Last year researchers associated with a company called Integrated Tissue Dynamics (INTiDYN) in New York discovered excessive numbers of nerve fibers in the skin of the hands of a high percentage of Fibromyalgia patients. We covered that study in a blog called “Hands up! A key to the fatigue, pain and sleep problems in Fibromyalgia found?”.
A recent update on their progress from the President and lead researcher at INTiDYN, Frank Rice Ph.D, indicated that they, in collaboration with Frank Ruscetti Ph.D, Sandra Ruscetti Ph.D (formerly of the NIH), and Judy Mikovits, Ph.D (formerly of the NIH and the Whittemore-Peterson Institute) are also studying viruses in Chronic Fatigue Syndrome (ME/CFS).
We took the opportunity of the update to review a recent podcast by Dr. Rice and ask him about his Fibromyalgia and Chronic Fatigue Syndrome research.
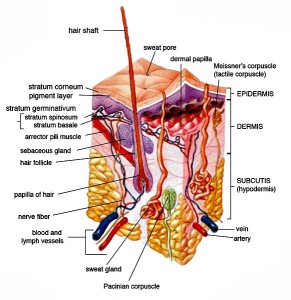
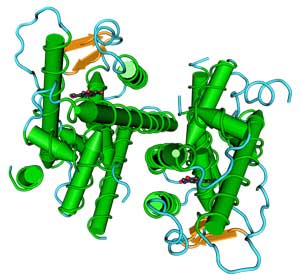
INTiDYN, a for-profit company created in 2008, uses complex tissue analyses to understand the effects of disease, toxins, and drugs on the body. INTiDYN asserts that the integration of the nervous, cardiovascular, immune, and endocrine systems in the skin make it an easy-to-access and cost-effective portal that can help us understand many of the problems happening in the body. Their testing of small biopsies of the skin includes examining the vasculature, nerve innervation, immunohistochemistry, gene expression, and sensory function. Their integrated approach allows them to assess the effects of disease, toxins, and drugs on the morphology, biochemistry, and genomics of tissues.
They used their ability to provide detailed analyses of microvasculature and the vascular sensory and autonomic nerves innervating the skin in their Fibromyalgia study. That study grew out of work they’d done with chronic regional pain syndrome (CRPS) patients.
First we cover a podcast interview with Dr. Rice on Fibromyalgia and his work, and then go to our interview with him. (The podcast with Dr. Rice starts about seven minutes in.)
Dr. Rice’s Podcast
A Personal Experience Flips Rice From Doing Basic Science Research To Doing Applied Research
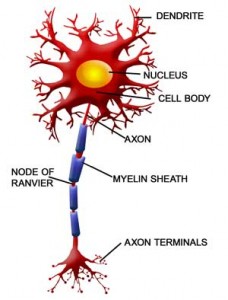
During Dr. Rice’s Ph.D studies in neuroscience at John Hopkins University he became interested in nerve endings in the skin. New methods had been developed that helped them see nerve endings in a way they couldn’t before. He was doing basic science at that point; he was not focused on disease – he was simply determining how the nervous system and how nerve endings in the skin formed. But then after a minor accident a friend with four kids developed complex regional pain syndrome (CRPS), a “horrible condition” he said, he became interested in pain.
How bad does CRPS get? He noted the plight of two CRPS patients in one of his studies. Their CRPS was triggered by rotator cuff surgery and by a broken toe. Their pain became so bad that one’s forearm and the other’s lower leg were amputated. That – and the changes he saw occurring in their skin tissue – stunned him.
Hooking up with another researcher, Howard Fields, he began using techniques never before used in pain research to examine the nerves in the skin of people with a variety of chronic pain conditions.
First came a study on shingles, then one on CRPS, and then last year a Fibromyalgia study. All revealed increased numbers of autonomic nervous system and, in particular, sensory nerves in the skin of the hands of FM patients.
