

This is the second blog to focus on Miller’s recent basal ganglia findings in Chronic Fatigue Syndrome. First a quick review of the first blog.
Review
“Recent evidence indicates that the basal ganglia and dopamine (DA) may be primary targets of inflammatory cytokines leading to cytokine-induced behavioral changes.” – Miller
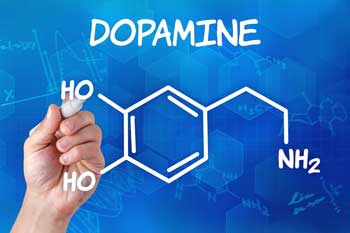
Reduced dopamine levels showed up big time in Miller’s study. Now we take a look at why they’re low and possibly how to fix them.
Reduced activity in the basal ganglia during a reward game was associated with fatigue in people with Chronic Fatigue Syndrome (ME/CFS). A similar pattern found in people with hepatitis C who have been given the interferon alpha (IFN-a) cytokine suggests immune activation may be driving basal ganglia problems, since the lack of reward and the fatigue is present in both groups. Studies suggest that reduced dopamine inputs from the striatum may cause the reduced activation of the basal ganglia. The basal ganglia problems in ME/CFS suggest dopamine may be reduced brain-wide.
Perhaps the most intriguing outcome of the Miller ME/CFS basal ganglia study is the idea dopamine production may be causing the brain to over-respond to inflammatory signals resulting in increased fatigue and other symptoms associated with “sickness behavior”. This suggests that mild elevations in inflammation found in many people with Chronic Fatigue Syndrome could be having exaggerated effects.
Now we turn to possible causes of the reduced dopamine in ME/CFS, and we are given evidence of reduced dopamine in Fibromyalgia (FM) as well.
The Fibromyalgia Connection ?
We may not be just talking about ME/CFS here. Several recent studies suggest an immune component may be present in Fibromyalgia, and FM often begins with a viral trigger. Pridgen, we’ve observed, believes an active herpesvirus infection causes FM.
Several studies implicate reduced dopamine in Fibromyalgia, including a recent fMRI study which found reduced levels of reward. The reduced reward was associated with reductions in activity in an area of the brain with high dopamine levels. (One hypothesis proposes brain reward circuit functioning plays an important role in determining pain sensitivity.)
Reduced dopamine functioning could also help to explain the poor responsiveness to opiates often found in FM. Reduced response in the regions of the brain associated with ‘reward’ is common in people who don’t get results from opiates. Opiates do help some FM patients, but in general their effects are blunted in FM.
Another study suggested reduced dopamine metabolism in FM was associated with reduced brain grey matter. A small PET scan study found reduced brain dopamine uptake, and one study suggests reduced dopamine levels are associated with increased pain sensitivity in FM.
Blocked Dopamine Synthesis – Focus on BH4
“It is reasonable to assume that slight elevations in Phen or the Phen/Tyr [phenylamine/tyrosine] ratio during chronic immune activation may confer physiological relevance, particularly in terms of predicting increased oxidative stress, behavioral alterations, and decreased dopamine synthesis.” – Miller
It all goes back to inflammation. Inflammatory cytokines and oxidative stress reduce the production of an enzyme co-factor called tetrahydrobiopterin (BH4) that converts phenylalanine to tyrosine, the amino acid precursor to dopamine. The low levels of dopamine found in the brains of ME/CFS patients could all start with inflammation or oxidative stress whacking the BH4 enzyme and thus reducing the amino acid dopamine is made from – tyrosine.
The degree to which tyrosine is available for transformation into dopamine can be measured in several ways in both the blood and cerebral spinal fluid.

Miller proposed a simple blood test (phenyalamine/tyrosine) could pick out people with reduced brain dopamine synthesis
BH4 is also an essential cofactor for the endothelial NOS (eNOS) enzyme at work in our blood vessels. During times when we have low BH4 levels, eNOS switches from producing NO to generating oxygen-derived free radicals that increase oxidative stress. BH4 is currently being evaluated in cardiovascular disorders.
Miller’s finding that increased levels of phenylalanine and reduced levels of tyrosine in the blood and the spinal fluid were associated with increased fatigue (but not depression) in hepatitis C patients treated with IFN-a suggested that immune activation and oxidative stress could be knocking down dopamine production in those patients and possibly in ME/CFS patients.
Miller proposed that a reduced phenylalanine/tyrosine ratio in the blood could be a marker of reduced dopamine production in the brain.
