Recently Dr. Lucinda Bateman proposed that neuroinflammation in the middle part of the brain could explain many, if not all, of the symptoms found in Chronic Fatigue Syndrome. With that intriguing hypothesis in mind, we take a look back at a fascinating MRI study by Dr. Leighton Barnden of the Department of Nuclear Medicine, The Queen Elizabeth Hospital, Adelaide, that came to a similar conclusion two years ago.
This study examined MRI findings, symptom, depression, and anxiety scores, and autonomic nervous system functioning via 24-hour blood pressure monitoring in 25 people with ME/CFS and 25 healthy controls.
Worries about the heterogeneous presentation in ME/CFS led Dr. Leighton Barnden to discard the normal ways of doing MRI studies. Barnden did do a straight MRI comparison of the brains of Chronic Fatigue Syndrome (ME/CFS) patients and healthy controls, but he also compared patterns of MRI results, autonomic functioning, and symptoms within each population. For example, if abnormal autonomic nervous system results in the ME/CFS group correlated with the abnormalities he found in his brain scans, Barnden would be able to zero in on areas of the brain that were of significance in ME/CFS.
Results
Losses in Midbrain White Matter Associated with Worsened Symptoms
“These results are consistent with an insult to the midbrain at fatigue onset that affects multiple feedback control loops to suppress cerebral motor and cognitive activity and disrupt local CNS homeostasis, including resetting of some elements of the autonomic nervous system (ANS).”
Reduced white matter in the midbrain suggested demyelination was interrupting signals to the other parts of the brain
As Barnden expected, a straight comparison of MRI results revealed no significant differences between the two groups. When he performed a regression analysis of his MRI readings against the patient’s symptoms, however, issues in the midbrain popped out in the ME/CFS group. His analysis indicated that reduced white matter volume in the midbrain was highly associated with fatigue; i.e., the more fatigued a person was, the more likely they were to have reduced levels of white matter in their midbrains. That suggested damage to myelinated cover of the nerves had occurred.
(It’s interesting, given the myelination problems in multiple sclerosis, that a small study recently found reductions in BDNF in both MS and Chronic Fatigue Syndrome. Check out Knackered Nerves: Do Low BDNF Levels Spell Nerve Exhaustion in Chronic Fatigue Syndrome?)
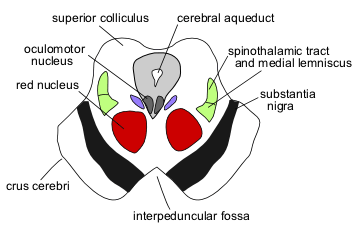
The midbrain or mesencephalon is a portion of the brainstem associated with arousal (alertness), motor control, sleep/wake state, vision, hearing, and temperature regulation. It is located below the cerebral cortex and above the thalamus/hypothalamus – quite centrally located.
The substantia nigra in the midbrain is closely associated with basal ganglia – an area of interest in ME/CFS. (A blog will appear shortly on basal ganglia dysfunction in Chronic Fatigue Syndrome. Miller’s findings suggest that reduced dopamine functioning in the substantia nigra leads to basal ganglia dysfunction in some people with ME/CFS.)
Calling the midbrain a conduit for information passing from the spine to the upper brain, the authors noted that it contains parts of the reticular activation system and centers of monoaminergic and cholinergic neurotransmission.
Grey and White Matter
Both grey and white matter were reduced in different parts of the brain in the people with ME/CFS.
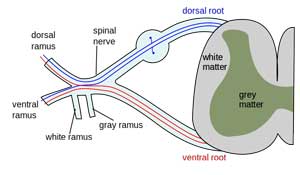
Grey matter consists of neuronal cell bodies, glial cells, and capillaries. White matter is largely composed of the myelinated axons or limbs that stretch out from neuronal cell bodies and communicate the nervous system signals to the rest of the body. It’s composed of glial cells as well. It’s the myelinated aspect of nerve axons that makes them whitish in color.