How the Fibromyalgia Study Got Done
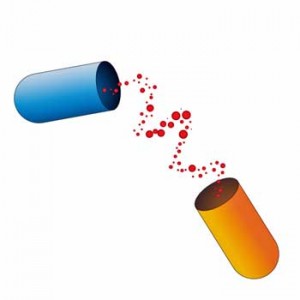
It took three years to get the Fibromyalgia study done. They’d noted that the serotonergic and noradrenergic reuptake inhibitors (SNRI) approved for Fibromyalgia affect the nerve fibers in the skin – in particular, the nerve fibers that converge on and regulate the blood vessels that control the flow of blood to the skin. Two types of sympathetic nerve fibers – one that constricts and one that dilates the blood vessels – are found. Through the production of noradrenaline these nerve fibers also influence that activity of the sensory nerves in the same way that SNRIs are supposed to work. Using that information they got drug company money to help them complete the study.
Study Results

INTiDYN’s sophisticated analyses found ten times the normal levels of nerve fibers in the hand of most FM patients
They found ten times the number of nerve fibers expected surrounding the shunts that regulate blood flows into the hands of people with Fibromyalgia. This suggested blood might be readily flowing into the hands of FM patients but might be having trouble flowing out. The hands, it turns out, serve as blood reservoirs for the rest of the body. They fill up with blood when the body is at rest and send blood to other areas of the body when needed. Their findings suggested that reduced blood flow out of the hands of FM patients could result in low blood volume in, say, their muscles, when they attempted to exercise, thereby causing fatigue and pain. They suggested that sleep, pain, and cognitive issues could also be associated with this problem.
Cautionary Note
He cautioned that it was a small study (24 FM patients) and needs to be validated, but the fact that 75% of the FM patients in the study demonstrated the pathology was striking. That kind of consistent result, he said, does not often happen. He said he was ‘very excited’ about the findings.
Drug Effectiveness Poor in Fibromyalgia and Chronic Pain
One reason for that excitement was the huge need for better pain treatments. He’d received many emails from FM patients thanking him for his work. Lumping in Fibromyalgia with irritable bowel syndrome, CRPS, restless leg syndrome, and other mysterious pain disorders, he noted, “There’s really nothing out there that can consistently and predictably work for a given patient. That’s the frustration in chronic pain.“
The best most pain medications do with disorders for some people with RSD and FM is drop a pain score from eight to about a four – a significant improvement – but since a score of three means you’re in significant pain, they’re still in significant pain. Of course many of these drugs can have severe side effects and work in a limited proportion of patients.
Possible Estrogen Connection
Dr. Rice’s preliminary data, suggesting that under normal conditions women appear to have more of the sensory fibers that become a problem, could help explain the gender imbalance in Fibromyalgia. That suggests hormonal issues could come into play, and preliminary evidence from his lab suggests estrogen may play a role in these nerve changes.
Stress Connection
Because the sympathetic nervous system (SNS) fibers that go to the blood vessels are particularly activated by stress, he noted that it’s possible that stress – triggered centrally in the brain – produces excess activity in the SNS fibers in the skin which then drives the pathological changes in the sensory fibers. Hormonally (estrogen) driven changes in the nerves in the skin could also trigger the stress reaction in the brain.
He noted that trauma (auto accidents) or infection (mononucleosis) or abuse can increase the risk for FM and suggested that the bodies attempt to do stress management may tip it past some threshold (system reset) into disease.
Ketamine Reset Works – Sometimes
When asked about ketamine’s effectiveness in Fibromyalgia, he noted that some patients with severe CRPS have been put into a ketamine-induced coma. When their system comes back or reboots, it appears to reset itself in some patients. In the right patients it can be very effective. Electroshock therapy can do the same thing for depression.
Staying Engaged Helps
“What we do know is that those who refuse to surrender to their pain and engage in activities
despite the pain, those individuals generally fare better in managing their pain.”
He also noted the importance of staying engaged. Rice acknowledged that it’s easy for him to say that, since he’s not the one that’s in pain, and acknowledged the challenge of staying engaged when you’re in pain, but nevertheless asserted that it’s important to stay engaged as much as possible.
By producing pain signals, your body is essentially telling you to stop doing anything, but it’s pretty clear that stopping doing anything makes it worse. Clauw has stated that his FM patients that go on disability tend to get worse.