Traditional Dopamine Enhancing Drugs Fail
Stimulants such as amphetamines and dopamine reuptake inhibitors which increase dopamine release may be ineffective because innate immune activation is blocking dopamine synthesis.
Increasing dopamine synthesis (not enhancing dopamine release) is a more likely target in disorders like ME/CFS, and it’s to that we turn next.
Increasing Dopamine Synthesis
Directly Boosting Dopamine Synthesis
Since BH4 appears to get hit hard by oxidative stress and cytokines in these disorders, and BH4 converts phenylalanine to tyrosine – which gets transformed into dopamine – Miller first focuses in increasing BH4 levels.
Sapropterin (Kuvan), a synthetic form of BH4 approved by the FDA to treat phenylketonuria (PKU) is a possibility. PKU, which refers to high phenylalanine levels in the blood, can be associated with significant brain damage, mental retardation, seizures, and behavioral alterations.
Supplements that impact BH4 synthesis/regeneration such as folic acid, L-methylfolate, and S-adenosyl-methionine (SAMe) are another possibility, and with them we’ve entered into the complex and fascinating world of methylation – which we will leave for another blog. It’s intriguing, however, to see this subject, which has been of great interest in ME/CFS, suddenly show up as a treatment possibility for dopamine-induced basal ganglia dysfunction, fatigue, and motor slowness in ME/CFS.
Enhancing Dopamine Synthesis By Blocking Oxidative Stress
The Kynurenine pathway – Miller noted the kynurenine pathway in his section on oxidative stress. Mady Hornig, who in a discussion with me called the kynurenine pathway her ‘favorite pathway’, is deeply interested in this pathway a. Some evidence suggests abnormalities in this pathway may be implicated in some Fibromyalgia and ME/CFS patients. A kynurenine gene polymorphism predicts the sudden appearance of depression in hepatitis patients treated with IFN-a.
In any case the high rates of oxidative stress invariably found in ME/CFS studies suggest that reducing oxidative stress could be a viable means of reversing the problems with dopamine synthesis present in some people with ME/CFS.
Enhancing Dopamine Synthesis By Blocking Immune Activation
Etanercept (Enbrel) is a tumor necrosis factor blocker used to treat a variety of inflammatory disorders. It’s possible a number of different drugs could be used to reduce an immune activation that is whacking dopamine production in some people with ME/CFS.
Drugs Effecting Dopamine Receptors
Drugs that can stimulate dopamine receptors (e.g. pramipexole, levodopa) fall into the experimental category but might be helpful as well.
Inflammation, BH4, Depression (and ME/CFS and FM)
It’s not surprising given the stresses associated with Fibromyalgia and Chronic Fatigue Syndrome that depression is common, but is it all due to psychological stress? Much of Miller’s career has been spent exploring the inflammatory aspects of depression. We’ve seen that a significant proportion of hepatitis C patients treated with the IFN-a immune factor suffer from severe fatigue, and some of those become depressed. Could a substantial portion of the depression found in ME/CFS be immune-mediated? Let’s take a brief look at inflammation and depression.
It appears that inflammation either augments or causes depression in about a third of depressed patients. We’ve just seen that low BH4 levels are associated with inflammation-caused reductions in dopamine and, ultimately, fatigue and depression in hepatitis C patients.
That’s an intriguing finding for Miller’s inflammation/depression work given that low serum levels of folate – a factor in BH4 production – have been associated with increased risk of depression and a poor response or even a non-response to antidepressants.
- See a recent blog on folic acid and ME/CFS – The Folic Acid Controversy, MTHFR and Chronic Fatigue Syndrome
If you’re depressed and not doing well on anti-depressants note that the inflammation-associated depression group tends to respond poorly to antidepressants.
Miller notes that L-methylfolate (marketed as Deplin and Zervalx), folic acid, and folinic acid (Leucovorin) have been shown to enhance antidepressant therapy, and that SAMe, in a placebo-controlled, double-blinded trial increased remission rates and symptoms significantly.
RNase L Returns – After a Decade or So
The fact that not all hepatitis C patients given IFN-a become highly fatigued indicates some other factor in combination with IFN-a is needed to produce the fatigue, motor slowing, and similar symptoms found in that group. Could that factor also be present in ME/CFS patients?
