

(Corinne continues her blogs of her visits with Dr. Peterson and other doctors)
Corinne’s Visits – October and December 2013
“We have to learn to let go of the life we had in order to enjoy the life we’ve been given.” – Joseph Campbell
To summarize my last blog dated September 2013 – I had returned to Dr. Peterson to have my third lumbar puncture hoping to find answers as to what was causing the cervical spinal cord lesion found on an MRI in February 2013. Test after test, including the lumbar puncture, had not revealed any answers so I was left with the more invasive biopsy of the lymph nodes in my chest (mediastinoscopy) as the next option on the list.

Corinne’s spinal cord lesion has neurologists jumping from one diagnosis to another and suggesting a possible surgical procedure
Ever since those very small nodes had showed up “mildly hypermetabolic” in a PET scan, this is what the neurologist Dr. G at UCSF had wanted to focus on. His suspicion was neuro-sarcoidosis even though I would be highly atypical as a sarcoid patient. When I found out that the nodes were so small that they could not be biopsied the easy way (down the throat), but would, instead, involve a small surgical procedure requiring general anesthesia and an overnight stay in the hospital, I was hesitant. At the least, I requested the possibility of doing it near home. Dr. P. and Dr. G. agreed.
So that is where the Mayo Clinic comes into this complicated picture – 23 years after I had visited them the first time, when I became ill and they sent me home saying nothing was wrong except perhaps depression. I had come full circle.
October 2013 – the Mayo Clinic, Arizona
Twenty three years ago, I had left there in frustration saying “never again”
Seriously?
I had made an appointment with a thoracic surgeon at Mayo in order to consult with him about the mediastinoscopy so I could make a more informed decision on whether to proceed. Twenty three years ago, I had left there in frustration saying “never again”, but here I was on my way south hoping that this time, with a glaring lesion on my spinal cord, I would get the respect I felt was lacking the first time.
The Mayo Hospital, where the surgeon’s office is, is about two hours from my home. My husband, Joe, who isn’t a fan of accompanying me to doctor appointments, agrees to drive me. Since he would be the one assisting me should I do the procedure, I felt it was important that he be here.
As we wait in the exam room, I still feel funny being here. I have a bad taste in my mouth, even after 23 years. But perhaps, I hope, changing times have changed minds.
After introductions, Dr. O.P. sits down, gives me a questioning look, and says the one word that needs no explanation – “Seriously?” He tells me this is what he asked himself after reading the order, PET report and records – “Seriously? You are considering having this procedure done for nothing but a few tiny, slightly hypermetabolic lymph nodes that could be anything? I can’t even tell if they are actually lit-up or if it’s due to background noise.”
He proceeds to explain that he does mediastinoscopies all the time and has never had a problem – but they are not risk-free. Dropping a scope down your chest past your aorta and airway is never risk-free and to do it for lymph nodes that may be too small to find is hardly warranted, in his opinion.
He adds that he does a lot of lung transplants on sarcoid patients and all have huge lymph nodes, nodules on the lungs and most are African-American males. In other words, in his estimation, the chances of me having it are slim.
I ask him to pull up the image of my C-spine on his computer and explain that my doctors feel that at this point those lymph nodes are the only abnormality that can be biopsied that may hold the answer to the mystery of what is causing the lesion. “They call that a lesion?” he mutters. He does not seem impressed. He does go on to say that if one of the Mayo neurologists insists it needs to be done, he’ll do it, but I would need to see their in-house doctor.
I am in shock – like a time capsule that just went back 23 years. In one way I am sort of glad the biopsy is not recommended and he considers it too small a payback for the risk, as I never wanted to do it anyway. But on the other hand, I have to blurt out “I cannot come back again to see a neurologist. I’m too sick!”
Thankfully, he accomodates me and finds me an appointment with a neurologist today, a cancellation, in 20 minutes! And it’s at the other campus, 25 minutes away! Dr. O.P. is yelling directions as we rush out the door, down the hall and to the car. We speed along the highway as fast as possible. Joe drops me off at the front entrance as he finds a parking spot. I grab a volunteer and wheelchair and make it up to the third floor still out of breath. As I check in, I explain the situation, not remembering the name of the doctor I am to see as it was only mentioned once, in haste. The receptionist looks at me funny. That should have been a clue.
After a few minutes a woman emerges from one of the offices, asks me a couple of questions, then begins to apologize profusely. Dr. O.P. had sent me to the wrong place! The neurologist I was supposed to see was back at the building I had just come from. It’s too late. I’ve missed the appointment.
I want to cry. She feels bad but I assure her it’s not her fault. She asks me to wait for another cancellation but I am adamant – I will not. I am exhausted. I do have to eat however, so I tell her if something opens she can call me while my husband and I have lunch. She said she will go out of her way to call each and every patient that has an appointment with a neurologist (they have at least 30 of them) that day and find out who is planning not to come. I thank her.
My head is in my hands when Joe finally finds me. I am embarrassed to have to explain the situation to him. The debacles associates with my ME/CFS and the medical community over the years are part of the reason why he has separated himself from my illness experience. And so far today, this circus act would only seem to add credence to his decision.
Neurologist #3
Joe and I are having lunch when the phone rings. They have an opening for me back at the Phoenix campus where I started in the morning. Within the hour, I am in the office of a resident neurologist, Dr. D. She appears young enough to be my daughter.

Which way Corinne? Corinne is at a familiar place for many with ME/CFS. She doesn’t fit the normal pattern and her neurologists are in disagreement
Not long after we begin, I can tell she is plenty intelligent, full of energy, with an attitude that I interpret as “I am going to cure the world!” In other words, her enthusiasm has yet to be dampened by cases like mine. My 23 years with this illness has prepared me for moments like this. I will be spending a lot of the conversation reining her exuberance in. Bringing her back down to earth, you might say.
