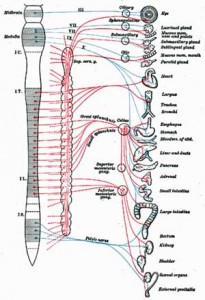
We just saw that some Japanese ME/CFS researchers believe they may have developed an objective test to measure post-exertional fatigue. Heart rate variability tests indicated that fatigue after a cognitive test is associated with reduced parasympathetic nervous system (PNS or ‘rest and digest’ system) functioning and increased sympathetic nervous system (SNS or ‘fight or flight’ system) functioning.
Heart rate and heart rate variability studies in Chronic Fatigue Syndrome and Fibromyalgia suggest that difficult cognitive tests aren’t needed to put them in a similar state – their ‘fight or flight’ system is up, and their ‘rest and digest’ system is down – all the time.
These two branches of the autonomic nervous system operate in a ying-yang fashion; when one is up the other is down. In the human body the default is to have the SNS on. Since the PNS is the only thing that can turn the SNS off, unless it does so, it will be on all the time. That suggests that the PNS, not the SNS, may be the problem in ME/CFS and that finding a way to boost it up could be helpful.
Since an over-active SNS has been associated with poor sleep, cognitive decline, inflammation, and increased pain and could play a role in many other symptoms in Chronic Fatigue Syndrome and Fibromyalgia, turning it down could be quite helpful.
Vagus Nerve
That brings us to the vagus nerve. Since the vagus nerve controls parasympathetic nervous system functioning in the body, boosting the activity of the vagus nerve should increase PNS functioning and reduce the SNS activity that’s of concern in ME/CFS and FM.
The medical community knows how to do this. In fact it’s been resetting the ANS by stimulating the vagus nerve in thousands upon thousands of patients for the last decade or so. The problem is that it involves the surgical implantation of an electrode and a generator in the neck region. It’s been effective in about 50,000 people with treatment-resistant epilepsy and has been approved for treatment-resistant depression as well. It’s been trialed in heart failure, inflammation, Alzheimer’s disease, chronic pain, and tinnitus, but the surgical requirement has meant, despite the benefits it could bring to a wide variety of disorders, vagus nerve stimulation (VNS) has not been widely used.
That may be about to change. If a new advance works out, vagus nerve stimulation may be available to many.
Listen Closely

The Study
(Non-invasive Vagus Nerve Stimulation in Healthy Humans Reduces Sympathetic Nerve Activity; Jennifer A. Clancy a, David A. Mary a, Klaus K. Witte a, John P. Greenwood a, Susan A. Deuchars b, Jim Deuchars b,* Brain Stimulation xxx (2014) 1e7)
In this study researchers from the University of Leeds in the UK, in a process called transcutaneous vagus nerve stimulation (vTNS), applied an electrode to the surface of the ear to stimulate the vagus nerve in healthy controls. They hoped to electrically put the body into rest and digest mode.
First the participants were asked to lie down while their autonomic nervous system activity was tracked. Then surface electrodes from a TENS unit were applied. The TENS unit was turned on in one group and not the other. Heart rate variability tests and muscle sympathetic nerve activity (MSNA) indicated if the status of their autonomic nervous systems changed.
Results
The electro-acupuncture-like treatment of the ear actually worked. The low frequency aspect of the heart rate variability measure increased in the treatment group (but not in the control group) indicating that the activity of the fight or flight system (SNS) had been reduced while the activity of the rest and digest system (PNS) had increased. A fifty percent decrease in muscle sympathetic nerve activity in the leg indicated the reduced SNS activity was large and far-reaching extending to the muscles in the limbs.
Much work needs to be done to validate this approach in disease. Some other studies using different techniques or smaller sample sizes have not had significantly positive results, but one study using electroneurostimulation of the ear in coronary artery disease had impressive results. After four days of fifteen minutes of tVNS their angina at rest had stopped and they were taken off vasodilators. After seven days their exercise intolerance had decreased enough and they were able to climb 5-7 flights of stairs without suffering from angina.
