells surrounding the dorsal root ganglia causing the immune system to attack them.
Channelopathies and Pain
Goebel proposed that ion channels in the nerves may be the target. Targeting the nerves was an important step, because Goebel had to find an ‘invisible’ factor that causes pain. As the swelling and pain first evident in CRPS disappears, CRPS becomes an ‘invisible’ disorder in much the same way that ME/CFS and FM are. If an autoimmune process is occurring in CRPS it’s occurring without the physical evidence of damage we associate with many autoimmune disorders.
Goebel noted that autoantibodies can exert their effect by changing how cells function perhaps by producing a channelopathy.
(A channelopathy has been proposed several times in ME/CFS and some researchers believe herpesviruses may be causing functional changes in cells in ME/CFS without destroying the cell).
In fact, damage to the ion channels involved in the transmission of pain signals is suspected in other types of chronic pain. A recent Martinez-Lavin study suggests mutated sodium channels in the dorsal ganglia near the spine are causing severe pain in fibromyalgia. An Israeli researcher using scorpion venom to better understand ion channel functioning in chronic pain believes he may be able to produce safe and effective drugs to wipe out pain signals before they get to the brain.
- Check out our blog series on Dr. Martinez Lavin’s “Fibromyalgia – How Stress Turns to Pain” here.
- Taking the Sting out of Pain: Scorpion Venom Could Provide Alternative to Narcotic Pain Drugs
Treating Autoimmune Pain
Goebel proposed three immune treatments: plasma exchange, immunosuppressant drugs (Rituximab, cyclosporine, high-dose steroids), and immunoglobulins. Noting that some of these treatments can have significant side effects, he stated medical practitioners should be begin considering whether using strong drugs and the risk they pose is acceptable in illnesses that essentially wreck a person’s quality of life but don’t kill. (Apparently, the answer is “generally not” at his point.) “What do patients want?” he asked, and then noted that his talk with patients indicated they wanted options.
A Mayo clinic study concluded that immunotherapy was more effective against chronic pain in patients with potassium channel antibodies than typical nerve pain drugs such as Gabapentin. Goebel is clearly pushing for more research into autoimmune causes of chronic pain as well as the use of immune drugs.
The Webinar Question Period
Post Trauma Autoimmune Disorders
The question period revealed that a variety of autoimmune responses that result in extreme pain have been identified.
Trauma Induced Peripheral Neuropathy – shortly after a trauma (in the form of surgery), Dr. Nathan Staff noted that some patients at the Mayo Clinic developed pain, weakness, and peripheral neuropathy. Often the neuropathies occurred in the same limb as their surgery. At first they thought nerve damage or some other sort of mechanical injury had occurred during the surgery, but further investigations revealed that an autoimmune response had occurred.
Here again we have a sudden onset associated with some sort of acute stressor that triggers an autoimmune response. Goebel almost jokingly suggested that they form a group of new post-traumatic disorders, and proposed that once they started looking for these processes they’re going to find a lot more. That’s not hard to believe. With few effective drugs available for chronic pain, it’s clear that researchers are still missing big chunks of the picture.
Neurologists Miss Potassium Channel Autoimmunity – Dr. Vincent noted the potassium channel complex antibodies have been associated with other types of chronic pain, but not with CRPS. Patients with those antibodies tend to have sometimes severe neuropathic pain, but they’re different from CRPS patients in that they don’t experience swelling of the tissues. That lack of visible trauma, similar to what occurs in FM and ME/CFS, often means they’re not attended to by neurologists.
Pain Occurring out the Blue – Mayo researchers also find that patients reporting pain that is not associated with injury, but which appears to occur for no discernible reason, is usually antibody-induced pain.
A Heterogeneous Pain Population
We can see from this short discussion how heterogeneous autoimmune induced pain is. Researchers have identified
- An immune or autoimmune response causing swelling and pain at the site of a minor injury in CRPS.
- An autoimmune response occurring in the same limb (but not at the site of the injury) after surgery.
- An autoimmune response associated with potassium complex autoantibodies that produces no visible signs but that is associated with severe neuropathic pain.
- An autoimmune response that occurs out of the blue which causes severe pain.
Dr. Staff noted the need to do in-depth analyses of pain disorders (including serum, genetic analyses, and fMRI) because of the high heterogeneity seen. As in ME/CFS, many pathways appear to be able to produce the same final result – severe pain.
Pain Plus
Goebel is finding that some of these central issues (disability, depression) resolve before pain relief occurs when treating CRPS patients with plasma exchange. First they feel calmer even though their pain is still present, and then their pain starts to resolve.
That suggests immune factors in the plasma exchange are causing changes in the central nervous system. Dr. Vincent noted that antibody-mediated central nervous system disorders can cause memory loss, seizures, and movement disorders, and she suggested that it’s the peripheral immune system at work in the brain – as has been suggested by Van Elzakker and others in ME/CFS.
Antibody Panels to Test for Autoimmune Sources of Pain in Five Years

One panelist believed tests to determine if you have antibody associated pain will be available in five years
Dr. Vincent believes that, in the next five years or so, antibody panels will be available to test for immune/antibody-associated pain. Dr. Staff suggested researchers and clinicians should begin testing antibodies across a wide variety of pain conditions.
Autoimmunity and Fibromyalgia
Some doctors refer to fibromyalgia as being the ‘quintessential idiopathic pain syndrome’. Infections and trauma can each trigger FM, and FM mostly affects women, but swelling and signs of overt damage are rare. Goebel noted that abnormal nerve activation patterns and the small fiber neuropathy found in FM could be due to an autoimmune response.