This is the third neurologist I have seen since February. The first diagnosed me with neuromyelitis optica (NMO) and sent me home without a referral nor follow-up. It was accidentally that I had read his report and found out I was “lucky to have avoided, so far, the blindness and paraplegia that usually accompanies it.” Whoa! Why didn’t he tell me that?
The second neurologist, Dr. G. at UCSF who Dr. P. referred me to, was the reason I was here. He was leaning towards neurosarcoidosis (tests seemed to rule out NMO) and he wanted the thoracic lymph node biopsy done to possibly prove it.
Each had performed complete and thorough work-ups and yet here I was again, doing a third. No matter how many notes and reports available for Dr. D. to read, she smiles and says, “Let’s start from the beginning.” Grrrrr…… Its 2:00 p.m., I’ve been here since 8:00 a.m., this is the last thing I want to do (sigh, deep breath). My brain is fried and it is exhausting having to repeat my family history and my 23 years with this illness…
Throughout the appointment, I only mention CFS once, explaining that I am not fond of the term. She, like Dr. G. at UCSF, does not appear familiar with what ME stands for. In fact, she never refers to it, or CFS, or neuro-immune the entire time.
Several times she suggests tests and several times I tell her that once she looks at my medical packet (she hasn’t had time to do so as I am a last minute fill-in), she will see that I have done every test conceivable, including some she has never heard of. When she leaves the room to consult with her supervising neurologist and they return together, she admits that I have undergone plenty of tests.
Under her supervisor’s watchful eye, she tells me that because my immune system is showing so many antibodies to so many things she would like me to come back to see the in-house rheumatologist!
I consider myself to be a nice person, but I am not cooperating at this point. I flat out refuse to return to see any more doctors. I tell them both that I am too sick and have already been to three states to see doctors about this lesion.

Things have changed. Her young doctor believes she had an autoimmune response to a pathogen 23 years ago – not depression …..
I am assuming they are thinking in terms of auto-immunity (AI), but two hours into this discussion, I fail to hear anyone putting together the whole ME/CFS picture – so I start asking them questions. “What do you think about my elevated cytokine panel?” They look at each other and the supervisor responds “Well, we don’t know much about that.” “What about my high viral load?” Dr. D. suggests that I have no viruses – “you have no positive PCR. It appears you are only making antibodies to antibodies (autoantibodies).”
Having told Dr. D. my experience at the Mayo Clinic 23 years ago, she perhaps senses that I have a chip on my shoulder. She tells me that she would not have sent me home without a diagnosis back then, if she had known what they know today. She believes that 23 years ago, I contracted a viral infection that resulted in (science doesn’t know yet exactly how) an AI attack on my autonomic nervous system which resulted in POTS. She then follows that up with a request for a tilt table test, suggesting that treatment could really improve my quality of life.
I’m impressed that she has this much insight into my condition but pardon me if I am a bit edgy – “I am not doing a tilt table test. At this point, I feel like I have tortured myself enough this past year. I already know I have POTS. Dr. P. diagnosed me years ago. But POTS is not the reason for the spinal cord lesion. I am here for the lesion. That is my priority right now.”
This isn’t the only time I feel I must redirect her focus. It feels almost as if the lesion is just too complicated (not just for her, but for everyone!) and she’d rather deal with what she’s more familiar with.
After a while we come to an agreement. She understands that the lesion is the focus for now. She says the mediastinoscopy may not be out of the question but instead of me having to come back for an appointment, she will consult with the in-house rheumatologists and neurologists for me. She also agrees that I do not need any more tests except for a few minor labs that will be redone, just to make sure that nothing simple was accidently missed – such as B12, copper, zinc, vit E, folate, etc. She says she will call me in a week with a plan. I am most grateful and express my sincere appreciation.
Blood is drawn downstairs and then I wobble and weave out to the parking lot where Joe meets me in the car. It’s 4:30 p.m., just another eight-hour day at the doctors plus a two hour drive home. And I thought visits to Dr. P. were rough!
December 13 – Back to Mayo
It’s actually three weeks before Dr. D. calls me with her plan. The labs drawn came back normal except for the usual slightly elevated ANA (1.5) and elevated Sjogren’s antibodies. She says she has decided the mediastinoscopy is not necessary at this point – she doesn’t want to have to put me through that, considering everything I have already endured vs. the chance of it revealing anything substantial.
Her plan does, however, involve two more procedures. She would like me to have a lip biopsy to rule out Sjogren’s and a conjunctival biopsy for a possible sarcoid confirmation.

The problem is that Corinne doesn’t fit any boxes except one – ME/CFS ( the disorder that doesn’t fit into any boxes) – which leaves Mayo doctor’s floundering (and trying to fit her into something they understand.)
The past year has been financially and physically taxing for me. I am trying now to be logical and efficient when making medical choices regarding this mysterious lesion. And, of course, I am weighing the pros and cons of whether a procedure will actually result in something productive towards my healing. Thus, I argue with Dr. D. about the need for the lip biopsy.
Dr. G. at UCSF clearly stated to me that Sjogren’s place in causing myelitis is highly debated and contested in the literature and, in his opinion, while a Sjogren’s diagnosis may help explain some of my other 23-year old symptoms, it would have no effect on leading us to a more targeted treatment – or really give us any insight at all – into the mystery of the spinal cord. So, in my opinion, it is a waste of time and money.
In contrast, the conjunctival (the conjunctiva is the lining that covers the eye) makes a bit more sense, as Dr. G said that studies have shown that sometimes sarcoid can be found there. Though rare, it’s a shot since it is relatively non-invasive and a sarcoid diagnosis would tell us a lot more about the mystery myelitis.