Miller’s earlier gene expression study suggests it might be. The only difference in the gene expression between the fatigued and non-fatigued patients receiving IFN-a was, remarkably, a gene associated with Ribonuclease L, a.k.a. RNase L.
Years after study on RNase L stopped in ME/CFS it shows up in IFN-a treated hepatitis patients with fatigue (This is interferon)
This is an IFN-associated enzyme that was implicated in ME/CFS well over a decade ago. RNase L and the IFN pathway was the cat’s meow for a time in ME/CFS, and an entire book by Englebienne and De Meirleir was devoted to the implications of IFN pathway problems in this disorder. Interest faded over time, and it has not been studied in ME/CFS for years.
Now the differences in gene expression of that very enzyme appears to predict who comes down with ME/CFS – at least for a time – in hepatitis C patients who are given IFN-a. When asked, Miller stated that his findings were consistent with what was seen in the RNase L findings of a decade or so ago. They suggested an upregulated IFN system could very well be associated with the basal ganglia problems found in ME/CFS.
That makes the IFN findings in FM all the more interesting. A gene expression study that strongly implicated the interferon pathway in Fibromyalgia suggests, at least to me, that a similar pattern of immune (IFN) activation, dopamine reduction, and increased fatigue and pain could prevail in FM as well. The study found that interferon signaling and interferon regulatory pathway genes were much more highly expressed in FM patients with high levels of pain (Lukahatei, et al.).
A Talk with Andrew Miller
Giving endotoxin to healthy controls reduces basal ganglia functioning. Giving IFN-a to hepatitis C patients makes many of them fatigued and depressed and causes the same kind of basal ganglia dysfunction that seen in ME/CFS. What would be your guess as to the cause of the basal ganglia problems in ME/CFS?
Increased inflammation as a consequence of chronic viral infection (IFN-alpha is an anti-viral cytokine) and/or chronic stress and/or issues related to diet or obesity, all of which lead to inflammation.

Andrew Miller has no ongoing ME/CFS studies but believes his basal ganglia work will help a subset of patients
from a chronic viral infection and in another could be associated with stress.
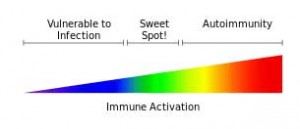
Any of these contribute to a central nervous system that has become unduly responsive to inflammation; i.e., a CNS which starts pumping out factors that cause sickness behavior at the drop of a hat, so to speak.]
That said, I think that if someone is chronically fatigued, they should get their inflammation level checked (CRP) and if it is high (>3 mg/L), they should begin a lifestyle plan of diet and graded exercise as well as possibly meditation to get it down. Anti-inflammatories might also be used, but I am not confident in that statement until I have done more research.
“Not specifically, but we are working hard to understand how we can treat the basal ganglia problem … which will have direct relevance to some CFS patients. CFS is a heterogeneous disorder, so it will help to get a biomarker that we can then apply to the CFS population to determine who might benefit from our therapies. … This will be a win for CFS.”
Miller was careful to point out in the study that, even though the study was positive, not everyone in the study had basal ganglia dysfunction. Clearly, those patients with basal ganglia dysfunction – and it is likely a substantial number – may very well benefit at some point from Miller’s and other’s long and now quite extensive research into the relationship between basal ganglia dysfunction and inflammation, immune activation, and fatigue.
- See Part I : Unrewarding Reward: The Basal Ganglia, Inflammation and Fatigue In Chronic Fatigue Syndrome
________________________
Tyrosine Metabolism During Interferon-alpha Administration: Association with Fatigue and CSF Dopamine Concentrations. Jennifer C. Felger 1,2,*, Li Li 3, Paul J. Marvar 1, Bobbi J. Woolwine 1,2, David G. Harrison 4,Charles L. Raison 5, and Andrew H. Miller. Brain Behav Immun. 2013 July ; 31: 153–160. doi:10.1016/j.bbi.2012.10.010








This is interesting but I can’t quite see how I fit into it! I take phenylalanine as a supplement.
I am relatively high-functioning. I managed to keep working until I was about 53, only diagnosed when I was 40 but probably had CFS since hepatitis at age 7. (I know I had all the symptoms in secondary school and didn’t know what they were.)
A few years ago I was aware that chocolate made me feel better. I was up to 150g per day. I was tested by applied kinesiology and that confirmed that chocolate helped. Further testing found that it was the phenylalanine in it that I needed.
I now take this as a supplement. Within a short time I stopped craving chocolate. I also felt much better in myself and had more energy.