Because tVNS simply turns down the SNS (instead of addressing why it’s increased) it’s not a cure. Three weeks after the tVNS sessions stopped the coronary artery patients’ relief ended.
If used regularly, though, it’s possible it could improve sleep, cognitive functioning, and perhaps even exercise tolerance. As an adjunct therapy that reduces the ‘load’ in ME/CFS – thus assisting other treatments’ effectiveness – it could be very valuable.
The Vagus Nerve Redux
The vagus nerve is a big deal in more ways than one. Not only is it responsible for telling the ‘fight/flight response’ to go to sleep, it’s also the conduit through which most of the body’s immune signals get to the brain and through which the brain’s immune signals pass through to the body.
The anti-cholinergic functions of the vagus nerve make it a key part of the anti-inflammatory response. Low PNS activity is associated with increased inflammation, making it no surprise that reduced PNS activity is common in cardiovascular disorders.
An over-active sympathetic nervous system, for instance, is believed to skew the immune response in the Th2 direction resulting in increased antibody production and decreased protection against intracellular pathogens. Turning the SNS down could then improve antiviral defenses and reduce autoimmune processes.
Chronic Fatigue Syndrome and Fibromyalgia
It bears noting that the general type of ANS dysfunction found in ME/CFS – increased sympathetic nervous system and decreased parasympathetic nervous system activation – is also found in a variety of chronic disorders. (One wonders if a base state of dysfunction (low HRV) is present that gets translated into different configurations in different disorders. The very complex ANS system provides many opportunities for different things to go wrong.)
From an increased heart rate while asleep, to the pounding hearts in POTS patients when they try to stand, to low blood volume, to blood vessel constrictions in the brain, to increased nerve fibers in the hands and more -there appears to be a lot going on with the autonomic nervous systems in ME/CFS and/or Fibromyalgia. There may be no telling what a treatment designed to broadly reduce SNS functioning would have on individual ME/CFS or FM patients, but to all appearances it’s trending in the right direction.
It’s clear that reducing sympathetic nervous system activity is simply good for one’s general health. Decreased heart rate variability is associated with an increased risk of death — not just in people with cardiovascular disorders, but in the general population as well.
Insurance companies surely won’t be paying for tVNS in ME/CFS at this point, but with low HRV well documented in ME/CFS, one wonders why they wouldn’t do so as this technology becomes better validated (as hopefully it will.) The next step for these researchers is testing the device in heart failure patients.
Much remains to be done before electrically stimulating vagus nerve endings becomes the du jour treatment for disorders involving the sympathetic nervous system. Some studies have not been successful. It’s not clear how long the boost to the ‘rest and digest’ system lasts either. It is, however, a non-invasive approach that does not appear to cause side effects and which may, this study suggests, have far-reaching effects on the autonomic nervous system.
Clinicaltrials.gov indicates that vagus nerve stimulation via the ear is currently being trialed in diabetes, in healthy people, to reduce fear in healthy people and nausea.
The Mind/Body Approach to Vagus Nerve Stimulation
You may not need a prescription drug, an electrical implant, or even an electrode taped to your ear to reduce your SNS and boost your PNS activity. Mind/body techniques that induce the relaxation response such as Qigong, meditation, yoga and others appear to be able, over time, to affect autonomic nervous system functioning in some people.
Next up we hear from an experienced meditator who abandoned her meditation practice when she came down with ME/CFS but then later picked it up again and experienced significant benefits.







I bet chanting would really stimulate the vagus nerve. I bet it could produce SNS/PNS rebalancing effects, too. If to chant you take deep breaths and expel them slowly with pressure, you’d also be getting that oxygen/altitude effect Cheney talks about. Definitely worth a try!
Was so fascinated by this article until I saw Cheney heralded in the first reply.