Dr. D. disagrees. She insists the lip is the priority, and I have no idea why. Her explanation is very vague as she uses something I had said to her earlier to persuade me. During our appointment, I had told her to be prepared – that I would not fit into any of the “labeled boxes” they would try to fit me in. That no matter how hard they tried to squeeze me in, I would not quite fit. I would be “atypical this” or “nonclinical that,” but never fitting the description nice and neatly (except of course the ME/CFS box which they do not possess). So to get me to do the lip biopsy, she says “You, yourself said that you would not fix into any box – so why not Sjogren’s?”
Boy, if I hadn’t already thought that nobody had a clue as to what is going on with me, I sure do now. Really? So that’s the best you can do? Well, how about ME/CFS being the explanation, I wanted to say!
Too drained to argue, I agree to do them both, but only if they can be scheduled on the same day. And, of course, the only day available just happens to be December 26. Hey, what else would I want to do the day after Christmas, anyway? What a life! J
Merry Christmas – Tissue Needed (and not the kind you wrap gifts with)
Yesterday, Christmas was spent driving down to a Phoenix hotel to spend the night for today’s procedures. The lip biopsy is scheduled first and is done in the Ear, Nose and Throat (ENT) Department. The doctor, Dr. C., is very accommodating. There is a mix-up in the coordination of how to prepare the tissue samples to be sent to Gunnar, Dr. P.’s research coordinator, who will then send them on to Dr. Lipkin at Columbia University. As I get the last minute orders from Gunnar by cell phone, Dr. C. kindly waits.
The fishing expedition is unsuccessful: this biopsy indicating Sjogren’s Syndrome is present is what they did not find
The prep and surgery take 15 minutes. Five salivary glands are removed from the left side of the lower lip for Gunnar and five for Mayo, for a total of ten. Dr. C. does comment that they are just “fishing” regarding this procedure and any answers it may provide regarding the myelitis. Unfortunately, that is not the last time I will hear this.
Putting in a few stitches, he warns me that it will be sore when the anesthetic wears off. I am also told that nerves have most probably been cut and I may feel numbness on that side of my lip for a long time.
Then I move on to the Ophthalmology Department for the conjunctival sample, using a wheelchair and volunteer. About the time we arrive, my lip starts to hurt until it becomes almost unbearable. The only thing I can think of that might help is ice, so I ask the volunteer if he can get me some from the cafeteria. I suck on a cupful until the pain subsides a bit. I am surprised at the amount of pain, but considering the lip area is so sensitive and filled with nerve endings, I suppose it’s no surprise.
The ophthalmologist is congenial and efficient. He looks inside both lower eye lids (that is where the sample is taken) to see if perhaps something abnormal would suggest taking the biopsy from one rather than the other, thus increasing the odds of finding something. But he finds nothing – both look perfectly healthy. Then he too mentions the word “fishing.” The tone in his voice suggests this is just a crap shoot and that the odds of finding something are very low. But he does say that I am doing the right thing by trying all of the least-invasive procedures, as I can possibly “get lucky” without having to do more.
None of this is news to me but it’s still disheartening to hear both physicians say it. I have been chasing answers to this spinal cord mystery for almost a year now and had already made up my mind that these were going to be the final two procedures I would undertake, other than the scans I must do every few months to monitor the lesion. I feel satisfied that I have given it my all.
A couple of snips and the surgery is over. I ask if this will hurt as much as the lip does and he says it will. Yikes! He hands me an antibiotic ointment to apply daily and then, I’m on my way.
On the drive home, Joe comments on the swelling that has begun on my face. Luckily, I do not have anywhere near the pain in my eye as I do in my lip. I must continue to suck on ice in order to bear it.
I have trouble sleeping that night as my lip throbs. The next morning I awake to Rocky Balboa staring back at me in the mirror – “Yo Adrienne!” My right eye is swollen shut and my lower lip looks like I had a bad silicone job. Both are primarily black and blue, but include every color of the rainbow. What a sight! J
Conclusion
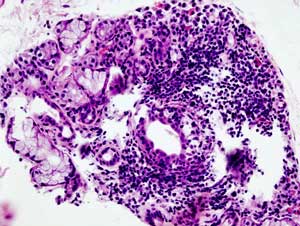
Despite always having elevated Sjogren’s antibodies on my labs, my pathology report is negative for Sjogren’s. “Non-specific inflammation” is all that is reported. Likewise the conjunctival biopsy is negative for sarcoid – “subepethelia chronic inflammation” – states that report. Ha! Years ago I had a biopsy done on the inside of my stomach and it showed “chronic inflammation of non-specific nature.” Add in my spinal cord and I’m just a walking chronic inflammation.J Personally, I feel the mediastinoscopy would have showed the same. So though we may know more about what I don’t have, we don’t know more about what may be the cause of the myelitis.
My follow-up phone conversation with resident neurologist Dr. D. at Mayo was a bit frustrating. Regarding the lesion and the possibility of treating it with immuno- suppressors such as steroids, which is the standard of treatment for auto-immune induced myelitis, she would not touch me with a ten-foot pole.
When I questioned as to whether it is acceptable to do nothing, referring to scarring, she said that spinal cords “do not scar, per se” – a statement that Dr. G. at UCSF vehemently rebuked. She said that these type of lesions do one of three things: go away, stay the same or get worse (duh?).

Some things have changed at Mayo and some things have not. In the end it comes down to an exercise prescription – something that Corinne -a former athletic trainer – knows will not work
If monitoring shows it is getting worse, then she would consider treating. When I told her my symptoms have gotten worse over time (the same areas-back, arms, hands, buttocks, legs and feet have progressed in numbness, constriction and pain), she said that unless I had new symptoms – new areas affected – it was not considered “getting worse.” This too was a statement that Dr. G., to put it kindly, totally disagreed with.