How does this fit in with the theory above?
Great! So glad to see someone finally looking at the kynurenine pathway again. Also one of my favorite pathways. I was asking my CFS doc about Rx BH4 6 yrs ago but its not available in the US as far as I know. Dr. Yasko and Dr. Pall also talk frequently about supplemental BH4 due to its role in the methylation pathway. It’s available through homeopathic preparations or Royal Jelly which contains trace amounts. I take Royal Jelly daily for BH4–it was a boon at first for improving overall symptoms. Ill advised for those allergic to bees, however.
Another kynurenine pathway fan 🙂
Interesting Cort, that could link in my restless leg which is possible caused by low dopamine as well as LDN being the only drug that gives me relief for restless leg?
Justin, have you had your ferritin (not iron) blood levels checked? Dr. Teitlebaum told me to have mine checked and they were very low (my iron levels were normal). I took iron supplements to raise my ferritin levels and as long as my ferritin levels were up my restless legs stop being restless ( I have had restless legs my entire life but they got much worse after getting CFS). Hope this info will help you or others.
Could you provide more detail concerning the recommendations for diet, graded exercise and possibly meditation for people whose inflammation level is high? Is there a direct connection between these measures and lowering inflammation? How does this work?
I don’t know what Dr. Miller was referring to. For me I can see the diet connection as gut issues can increase inflammation. I can see the meditation aspect as it could slow down the fight/flight system. I don’t get the exercise connection…
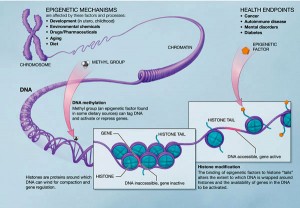
A good bit of the immune system lies in the gut. As does some neurotransmitters – like serotonin. One known help for those with MS is avoiding all dairy. Dairy and gluten are two things that may aggravate an immune system problem for some. Diet plays a key role in our health. It’s one of the hardest things to change. But the one thing we can have complete control over. It’s one thing we usually learn from our parents and adopt from our surroundings. The habits can be passed on for generations and contribute to epigenetic changes that could potentially affect our families for years to come. If we can change the bad habits we’ve picked up, the future people in our family may not have to suffer with those passed on flaws as badly. We need to take control of the one thing we can control and see where it takes us. Looking for a magic pill may never come. But we may not need it if we get our bodies working with the best fuels possible.
Issie
Answer your question about how chocolate relates to the article above I believe the problem of fatigue is related to the inability to produce enough Dopamine. Perhaps in your case, supplementing with phenylalanine is allowing your body to make more dopamine decreasing your fatigue. How much are you taking?
I take 2,000 mg per day. (That’s 4 x 500 mg.) I’ve read that you get serious problems if you take about 6-7,000, so I figure I’m taking a safe amount. I started with 6 tablets, cut down to 3, but when I tried 2 tablets, I started craving chocolate again. I upped it to 4 and I feel much better.
Since taking this, I now spontaneously smile and even laugh out loud occasionally. I hadn’t done that for years! At the start of this year I even managed to walk 2 miles a day. However, once the weather got humid, that added too much strain to my system and I couldn’t cope with that exercise level.
What I’m finding is that I can feel good and I am content in myself at a low level of activity. I can add in more activity when I need to, as long as I am prepared to put up with feeling lousy and ‘depressed’ for a couple of days.
I suspect I’m on these tablets for life. I wonder how fast-acting they are. Perhaps I could take a couple more on the days when I am doing more. (Hey, they’re cheaper than all the chocolate I used to eat.)
I’m beginning to suspect that for some reason my body is not getting enough phenylalanine from my food. I certainly eat the right foods for it, but perhaps my system is not isolating it. That may be why I need to provide extra in tablet form.
Hey Diane, I’ve been in the Alternative health field + practice Applied Kinesiology since the ’80s. I found years before my FM diagnosis (’08) that I am sensitive to “phenols”. I always tested well for tyrosine and Not phenylalanine. I’ve read that many FMers don’t convert phenylalanine well. Maybe try l-tyrosine instead. Since I started taking it my pain level went down 70%! I wouldn’t have been able to wean off opioids in order to start LDN without it! NOTE: the Best (AK tested) N-Acetyl L-Tyrosine = Swanson Brand- $6 for 60- 350mg caps (often on BoGo!) I only need to take 2 (or 700mg) N-Acetyl L-Tyrosine, where I needed to take 4 (or 2000mg)”regular” (free-form amino acid) tyrosine. Hope this can save you some $! NOTE #2: Please make ur 1st order w/my link: We’ll both will get a $5 coupon!
