

Pain Reliever, Anti-inflammatory, Microglial and Mast Cell Inhibitor?
“However, a great body of evidence exists for PEA, comprising at least 40 clinical trials in around 6,000 subjects. This body of evidence shows a positive risk/benefit ratio for PEA, warranting much wider use of this compound by the medical community” Hesselink
First isolated from soybean lecithin, egg yolk and peanut meal in 1954, palmitoylethanolamide or PEA is a naturally occurring substance produced in our body, apparently in response to inflammation. A fatty acide amide and nuclear factor, PEA binds to receptors in the nucleus, affecting processes involved in inflammation and chronic pain. PEA is not well known in the U.S., but it’s well-studied with over 350 references in PubMed dating back more than fifty years.
PEA appears to be produced on demand in areas of local inflammation. It’s purpose appears to be to tamp down inflammation/microglial activation where it occurs. For instance, PEA synthesis triggered by glutamate excitotoxicity appears to be an attempt to heal over-stimulated neurons and return them to normal status.
Jan Hesselink, of the Dept. of Pharmacology at the University of Witten/Herdecke in Germany, has produced several review papers on PEA. He has proposed that PEA represents a case study of how the research community ignores effective treatments it does not understand. He asserts that studies from 1957-1992 demonstrated PEA’s effectiveness in the clinic, but it was not until Nobel Laureate Levi-Montalcini’s paper in 1993 demonstrating PEA’s effects in mast cells that PEA began to be taken seriously.
Animal model studies

Human Studies
Hesselink reports PEA may be helpful in autoimmune conditions (influenza pap). Recently PEA was shown to shown to reduce the levels of reperfusion injury occurring during ischemia (low blood flows to the tissues).
Chronic Pain
A Wikipedia article suggests PEA may be most effective in chronic pain disorders such as peripheral neuropathy, chronic regional pain syndrome (CRPS), sciatica, and nerve entrapment. A recent study suggests it could be helpful in fibromyalgia.
Hesselink reports that clinical trials involving over 6,000 people have established PEA’s effectiveness in treating chronic pain and inflammation. Animal models suggest PEA is able to prevent or inhibit two key processes in production of chronic nerve pain: nerve sprouting and dorsal root ganglia activation. cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS).
Why is PEA not better known in the West? PEA appears to have been used in Italy and Spain for quite some time. Interest picked up in the Netherlands and Germany when a Netherlands distributor came on the scene. It’s hardly known in the U.S., although Palmitoylethanolamide For Pain reports that “many people” on the West coast of the U.S. as well as Australia and Canada are using it.
My first glimpse of PEA was in Dr. Younger’s list of possible microglial inhibitors. Hesselink reports that forty PEA clinical trials for chronic pain, alone, have been done, but most have been published in Spanish and Italian medical journals. Most studies published in English journals continue to involve animals or are lab studies, but some studies suggest PEA may be effective in endometriosis and chronic pelvic pain. The few clinical trials currently underway include trials on neuropathic pain, IBS, and post-operative pain.
Microglial Inhibitor
Jarred Younger included PEA in his list of potential microglial inhibitors that might be of use in ME/CFS and FM. Microglial cells surround the neurons and are responsible for the elimination of pathogens that attack them.
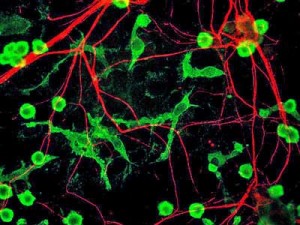
Several German researchers believe PEA may be up to upregulate microglia killing ability without causing inflammation
Not all microglial cells may be the same. Some microglial cells may specialize in phagocytosing invaders while others kill invaders using nitric oxide causing inflammation and potentially killing neurons. Most treatments that appear to turn off inflammation also appear to reduce microglial cells’ ability to clear central nervous system pathogens. Finding a way to support microglial cells that kill invaders without causing inflammation would be very helpful.
Mast Cell Inhibitor
PEA appears to play a similar role with activated mast cells to what it does with over-activated neurons.