As a former patient- He is the biggest disappointment in any of my diagnosis.
Completely set me back so much and was so wrong on so many levels it is scarey.
TELLING HIS PATIENTS THEY ARE TOXIC TO OXYGEN? I AM ON A CPAP
MACHINE NOW AND NEVER FELT BETTER. COMPLETELY STOPPED ALMOST ALL OF MY HEART PALPITATIONS.
Carole
Its is possible for oxygen to oxidize if the patient
is highly toxic. Likewise, some breathing exercises
can be extremely harmful as can be some type of meditation..
Dear Carole,
I’m sorry you are on cpap. I find it doesn’t help our cause to focus your frustration on our precious docs. Not all of us have the same physiology. But oxygen toxicity exists! You surely don’t belong in that cohort.
Wish you all the best.
Susan
This saved my life after 6 years of being bedridden in more pain than giving birth to my daughter, 24/7. Took about 2 mins with nothing but my hands. But then, I went all HecK Yeah! Started shocking it & I’m bedridden again.. & it isn’t looking good. From seizures to strokes, looking to be my future. I have a spinal tap coming up & autonomic crisis is on blast. So I highly recommend it.. However, use your hands or extra low voltage. This can kill me. Don’t be me.
One of the effective modalities I have found in my fifteen year search to balance SNS and PNS is the use of an alpha-stim device and addressing the polymorhisms that cause methylation disruption. Using Nutrigenomic concepts presented by Amy yasko and Rich Von Konynenburg I have found renewed energy, mental clarity and a reduction in fibro-pain to the point of enjoying and participating in life again. Very grateful to all the people who participate in the quest to find some answers and share their knowledge.
@Sean L — which alpha-stim device did you you use? How do you use it? I’ve done everything I can with treating methylation disruption, and I need to move on to the next step. Thank you!
Anyone report any vertigo side effects with this stimulation? Get intermittent vertigo so am careful with ears and wrist accupressjre points
Also, been over 4 years since this very nice opinion piece. Any updates?
I want the vagus nerve stimulation. I have a practically dead intestinal system for almost 3 years. I cannot relax even with meds and practicing the mind/body relaxing techniques. I am getting sicker every day. Where can I go to get this done. I live in PA near Philadelphia. I am so looking to try new therapies. If any doctor will see me; I would be so thankful.
Dear Debra,
I have suffered from fibromyalgia and chronic fatigue & immune dysfunction for over 20 years now. I found a doctor associated with the Holthorf Clinic in King of Prussia PA whom I adore. His name is Joseph A. Garabedian and he has done work with the likes of Dr.Jacob Teitelbaum and Dr. Ken Holthorf, both of whom were also CFS sufferers. Just google Dr. Garabedian and you will find lots of info on his protocol and practice. He also has an associate doctor and a nurse practitioner Andrea who is very good and not quite as expensive I believe. Best wishes for coping with this painful affliction! Perhaps Dr. G can find some things to help you feel at least a bit better. I would say that my health ranges from 50 percent better (on bad days) to 75 percent better (on good days) than what I was before seeing him. Sincerely,
Amy Lang
Dr. Garabedian is part of our ME/CFS experts panel which answers one question a month on ME/CFS. That’s going to start up again in September. 🙂
Yes, Dr Garabedian is wonderful, compassionate and helped me quite a lot. Also, Dr Chung at Chung Institute is excellent. Both helped my Fibromyalgia/CFS greatly but no one seems to have answers for chronic migraines that seem to go along with the Fibromyalgia?
I am reminded of how sick I was 8 months ago before I started taking Low Dose Naltrexone. Now although I still experience whole body pain etc., I have endorphins which help me think and deal better. I was even able to find a Walgreen compounding pharmacy which is able to bill my Medicaid insurance for it. Please read up about LDN for FM/ CFS. God Bless You. Get better!
Glad to hear Ingrid.