Think of grey matter as largely being the neuronal cell bodies and white matter as being their limbs. The nervous system signal is produced in the grey matter, and the white matter communicates the signal between different parts of the brain and the spinal nerves. Grey matter issues imply problems with nervous system signal processing and cognition (or a problem with the capillaries or the glial cells) while white matter problems imply problems communicating the signal and coordinating activity between parts of the brain.
Autonomic Nervous System Problems Associated with Losses in the Brainstem, Prefrontal Cortex and Hypothalamus
Next, Barnden regressed his fMRI findings against ‘hemodynamic scores’ produced by analyzing blood pressure and heart rate over a 24-hour period to determine if parts of the brain were associated with altered autonomic nervous system functioning. ANS functioning was assessed while seated, while asleep, and at all other times.
Barnden found alterations in 24-hour blood pressure and heart rates in ME/CFS patients compared with controls. Those alterations were associated with reductions in grey matter in the brainstem as well as white matter in the prefrontal cortex and hypothalamus. It appeared that problems in these areas of the brain were causing autonomic nervous system problems in ME/CFS.
Activating System in the Brain was Hit
With the strongest correlations showing up in the reticular activation system (RAS) the authors drew special attention to it. The RAS is responsible for maintaining cerebral cortex activation. It also transfers messages between the central and peripheral autonomic nervous system neurons.
With the reticular activating system presumably not activating the cerebral cortex properly or relaying all the autonomic nervous system messages from the brain to the body, the stage appeared to be set perhaps for the ‘slowed brain’ that the Zinns spoke of at the Stanford Symposium as well as the autonomic issues present in ME/CFS.
Highly significant reductions in brainstem white matter over time also suggested that the longer a person had been ill with ME/CFS the more declines in brainstem white matter occurred.
Brain Blood Flow Problems
Brainstem grey matter reductions, on the other hand, were associated with altered pulse pressure in ME/CFS patients. The authors proposed this correlation suggested problems with cerebrovascular autoregulation (i.e., regulating blood vessel flows in the brain) were present in ME/CFS.
Specifically, they noted their findings suggested that problems controlling capillary hydrostatic pressure in the brain were present. Cerebrovascular autoregulation is primarily a function of the arterioles that control the rate of blood flow into the capillaries. Arteriole activity is regulated both locally (myogenic reflex) and centrally via the brainstem as well as via astrocytes.
The authors suggested problems with astrocytes – a form of glial cell – in the brainstem were probably responsible for the problems with brain blood vessel flows.
Glial Cells Take Center Stage
Their findings suggested, then, that problems with glial cells – in particular, astrocytes – either localized in the brain stem or possibly widespread throughout the brain were causing both the white matter shrinkage and the autonomic nervous system problems found.
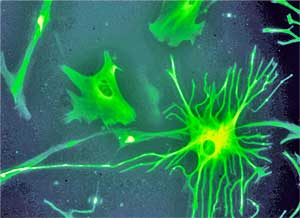
Glial cells provide both scaffolding and protection for the neurons. Through the production of a wide array of pro-inflammatory factors, glial cells also direct much of the immune response in the brain. Overactive glial cells are believed to be major drivers of central sensitization. Glial cell activation may be behind the widespread neuroinflammation found in the Japanese ME/CFS study.
Prefrontal Cortex
One of the odder findings concerned increased heart rates when asleep. This finding, which has been validated in several studies, appears to reflect increased sympathetic nervous system activation in ME/CFS. The study found that increased heart rates when asleep were associated with reduced prefrontal cortex volumes in ME/CFS patients and increased prefrontal cortex volumes in healthy controls. The authors noted that the prefrontal cortex communicates with various regions of the brain (anterior cingulate, dorsolateral cortex) involved in the autonomic nervous system, and then pinpointed perhaps the locus of ANS problems in ME/CFS – the hypothalamus.