Pain itself, of course, is very stressful and that stress is going to activate the sympathetic nervous system, causing more pain. (This is a key facet of Dr. Martinez-Lavin’s hypothesis.)
Doing things that get you outside of the pain as much as possible is helpful. It’s simply a management technique to use while researchers uncover the causes of and treatments for pathological pain.
The Dr. Rice Interview
In the interview Dr. Rice reported his team is engaged in a study examining the efficacy of a possible treatment for a similar kind of nerve fiber loss that occurs in chemotherapy patients. (An earlier Health Rising blog Could Cancer Treatment Improve the Treatment of Widspread Pain in Fibromyalgia and Chronic Fatigue Syndrome? revealed that cancer pain may be associated with mitochondrial problems.) Rice’s statement that small fiber nerve loss is sometimes associated with pain – and sometimes not – also suggests there’s more to SFN in FM than we know.
Your team explores a very wide variety of pain issues and you’re also examining the intersection between viruses, immune factors, and chronic fatigue syndrome and fibromyalgia. That seems like quite a new direction for you. Can you say how this study came about?
Actually, we have long held a globalist point of view to our research which involves a multi-component approach to diseases involving peripheral tissues and their nerve supply.
We have a long publication record on a comparative assessment of normal innervation across a variety of species including mice, rats, gerbils, rabbits, cats, ferrets, African naked mole rats, kangaroos, manatees, raccoons, monkeys, humans, and recently whales. The reason for this is that there are variations among different species that help them survive in their particular environments.
Dr. Rice has brought findings from other animals, including Africa mole rats, to inform his work in FM
Consequently, we often find something that is exaggerated in some species that draws our attention to it in others. For example African naked mole rats and manatees have some extremes in their blood vessel innervation that drew our attention to this in humans, which contributed to our discovery of pathology in this innervation in patients with Fibromyalgia.
We also have a long publication record in developmental neurobiology involving the impact of various molecular mutations of trophic factors and signaling molecules in tissue structure and innervation.
In all these studies, we have long taken a comprehensive multi-molecular approach to evaluating all components of the tissue structure and innervation, which, in skin, looks at epidermal cells (keratinocytes), hair follicles, sweat glands, blood vessels, and nerves.
This multispecies, developmental, multi-molecular, and multi-structural approach laid the foundation of our research on disease conditions and caught the interest of clinicians and the pharmaceutical companies.
Therefore, we have adopted a globalist approach of doing research across a variety of diseases where we look for differences and commonalities between diseases, and each disease teaches us something about another. So Chronic Fatigue Syndrome, PTSD, low back pain, etc., are a natural extension of our research.
The skin is particularly interesting in that it is a multifunctional organ that has a convergence of numerous body systems including nervous, vascular, endocrine, integument, connective tissue, and immune. We have mostly focused on the former five, so the recent addition of immune components and related virology was long overdue.
What viral infection and immune system factors are you, in collaboration with the National Cancer Institute, examining in the Chronic Fatigue Syndrome/Fibromyalgia study? Who are you collaborating with in the NCI?
Herpes zoster and retroviruses. The evolving new collaborations are with Drs. Sandra and Francis Ruscetti (who both recently retired from NCI) and a collaborator of theirs, Dr. Judy Mikovits. Their work on the possible contribution of retrovirus to some types of CFS is controversial but nonetheless intriguing and overlaps with some preliminary work that we have been doing with the Center for Functional Genomics here in Rensselaer. They have a new company called MAR consulting.