People unfamiliar with LDN might want to check out our LDN Resource center
Have you tried a pro-biotic?
Like
Renew Life Ultimate Flora Critical Care 50 Billion
http://www.amazon.com/gp/product/B001LIW11Q/ref=wms_ohs_product?ie=UTF8&psc=1
or the stronger one
Renew Life Ultimate Flora Super Critical 200 Billion
http://www.amazon.com/Renew-Life-Ultimate-Critical-23-1-Gram/dp/B001LA1RKU/ref=pd_bxgy_hpc_text_y
If you’re having constipation problems, you might want to try a course of aloe capsules. If you are also having trouble with dry skin and mucous membranes, try
guafenisen tablets (Mucinex) (helps “moisturize” your colon)..
Kim & Kelly Derrick
Any one work with BradYates YouTube? Has videos. Faster eft’..I have pTSD startle mode response
Janet
Thanks. Is there a way to know what points on the ear to treat? I have an electro acupuncture device already and I’d love to try this!
Susan, Here’s a link to the abstract. If you look under “methods” it shows the frequencies they used (I think), but I didn’t see what points on the ear they used.They only mentioned the “skin of the ear”, which I assume is the outside of the ear. But where? If you try this, can you update us on your experience?
It’s the “concha” of the ear, which is that part in the front of the ear canal that sort of sticks out. You can see it on line under ear anatomy. Not all the charts have it but some do. check it out.
That flap is actually the tragus, and that’s where the electrodes hook up. The concha is the little bowl-shaped area beneath the tragus. You can see a picture of this at http://www.sciencedaily.com/releases/2014/08/140819200211.htm, with the electrodes hooked up. Be sure to put the “live” part of each electrode on the outside of the tragus.
Great to see a story like this being covered, instead of the usual drug-based research/therapies. I did notice though, that the study used healthy controls, rather than people with CFS. Given that CFS seems to turn everything on its head, can we necessarily presume that transcutaneous stimulation of the vagus nerve would have the same calming effects (or last as long) as it does for healthy people?
It will require studies on sick people. particularly people with ME/CFS and FM to know. Clinicaltrials.gov indicates that vagus nerve stimulation via the ear is currently being trialed in diabetes, in healthy people, to reduce fear in healthy people and nausea.
Another mention of this study said they appled electrical pulses to the tragus, the small raised flap at the front of the ear immediately in front of the ear canal.
There’s a photo too. Here’s the site: http://www.sciencedaily.com/releases/2014/08/140819200211.htm
Can’t wait to try it!
Has anybody had good luck with HeartMath programs?
Thanks Laurie!
Wow, thanks for finding that Laurie. I love the clear photo. So, you’re going to try this?
This article on “resetting” the autonomic nervous system has me curious. A year ago this month I had a minor gyno surgery procedure done that I was dreading. I feared the anesthesia would mess me up and hurl me into yet another painful fibro relapse. Or worse yet, that my weak immune system would pick up some nasty infection while I was at the hospital.
To my great shock and surprise, my fibro pain greatly diminished after my surgery and flareups are now few and far between. I have honestly felt better this past year than I have in the past twenty! Has anyone else had a similar thing happen to them? My doctor laughs at me, but I really think somehow my nervous system was “reset” by being put under anesthesia. What else could it have been? Maybe the oxygen? I don’t think I got any painkillers. After all, if the reset button works on my computer, is it that far off to think it could work on me? Maybe we all need to reboot!
People with severe Complex Regional Pain Syndrome are sometimes put into a ketamine induced coma to reset their nervous systems. It works in a significant portion of them. I’ll bet it was the anesthesia. I actually feel better – calmer and with more energy- after dental anesthesia :). Congratulations.
I have a tens machine (very inexpensive) and also a Fisher Wallace Cranial Stimulator. I may be my own guinea pig and try this. The tens can give jolt so I’d use it very low or on the front ear flap.