Hypothalamus
The hypothalamus, which sits right below the midbrain, has long been suspected as the cause of the HPA axis issues in ME/CFS, but the hypothalamus also plays a key role in autonomic nervous system regulation. White matter volume alterations in the hypothalamus were associated with sleep heart rate differences in ME/CFS. Those alterations suggested the messages from the hypothalamus to the rest of the brain and the body were perhaps not getting through.
Lying at the center of all the brain structures involved in autonomic regulation, the hypothalamus also communicates with autonomic nerves in the body via the reticular activating formation in the brainstem – the very locus of the midbrain problems the authors found. The hypothalamus also modulates and is modulated by the immune system. As with the midbrain, the authors believe glial cell issues are behind the white matter changes detected in the hypothalamus.
The authors stated that a second study looking more deeply into the autonomic nervous system and the brain was forthcoming, but it’s now several years later and no studies have been published.
Conclusions
“These findings therefore support our original hypothesis of involvement of the midbrain, prefrontal WM and/or supraspinal autonomic control regions in CFS, and indicate that CFS is associated with biological changes affecting fundamental and evolutionarily primitive structures of the CNS.”
Suggesting these findings provide a ‘unifying’ observation, the authors proposed that demyelination in the midbrain that impairs communication and coordination with the rest of brain may explain many of the symptoms found in Chronic Fatigue Syndrome, including those associated with the autonomic nervous system dysfunction.

Is white matter damage in the primitive areas of the brain causing many symptoms in ME/CFS? More studies are needed…
They also found evidence that grey matter issues in the brainstem were associated with impaired blood flow regulation in the brain. The hypothalamus and reticular activating system received special mention.
Glial cell problems – already of great interest in ME/CFS – were front and center, with the authors proposing glial cells were behind both the white matter and grey matter problems found. The authors noted that glial cell problems may be more widespread in the brain.
It will be intriguing to see if these findings correlate with the Zinns’ findings of a ‘slowed brain’ and their proposal that a limbic encephalitis is present in ME/CFS. The Zinns highlighted problems in similar parts of the brain: the brainstem, the limbic system, and the prefrontal cortex. Their suggestion that a pattern of ‘global hypoactivation’ could fit with the Barnden findings of damage to the reticular activating system.









Could the glial cells be inflamed by a virus, perhaps of the vagus nerve? Since rituximab turns off the immune response, it must relieve the inflammation in the glial cells but ultimately leaves the virus intact as the symptoms return after treatment. Just wonder how Van Elzakker is doing, and rituximab.
I emailed VE. He’s been swamped with his PTSD work (his paying job) and hasn’t had the free time to work on ME/CFS much this summer. He does have some money for testing and hopefully that will get going soon.
Viral attack on the glial cells – which are in immune protected territory – that is, they are tissues the immune system has a hard time getting to if I remember right – is very possible.
Thanks for checking, Cort. Very frustrating re VE’s time constraints.
One more point: The statement that the white and gray matter may shrink with time is – I hope – speculative. If that were true, CFS would be degenerative, but in most people the symptoms decrease with time, so I’d like to think that’s not true.
I think its true that for most people symptoms do decrease over time. I think adjustments to ones limitations probably help a lot. He found 1% decrease a year – quite a bit – that’s 10% over ten years and 20% over 20 years (!). That seems like an awful lot.
According to a report on a recent seminar he gave though, it appears there was compensatory myelination in some areas. It could be that a loss is one area is being compensated for in another.
Yes, that must be why I have a lopsided brain.
Hmmmm. Still nothing regarding causation!
Nope – nothing regarding causation. Although if the glial cells are doing this – and that is speculation – the results suggest it but don’t confirm it – that narrows it down.
Having a couple of studies find problems in the same areas of the brain is validating as well. We really need something to shock the research world into paying attention to us.If the Zinn’s and other studies line up with this one may be that will help – and we’ll get to causation at some point.
We don’t need to have the cause to find treatments, though. If you can verify something that’s gone wrong then you can aim treatments at it without knowing the cause.