[Herpes zoster causes shingles. Dr. Rice’s work here and Dr. Pridgen’s work with Fibromyalgia patients both seek to extend the herpesvirus connection in ME/CFS and/or FM beyond the usual herpesvirus suspects: Epstein-Barr Virus, HHV-6, and cytomegalovirus. Herpes zoster infection of the dorsal root and other peripheral ganglia in Chronic Fatigue Syndrome was proposed by Shapiro five years ago. Shapiro noted that varicella-zoster hides out in the dorsal ganglia, can cause severe disease, causes symptoms similar to ME/CFS, and could account for cases of rapid onset. Check out a review of that hypothesis I did at the time “Varicella Zoster Virus, Shingles and ME/CFS – A New Herpesvirus for ME“.]Apparently the altered skin sites you found are only present in the feet and the hands. As laymen we’re struck by the evidence of nerve problems found there and in the other parts of the skin in the small fiber neuropathy studies. One, if I understand this right, involves a buildup of nerves (hands) and the other the destruction of nerves in the skin (small fiber neuropathy). Is there any reason to believe that these two issues are related in some way?
Yes, you understand correctly. The destruction you are referring to is a partial loss of sensory nerve fibers that terminate in the epidermis that was found by Dr. Oaklander’s team at Harvard, and Dr. Claudia Sommer’s team in Wurzburg, Germany. The later study was the better one.
A loss of nerve fibers in the epidermis (referred to a small fiber neuropathy) has been seen in several other pain conditions such as diabetic neuropathy, complex regional pain syndrome, and postherpetic neuropathy which has been described in many studies by others including us.
Nerve fibers in the skin of Fibromyalgia patients may be a) damaged b) hyperactive and/or c) greatly increased depending on where in the body you look
It is a paradoxical finding in that such nerve fibers were assumed to be a potential source of chronic pain, so it was somewhat strange to see them reduced in chronic pain conditions. However, a technique called “microneurography” (which actually records the electrical activity of nerve fibers using thin electrodes inserted through the skin) has revealed that there is excess activity among the remaining nerve fibers that supply the skin.
A group based in Spain headed by Dr. Serra confirmed that such hyperactivity also occurs among nerve fibers in Fibromyalgia patients. However, this technique cannot determine whether the nerve fibers are those whose endings remain in the epidermis or whether they might be the fibers that we found affiliated with blood vessels.
The Oaklander and Sommer studies looked at the epidermal endings in the arms and legs of Fibomyalgia patients. In our study, we also found that the epidermal endings were reduced in the skin over the back of the shoulders in a location of one of the “tender points” that have been used to diagnose Fibromyalgia. This finding did not get much attention in view of our finding of excessive fibers around blood vessels.
However, we did NOT find reduced sensory endings in the epidermis in the skin over the palms of the hands. Although, a reduction of endings in the epidermis has commonly been found in a variety of chronic pain conditions, it is important to note that reductions have also been found in conditions where there is no chronic pain. So a reduction in epidermal endings does not necessarily mean that there will be pain.
Likewise, we have found patients with severe postherpetic neuralgia who do NOT have reduced endings in the epidermis. So having chronic pain does NOT NECESSARILY mean that there is a loss of sensory endings. Oaklander actually provided very little data in her study. Sommer did a much better job showing her data. Importantly, the reduced endings was the AVERAGE over all her patients, but did not occur among many of them.
The “build up of nerves in the hands” that you are referring to was in our study, and refers to excessive nerve fibers associated with the arteriole venule shunts in the hands of the Fibromyalgia patients. This was a much more consistent and a more highly significant finding than the reduction of epidermal endings. We do not know if these two phenomena are related.
Will the expanded ‘hands’ study, if it is funded, examine the role estrogen may play in producing the increased levels of sensory fibers you found? (INTiDYN, in collaboration with the Center of Excellence for Pain Medicine at the University of California at San Diego, applying for a major NIH grant to further explore their FM findings. We should know the grant’s fate soon.)
That is part of the intent. At this point we already have considerable data on normal women and men of comparable age that shows women normally have about twice as much of the sensory fibers affiliated with the blood vessels as men. So there is clearly a gender difference. We suspect that women more often have Fibromyalgia because they start with more sensory fibers than men.
Since there is a gender difference, an obvious question is whether estrogen is involved. We now have preliminary data indicating that the sensory fibers do have a receptor molecule that is known to respond to estrogen. So one of our objectives will be to determine whether men with Fibromyalgia also have excessive sensory fibers affiliated with the blood vessels. So we will be recruiting men with Fibromyalgia as well as more women, and we will be measuring estrogen levels in blood tests.