Anybody think this is a really bad idea, practicing on myself?
I’m pretty desperate. My SNS is always on and I know this is making me worse and I get a teeny bit of PNS after 5 mg. of Xanax which I hate.
Hi Laurie,
I bought a device from Heartmath but it hasn’t really helped me and I haven’t used it for awhile. It does give you feedback though as to whether you are in “coherence.” I think it’s a bit overpriced but they have 20% off sales occasionally, and have good customer service. A lot of folks like it though, so don’t let me discourage you from trying it.
thanks Betsy
Is not the entire ear be a useful site for accupressure work? I suspect this is something known for millennia to the Chinese.
Hmm. There’s a device called the “P-stim” being used for pain relief in chronic and post-op pain. Electro-acupuncture to the ear. See: http://www.biegler.com/pstim.en.html.
TEns machines are often used in pregnancy and in the uk can be rented for a few weeks quite easily, I imagine it’s the same in the US. However a quick google also turns up this for the US http://www.amazon.com/Tens-Handheld-Electronic-Pulse-Massager/dp/B007TOJ948/ref=sr_1_1?ie=UTF8&qid=1409379290&sr=8-1&keywords=tens+machine
and in the uk http://www.lloydspharmacy.com/en/lloydspharmacy-tens-dual-channel-digital-pain-reliever-253601
Possibly cheaper models available and you might want to look at the cost of replacement gel pads.
This is interesting, I would like to try it; a 50% reduction in nerve activity is huge! I wonder if self administered acupressure of the tragus will help? I will certainly give it a try.
Mediation, visualization and deep beating (in the «hara») helps me when PEM is on the rise. But the truly helpful intervention is beta-blockers – I would not function without them! I wonder how much relief cardiac patients will get from the TENS machine compared to beta-blockers. I look forward to more research on ill people.
A curious thing about the ANS is that sexual arousal also calms the over active SNS. My doctor informed me that the PNS drives sexual arousal, but it is the SNS that controls the climax. So arousal but no climax will be the thing if we want to rebalance the ANS. FYI.
Funny – I was stuck with some obstinate thoughts last night that made it even more impossible to sleep, so I diverted attention by stimulating myself a bit. It really helped (but that’s because I was receptive that night, unfortunately it’s not often). Good point, thanks, will continue practicing 🙂
I have had ME/CFS for 18 years.
Recently I started the Amygdala Retraining program (aka The Gupta Programme). This program had been available for yeas now.
The basic idea is the same: the nervous system is on ‘high alert’, and needs to be calmed, brought back down to a healthy level. This is what the whole program is designed to do – and it works: I’ve already enjoyed significant improvements. It is by far the most promising, helpful, and comprehensive course of treatment that I’ve encountered – and it feels ‘right’. The ongoing support and optional extras (live, interactive web broadcasts for example) are very good.
The program also works on Fibromyalgia and MCS (Multiple Chemical Sensitivities).
Thanks Jonny. Congratulations on your improvement -and after 18 years with ME/CFS!. Please keep us posted on how you’re doing.
Aural acupuncture is a well developed speciality. You can qualify without having any acupuncture training. There is a British professional association which regulates training standards – which are quite rigiorous- In Britain it is routinely used in the treatment of people struggling with the side effects of cancer chemotherapy to prevent nausea and for those being treated for addictions to RELAX. Interesting that it has been used for years for this.
I wrote about my own research and a chart I created further down this thread. I have absolutely no money for anything so am trying to find my own solutions. I believe my chart should be correct and it’s certainly worth testing. I wouldn’t do too many points in one go, I often feel woken up rather than sedated.
Fist we need to know if the ANS is turned on to compensate or is it ‘defect’. This is for me the one million dollar guestion. I think HRV is required to validate ME for at least a subgroup.
Surely it’s a defect, just programming that’s gotten stuck in a rut as suggested in an article on this blog about a Mexican fibromyalgia doctor’s research.