Because mast cells are often found near sensory nerve endings, chronic mast cell degranulation – which produces a variety of pro-inflammatory and pain-enhancing substances – could play a role in many pain disorders including pelvic pain, sciatic pain, headache, postsurgical pain, CRPS, fibromyalgia, and ME/CFS. Nerve growth factor – one of the many substances mast cells synthesize, store, and release – produces inflammation and sensitizes sensory neurons.
Studies suggest PEA can reduce mast cell migration and degranulation and can shift them from their activated to their resting states. Hesselink reports that over twenty studies have elucidated PEA’s mast-cell inhibiting effects.
Fibromyalgia
A retrospective study found that PEA may be helpful as an add-on treatment in FM.
COVID-19 and Long COVID
PEA produced a “significant reduction in inflammation” and may help reduce coagulation in COVID-19 patients. A long COVID trial of uncertain rigor found that PEA plus olfactory training help improve the ability to smell in long COVID more than olfactory training alone – suggesting that PEA have have reduced neuroinflammation.
Chronic Regional Pain Syndrome (CRPS)
Hesselink reported a case study of a 13-year CRPS patient who had not responded to numerous prior treatments. Her CRPS had progressed in typical fashion. Following a minor injury (bruised ankle), she experienced pain, swelling, changes in skin color, and severe burning pain that increased over time and then spread to her opposite foot. She subsequently developed allodynia and had trouble walking and sleeping. A second injury to her knee caused CRPS to flare up in her knee, and she became largely wheelchair-bound.
She was given ketamine 10% cream to be applied locally three times daily and PEA, as PeaPure® 400 mg capsules (JP Russell Sciences Ltd, Nicosia, Cyprus) which were taken orally three times daily. For the first ten days, she poured the capsules under her tongue and then took them orally.
After ten days she entered the doctor’s office walking with a cane with the swelling and discoloration in her legs and pain reduced by more than 50%. She continued to improve and soon was able to discard her cane.
Small Fiber Neuropathy
One woman with small fiber neuropathy reported on a pain group site that she was in complete despair until she was able to get off prescription pain drugs by using PEA and alpha lipoic acid. She was still in pain but life was bearable.
MD recommends PEA
Jan Keppel Hesselink MD reports side effects are rare, and he’s found it effective enough to use as a first-line treatment for neuropathic pain. He states he’s used it in 200+ patients.
Side Effects – The only side effects he’s seen are a feeling of heaviness in the story and rarely gastrointestinal upset and diarrhea with the sublingual preparation, probably due to the sorbitol in it. He has not seen any side effects with PeaPure.
Interactions – Hesselink reports no adverse reactions with other commonly used pain relievers such as tramadol, pregabalin, gabapentin, amitriptyline, and duloxetine.
Getting PEA
In 2008 and 2012, PEA became available in Italy and Cyprus under the brand names Normast® (Epitech Group Srl, Milan, Italy) and PeaPure® (JP Russell Science Ltd, Nicosia, Cyprus). Normast is available through www.ergomax.nl. PeaPure is available in the Netherlands via this website.
Medical Food – Normast is classified as “a food for medical purposes”. Because of that designation and a statement that it should be used under a doctor’s care, some people in the U.S. have reported some difficulty in getting it through the mail (i.e., a doctor’s note may be required). Other PEA products produced as nutraceuticals or supplements such as PeaPure apparently don’t encounter this problem.
Nancy Sajben MD reports that a compounding pharmacy in San Diego called PJ’s Prescription Shoppe carries PeaPure shipped over from the Netherlands.
There’s no information available suggesting that one product is better than the other; however, an author of a review article suggests using PeaPure because it is 100% PEA.
Some of the more popular formulations are below.
- Normast compressed tablets contain 600 mg micronized PEA in a magnesium stearate matrix.
- Normast sachets for sublingual use contain 600 mg micronized PEA that is sweetened with 300 mg sorbitol.
- PeaPure is produced in vegetable capsules containing 400 mg micronized PEA only or as a cream via this website.
- Palmitoylethanolamide For Pain states PeaPure contains the most PEA per serving and that a recent review article recommends it. It costs about a dollar a pill (without shipping) or about .80/pill if you buy in larger quantities.