What factors are you examining in the cancer/chemotherapy/pain study?
We are working on a project with the MD Anderson Cancer Center. It is known that Taxol also causes a reduction of sensory fibers in the epidermis in cancer patients who can also have reduced skin sensation and chronic pain. We are involved in research that attempts to prevent or restore the lost innervation. The specific details are proprietary.
Can you say how the new techniques for examining blood flows in fibromyalgia being developed will enhance your understanding of blood flow issues in FM? (Dr. Rice reported he is, in collaboration in UCSD and Georgetown University, using new techniques to study blood flows in FM.)
One INTiDYN study is examining treatments that might repair the type of nerve problems found in some FM patients
The discovery of the excess innervation affiliated with the AV shunts in the hands led us to an extensive literature search on the normal functional role of the shunts which is where we found indications that they play a key role in thermoregulation and metabolic vasoregulation.
But, there was really nothing that explicitly described the normal functional role of the shunts. What we wrote in the discussion of our research paper and subsequent public summaries are a logical speculation based upon piecing together the available literature.
So first we need to enhance our understanding of blood flow issues in normal individuals to make sure that that the shunts normally work the way we think they do. Next we speculated what would be the functional consequence of the excessive innervation that we found. There was very little on this topic on Fibromyalgia patients in the literature. So once we have a better understanding of the normal function, we will then assess the impact of Fibromyalgia on that function.
An Unusual Company
Dr. Rice and INTiDYN have shown an unusual degree of compassion for a research laboratory. (They cannot recommend treatments, by the way – they are medical researchers, not medical doctors).
Recently they stated, ” … many of you have felt that your particular case is unique and unlike anyone else. That is not entirely true. We want to assure you, that among all the Fibromyalgia patients, there are others who share your story and pain. Regardless of the differences, nearly all of you share the devastating impact that Fibromyalgia has or has had on your quality of life, and the frustration of finding a treatment that works. Some have been fortunate to find improvement and others have not. Unfortunately, that is a major problem with almost EVERY
type of chronic pain condition.”
Finding a Pain Specialist Near You
INTiDYN is also interested in helping FM patients hook up with good pain specialists. To that end they stated: “Many of you are seeking specialists in your local area for Fibromyalgia and other forms of chronic pain. We will work with the NRPC and others to seek their recommendations for top pain specialists over as many areas of the country as they can cover. We will work with them to develop a way to disseminate this information. To do this, if you haven’t already done so, we would appreciate it if you would visit our website and submit your information and where you live on a form that can be found on our home page.”
In their recent update Dr. Rice reiterated:
“In some cases we have been able to make recommendations where you may find a well-regarded pain specialist if you are not already in good hands. Most University-based medical centers are more likely on top of the most up-to-date information. Most of you have sent us information about where you live to help with this, though we haven’t been as systematic as we could about doing this. If you are not sure if you have provided us information about where you live, and you wish to do so, you can register this through a form located on the home page of our website (www.intidyn.com).”
- Check out the original FM study – Hands Up! A Key to the Fatigue, Sleep and Pain in Fibromyalgia Found?










Re Ketamine Reset
I have noticed feeling considerably better, on two occasions, after coming out of a general anaesthetic for an operation, which lasted some days afterwards. My sensation certainly was of the ever-present muscular tension in fibromyalgia having gone. The period of rest in hospital following the operation felt good too.
I have a milder but still noticeable affect after dental anesthesia 🙂 Muscle tension is down – energy is up. Lasts a few hours.
I agree! After any surgeries involving spinal anaesthesia my symptoms have been greatly improved. If only they could find away to make the feeling last….
Ketamine is actually a wonderful drug for many indications and is slowly being studied for more and more indications. It was recently found to be extremely effective at tiny doses for refractory depression in middle aged women. Unfortunately it also holds the stigma of “Special K” so it is little studied.
Greg
It is all very well to say that a person should not go on disability and instead go off to work while realizing that scientists are finding a solution, but I have seen disabled people being under extreme stress and losing their job because they were too ill to perform. Frankly, they made a mistake to go back to work when they were not solid. And what if the answers are not that close on the horizon.