Conclusion
The recognition that autoimmunity processes may cause chronic pain disorders is growing. It’s not uncommon in these cases for an infection or injury to prompt an autoimmune response that is often invisible (does not cause swelling, etc.). Ion channel damage may be involved. One panelist believes antibody panels for chronic pain will be available within five years.










Thanks for the write-up, Cort. Sounds like promising stuff. All that much more of a shame that the CAA’s comprehensive ME/CFS antibody research study from a few years ago didn’t get funded. Also, I didn’t see a link to the actual webinar anywhere in the article?
Indeed – that study is looking like a better and better idea all the time. Here’s the link to the webinar – http://www.painresearchforum.org/forums/webinar/41344-webinar-autoimmune-causes-chronic-pain
Extraordinary writing on a complex and difficult to understand subject. I can only imagine how much time it took to listen to the webinar and then assimilate all these details and into a understandable blog. Once again, I punched your donate button. Thanks.
The pain in CRPS is commonly localized in only one limb, why would these autoantibodies cause pain in a specific limb rather than a more general or multi site pain?
Maybe I can help?
I watched this webinar some time ago but took some notes and if memory serves correctly he gave allopecia as an example of ‘local autoimmunity’. So it may sound counterintuitive but it is possible.
As far as I’m aware, CRPS can also result in widespread pain (and other symptoms) away from the initially affected limb although its not clear if this is also due to autoimmunity or to other secondary mechanisms.
Yes, he did reference allopecia. Didn’t know widespread pain is present in CRPS…but it makes sense given that he did say the central sensitization present in CRPS is similar to that found in other chronic pain disorders. However, low back pain is pretty localized – whether the pain is localized in CRPS or not, it appears that CS can result in widespread sensitivity to pain or localized sensitization to pain.
If Alopecia Areata can be successfully treated by Ruxolitinib as this report suggest http://www.bbc.co.uk/news/health-28834058 then what does that tell you about the nature of the disease ?
It seems to me that there is an informative chimeric parallel between the use of Rituximab in M.E. and Ruxolitinib in Alopcia Areata.
More info on using Ruxolitinib to treat Alopecia Areata here: http://www.nature.com/nm/journal/vaop/ncurrent/full/nm.3645.html
Once again, thanks Tim….I think the potential overlap between ME/CFS and FM with the infection triggered autoantibodies is fascinating. If the autoantibodies attack and deform the sodium channels on the dorsal root ganglia I have no idea why the pain would stay so localized – good question!
Two treatments he suggests, plasma exchange or immunosuppressive drugs like corticosteroids or Rituxan, are the same ones used for Autoimmune Autonomic Ganglionopathy–one specific, recognized type of autoimmune attack on the nerve ganglions of the autonomic nervous system.
Low-dose IVIG sounds great–to also stop the autoimmune attack on the nerves, when the patient has low IgG. I think a patient would have to test as abnormally low on IgG in order for a somewhat dangerous treatment to be rationalized. Maybe the expense of it would incline insurance providers to nix it and the necessary research too.
But I think this is a great direction for research and treatment. Thank you, Cort, for writing such a thorough article!
RE IVIG immunoglobulins as a treatment option for ME/CFS. This already has been tried with the most unusual outcome of 100% recovery in some very Severe ME cases. See Dr Nigel Speight on the recent you tube video “exercise and ME/CFS” here if you haven’t already to check it out:
https://www.youtube.com/results?search_query=exercise+and+ME%2FCFS
Thanks for an interesting article.
Tim
As John above says, no link to this specific Webinar session. I may already have booked it as I booked a couple a few days ago when the various sessions formed part of your blog.
I firmly believe the key to fibro/ME/CFS will eventually be shown to be in the immune/endochrine area of our bodies functions.
BTW, apart from the system hardware requirements shown on the original webinair piece, is there a specific Webinar software?
Keep on keepin’ on Cort.
Christine – with gratitude.
I thought I put it in but I guess I didn’t. Here’s the link https://www.facebook.com/pages/ME-CFS-Research-Newcastle/526359017390431
I don’t know of any specific webinar software. I would have embedded it but it looked like they don’t want me to do that.
Hi Cory,
I am so happy to have found this information. I have ANS dysfunction . With that comes CFS and low blood pressure, to name a couple of problems. I live in Canada, but it took the Mayo Clinic in the USA to diagnose me. My Neurologist at the time tried the IVIG treatments on me. I had 3 out of 4. My body could not tolerate them. I also felt no relief from chronic pain.
I also see in the blog that some people don’t get Neurologists to treat them. I was discharged as a patient from the Neurologist after the IVIG didn’t work. Right now I am on Naproxen and Gabapentin. They help a bit but not the best. Like others I have no quality of life. I look forward to the next 5 years to see how research and clinical treatments are going. I am willing to be tested on when the time comes for needing patients. I must tell you though that I had to have a pacemaker put in due to low heart beat. Therefore I can’t have MRIs. This could be a drawback for a potential clinical patient.
Thank you
Thanks for another very important article that is understandable and informative. Too often we read about these diseases and can’t seem to get what they are trying to say. You (Cort) help make things easier to understand. I am learning more from your blog than I have in the 24 years since the onset of CFS/Fibromyalgia. Thank you so much for all you do for our community. Sincerely!!!
Thanks Patty – that’s very nice of you to say. I am certainly learning a lot 🙂
It makes sense to me, as I consistently feel worse during flu season in the fall and allergy season during the spring.
Cort, I would be interested in being in clinical studies in the next five years as I was “officially” diagnosed w/Fibromyalgia 9 yrs. ago. Thank you for the article! 🙂