Using PEA
In a discussion on a pain group site, Hesselink suggested using ultra-micronized Normast (sachets) under the tongue for the first ten days to fill up the cells with the compound. After that continue for 6 weeks with 600 mg tablets twice daily.
If pain decreases of more than 30% are not seen, he adds “a period of 10 days with the powder under the tongue” and do not lower the dose for another 6 weeks. Once 50% reductions in pain are seen, he reduces the dose to 300 mg twice daily. He cautioned to “Always use this food for medical purposes in the context of a treatment cycle supervised by your own physician.”
Palmitoylethanolamide For Pain reported that pain relief is sometimes seen within a week but may take up to six to eight weeks.
Resources
Palmitoylethanolamide For Pain is a non-commercial site devoted to spreading the news about PEA and other non-pharmacological products that can help with the pain.
(Health Rising is not associated with any PEA products)
Keep the Information Coming – Support Health Rising







I thought I’d read about PEA online, while researching Phenylalanine. I’ve done a quick search and discovered that PEA is also used as an abbreviation for Phenylethylamine. Don’t get confused and order the wrong substance!
Interesting, Cort. Will ask some naturopath friends on west coast.
Thanks for heads up.
My Dutch is pretty rusty and that Dutch pharmacy site is is, ah, well, all in Dutch…
I wouldn’t mind some of that ketamine 10 % cream mentioned;that is not available in US., is it? Allodynia gets old quickly.
The Dutch website can be converted into English–look at upper right corner on main page, click on the British flag, and instant English!
Creams like this are compounded medications. You need a physician to order it for you to be prepared by a compounding pharmacy. The prescription can simply state Ketamine 10% PLO gel with the usual instructions for amount and instructions for application.
You can get lidocaine creme from Amazon. There are different concentrations, so make sure you get the highest concentration. I’ve also had help from Nectar Balm Bee Venom Cream, also available at Amazon. I’m going to order some PeaPure. I couldn’t find Normast at the website given above, however.
Kim & Kelly Derrick
Im in the uk, you can buy it cheaper here from pharmahorse – as a dog supplement no less haha. But it is human grade. Cheaper than importing from the Netherlands.
Hi Helen are you using the PEA from Pharmahorse for long. It is a lot cheaper that way. I am in Ireland . Thanks, Cathal
Have you benifited from the PEA? And definitely fine to take through your order recommendation? Thanks
Sounds Ike it would be good for what ails me. What is it taken from in the years of 2000’s? Would someone with soy, egg and peanut allergies have a problem? Can you give us a link to the compounding pharmacy in CA?
Issie
http://m02404.wix.com/pjshoppe
I found the link to the place in CA.
Issie
Thanks 🙂
I was about to ask the same question regarding soy allergies… Did you find an answer?
Steve- click on the British flag in the upper right of the Dutch pharmacy and you will get the English version of the website.
this reduces gastrointestinal motility http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1573032/ and reduces intestinal permeability http://www.pa2online.org/abstracts/vol11issue1abst020.pdf so it might help those who have IBS type problems as well as those with pain. However probably not a great idea for anyone who suffers from constipation unless you take the brand with added magnesium.
Soy bean lecithin is part of the methylation protocol, interesting…….
This is exciting, thanks for the write-up, Cort! There are some PEA creams on the marked, are these only for skin problems or a substitute for orally administered capsules?
Hesselink uses them to get the substance into the nerves near the skin better. That suggests it might be good for allodynia? (Although he did use ketamine cream successfully with that CRPS patient.)
Hi Cort
Would LDN and PEA go together ?
Bettina
I don’t know, but thus far PEA, a natural substance and possible microglial de-activator (like LDN) hasn’t had any bad interactions with anything reported. I assume the same would be true with LDN….It sounds like an interesting combo 🙂
LDN and PEA go together, quite good actually for treatment of resistant chronic pain syndromes
Must use LDN with extreme caution. Too much of it, and if using things affecting NMDA receptor (tryptophan, inositol, l-theanine, etc. (I guess whatever affects serotonin)), causes extreme mast cell activation; from experience. Think the 3 mg might have been ok, but son should have been off all NMDA stuff, and pharmacist clearly shown us proper amount of cream.