Maybe those who went on disability did not do as well because they were not as well.
Well done Cort.
Agreed and I would note that those were Dr. Clauw’s words not Dr. Rice’s and I think an ‘in general’ probably applies. For me it’s good to ‘stay engaged’ as well – although I’m lucking that I have a sedentary occupation (writing) I can do…
I wonder whether the common sensory experience in fibromyalgia: feeling subjective swelling in the hands (in my case the first knuckle of only one hand) is related to the excess arterio-venous shunts. Dunno.
Great post!
It certainly sounds like it could…Thanks 🙂
Swelling–edema–in the hands can also be a symptom of low blood volume, the subject of other fairly recent posts.
My head is spinning after reading this post. I have an MSc in Public Health and was about to start a PhD when I realised I was no longer able to take in the content of the many research papers I had to read.
I usually love your posts Cort but this one has made me feel even more hopeless. My limited ability to assimilate information may form my opinion. However, it seems to me that what it amounts to is that researchers are looking at so many different possible causes, triggers etc of FM that they are going off at too many tangents.
I feel incredibly grateful for your blogs which usually open a sliver of light at the end of my dark tunnel. Today, I’m left confused and concerned that the researchers will never tie this bowl of possible leads (the size of a planet made of spaghetti) together.
Sorry, you can delete this if you like. My pain level is at 10 today and it’s probably just me!
Thank you for all your hard work Cort.
Christine
🙂
The confusing thing for me is that there are so many positive studies in so many different areas. I have no idea how to put it all together and I’m not even going to try. For now I’m mostly following it piece by piece and hoping the puzzle pieces will start to fit together at some point 🙂
I do also think that FM, like ME/CFS, is probably quite heterogeneous and contains different subsets and we may be seeing those subsets pop up in different studies. I saw that only 30% of people with depression need to have mild inflammation for a study on depression to indicate it’s an inflammatory disorder!
If that’s true then there’s all sorts of room for things to pop up in a heterogeneous disorder like Fibromyalgia.
I’m afraid that our best attempt, Christine, until subtypes (I suspect) are identified, is to throw meds and treatments at ourselves, if not too destructive, and see what sticks. As a psychologist, I, also, find the hypothesized multiple etiologies and treatments for FM to be disheartening and I’m at an 8 as I write. Not to get OT, but that has caused me to start a gradual trial of LDN (earlier topic here) as my best hope.
Back on topic, maybe someone can use Dr. Rice’s info to help me figure out whether learning to change the temperature of one’s hands with biofeedback, a common approach for stress reduction, could be helpful in reducing the nasty FM burning and “bone pain” in my hands. Theoretically, would raising one’s hand blood temperature and thus increasing blood flow reduce pain? Or is the problem with the shunts and blood outflow such that my approach won’t help?
If herpes zoster virus is a player in at least some of the illnesses, is it known what the likely implications should be in receiving the shingles vaccine?
Thanks again, Cort, for pulling all this info. together.
Interesting question. I have no idea – would it inhibit an active virus?
I’ve been dealing with chronic VZV for 5+ years on top of being disabled by ME/CFS for 10+. Early on with VZV I was told that one has to be shingles-free for two years before you can get the shot. I would also have to be (able to be) off of Acyclovir in order to get the shot. So far I have not been able to accomplish either scenario. While I recommend that anyone with ME/CFS who has not had VZV/shingles get a vaccine, there is that chance that getting the shot will create a flare up of ME/CFS or VZV itself because of our underlying immune condition, or at least that of a subset of us.
In case my story helps someone decide about the risks of immunization: VZV began for me in 2009 after receiving both the season flu shot, which I’d received with no trouble in the previous five years of ME/CFS, and the H1N1 shot which was so highly recommended for people with weak immune systems that year. My mother was also dieing in a different region of the county, and at great expense to my health I flew to be with her. Dr, Chia started me on Valtrex but after time had to switch me to Acyclovir because the other anti-herpetic drugs can’t be taken long term because of side effects). Since then I’ve had to remain on the highest/acute dose of Acyclovir (800 mg 5x/day) with the boost of Cimetidine (200 mg, 2x/day) which is both an immune modulator that helps tip us toward a preferreable Th1 response and also helps keep the Acyclovir in the system longer. I still have break-through flare- ups. I have had them everywhere except my right foot, including my eyes and left ear.