Cort nailed it exactly – causation is secondary as long as we have treatments! Of course, it would be nice to be able to turn the damage off at the source, but if treatments can at least halt the progression (assuming it does progress, which I would tend to assume, even as just a normal course of aging), then at least that is something. Reversing the damage with treatments would be even better.
As for me, I’m going to start doing and taking everything I can to increase BDNF, including SSRIs, music, meditation, etc. Doubt there will be any overnight results with this focus, but every little bit I’m sure will help.
Want to thank Cort for revisiting this topic – I had forgotten all about the earlier MRI studies, if in fact I even saw them. I seem to remember the BDNF connection, so this article was a good jolt for the memory! :- )
Thanks jrez – good luck with your protocol 🙂
Rituximab kills B cells where stealth viruses or bacteria hide. The infectious agent(s) may return to reinfect B cells because they were not completely knocked out by rituximab…only in B cells.
Van ElZakker and Pridgen have already wrapped this up in terms of causation.
Why others aren’t jumping on the bandwagon to treat/cure this is what I am struggling
to understand.
How much longer must we wait.
No group has aided in self research as has
the CFS community.
Now reward us.
🙂
I hope you’re right! The medical world requires validation, though. It’s so hard when you’re a disorder that gets little funding for anything to move quickly or at a normal rate of speed (which is pretty darn slow.)
Looking forward to Pridgen’s results in November.
Please just validate something and get us some treatment!
As always it leaves me feeling overwhelmed with so many things that can be out of whack when nothing is wrong with us. In the meantime since you guys are bringing a rituximab has any of you tried Plaquenil which my rheumatologist says is a less risky way to go after the B cells
I also would love to hear if anyone diagnosed with CFS/ME has taken plaquenil, and if so what were the results. My brother suffered from crippling mixed connective tissue disorder, went on plaquenil for 1 1/2 years and returned to normal functioning. He’s been status quo for 8 years now. I know it’s not a cure but it did settle his immune system down to where he leads a very active, full life.
I was in I think it was their second study (had my MRI and SPECT etc in late 2010) was this article about that study or the earlier one?
Once again I forgot to put the study in the blog (sigh…) It was a 2011 study. They mentioned another study coming out in the paper and at a recent seminar in Australia it appears that that study will be coming out – hopefully soon.
NMR Biomed. 2011 Dec;24(10):1302-12. doi: 10.1002/nbm.1692. Epub 2011 May 11. . A brain MRI study of chronic fatigue syndrome: evidence of brainstem dysfunction and altered homeostasis. Barnden LR1, Crouch B, Kwiatek R, Burnet R, Mernone A, Chryssidis S, Scroop G, Del Fante P.
I tried plaquenil on two different occasions but unfortunately could not continue with it because it caused my WBC count to go very low, my feet to rash, and bad nausae.
I guess if this study regarding damage to parts of the brain is on the right track you can all go and tell your GPs, who told you that ‘it was all in your head’ , that they were to some degree right….. And should therefore have paid you a lot more attention.
Keep up the good work and interest.
My daughter is in her fifth year of fatigue (now 18) and I am desperately hopeful that there will be some kind of breakthrough…..soon!
Agreed….Good luck with your daughter; she’s young and hopefully that will help.
Can low bloodvolume causes these problems? I think it can.
I wonder if it problems in the midbrain and the autonomic nervous system issues they cause could be contributing to low blood volume? Could some messages about increasing blood volume not be getting through?
yep
This hits it on the head (No pun intended), this makes the most sense thus far. The hypothalamus also controls the immune system, which would make it hard to fight the viruses, therefore letting them ramp up. The nervous system is not getting the correct messages, which in turn effects fatigue, brain fog, nerves, heat/cold regulation, obviously, basically a brain injury. Why or how did we get it? What would treat it? I don’t know about you guys, but I can hardly tolerate the heat, everything amplifies, symptom wise. I am always telling my family “there is something wrong with my hypothalamus”. This study needs to be fast forwarded, and funds provided.