Sounds like a wonderful product. However with this much research, why has it not been approved in the country? Also anyone using Ketamine products for pain need to know it is an anesthesia drug Vets use for animals and can be very addictive-even or short term use. Most do not use it anymore as very dangerous if dosage is not correct.
I am Gluten intolerant -can I use this product?
Carole
Ketamine is commonly used in anesthesia. As a topical cream it has become popular for pain treatment. Addiction to ketamine is very unlikely, especially in a topical cream! It is certainly not dangerous in this form; debatable that it is dangerous in any form. Much media hype has damaged the reputation of many useful drugs.
Ketamine is a very addictive drug in any form. Some tolerate it better than others.
Vets have pretty much quit using it for that reason.
Do your research.!!!!!
Carole
Nobody has mentioned any fillers containing gluten so I imagine gluten intolerance is not a problem.
Like LDN it’s not a drug – so big pharma is not interested in it – and it’s mainly been researched in Europe. It’s one of those possible treatments that is being used elsewhere but not in the U.S. much yet.
Cort – Question- It was stated that th Sorbitol may be in this product . Anyone that is Gluten Intolerant as I am cannot have any Sorbitol. That goes for Celiac people also.
Would like to ck again the % of Sorbital.
Does sound like a great product.
The VSL#3 is also a medical food for IBS and Gut issues.
It is the only thing that works for me and is a wonderful Probiotic along with Pro 5.
Good write up.
Carole
Didn’t know that about sorbitol and gluten!
If you’re going to try it I would go for the PeaPure – no fillers – it’s all PEA.
There is no sorbitol in PeaPure, neither any other fillers, you can check the certificate of analysis on the website of the producer, it is 100% pure PEA and nothing else, so no worries for gluten allergies etc!
I forgot to add that Big Pharmacy isn’t interested in LDN, as far as I’ve read, because it’s too old / can NOT be patented. They won’t make any money off of it. They’ve taken steps- allegedly- to make it more and more difficult to obtain. Many doctors are nervous and hesitant to write the script for it, for fear of setting off a red flag with government oversight agencies ( who wins- the lowly patient and inexpensive drug- OR- Big Pharma with their big lobbying and campaign bucks ?) that’s a no- brainier
Outstanding research PEA, Cort! I
really enjoyed the article.
My mother has started using PeaPure
yesterday and I hope it can help her with disabling
neuropathic and OA pain.
Thanks again Cort!
I hope it helps. It certainly was interesting to find out about it.. Good luck!
Hi !
I was hoping for clarification about LDN. Im fairly certain that it Is a Drug ( if you’re referring to Low Dose Naltrexone.). I take it here in the US. It requires a prescription- even though it is compounded. That’s because the starting dosage for a Naltrexone pill/ tablet/ capsule….is 50 mg. I only use 3.5 mg- as is common for off-label use ( mostly for pain and autoimmune issues- though it does boost endorphins- thus my mood :). The RX is approved to damage opioid issues. Have I gotten my facts mixed up? It wouldn’t be the 1st time! LOL !
I could not find Normast through http://www.ergomax.nl.
Kim Derrick
I ordered PeaPure from the Netherlands site: http://www.rs4supplements.com/
It came in about 2 weeks. I just started it, so we’ll see how it goes.
Kim
Good luck!
Fantastic News! I have been in extreme pain for about a year (and stuck in bed). There’s been a question as to how much of the pain is CFS related, how much because of degenerative disc disease, and how much might be caused by something like MS. I have been using 3000 mg/day gabapentin and 75 mg/day baclofen (max doses for both). Even then, I was supplementing with small amounts of oxycontin (during the day, especially on days when I got in the shower) or carisoprodol (during the night). I was still having partial seizures (probably not associated with CFS?) related to the neurological symptoms and pain, and other pain related symptoms. I started to notice a slight but noticeable lessening of pain on about day 6 of emptying the PEA capsule under my tongue. The pain level has continued to decrease!!! Wonderful!!! I haven’t used any more oxycontin and I’ve needed less and less carisoprodol. And PEA works without any “fuzziness”, etc. or a prescription! These over-the-counter things are my favorite! No need to try to convince a doctor that I should try it.