When asked if going back on IVIG would help, (she had suggested before that it may have been “too little too late” when I was on it when the lesion was discovered), Dr.D said it was the only thing she would consider, if and only if I came down to do a baseline tilt table test first and a complete POTS autonomic reflex panel.
What? I have a serious myelitis that could possibly benefit from IVIG and you would withhold it unless I make another trip down and do a series of tests for POTS which is completely separate from the spinal cord issue? I felt as though she were dangling the proverbial carrot in front of me, baiting me, “I’ll do this for you, if you do this for me.” Her reasoning centered around the fact that the IVIG might affect the POTS and so affect the baseline data. But at this point, I just wanted help for my lesion. I was not concerned about POTS data!
I may have been persuaded had the “E” word not followed. When I tried to pick her brain about POTS treatments she might have in mind, I mentioned knowing about drugs like Florinef, Vasopressin, Midodrine and drugs I was taking for volume like Epoetin Alfa with IV saline, but was there really anything new? Her answer – “Yes, there are new drugs (pause) but the main component of the protocol would be exercise!
Well, that was it. She had totally lost me and any interest I may have had. I blurted out “But I told you I cannot exercise.” She casually remarked “not even on a recumbent bike?” (In other words, come on, who can’t do that?).
I was appalled. In a not too friendly voice I did the best I could over the phone to bring her back to reality. I told her that although she may not understand my ME/CFS exercise intolerance, how can she ignore the fact that I have an inflammatory lesion on my spinal cord that affects everything below it? My legs do not feel nor do they work properly! (At this time, because of the lesion, I was getting constriction and cramping in my feet and calves when I walked more than a few feet…besides the persistent numbness and hypersensitivity throughout my back arms and legs.) How can I exercise?
I do not even remember if she answered. I had emotionally disconnected by that time. I knew Mayo was not the direction I wanted to go. My exercise intolerance is not based on deconditioning. How could it be when it began the day I got ill, and I was as fit as they come? Mayo did not get it and they were not going to address the lesion so it was time to move on.
I must also add that I did not like the fact that though I had been adamant that they send reports and include the doctor who knows me best and referred me here, Dr. Peterson, and the neurologist at UCSF, Dr.G, in their consultations they, despite having been given all contacts, did not fax, email, phone or snail mail either doctor.
So, one year since the discovery of the lesion, I still have no answers. My lip has a big knot where the biopsy incision was made and remains numb on the left side, and when I have a pain flare, it, and the eye, are one of the first things to ache. I do not regret, however, pursing the possibility of “getting lucky.”
The next stop in my journey is to return to Dr. Peterson’s in March 2014 for a consult with him and, jointly by phone, with Dr.G. at UCSF regarding what to do next. Meanwhile, my three month MRI shows a stable lesion but my symptoms gradually worsen with each flare.
As far as my meds go, as of March 2014 (pre-Dr. P. visit), I continue with my IV saline (two liters twice a week) with the Epoetin Alfa injections (twice a month) for blood volume. I remain on Klonopin (.5 mg) for sleep and Valtrex (500mg twice a day) for some herpes virus control. I continue meclizine as needed for dizziness.
By suggestion of my local physician (who has been an absolute angel whenever I need help implementing Dr. P.’s protocol at home), I started gabapentin (200 mg twice a day, but am titrating up) for my nerve pain, and topiramate – a migraine medication – (25 mg once a day) for my headaches. As of this writing it was too early to tell for the gabapentin, but the topiramate seemed to be helping with my head and my ability to use the computer. J
Next stop Dr.P’s, March 2014…with my good friend Cort and his two canine buddies River and Sky as my ‘drivers’ :)…
‘Til then…feel good!
- Check out more of Corinne’s blogs here








Well, the take home message is to have the biopsy done where the “diagnosis” is made. I’ve been amazed at the efficiency and timeliness of UCSF. When they say you’ll be discharged at 10:15, it’s usually 10:10! When you enter another DR/Institution you just open yourself up for more BS.
Greg
i actually loved UCSF and Dr G , but the traveling back to San Fran was not an option. And the treatment option of steroids or other immunosuppressors, which UCSF wanted to treat me with could have created havoc in an immunosuppressed patient with ME like me.
What awful bloody people. The Mayo is a great example of how if nothing changes, nothing changes. Could not help but feel protective anger on your behalf. Thank you for continuing to share your journey. Your courage inspires me x
I went to Mayo in Rochester in 1993. I had not been diagnosed with CFS yet, and was gravely ill, and my docs in Ohio we worried I would not survive whatever it was I had. My GI guy, who had done his residency at Mayo, sent me there. The coordinating doc at Mayo listened to my history and immediately decided there was nothing wrong with me, but put me through a week of tests anyway. The only diagnosis I got from anyone was the rheumatologist who told me I had “a little bit of Fibromyalgia, maybe.” When I got home, I got to the Cleveland Clinic, and, armed with a FMS diagnosis, got to a rheumatologist who diagnosed me with severe CFS and moderate FMS. Was definitely not impressed with Mayo!
I am wondering whether Corinne might try (or if anyone has tried) the NIH undiagnosed disease program, for people who have been trying for years to get a diagnosis, unsuccessfully. They take a very small number of people who apply, but it might be worth applying? Here’s the link. http://www.rarediseases.info.nih.gov/research/pages/27/undiagnosed-diseases-program
I have always found that the most important trait in a doctor to treat me is one who likes mysteries. I often ask the docs who I trust to recommend me not to someone in another specialty who is an expert in one thing, but to someone who is like them. I have built up a team of people who are comfortable with the fact that I am, as they all are happy to say, “weird”, physically. They like the challenge. I ask doctors whom I like which other doctors they have a beer with, then ask them to send me to them. Haven’t had much luck with going to docs who are “experts”.
