

“A functional symptom is a medical symptom in an individual which is very broadly conceived as arising from a problem in nervous system ‘functioning’ and not due to a structural or pathologically defined disease cause.” – Wikipedia
“… on finding itself unable to discover effective treatments or physiological causes for symptoms, the medical profession [is] subject to a temptation to minimize the explanatory role played by the many gaps in its own current scientific understanding, and instead to grope for theories of psychosomatic etiology …” – Wikipedia
Many have thought IBS is more of a central nervous or mental problem than anything – but this study suggests otherwise
Liked the other disorders allied with irritable bowel syndrome (IBS), the cause of IBS itself has been hard to track down. The so-called “functional disorders” like fibromyalgia, IBS, and interstitial cystitis are similar in at least six ways:
- they commonly occur with each other.
- more women than men are affected.
- fatigue and pain levels are high.
- mood disorders are common.
- similar parts of the brain such as the insula appear to be activated.
- attempts to find the source of the pain where it occurs (IBS-gut, FM-muscles/joints, IC-pelvic area) have mostly not been successful.
These disorders tend to impair functioning to a great degree, but when researchers turn their instruments on their apparent source of the problem – in this case the gut – they find little or nothing wrong: no structural damage, little evidence of inflammation, nothing. Direct evidence that something has gone wrong in these patients’ muscles, gut, or pelvis has been hard to come by.
The constellation of high rates of fatigue, at least somewhat high rates of mood disorders, and, in particular, few successes at finding problems in the body have led to the perception that these disorders are all in their patients heads.
Foods Provoke Problems – and a Study
Recently, however, studies using newer technology have begun to uncover problems, and this is one of them. The fact that people with IBS often experience symptoms after eating provided one clue. Observations that highly fermentable, difficult to digest foods called FODMAPS (fermentable oligo-, di- and mono-saccharides and polyols), in particular, often provoke pain, bloating, etc., provided another clue.

Researchers gave IBS patients food guaranteed to cause problems and then used an MRI to see what happened
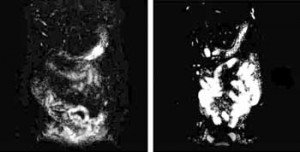
Despite failures to find structural abnormalities in the gut, the problems with food intake indicated that something must be happening in the gut. Putting two and two together, radiologist Ragnhild Undseth of Lovisenberg Hospital in Oslo did to her IBS subjects what chronic fatigue syndrome researchers have doing to their ME/CFS subjects for years – she knocked their systems for a loop.
She stressed the guts of IBS patients (and healthy controls) by feeding them an undigestable and highly fermentable substance called lactulose that draws water into the gut. Then she used MRI to assess the water content and diameter of the terminal ileum and descending colon before and after the lactulose moved through it.
Food moves from the stomach to the small intestine where the minerals and nutrients from the food are digested. The terminal ileum is the last way station for digestion at end of the small intestine. Everything that didn’t get digested in the upper part of the small intestine ends up in the terminal ileum. The terminal ileum is also where B-12 gets absorbed.
Results
“The results may suggest a functional impairment of the small intestine in patients with IBS.”
Asking IBS patients to ingest an undigestible substance is akin to asking people with Chronic Fatigue Syndrome to exercise – it’s going to make them worse, and it did. The IBS patients’ gut symptoms soared while the healthy controls experienced few problems.
It also did something bizarre. The terminal ileum responded in the opposite way in the two groups; it got smaller in the healthy controls and larger in the IBS patients as the lactulose hit their systems, and not just a little larger. The difference between the small bowel diameters in the IBS and healthy controls was a highly significant one.
That was really something given that the diameter of the terminal ileum in the IBS patients before the ingestion of lactulose was significantly smaller in the IBS patients than the healthy controls. To summarize: while the IBS patients TI was smaller than normal before the undigestible food reached it, it got larger when it did. In the healthy controls, the TI was getting smaller, not larger, with the introduction of lactulose.