A psychologist recommended an Alpha Stim device for me. It induces alpha brain waves through electrodes attached to the ear lobe. Will this also stimulate the vagus nerve?
I have seen it said that it is hypothesized that the Alpha-Stim stimulates the vagus nerve. However, the vagus nerve has very few nerve endings in the earlobe area, where the Alpha-Stim is supposed to be attached.
In general, the Alpha-Stim works much better than TENS units when used for the same purpose (which is why the Alpha-Stim costs so much more). I tried the method described in this article using the TENS mode of a multi-purpose device that I had. There was a definite calming effect from it, although it didn’t last long.
The next morning, I was doing my regular Alpha-Stim treatment when I thought, Why not try this on the tragus instead of using the TENS unit? So I did.
The results were dramatic – far greater that those of the TENS unit. During the treatment, everything looked brighter and sharper – an effect that Dr. Goldstein has reported his patients saying when he finds the pharmaceutical treatment for them that relieves all symptoms. Certainly, I felt fine during the treatment. I am going to continue using this treatment using the Alpha-Stim, and based on my experience and Dr. Goldstein’s reports, I have high hopes for it.
Steve did this continue to work for you?
Just a word of caution for anyone with a normal TENS machine and wanting to try this.
It is virtually impossible to attach the usual self adhesive pads to the small triangular ear flap. They’re much too big and they stick together rather than to the ear – ear hair doesn’t help if that’s an issue : )
I eventually managed to cut the pads as small as possible and with the help of a plastic clothes peg, some superglue (and an ear hair trim) I got something that works.
Much better though if you can source something purpose made.
PS – Keep the levels low to avoid nearly zapping your ear off like I did!
Good luck!
You can get the same ear clips used in the study at http://www.tenspros.com/Electro-Stim-Ear-Clips-for-Depression-Anxiety-Pain-and-More_p_196.html. To duplicate the results of the study, you should have the “hot” side of the ear clip (the one with the wire going into it) on the outside of the tragus. However, if you can get access to an Alpha-Stim, I have found the results to be much more powerful; please see my post above.
I’m literally killing myself because permanently live on adrenaline with an ineffective digestive system, and through many techniques just can NOT switch off. Would love to try this, any ideas how?
I’m permanently live on adrenaline with an ineffective digestive system, and through many techniques just can NOT switch off. Would love to try this, any ideas how?
Please have a look at my chart for ear acupressure, link provided in a post further down. It’s worth a try!
It’s not “ying.” It’s “yin.”
As a Taoist, I find the use of “ying” along with the symbol of my spiritual practice offensive.
I find you being so easily offended offensive !( actually rather sad). your spiritual practice obviously needs more work so as to avoid being so offended by such small matters.
Cort,
I’m glad that this has helped others. My daughter has CFS, FM, IBS among other issues. She did find a very progressive medical dentist who recommended and installed the P-STIM device for a trial for several weeks. She felt no improvement with this device, and so, upon the doctor’s recommendation, we cancelled the trial. So, even though it didn’t help her, I’m glad it can still help others.
Scotty81
Thanks for passing your daughter’s experience on Scotty – good luck with your daughter 🙂
I found this wee video that shows how to do an ear massage on yourself – you never know, it might have similar benefits.
http://www.acupressure.com/blog/?p=2417
The man in this video doesn’t even touch the area of the ear that we are talking about, the tragus. The tragus is the small raised flap at the front of the ear immediately in front of the ear canal, shown here: http://www.sciencedaily.com/releases/2014/08/140819200211.htm
I love this article – we have some hope! If it works for PwME/CFS, then this could improve many of our symptoms dramatically. I wouldn’t mind waiting for a “cure” if we have a really effective coping tool.
Enjoyed reading all the comments as well. I know someone that is doing HeartMath and she seems to like it. Just took a look at their site and I’m intrigued.