Corrine- I too applaud you and agree with Tamesin.
I am not immobile but having severe Gut issues at the moment.
Same story no one will listen. I agree with finding someone that likes mystery.
That thinks outside the box.
Please continue to let us know of your journey and stay strong.
Carole
luckily i already have that doc who loves mysteries…Dr. Peterson. In my last blog you would read that he even said…”I love a challenge…i will stick with you til we figure this out”.
Corinne,
I am touched by your strength + courage.
Good for you for sticking up for yourself despite such obstacles
(i.e. the Mayo Doctors + your declining health)
As a fellow sufferer, I wish you strength + a definite diagnosis!
Corinne,
Such a chilling heartbreak to read of your return to Mayo Clinic. I went there (Rochester) in utter despair and agony in 1990 and was told, following a week of tests and clinics and doctors, that “…you MIGHT be allergic to beef and tomatoes..” The doc said to go home to Oregon, wear a little white fabric mask outdoors, and see what happened over the next 6 months. Twenty-four years and some $250,000+++ out-of-pocket medical expenses (“not medically necessary”, “not conventional medical treatment”, I still stick my neck out from time to time and ask for something new. Nothing comes of it, but I always keep hoping. We all know well how complex it is, but hard to understand that we really get just about nothing as patients and people out of the medical community. I well understand your disappointment, deflation, and surprise (that little of anything comes of all the talking on and on of all your symptoms, everything that has gone wrong, reiterating the history over and over again. I hate going to new doctors and even opening my mouth and hearing my own story again. Keep taking those long deep breaths that give us the determination to keep on and to try again. My husband has gone with me on all these medical journeys (he worked in a medical school for years) and has been stunned by the inability to think outside the box, to follow clues, to simply want to solve the problem.
My heart goes out to everyone out there with this illness. Be bold everyone, and keep pushing on them. I think it will take an “army” not just a village of ME patients to win.
Connie, reading you returned home to Oregon, I wonder if you would be willing to correspond with me about doctor experiences in Oregon. I have ME/CFS, FM, POTS, +. I live on the Coast. My email is srgreenough@gmail.com. I am looking for support groups/people in OR.
Corinne, I too went to the Mayo Clinic ( one on the way to Fountain Hills) about 25 years ago thinking they’d know how to help with my FM, but they knew nothing. I’m so sorry for all you’ve been through. I recently had 6 doctors look at my EKG and either not know what was going on or said it wasn’t concerning. A nurse practitioner had the sense to monitor me and I’ve since had an ablation. It gets frustrating. I sure hope you’re doing better by now- you’ve been through so much and have handled it with such courage.
i thank you sincerely for your kind words and encouragement
i hope you are doing better. My experience with Mayo, and the other medical doctors, has actually been helpful in assisting me in realizing that i did my best searching and really the truth is, only Dr peterson gets it and now i can go back to him with the confidence that i am in the best of hands. Dr peterson did what he had to do, in getting second and third opinions, hoping that he could get someone to put the whole ME/CFS picture and my myelitis issue together. When it doesn’t happen, it is as heart breaking to him as it is to me.
I went to the Mayo Clinic after 18 months of CFS hoping they would do something (this was in 2009). I had a similar experience. No knowledge of CFS and the Dr. who was my intake doctor actually suggested anti-depressants before we even finished our meeting. They sent me through a long list of tests, one an EMG which was extremely painful. Of course they did their own tilt table test, which as most of you know makes you miserable and feel sick for days. Their final diagnoses after 7 days – I had low blood pressure and I need to meet with a physical therapist to get on a work-out regimen. Same “recumbent” bike comment. Anyone out there with CFS, please DO NOT waste your time, energy and money. Go a ME/CFS Specialist. PLEASE don’t waste your time at Mayo. And lastly, Mayo Clinic, please stop sending me mail every month for “donations.” You have GOT to be kidding me.
What an amazingly similar story! Which clinic did you go to? (I wonder if it matters?)
YES!!!!! YES!!!!!! THE DONATION THING! WHAT IS THAT ABOUT?? SERIOUSLY???
YES!!!!!! THE DONATION THING! WHAT IS THAT ABOUT??
SERIOUSLY? 🙂
We’ve corresponded before – and it really breaks my heart that they have done such painful and invasive things to you just one the off-chance, and ‘because they can’. I believe strongly that when medical help doesn’t seem to be available (as in something that is based on understanding the pathology and addresses it effectively) our only recourse needs to be to treat our body kindly enough to allow its natural healing processes to operate. That means as good a diet as possible, and, in the case of ME, absolutely conserving muscular exertion. We always get back to the fact that muscular exertion (and cognitive effort, and emotional stress, but mainly just using our muscles) causes all our symptoms to get worse. I do believe that putting oneself through so much travel, effort, stress, and diagnostic procedures that challenge our body’s resources – can get in the way of our body’s ability to direct its energy to sorting out the complex mess that ME is. I know that advice like ‘try going to bed for three months’ sounds like advice to give up, but to me it is ‘give your body a chance’. I know the lesion thing is very frightening – but after all you’ve done to get it understood and treated, how much help have you actually had? (And the appalling suggestion that you have treatment of which exercise is the main component is pretty much a giveaway that behind the scenes, they belong to the ‘medically unexplained’, ‘somatoform’, CBT and GET school of thought. Especially as they don’t recognise ME/CFS as a diagnosis. Someone has definitely got at Dr. D., and it would be interesting to confront her with that. Also they have shown immense disrespect for your good doctors, and for you.) The other thing I have a lot of respect for is Les Simpsons research on blood flow problems in ME/CFS, and I know that many patients, from years back, have benefitted from trying out his suggestions for improving blood flow – 6 g of fish oil per day, or 4 g of genuine EPO, or B12 as hydroxocobalamin (injected, so I haven’t done it), or pentoxyfilline. It stands to reason that if the red blood cells can be helped to perform their basic functions of providing oxygen and removing waste products better than they do in most chronic illnesses, then at least the necessary fundamentals are there. There are so many research papers indicating that our problems are related to failure of our aerobic metabolism, yet for some reason, despite his perfectly sound research procedures and results, his work has never been accepted into the mainstream. I suppose all I can say, in encouraging you to experiment with these ideas is that it sounds as if you don’t have much to lose…you aren’t getting any constructive help re the lesion from the guys you’ve been to. Anyway, whatever your views on this, I wish you very well, and hope that you do find some path towards recovery – it just doesn’t sound like, at least so far, the medical guys have offered that path… I suppose I am most horrified by the removal of ten salivary glands? Was that really necessary? It sounds so horrible, and so extreme…I do hope you recover as quickly as possible from that. (I’m sorry but the phrase ‘medical abuse’ keeps coming round…) I’m not surprised that your husband wants to dissociate from all that, it must tear him up to see this stuff being done to you. Do keep up the blog…and I hope you feel and benefit from all the good will that is coming your way…Best wishes Nancy
Thanks for sharing your story, Corinne. This issue of what to follow up on and what to let go, especially as we age, is a very difficult one. I expect there are no right answers; we each need to decide on our own.