I’ve been trying to get in to see the local CFS expert since May 2013. She’s said she “might” be able to see me in 2015. Cort’s Blog has saved me! Her blog has helped me help myself. Cort has earned my meager donation (meager because I am financially strapped and couldn’t afford more). Thanks again, Cort!
I have also been following a modified reset protocol based on an ice bath protocol given to my sister and I by the CFS doctor we had in the early 1990s. (See my comments on Cort’s System Reset blog – http://www.cortjohnson.org/blog/2014/08/29/system-reset-reduce-fight-flight-response/ – search for modified reset ice bath protocol.) That was helping somewhat with the pain, at least during the time that the worst areas were “frozen”, but the PEA gives lasting, consistent improvement. ABSOLUTELY WONDERFUL!!! THANK YOU CORT! AND THANK YOU TO ALL THOSE WHO STUDIED PEA!
Isn’t that something 🙂 Congratulations and continued good luck with it and thanks for passing it on 🙂
I hope people here report on their experiences with this. I wonder if just eating soy or soy lecithin, peanuts and eggs would help? It is interesting to me that I eat these foods regularly–more soy and peanuts and fewer eggs, but still all three. They seem soothing and nourishing.
PEA can be found in all organisms (apart from insects) and all food (including seeds) but the concentration is far too low for it to have robust physiological efficacy; you need between 800-1200 mg/day and (in case of heavy people) even up to 2400 mg /daily. Not to worry PeaPure contains only PEA and no traces of any other compound like peanut, soy, nuts etc.
I’ve now ordered PeaPure capsules from the Netherlands. Really looking forward to try this as PubChem defines palmitoylethanolamide as both an analgesic, an anti-inflammatory agent (non-steroidal), an antiviral agent, and a cannabinoid receptor agonist. I believe this is what I need in addition to my other meds.
http://pubchem.ncbi.nlm.nih.gov/summary/summary.cgi?cid=4671&loc=ec_rcs#x291
To elaborate what PubChem states about palmitoylethanolamide:
1. Analgesics: Compounds capable of relieving pain without the loss of conscioussness.
2. Anti-Inflammatory Agents, Non-Steroidal: Anti-inflammatory agents that are non-steroidal in nature. In addition to anti-inflammatory actions, they have analgesic, antipyretic, and platelet-inhibitory actions. They act by blocking the synthesis of prostaglandins by inhibiting cyclooxygenase, which converts arachidonic acid to cyclic endoperoxides, precursors of prostaglandins. Inhibition of prostaglandin synthesis accounts for their analgesic, antipyretic, and platelet-inhibitory actions; other mechanisms may contribute to their anti-inflammatory effects.
3. Antiviral Agents: Agents used in the prophylaxis or therapy of virus diseases. Some of the ways they may act include preventing viral replication by inhibiting viral DNA polymerase; binding to specific cell-surface receptors and inhibiting viral penetration or uncoating; inhibiting viral protein synthesis; or blocking late stages of virus assembly.
4. Cannabinoid Receptor Agonists: Compounds that interact with and stimulate the activity of cannabinoid receptors.
Isn’t this exactly what we need?
In the past one thought PEA is an endocannabinoid, but now we know it is not. It is a lipid messenger and it goes to the central PPAR receptor, were it turns the receptor on; as a result all overacting inflammatory genes are turned off…it is a paradigm shift because one never thought food stuff can turn on genes….
Thanks Robert…
Thank you!!!
PEA sounds interesting, but you would want to be careful in any ME patient who is salicylate sensitive or has glutathione issues. I think we often have too much COX-2 activity, but in the wrong places. If you shut it down you will not only reduce inflammation, but shut down essential fatty acid metabolism … which produces hormones essential to life. Care would be required in this subgroup of patients. Having said that, and being in this subgroup, I would still be interested in trying this, with care.
Always start slowly…Thanks for the warning…
Alex, how did you fare with the PEA. I’m quite keen to try it for CFS/FM but have salicylate intolerances and I suspect poor fatty acid metabolism as my skin is so dry.
Alex, PEA has been extensively used in the netherlands for treating ME and CFS and no issues arose…even people as sensitive as u describe should have no issues since PEA is a modulator and does not shut down systems!
Good to hear – thanks Peter.