I would love to crowdfund the money needed to get trials on ME/CFS done. Hmmm…..since trials are already being done by the US gov’t for other conditions, maybe they wouldn’t mind throwing a few bucks into an ME/CFS study? Yes I know they are stingy, but at least this is already a proven technique!
There is a technical problem preventing this great post from being pinned on Pinterest.
uh oh – thanks for letting me know.
Here’s a link to the set-up these researchers used (photos):
https://drive.google.com/a/bgi.edu/folderview?id=0B_5idc3rcKskODI0VWlzQ1VZMG8&usp=sharing#
I found the device they used but the crocodile clips are extra. Kind of pricey.
http://www.bodyclock.net/acatalog/V-TENSplus.html?gclid=CLiEy7Pyu8ACFRRhfgodz7UAVthe frequency you need to tune in to to make it work. 200 μs, 30 Hz
Here’s another study that reports similarly promising results using acupressure on the ear.
http://www.ncbi.nlm.nih.gov/pubmed/24865945
Love the hope this article provides. I’ve found that reducing sympathetic nervous system activity is very important in this condition. So far I’ve helped my clients achieve it with meditation, Gupta Amygdala Retraining (disclosure: I’m affiliated with it), pacing, chanting, and more. Love the prospect that some day we might be able to just find a switch or trigger point that calms down the nervous system directly.
I wouldn’t mind being a guinea pig. I found this MicroCare Tech Acupuncture Pen on the web.
http://www.goacupuncture.com/med-alternative-therapies/acupen
Does anyone think that it would work for this purpose?
Lynn
I was interested in auriculotherapy, that’s Chinese ear acupuncture. I couldn’t find a god chart of the right points to turn down the overactive nervous system and balance it, so I put together my own. It should be more or less correct. I’m not quite sure what else to do than just pressing on some of the points for about 5 minutes. It appears that the Vagus nerve covers the whole inner area.
You can also get seeds with herbal properties that you attach to the points, and I will try that too one day. I also have a small acupuncture machine and have tried applying the stimuli onto the points in the ear. I have not experienced any immediate effects but then it’s very hard to tell. I think that with severe ANS dysfunction changes are subtle and long-term. If you want to have a look at my chart you can go to this blog post > http://chronicillnesshealthissues.blogspot.co.uk/2014/08/patience-and-good-faith-are-required.html
Here is an related article (Auricular Acupuncture and Vagal Regulation) that gets quite technical but may be helpful: http://www.hindawi.com/journals/ecam/2012/786839/
Thanks Ellen 🙂
Follow
I have used an alpha stim for 18 years, I will try it on the tragus. I have always fou d it helpful I also practice meditation, guided imagery and hypnosis. LDN was great for pain BUT it seemed to push me over the edge for histamine intolerance to the point of anaphalaxis a few times. I am now only using supplements , at least I have figured out these strange food reactions when for several years I could not connect the dots for reactions to cauliflower, spinach, tomatoes, eggplant, chocolate and to make it even more difficult it does not happen everytime I eat the food. The Low Histamine Chef has a very helpful website. So many different factors involved it becomes overwhelming…… I am sure everyone can relate. I am still working on the methylation pathway but I have not fou d the best person to advise me yet and I am still searching while doing a few supplements and hydroxy B 12 and molybdenum. I have many snps, many homozygous. They explain the histamine Intolerance, DAO, gluten intolerance, anxiety and many other diagnoses throughout my life. I am still hopeful this will all come together and improve. I have improved a great deal already, the ldn induced histamine exacerbation really set me back but watching my diet is helping alot. I also use a sleep CD throughout the night that helps me stay in a deep restful sleep. Healing thoughts to everyone.
There are other reset methods. I’ve been trying a Modified Reset Ice Bath protocol based on an Ayurvedic ice bath protocol given to us by our CFS specialist in the early 1990s. The Ayurvedic ice bath protocol (see below***) did work, but we would have been better off truncating it. It calls for 80 days of graduating ice baths. The PEM from the exertion required to do the ice baths kicked in about day 35-40 so we kind of undid a lot of the good we did by continuing through to the 80th day.