Fantastic post, Cort.
I clicked the “donate button” for this one. Nerves and Blood flow again!
Thank you sir 🙂
Cort ,
will you ask Dr.Rice
Does a woman have less pain throughout the body
and do better with Fibromyalgia if she does
use estradiol, hormone therapy post menopausal?
I will mention women but also want to address this for men with fibromyalgia with no incidence of cancer..
Would a man have improved pain levels using Testerone injections
from a urologist or doctor monthly?
I ask this for those that have had the uterus removed and ovaries and no family
incidence of breast cancer
would hormone therapy help with their pain from fibromyalgia?
Which forms of hormones would help and amount per day or week?
would that possibly help with fibromyalgia pain or make it worse to use hormone replacement
such as vagifem?
I have been reading on users comments but never until mentioned in this article
read about an association with hormones..and fibromyalgia.
My fibromyalgia was severe long before I was in menopause at age 30 years old.
Then followed CFS and Multiple chemical sensitivity illness.
My husband has Fibromyalgia , CFS and MCS also.
Sheri
Hi Sheri, I would be very surprised if he would answer as he’s been careful to make it clear that he’s a researcher and not a doctor and therefore is leery about talking directly about treatments.
Those are great questions, though. I have heard there is a strong estrogen- pain connection and hope to be looking into it. As you may remember Broderick’;s model for ME/CFS predicts a hormone-immune interaction has gone awry in ME/CFS and he believes testosterone is protective in ME/CFS.
I believe the peak times for getting FM and ME/CFS are as adolesecents/young adults and in middle age – times of high hormonal changes. This is not to say hormones are the answer but I would be surprised if they’re not part of the picture.
I was wondering the same thing about use of bio identical hormones, specifically estriol and estradiol. If someone knows anything about associations with Fibro pain and the use of hormones, please speak up . I would think it would be helpful to balance the hormones if body is out of sorts due to many factors.
Sheri, what do you attribute to both you and your husband having the same thing? Were you both exposed to some environmental toxins? Or virus?
Thanks,
Carrie
Oh left off one thing. Had anyone tried HCG ( Human chorionic Gonadotropin ) for intractable pain? If so, would you comment on your experience with it? If not, might be something to explore if your a level 10 pain or close to a 10.
Carrie
I know I can’t wear tight rings without worrying that my fingers will swell up to the point that I can’t get them off…the first pain I felt that started to make me think I had something seriously wrong was the shooting pain I felt in my hands when I hit the tips of my fingers on my washer when I missed the door and hit the side instead..also the web between my thumb and first finger on both hands and the bottom knuckle of my thumbs ached terribly..
I’ve always been weaker than my peers, never had much energy, was thought to be lazy by my parents as a child…if I hit my hand on anything, the veins stand up, and the swelling and pain is intense..I always thought that was kind of weird…
I have a list of other symptoms such as post-exertional malaise, breathing disregulation, muscle cramps, tremors, headaches, cataplexy, inability to swallow at times, pain everywhere:muscles, tendons, skin, it feels like the pain goes into my bones, rashes, thin skin, I easily bruise, my skin bleed without much effort, I can’t wear any kind of heel because of the pain in my feet.
Also I have stinky ear wax, that I don’t think is normal, I have had earaches that appeared to not have any cause, disregulation in my ability to keep warm, my feet are always cold even when I burning up, I am always sick, a doctor told me recently that I might have a chronic epstein-barr virus infection, some gland or other on my body is always painful and swollen.