Right now I’m debating whether to get a second tilt table test and whether to subject myself to 4-6 hours of neurocognitive testing. The question turns on whether there is something actionable that can be done to improve my quality of life depending on the results of these tests. Otherwise, I’d rather skip them. There is no cure for ME/CFS as one of the doctors announced at the Stanford meeting this year.
I need help figuring this out because some things are beyond my understanding. In a way what I’m looking for is palliative care coupled with catching anything life threatening or debilitating that can be fixed or ameliorated to improve my longevity and quality of life.
Taking issues to doctors who don’t understand anything about ME/CFS or don’t recognize it as real makes everything too complicated for me. Which is why I’m back in California being seen at PAMF and Stanford rather than Vanderbilt Medical where there is not a single doctor in all of Nashville who treats ME/CFS. Unfortunately, the head of the IOM group working on ME/CFS definitions is from Nashville…
My best wishes to you; I hope you find something that helps soon!
Hi Esther,
You mentioned you are “debating whether to get a second tilt table test”. I am wondering if this is for insurarance/income support purposes, for diagnosis (to help determine treatment options), or perhaps only for your own information. If the latter, the following may be of interest.
During the early 1990’s, my GP (considered the most knowledgeable about ME/CFS and FM in my large city) conducted what he referred to as a “poor man’s tilt table test” in his office. This procedure is only suitable for patients who are able to stand. The doctor’s nurse took a baseline blood pressure reading, and then had me stand, perfectly still, for a period of time. Every 5 minutes, she took another blood pressure reading to determine the effect of being upright. She stayed with me the entire time, to ensure I didn’t fall. Four additional BP readings (each one lower than the previous one) indicated what my physician referred to as “posturally mediated hypotension”. It seems this explained why I felt so weak while standing.
For anyone who is merely curious, this test can easily be done at home — but make sure someone is with you, and that you are standing beside something soft (eg. a bed) . Of course, simple tests of this type are unlikely to be accepted by skeptical doctors. But, they can point you in the right direction, and in some cases eliminate the need for costly testing in a medical facility.
Esther, please be very careful about neurocognitive testing. I may be repeating what you already know, but unless the tests are administered by a doctor legitimately knowledgeable about ME/CFS, many of the tests used misdiagnose/overdiagnose depression, etc. in patients like us. Drs. Taylor and Jason wrote a great paper on this topic. I think this is it: http://www.tandfonline.com/doi/abs/10.1080/08870449808407452#preview
Thanks for this link – I’ll download the whole article through Lancaster University – in the meantime, as a very experienced psychotherapist who has ME (1986, in fairly good shape now, thanks to being determinedly unwilling to do anything that made me feel worse, and I noticed fairly early on that it was physical exertion that made me feel worse), I think a differential diagnosis is pretty straightforward. It involves being able to tell the difference between a person too sad and apathetic (depressed!) to want to do anything – but whose mood lifts after exercise – and someone who is desperate to do something, tries, finds out they can’t, and gets upset about it. I would guess that anyone with ME would be able to tell the difference in a five-minute normal conversation. But the psychiatrists have an interest in confusing the two. I have looked at a few ‘depression’ scales, and they conflate symptoms of depression with symptoms of ME.
For example, they say that being ‘tired’ is a symptom of depression. But it isn’t. If a depressed person says ‘I don’t feel like doing anything’, that is not being tired, it is being discouraged (mood). Being ‘tired’ is a physical state, resulting from exertion. Different thing. Again, they say that cognitive difficulties are a symptom of depression. What cognitive difficulties are they talking about – if a person can’t follow a plot or solve a problem because they feel too sad or apathetic to bother, that is depression. If a person wants to solve a problem, or follow a plot, but finds that they get confused and tired from the effort, that is ME. Short term memory problems are not a symptom of depression, they are a symptom of ME.
Depression is a mood disorder. ME is a physical problem. The Beck Inventory is one of the worst examples of conflating the two, but others are similarly sloppy in the questions asked and how they are interpreted. As a psychotherapist, I never wanted to mistake a physical problem for a psychological one, and was as careful as I could be not to make that mistake, or let my staff make that mistake. As a person with ME, I didn’t want to be a victim of that mistake, and my drive to do this Ph.D. is to give some credibility to the argument that none of us should be. I haven’t yet studied the instruments mentioned in Jason’s article, but I can make a very confident prediction that the difference between them is that the one that is better at differentiating ME from depression is the one that does not make the mistake of listing the physical symptoms of ME as symptoms of depression.