I was recently reading that 2/3 of CFS patents responded positively to anti-virals, at least in one study reported, and positively in varying degrees in others. I would be curious if anyone has any idea how a viral infection in the nerve tissue could reduce dopamine levels. Certainly increasing inflammation and cytokine levels makes intuitive sense.
And just a comment: If CFS was not caused by a virus, wouldn’t the percentage of subjects showing improvement from anti-virals be close to zero?
I would seriously like a link to the study you are talking about. Our personal theory for why anti-virals help is: ME/CFS is an autoimmune disease. Anti-virals calm the autoimmune reaction being generated by the immune system, thereby slowing or eliminating the autoimmune attack and symptoms.
We were given acyclovir in the early 1990s, and it helped. We haven’t had any luck getting subsequent doctors to prescribe it. That’s why I’d like the link. We’re trying to collect evidence to get another subscription for acyclovir or amantedine.
My sister & I have had CFS since we were toddlers (at least), giving us over 100 years of data and experience in the field. We’ve become a CFS research institute, in a way.
To the CFS Research Institute 🙂 – http://www.ncbi.nlm.nih.gov/pubmed/24858857
Be sure to check out the first blog in the series.
Dr. Henderson recommends Valtrex, as it has few side effects.
It’s an open question as to what, if any, virus is involved. Van Elzakker was supposedly going to investigate viral presence in the nervous tissue as he theorized that the vagus nerve was infected. Since the disease started as a flu-like illness and subsequently stimulates the immune system, often permanently, I tend to go with the virus theory. I thought I read that German researchers suspected EBV.
It could do it by tweaking BH4 through increased inflammation and oxidative stress. That could reduce dopamine which in turn may render your CNS more susceptible to the effects of inflammation and cause increased fatigue, reduced reward, etc.
Having my first wrong DX being Parkinson disease – because of my POTS tremor we tried the meds which ups dopamine. We first tried Sinemit and later Wellbutrin. Both a huge disaster. Not only did it not help it made me so much worse. To the point of the doctor thinking I had Multiple System Atrophy and Lewey Body Dementia. It was one of the worst directions we went. So please be careful. If dopamine is low there could be a compensatory reaction. But increasing dopamine could cause other issues. I learned the hard way.
Still thinking correcting mutations in methylation may be of benefit. I do have mutations on BH4. I also have issues with CBS which has to do with breakdown of sulfate. You have to address things in proper order before you jump in and focus on one thing. It may require a diet change to get the body’s cycle going in the right direction before you can be functioning optimally. Addressing inflammation with diet and supplements another good direction. Just be aware that even alternative supplements are a concentrated form and at that point becomes a medicine. It might help one thing but create another issue if not all properties and health issues are not looked at. Especially if there are generic mutations that are causing dysfunction. We are all so complex.
Issie
Indeed. Miller suggests doing the phenylaline/tyrosine blood test first and emphasizes diet and meditation – some very simple ways of getting inflammation under at least somewhat control. He also notes his findings apply to a subset of patients – not all of them -something ALWAYS to keep in mind when considering treatments.
Thanks for the cautionary note.
Hello Issie, I have a few similar issues like you mentioned – high phenylalanin, low tyrosine, low BH4, Sulfate issues etc. Have you been able to overcome the low dopamine, bh4 and sulfate issues? Thanks, racerbiker
Some of dopamine’s notable functions are in memory, cognition, sleep, inhibition of prolactin, (prolactin is an immune system stimulator) mood, pain, learning and control of nausea. Every morning, I restore my depleted dopamine stores with a small dab of powder from a capsule of tyrosine, along with some other supplements and a cup of coffee. Through trial and error, I have found that this small dose of tyrosine is all I need and I never take a whole capsule. I have discovered as with most medications, supplements etc, that I require much smaller doses than the average person. Whether, this has something to do with brain structure/chemistry and if this difference somehow contributed to my development of ME/CFS in the first place, I’m not sure. All I know is that I immediately feel better, less anxious, less fatigued and less malaise after I take my tiny dose of tyrosine in the morning. I feel that I am no longer running-on-empty; my small dopamine stores have been replenished. I now have something to work with if I come under stress, if I am doing something strenuous, or if I take medications that require a dopamine source.