I think my immune system is messed up…but I can’t get any other diagnoses except fibromyalgia..when I mention I might have ME/CFS I get a snicker from the attending be it doctor, NP, etc..my primary told me that I couldn’t have ME/CFS because my tonsils aren’t swollen much of the time..I don’t have tonsils, and she never asked me if I did or not…
I’m beginning to feel like I live in a medical desert. No one in my area appears to know what ME is, and my insurance company doesn’t acknowledge that there is such a thing…so good luck to all of the researchers…
I’m not holding my breath…my honest opinion is that is all a immune related disfunction is caused by the ingredients in vaccines, and the reason that vaccines are supposed to work, by attacking things in our body..unfortunately after they are unleashed in the human body, they are not restrained in what they attack, and the aluminum, thirmerosal, msg(I’m highly allergic to msg, hmm wonder how that happened?), formaldehyde, peanut oil, and etc. causes many of the diseases we suffer from, many beginning in childhood, including cancer and diabetes…but when researchers are getting funding from the gov’t, we will never see any research on just how devastating vaccines are on the human body…look everywhere else but there or get no funding…what IS the catalyst…we can understand the biology of this disease, and how to cope with it, but how do stop it from happening in the first place?..
some might say, oh they don’t use thiremosal(mercury) in vaccines anymore..well hello, I was vaccinated in the 50’s-60’s and I’m still alive..and I’m suffering from what?..immune problems and there are a lot of us out there just like me in their 50’s that are suffering tremendously..oh and by the way, there is still mercury in flu vaccines..so all you pregnant woman line up for you poison and good luck to your babies born with problems as well..and you can be guaranteed that your doctors won’t know what the problem could be…thank you for the article..it was very interesting…
Thanks Jennifer,
you’ve really been through the wringer. That tonsils thing from the doctor – that was a first for me….
These skeptics, these snickerers – the arrogance of the medical community can be amazing..they have a lot to make up for.
Surely these changes to the shunts in the hands are merely a natural adaptation of the body to provide better temperature control when the hypothalamus is no longer functioning properly as we believe is happening in our illnesses. Cold hands when the cortisol levels are high and hot hands when they are low. I really cannot believe that we can store enough blood in our hands to supply all our muscles when needed. Painful hands was one of my first symptoms 30 years ago but I know now that it was caused by trigger points. I haven’t had consistent pain in my hands for 20 years. I get the occasional swollen knuckle and once had a painful thumb but can fix it with trigger point therapy. The trigger points never fully disappear and cause bony nodes to form on the knuckles but the hands remain painless. I don’t believe that taking oestrogen would help matters as my worst overall painful period was when I was oestrogen dominant (premenstrually and then in peri menopause) and taking oestrogen alone only made matters worse. Oestrogen needs to be balanced by an adequate amount of progesterone. Since taking progesterone and then pregnenolone which is the precursor for progesterone, I rarely have widespread pain unless I have a severe flare from severely overdoing things and then is usually no more than a 2 or 3, unless it is a trigger point cascade which is very painful in a localised area but resolves quickly once treated. Fatigue is my biggest problem and I can have plenty of that and be pain free. Oestrogen dominance causes fluid retention which can often be seen in the hands but swelling in the hands can also be caused by thoracic outlet syndrome where trigger points in the scalene muscles in the neck compress blood vessels and impede venous return from the hand.
I forgot to add that I believe my fatigue is caused by widespread latent trigger points that cause an overall weakness.
Regardless of the role of AV shunts in the etiology of fibromyalgia, I’m grateful for an explanation of the effects of SNRIs on body temperature regulation. Patients taking SNRIs and some SSRIs may experience difficulties with temperature regulation, exhibit hyperhidrosis, and are more prone to heat exhaustion. There hasn’t been a credible account of why that happens.
Personally, ever since starting pharmacological treatment for anxiety/depression, when I exercise heavily in heat–such as farm work or trail maintenance–I sweat like a sprinkler and yet still get mild heat exhaustion. Sometimes it’s followed by chills 1-2 hours later. This has been especially problematic on milnacipran. Also my wife, formerly an outdoorsy gal who enjoyed backpacking trips with me, became extremely intolerant of heat while on long-term high doses of venlafaxine. If SNRIs interfere with the normal dynamics of peripheral AV shunts in response to thermal signals, that would explain a lot!