Too right. Some of the immune dysfunction observed in CFS is likely to be the result of influences of the brain / CNS, rather than the other way round.
Some researchers harp on and on about NK cells, but NK cell activity is reduced in many illnesses so its hardly unique.
This hits it on the head (No pun intended), this makes the most sense thus far. The hypothalamus also controls the immune system, which would make it hard to fight the viruses, therefore letting them ramp up. The nervous system is not getting the correct messages, which in turn effects fatigue, brain fog, nerves, heat/cold regulation, obviously, basically a brain injury. Why or how did we get it? What would treat it? I don’t know about you guys, but I can hardly tolerate the heat, everything amplifies, symptom wise. I am always telling my family “there is something wrong with my hypothalamus”. This study needs to be fast forwarded, and funds provided.
I tried plaquenil many years ago , it was not helpful. LOW DOSE NALTREXONE has been the best drug I have tried. It does affect the microglial cells so maybe the reason for positive results in so many with me/ cfs. I cannot personally agree with the degeneration of the brain but perhaps the LDN has changed that issue for me. I will always stay on LDN unless something better is discovered. Absolutely recommend meditation, music, happiness and exercise to whatever degree is possible. When I could not walk, I would visualize myself power walking like I did prior to this devastating disease. I have NO RESPECT for the medical community after 18 years of this illness, who allows this to continue to destroy peoples lives, they are worse than Nazis. Guess I had better meditate a bit more, obviously some repressed anger still just below the surface. -:)
Yes, still a bit of repressed anger there! 🙂
Thanks for the word on the LDN; it’s great that a relatively cheap alternative is present even if the vast majority of doctors know nothing about it.
This anger is so
Justified!I am sure that with just some small, joint pushes, the medical profession around the world could cooperate and build on research such as this. Now that some doctors in the US are taking away effective pain control, we need a way of controlling ME/CFS sooner rather than later. I salute all Fibro warriors, may our cure come soon enough for us to have a few good years at the end of our lives.
In my own case, I’ve had abnormal cognitive testing, abnormal PET scans and white matter lesions on MRI. And my brain does seem to be getting worse. In my case, I’d say this thing is neuro-degenerative. But I can’t speak for the group, and we’re a heterogeneous cohort to begin with…
I’ve been saying it for years…it’s all in the brain!
So it IS all in our head – so to speak 🙂
Looking forward to their next paper….
Andrew Lloyd from Sydney is a guy in CFS research I really really respect. He hasn’t always been liked in the CFS community because some years ago he formed the strong view that CFS was essentially not immunological (well at least its perpetuation was not immunological but may have been triggered by an immunological insult).
Many many people in the CFS community cling to the immunological hope, and its a forlorn one.
Thankfully, more and more effort seems to be going to the brain / CNS where the real problem is (granted there may be some immunological / inflammatory overlap) so let’s hope for progress there, rather than the big immune distraction that has yielded almost zilch in 25 years.
Dr. Barnden looks like he is continuing his ME/CFS research at NCNED: http://jobs.theconversation.com/jobs/8151-researcher-imaging?utm_source=theconversation.com&utm_medium=website&utm_campaign=sidebar_job (deadline for job advert is August 29, 2014)
I don’t know how you find this stuff, Tom but that is very encouraging – a full time position, too – thanks 🙂
I am NOT associated with selling any products, I have been taking ALGONOT NeuroProtek by Dr Theoharides and so far I think it is helpful. Everyone is different so it may not be helpful to others. I have recently experienced anaphalaxis to foods which I believe to be histamine intolerance and a new allergic reaction to nuts now -:( Until I see an immunologist I am using supplements as well as avoiding nuts and other foods. This is all so complex. I don’t think that’s in my head…well it could be if mast cells were degranulating in my Brain which seemed to be the case. It is actually a miracle I am alive….I did not expect to be. We really deal with more than anyone can ever imagine.