Im the same way. Small amounts are definitely better for me. I tried tyrosine years ago, but not a tiny amount. A whole cap was too much. Maybe a smaller amount would be enough. (Very small amounts of other minerals and supplements are used to help the methylation pathways. Lithium is used to help b12 and folate go into the cells. http://chronicdiseaserecovery.wordpress.com/2013/04/30/mthfr-and-lithium/ It also stimulates tyrosine and inhibits glutamate excitotoxicity – according to Dr. Mullan in the above report. )
Some of us with HyperPOTS figured out that even though we have high NE (norepinephrine) levels, when we need a “good” day, pseudoephedrine seems to work for a short time. (This is thought to increase NE. It is believed NE can both vasodilate and vasoconstrict in different parts of the body. ) Pseudoephedrine seems to become ineffective in about three days of use to modify our POTS symptoms. We feel that maybe our NE response is a compensatory response because of our autonomic dysfunction. NE is synthesized from dopamine. All are converted from tyrosine. Both NE and dopamine act as neuromodulators in a the central nervous system and play a role in blood circulation.
Issie
I think I’m going to try tyrosine…Thanks for that suggestion. Every little bit helps…
http://www.helpmychronicpain.com/blog/bid/115600/Why-Tyrosine-Can-Ruin-Your-Chances-With-Hypothyroid-Symptoms
Something to keep in mind with tyrosine and also shows what I earlier said in regard to something helping one thing but potentially creating other issues. Tyrosine affects thyroid function.
Issie
Cort, maybe you could ask Dr Miller or others in this line of research why they don’t recommend supplementing with tyrosine as opposed to trying to raise BH4 or using a reuptake inhibitor? It seems like this would bypass the problem of converting phenylalanine to tyrosine?
http://www.progressivehealth.com/thyroid-l-tyrosine.htm
This tells a little bit of what side effects too much tyrosine may cause. Some use kelp to up tyrosine and increase their iodine. My being a vegan, kelp is my choice and necessary for iodine. That with B12 and Vit D3 are things my doc has me supplement.
Issie
Really interesting. My health issues predated a year on interferon alpha/ribavirin for Hep C, but I think it did definitely permanently skew my immune response. I also think the emerging cohort of post-interferon patients have a lot of useful data locked up in their clinical histories of wider relevance. Good to see some researchers paying attention.
Agreed! It’s a fascinating field that provides a lot of promise for at least a subset of patients.
Sian James interferon gamma is disastrous, totally destroys biochemical pathways. Just wondering how it’s effected you in the long-term?
“Could an overactive immune system be the trigger for some people’s life-threatening depression? If so, we might just be on the way to a cure, says Phyllida Brown”
Here’s an interesting article about people who have become suicidal after taking alpha interferon and interleukin-2, two popular immune-boosting drugs. Hundreds of others have become seriously depressed.
“Most of us associate depression with being run down and having poor immunity to infections. The startling side effects of the immune-boosting drugs turn that notion on its head. They suggest that some people who are depressed may actually be suffering from an over-heated immune system, and that damping down inflammation could offer a brand new way to treat routine clinical depression–while making billions for the pharmaceuticals industry into the bargain. It’s a theory that recasts depression–one of the great plagues of our time–as a chronic inflammatory disease like rheumatoid arthritis.”
“For the first time it became clear,” says Dantzer. “Sickness behaviour is like fear–it is a state that makes the animal reorganise its priorities.” Just as the sight of a predator makes animals release hormones that drive the “flight-or-fight” response, infection triggers the release of cytokines, which make the animal rest and conserve its resources to fight the infection. And of course, sickness behaviour is not exclusive to rats–think of the last time you got flu.”
Soure: New Scientist
Date: 16 June 2001
http://www.biopsychiatry.com/immunesystem/index.html
Love it. Thanks, Rachel, for posting that….:)
SAMe wasn’t strong enough for my sister & I. We resorted to mucuna. We have had CFS since we were toddlers (at least), giving us over 100 years of data and experience in the field. We’ve become a CFS research institute, in a way.
Could you tell me which brand of mucana capsules you prefer and what dosage you have found helpful? Thank you.
I’ve only just learned of mucuna after believing for decades I needed help w dopamine. Are you still taking it?