Hi Peter,when you say modulator. Do you know if it could down regulate overactive Th2 cells?
I wish to buy micronized palmitoylethanolamide (PEA).
I am a retired pharmacist from Victoria, Australia.
Please advise how I can purchase same.
Thank you.
Mr Chris. Bridgland.
I a pharmacist/naturopath in Perth. I make PEA capsules for a lot of my patients.
I make 400mg capsules. 30,50 or 100 capsules can be posted to you.
Hi – you can also get PEA and PEA Skin Cream at the Caboolture Super Clinic Pharmacy in Brisbane. There is a good collection of research articles on their info page https://caboolturesuperclinic.com.au/compounding-pharmacy-caboolture-2/palmitoylethanolamide-pea-supplement-for-chronic-pain-and-inflammation/
Just wanted to add my experience here. After reading this article I decided to give this a try with my 16 year-old daughter. She has ME/CFS with a lot of body pain, particularly mid-back pain, on exertion. I love things like this that have a ton of potential and very few downsides. We live in the UK, so ordered Normast from an Italian pharmacy via Amazon UK. She’s been taking 1200 mg/day for a little over a month now and I have to say the results have been impressive. I haven’t heard her complain of back pain for at least two weeks now. We’ve had some days where she’s really pushed herself activitywise. In the past this would have meant a lot of pain over the following days, but she’s barely complaining of pain at all. Fatigue, yes, but not the pain. I am so amazed at the effectiveness of this and so sad that this is not more widely used in the US, UK and elsewhere. What a shame.
I will say that there has been one side effect, which is an increase in acne. I did a little digging and came across this paper:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2757311/
Seems to be saying that anything that upregulates the endocannabanoid system in the skin (don’t know if I’m saying this right) would exacerbate acne. PEA would upregulate this. Relatively small price to pay for pain relief, but thought I’d mention as everything says no side effects.
Since the idea with PEA is that once you achieve the pain reduction you start to taper the dose, this unwanted side effect should decrease soon. We’re going to lower the dose today. I guess a drug/supplement where you take less and less the better it works is never going to win over pharmaceutical companies even if it could be patented, but I think it’s one of the best things about this.
Anyway, thank you Cort, as ever, for highlighting potential treatments from all corners of the globe. Your piece on the Perrin technique within the last year convinced us to give that a try, as well, (very lucky to have a practitioner very close by) and that’s been another really important part of daughter’s road to recovery. Yet another treatment with no side effects and a lot of potential to help. Thank you thank you!!
Wow. Great to hear. I’ve got to give it a try?. Thanks for sharing your experience
IS THIS GOOD FOR HAND AND FOOD NUMBNESS CAUSED FROM A SPINAL COURD INJURY FROM BIKE ACCIDENT
I have been using Palmetoylethanolamide for the last 2,5 years and would not go without it. I take 800 mg twice daily and when get PEM I take 800 mg 3 or 4 times until I get better.
If you ask the supplier to give you the complete ingredients list they will.
I have chosen PUREPEA as it has no additives and it is made by extraction of green peas.
In the US available on
https://www.amazon.com/vegetable-Palmitoylethanolamid-Clean-Foods-certified/dp/B01NCAJP2S
I Europe I buy from Naturheilpraxis-Bedarf. If you contact the shop you they write english and you can pay using PayPal. If you like the product they have a bay 7 pay for 6 offer.
https://www.nhp-bedarf.de/de/PEA.
Is this still a valid treatment? I have had this tab open to read the article for some months, and today I am finding that few to none of the links work in trying to obtain a source of PEA to try.
Yes it is, Lori Joslyn. There are a few places that sell it now. Nootropics depot (on Amazon or their website), peacure.com is another.
Clarification on side effects of PEA. I don’t understand this… “The only side effects he’s seen are a feeling of heaviness in the story.” Thanks!
I took one dose of 400 mg of PEA in veggie caps and experienced severe pain in my stomach, migraine, explosive diarrhea (once) and nausea only a few hours after taking the first dose with my lunch (and I drank plenty of water too). I’ve been suffering for 4 days of terrible stomach pain. Anyone else can relate? Hopefully, the pain will resolve soon. I didn’t take a second dose….