The degree of water accumulation was not significantly associated with increased symptoms – not an unusual finding in this complex disease. That could have been due to the small study size and/or the fact that the highly fermentable food substance was doing other things to the gut as well.
Functional Indeed
Why is this important? Because this study indicates that something in this so-called “functional syndrome” has actually functionally gone very wrong–not with the central nervous system, but with the gut. IBS patients have faced the same bias – that IBS is mental–as have ME/CFS and FM patients. Studies do show that mind/body therapies can be helpful for some with IBS, but that doesn’t mean that something is not “functionally wrong” either.
In Nordic Science, the lead author of the study, Ragnhild Undseth in Oslo, emphatically stated that her study indicated IBS is not some sort of gut-associated mental disorder. “No,” she said. “This is not psychological.”
Another researcher added that this study indicates there is an “organic basis” to IBS.
Cause
Exactly what is causing the higher accumulations of water is not clear. When food is present the gut should be both absorbing and secreting fluids. Either the small intestine is not emptying as much fluid into the large intestine as expected, or more water is being secreted into the small intestine than normal.
If increased secretion is the problem then mast cell activation may play a key role. An earlier study found increased numbers of mast cells in the terminal ileum, ascending colon, and rectum of diarrhea-prone IBS patients.
Low serotonin levels are a possibility as well; serotonin stimulates the gut muscle to move (motility) – an important factor in IBS. Low serotonin levels have been found in gut tissues in IBS, and low serotonin is associated with increased rates of mood disorders. Serotonin, then, fits the bill in several ways – but since serotonin levels vary widely in IBS patients, serotonin is not going to be the answer for all of them.
Indeed, with four types of IBS distinguished so far, no one factor is going to be responsible. While small intestine water accumulation was found in most people with IBS in this study, they weren’t found in everybody; like FM and ME/CFS, IBS is a heterogeneous condition. (At least four different types of IBS have been characterized.)
Conclusion
Why the small intestine’s of the IBS patients reacted in such an unusual fashion is not clear, but what is clear is IBS is a functional disorder – just not in the way the phrase is usually used. When confronted with certain foods the small intestine functions incorrectly; instead of getting smaller – it gets larger. It may be that in order to really get at IBS researchers need to do what they’re doing in ME/CFS – stress the system to more fully reveal its breakdowns. The fact that water secretion or retention in the small intestines is clearly a problem points researchers in a new direction.
The problems with the terminal ileum make another thing clear – a FODMAPS-based diet that restricts the intake of ‘highly fermentable’ foods is a very good idea. It doesn’t work for everyone with IBS, but it is helpful for many. We’re going to be covering that diet in a future blog that’s coming up – after Thanksgiving :).







The symptoms of IBS are usually caused by Small Intestinal Bacterial Overgrowth (SBIO). This is diagnosed by a 3 hour breath test that measures levels of gas in the small intestine after ingesting lactulose and treated with specific antibiotic drugs (Rifaximin & Neomycin) followed by a prokentic drug that stimulates gut motility by increasing serotonin levels. I am surprised that this article and the quoted researchers do not mention SIBO and the work of Dr. Mark Pimentel who is a pioneer in the understanding and treatment of IBS. A FODMAPS diet has shown to be helpful for many patients but cannot reverse this condition in the long term.
I imagine that Pimental is right on, but the blog was not meant to be an overview of IBS or SIBO. It focused on a new finding that helps to balance the many studies and papers that have focused on mental aspects of IBS. For instance a review paper from this year (World J Gastroenterol. 2014 Jul 21;20(27):8807-20. doi: 10.3748/wjg.v20.i27.8807. Irritable bowel syndrome: a disease still searching for pathogenesis, diagnosis and therapy.