To go back to the fact that exercise lifts the mood of people who are depressed (because it lifts the mood of healthy people as well), that can be a danger to people with ME. I can’t remember the number of times I have gone swimming, done a couple of very gentle laps, started getting the endorphin high of a bit of exercise, and proceeded to joyfully swim until I made myself sick for a week….We do need to be careful! (I had to give up swimming because I couldn’t afford to keep making myself really ill ….
Oh my gosh, Corrine, where do you get the patience to handle your ‘medical abusers’ so politely? I know I surely couldn’t. So in addition to the energy expenditure, the financial expenditure, the instructional expenditure, your output of manners, patience and courtesy blows all those categories in the weeds! How do you do it?
The irony we find ourselves in is that as we, as individuals, push the Sisyphusian ball of shit up the hill with our noses in search of a cure, the medical industry is thwarting us. It was staggering how much educating you had to provide to your so called medical providers. Instead of you paying them buckets of money, they should owe you for all the instruction you are providing to them. We need to find a way not to waste time and money on medical appointments that require us to do the thinking, research, physical effort, educating the doctors and then having to suffer physical pain and distress from the pokings and jabbings doctors administer.
The further irony is that at just the time a few ME/CFS researchers might be on the verge of a breakthrough, the medical industry, as a whole, is breaking down. As in your case, Mayo is going retrograde. But then you have to realize the standard of care here in Arizona is so much lower than in SF or LA. Its got me stymied for care. Just be glad you are not on the state Medicaid health insurance like I am.
Your fortitude, patience and stamina are to be congratulated. You’re a better patient that me.
Maggie
Glad someone thinks i’m kind and polite and patient 🙂 My poor, exasperated, had-enough, confused husband said on the way home from Mayo that he would not want to be one of my doctors either since i acted like i knew more than they did :)…I said when it came to my body, I DID!!! I do not think i was polite and patient, but i knew what i had to do to not waste time and energy and at this point after 23 years. I’m too old to worry about what doctors, or what anyone thinks anymore if it is going to cost me my health. Thank God i have Dr. Peterson.
Thanks for your support. Good health to you!
reading this makes me fell glad, for once, that I’m in the UK where they don’t put you through invasive procedures unless they would make a difference to your treatment.
Corinne,
Such a chilling heartbreak to read of your return to Mayo Clinic. I went there (Rochester) in utter despair and agony in 1990 and was told, following a week of tests and clinics and doctors, that “…you MIGHT be allergic to beef and tomatoes..”
The doc said to go home to Oregon, wear a little white fabric mask outdoors, and see what happened over the next 6 months. Twenty-four years and some $250,000+++ out-of-pocket medical expenses (“not medically necessary”, “not conventional medical treatment”), I still stick my neck out from time to time and ask for something new.
Nothing comes of it, but I always keep hoping. We all know well how complex it is, but it’s hard to understand that we really get just about nothing as patients and people out of the medical community. I well understand your disappointment, deflation, and surprise (that little of anything comes of all the talking on and on of all your symptoms, everything that has gone wrong, reiterating the history over and over again. I hate going to new doctors and even opening my mouth and hearing my own story again. Keep taking those long deep breaths that give us the determination to keep on and to try again.
My husband has gone with me on all these medical journeys (he worked in a medical school for years) and has been stunned by the inability to think outside the box, to follow clues, to simply want to solve the problem. Physicians generally just follow the ‘cookbook’ they learned in medical school, and CFIDS/ME is not taught. National efforts need to bring pressure on medical schools, despite their resistance to change.
My heart goes out to you everyone out there with this illness. Be bold everyone, and keep pushing them to learn and treat.
Corinne, I was aghast at what you have been putting yourself through. I think most of us know why we are in this dilemma. Just take a peek at the NIH grant funding for the past few years, the more I research the numbers the sicker I feel. Millions wasted on things that should have been put to rest long ago. We get to fund our own research while our tax dollars go to helping other illnesses get huge grants. Since most doctors don’t seem willing to learn very much about ME/CFS we are still in this crazy “no man’s land'” of medical ineptitude. My attitude is ; why get frustrated at a useless medical appointment when I can stay home and be at peace. We are stuck in this constrained version of life for now, so don’t let others tear you to shreds. As for me, I will sit home with my kitty by my side and send Ian Lipkin some money because its good to hear the sound of hope. Thank you for caring enough to share your experiences with us.
I was diagnosed with viral myelitis in May. Valcyte and Valtrex have helped immensely.
i believe this is the train of though DrP has had from the beginning, but having to get a second opinion was the reason i have been on this tangent journey. i am most likely back to the viral issue now.
http://myelitis.org/symptoms-conditions/transverse-myelitis/diagnosis-tm/
I’ve had Sjogren’s for years. Just like my mom. I was diagnosed by my eye dr., with a test called Shirmers’ I think. Just a little piece of paper in my eye for a second or two. It’s a hard illness, always with more complications than one expects. I treat the symptoms, but I do believe some of my fatigue is due to it.
I am so sorry that you’ve been put through so much. And in one day yet. I haven’t the stamina. The meds that have helped me the most is Xyrem for sleep. Good, deep sleep makes a big difference the next day. Also, Lyrica, which I started 40 lbs. ago, has taken care of most of my neuropathic foot pains. They were so bad that I yelped outloud in the street.
For exericise I take Pilates once a week. The teacher understands that I know my limits. I do try to walk daily. If I don’t, then starting again is very painful. I’ve just got to keep it up. Ageing isn’t helping any. Though I think I’ve become kinder to myself, and more resigned to being ill. Sending you my love and empathy, I know just how you feel, Abby
“We must be willing to let go of the life we planned so as to have the life that is waiting for us.”