However, we’ve designed a new one that’s a lot less grueling and seems to be working. We got ice caps at Amazon (see below+++) and some gel ice packs. We put the ice packs down my spine and the ice cap & another gel pack on my head. We’re thinking this might reduce the mid-brain swelling/damage? And do a system reset. I have been doing this twice a day, but we’ve purchased more so I can do 3-4 times a day, or 2 packs in succession twice a day. Talk about brain freeze! This is less labor-intensive than the ice baths, and a lot less painful. NB: The Smart Temp HC1302 pads are colder, and stay colder longer than the 11×22 pad or the cranial cap. This route can be more expensive than the TENS units, but the TENS unit reviews at Amazon are not encouraging. My sister & I have tried TENS for other things & it didn’t help.
This and the PEA therapy is pulling me out of the worst CFS crash I have ever had. (I’ve been in bed for over a year, and in a massive amount of pain.) I am doing a number of other supplements as recommended here at Health Rising and other places, but the PEA & ice packs are making the biggest, noticeable strides.
+++ELASTO-GEL HOT AND COLD CRANIAL CAP
http://www.amazon.com/gp/product/B001ED3TSM/ref=wms_ohs_product?ie=UTF8&psc=1
Hot or Cold Pack 11×22,
http://www.amazon.com/gp/product/B001V6POOY/ref=wms_ohs_product?ie=UTF8&psc=1
Smart Temp HC1302 Portable Reusable Hot/Cold Pad
http://www.amazon.com/gp/product/B0009HAZDG/ref=wms_ohs_product?ie=UTF8&psc=1
***If you still want to know how to do the Ayurvedic ice bath protocol calls for 80 days of graduating ice baths:
1. You start out walking in calf-deep 68degreeF water for 10 minutes increasing the time by 5 min increments; then you drop to 66degreeF for 20 min.
2. Then you start lying down in the tub, 10 min @ 68, and graduate as you did for #1
You need someone to help you by adding ice as needed. You’ll need a good digital thermometer that can measure water temp down to 60degreesF. Your helper also must to keep stirring the water to keep the coldest next to your skin.
By the time you reach lying down for 20 min in 66degreesF for 5 days, you should have reached the 40th day of treatment. You will also be swearing a blue streak by then!
Then do the reverse of what you did the first 40 days – another 5 days of 20 min at 66, etc. Make yourself a chart, graduating the times by 5 min increments. Sorry, I don’t have the article or the chart any more.
This procedure was given to us by our CFS Specialist & we were his only patients that did all 80 days. As I said, we thought it would be best for CFS/PEM to collapse it down to 40 days, at least, maybe more.
A few things I left out:
I am also supplementing the ice pack therapy with cold water in the shower. I gradually turn the water colder at the end of my shower, until I am using straight cold water. I have the water running as low as I can, and I run it until numbness and redness set in. I run this cold water along the spots I’ll list below. This only works because I am living in Utah. When we originally did the ice bath therapy, we lived in Phoenix, so turning the water colder in the shower wouldn’t have accomplished much because the tap water isn’t cold, especially in the summer.
I should have included a summary of the areas that are targeted in the ice bath therapy. I’m only hitting some of these areas with the ice packs, but I can hit all of them with the cold water in the shower.
Basically the reset areas include:
from the top of the head down long the back of the head, down the neck and back on either side of the spine, around the base of the neck, armpits, under the breast area, along the back of the arms, and along the inside of the legs. Another way to look at it is everywhere you sweat.
Questions? Post them here.
Wow – very similar to Wim Hoff. How are you doing now? What CFS specialist did you use?
I’ve been bedridden from CFS for 3 years I’m interested to hear how you are doing now?