Check out sections of book on immune effects on depression and other disorders written (but not completed) by a pioneer in the field – Ronald Smith – shortly before he died (and not published).
http://www.cytokines-and-depression.com/chapter1.html
It provides a history of the field. It’s an interesting addition given these blogs and the recent blog on the psychiatrist using antivirals to treat adolescents wrongly diagnosed as having treatment resistant depression.
Sad he didn’t get this published. Its so insightful. Advancement in this field is still lacking. Even though most people realize the head and brain are attached to the body, sadly, they still try to dissect it from the body and treat illness without full body connections. Having just lost both parents and there being dementia and other issues involved, I could see how much of it was related to physical reasons and much was inflammation and autoimmune.
A supplement my doctor has just started me on is curcumin. It helps autoimmune issues, inflammation and has helped some with depression. It is a vasodilator and there is a fine line as to how much a POTS person can dilate. I had to back down on my amount. But it is helping my pain. We hope to avoid Plaquinol with its use. I had found on my own that turmeric is absolutely necessary for me. I intend to take it also. (As with other supplements, you can help one thing but potentially cause another issue. My research shows it could potentially up estrogen levels.)
Issie
Curcumin is the “active” part within turmeric; the part that has the bulk of the anti-inflammatory properties.
This sounds like there on to something at last ive heard from a group in the usa that have been doing studys into low hormones and higher levels have helped upto 80% of the study group
my naturopath has tested me for low level viruses and bacteria. When I started with him about 3 years ago I had 6 of those. With treatment primarily withsupplements I’m now down to two a bacteria I don’t remember the name of and Epstein Barr. I am taking an antibiotic for the bacteria finally responding. All the supplements help with the epstein-barr. The spelling may be wrong for Epstein Barr.I recommend getting tested for the viruses you have rather than relying on studies. My naturopath is Paul Anderson in Seattle, Anderson Medical Specialties associates.
Amazing Thread!
Anyone else tried mirapex, abilify, modafinil or something similar?
Anyone else tried any dopamine agonists?
To answer your question, Grant Michaelmas, I have tried modafinil (Provigil). It helps boost my energy for the day, but then I am burned out the next day. I take it when I absolutely have to get something done or have an appointment. My doctor prescribed the 100 mg tablets. My body can’t handle that much, because I have metabolizing pathways that don’t work well according to genome testing, so I am ultra-sensitive to sime meds & have side-effects. So I take about 1/8 of a tab. For those who are sensitive to meds, it could be compounded at a pharmacy into a smaller dose.
Also, by genome testing, you can find out what meds you would be poor metabolizers of to help identify which medications are likely to cause a great deal of side effects, so you can avoid those meds. I don’t know if it is common for people with CFS/ME to be poor metabolizers, but I certainly have that problem.
This is interesting work. I’ve tested amino acids and learned that my phenylalanine is indeed quite high while my tyrosine is low. I never put much thought into this until now. I wonder how common a finding this may be in ME/CFS and related diseases.
Playing guitar I’m keenly aware of my reward system and how it’s functioning. Reward is the encouragement one needs to go further. I find that when it’s working well, one note flows into the next. When it’s not I can hardly play, certainly not improvise. Interestingly, a macrobiotic diet (generally lower protein) always ensured this reward system was functioning more or less normally and I could enjoy playing. A lower acid diet likely carries with it less oxidative stress. Less oxidative stress may lead to less interference with BH4, and hence greater dopamine production and reward. The downside is I shed muscle mass, which is why I never fully adopted the diet.
Recently I’ve found treating a pathogen (babesia duncani) also produces the same effect and I’m able to enjoy my guitar a whole lot more. It appears to be relieving me of oxidative stress and excess acidity (noted by less facial skin irritation from acidic sweat).
So I believe pathogens and toxins can produce oxidative stress in the brain that can have a profound effect on the reward system. That this down regulated reward system can then lead the brain into over-responding to relatively small amounts of inflammation is the kind of loop that makes sense to me with regards to chronic illness, especially my own.
Thanks for this report.
Thanks GeronimoG and good luck with having more rewarding guitar playing.
I have 2 bad variants of CYP2D6 (*4 and *5) that make me a poor metabolizer of MAOIs, SSRIs, and many other meds. It also makes the conversion of tyrosine to dopamine impaired. Have there been any studies directly linking poor metabolization of CYP2D6 to CFS and the relevant research in this article? I think that may be worth looking into? If we could create better CYP2D6 inducers, I also wonder if that would help with the conversion of tyrosine into dopamine.