UGH, this sounds so familiar….especially the gun ho part where something abnormal shows but then they can’t figure it out so you are just out of luck. I think its odd how a lesion on your spine can be taken more seriously if you were well beforehand but you add the mysterious illness along with years of other symptoms and somehow its just not treated with the same quality or care or respect. your story makes me angry and I feel upset that as a patient you were treated in this way, how exhausting to have to explain everything over and over to people who know nothing about your illness and have closed their mind to anything they can’t understand….with an unwillingness and lack of any enthusiasm to really learn new things. Shouldn’t people ,medical TRAINED professionals at the MAYO CLINIC be expected to know more about the very real, life altering illness me/cfs? This is so wrong. I agree with the person who said she would rather stay home and be sick than put herself through the medical abuse cycle (that parts my description not hers) I also think she had a point with sending $ to Ian Lipkin rather than paying any $ to places like the Mayo clinic. Clearly, i feel a sense of familiariaty with your stor…my latest have been stomach inflammation (unresolved of course) and unresolved sleep studies,unresolved nerve pain, etc…etc…etc…i’m done taking drs seriously unless ivebroken a limb or something readily fixable. Ive become a firm believer in natural homeopathic remedies also. I applaud your bravery to keep trying.
Corinne, you are amazing in how you are dealing with all this. Thank you so much for posting about it here – I can’t wait to read your blog about your March Dr P visit!
Very interesting to read how your biopsies showed inflammation. I have had a biopsy done on the thyroid (showed signs of inflammation) and of the skin on one toe, because of acrocyanosis (showed inflammation). Familiar? What if it is like you say, maybe we ME/CFS patients (or at least a subset) are “just walking chronic inflammations”. Can we get more researchers to look into this? (And, I know, we do need to make NIH fund them…)
About Gabapentin/Neurontin: Were you taking 200 mg twice a day, so 400 mg a day in total?
Are you still on that same dosage or have you increased it? If you have had side-effects, have they subsided with time?
Hi Anne
Yes, i think the going thought is that we all have a form of inflammation that medical science does not test for. In other words the tests they use for inflammation, CRP, etc, are usually normal in us. Our inflammation shows up as some kind of unexplained non-specific type, and yet that is the type we all have!! Seems they just don’t have a test for our type yet. I think the word auto-inflammatory may sum up our form of inflammation best.
Yes, at that time i was taking 400mg of gabapentin per day. I am now up to 600mg/AM and 600mg/PM. I have found that the side affects disappear within three days. Just a little drowsiness and by day 4 they are gone. I quickly adapted to it. It has also helped my sleep immensely!
Good to hear from you as i had lost your email. Hope you are doing well 🙂
Thank you for another wonderful blog post and for the generous use of your time and energy in sharing.
I’m so sorry to hear about both ordeals at Mayo. I went to their MN clinic in 1999 — very similar experience. I already had a diagnosis of autonomic dysfunction from Hopkins, yet not one Mayo doctor told me that Mayo then had one of the world’s foremost dysautonomia experts — Phillip Low — you would have thought someone would have recommended I see him. I didn’t find out about him until years later. Instead, the Mayo doctors added nothing except to recommend I return a second time to be tested for depression. “Well, who wouldn’t be depressed after you lot” is what I wanted to, but didn’t say.
But I would have also definitely considered going back given a baffling new diagnosis like you describe. After all, they are supposed to be the best and our understanding of our complex illnesses is so much better now. Right? Right, Mayo Clinic?! I hope you can find some much better answers soon. It sounds like they were more intent on proving how clever they are then on easing your suffering and only ended up compounding it. Terrible. Shame on them.
They had a Dr. Goodman, a POTS expert there, and that was who they were trying to ‘herd’ me towards. Its funny because they said people came from all over the world with mysteries for them to solve so that i should feel confident i was in good hands. then at the end it was like they wanted to ignore the ‘mystery’ because it was too complicated for even them.
I get that doctors can’t know everything but the thing that bothered me most was the way they ignored all my past workups, the other doctors involved in my case, etc. etc and tried to just keep everything in-house and get me to do tests only at their facility. i don’t want to sound harsh or judgmental but when i walked out of there i felt as though i were ‘escaping a cult’. granted i know they help thousands of people all the time, but that was my experience…and i have spoke to others who have felt the same way.
Corrine, so sorry you had such an awful experience. I wish you had waited for Dr. Goodman. He’s the man. I had a really bad experience with Dr. D too. Ive written Cort to send to you. Don’t want to go into details here. After 3 visits to Mayo and getting changed to Dr. Goodman and seeing Dr. Lewis and also using another doctor outside of Mayo Dr. Stephen Fry – I got my answers. Not all doctors are like Dr. D. There are some very good doctors there. Sad you got one that was not. It took me 5 weeks of testing at Mayo to come up with about 5 different DXs and 2 in the rare disease catagory. So sorry you had to experience heartache with this doc. I know your pain, I had it too.
Issie
Make that 7 weeks of testing. Had to go three times. First time 3 weeks. Second time 2 weeks and third time 2 weeks. I almost gave up after such a bad experience, but glad I didnt.
Issie
So sorry to hear about your experiences at the Mayo in Arizona.
I live in Arizona too and the Mayo here is not the same quality as the Mayo in Rochester. It does NOT have a good reputation for CFS/ME/FM issues.
I have FM with inflammation and my son has severe CFS. I have experienced remission with steroid injections of kenalog (sp?) once every three months.
My sons symptoms are primarily neurological, He too gets worse with each flare up.
He sees Dr Chia in LA, a virologist. But you are doing everything that he would recommend.He does use Imunoglobulin. He does not use Valcyte but also uses other antivirals and interferon injections. You can google him.
Feel free to contact me by email for more information.