Bellini M, Gambaccini D, Stasi C, Urbano MT, Marchi S, Usai-Satta P.http://www.ncbi.nlm.nih.gov/pubmed/25083055 ) states
“Because the probability of organic disease in patients fulfilling the IBS criteria is very low, a careful medical history is critical and should pay particular attention to the possible comorbidities.”
The review article also says
“The pathophysiology of IBS is not yet completely clear. Genetic, immune, environmental, inflammatory, neurological and psychological factors, in addition to visceral hypersensitivity, can all play an important role, one that most likely involves the complex interactions between the gut and the brain (gut-brain axis)”.
Pimental has participated in some of the largest IBS trials to date. The results have been good but not overwhelming – perhaps because not all the treatments he uses were incorporated into the trials
“A total of 1260 patients were enrolled in the two trials, making these studies among the largest in the IBS literature. In looking at the combined primary endpoint, 40.7% of rifaximin patients reported global improvement in symptoms compared to 31.7% of placebo patients (P < 0.001; NNT = 12) in the two studies combined. Numerous secondary endpoints, including abdominal bloating, were statistically better in the active treatment arm compared to placebo. This benefit was largely maintained throughout the study period, up to 10 wk after treatment ended. No significant adverse effects were reported in the rifaximin arm, and no cases of Clostridium difficile-associated diarrhea or ischemic colitis were seen. The authors concluded that a two-week course of rifaximin may provide lasting improvement of symptoms in patients with IBS without constipation.” Of the 70 patients re-evaluated later most required followup treatments.
A recent review stated “Gastroenterology practitioners have more agents than ever before to treat the symptoms associated with IBS. Unfortunately, despite advances in our understanding of the pathophysiology of this disorder, targeted treatments do not yet exist.” http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4112883/
I’ll bet Pimental is right on but it’s going to take time to prove it to the rest of the medical community
I think since Medicine began if they couldn’t find a cause for a disease it was either “stress” or psychological- hope they hurry up and find the cause for ME/CFS!
“more women than men are affected”
Every time I read or hear this, my stomach gets queasy, and I want to scream like a woman, “I DO NOT BELIEVE THAT FOR A SECOND”! I am literally sick of it. There is no study, or corroborating evidence to even suggest such a conclusion. The simple fact is, men are not tested or diagnosed for a multitude of conditions “affecting women”. We do not go to the doctor and simply “tough it out”. I would say it is our own fault that we are overlooked and under diagnosed, but we are no less at risk, or somehow better off than the ladies.
Watch this, male and female immune responses very different, other autoimmune illnesses also more prevalent in women
http://www.abc.net.au/catalyst/stories/4090272.htm
You can download a pre-recorded webcast of the 2014 Global Outreach Symposium on IBS hosted by Dr. Mark Pimentel, Director of GI Motility at Cedars-Sinai in Los Angeles at:
https://www.regonline.com/builder/site/Default.aspx?EventID=1510950
This is a good source of information about the latest research on IBS, its cause and the effectiveness of antibiotic treatment and diet.
Hi…my pain doctor gave me lactulose for occasional constipation from pain meds. It makes my gut sort of hurt, but works well. I don’t have IBS, though. just sayin’
If mast cells are causing the problem, then GastroCrom (ingested cromolyn sodium, same stuff that’s in Intal (for asthma) and OptiCrom (allergy eyes). The names may have changed since I tried them. I wonder if it’s worth asking my dr for an rx?
I totally agree with you, my brother suffers from ibs and did finally go see a Dr, but as you say men dont go to a Dr as often as women do don’t get diagnosed!!!
I had the systemic mastocytosis blood work done which came back normal ranges but there are a lot of patients now being diagnosed with HIT histamine intolerance with low DOA there are now numerous sites up on histamine intolerance on Facebook but I do not see any major
success stories from this aproach therefore I will stick to high doses of vitamin D which Dr. Coimbra is finding in M.S. numerous auto immune conditions, Parkinson’s, Alzheimer, autism, cancers, diabetes he calls it ‘partial vitamin D deficiency’ I take now 5,000 i.u. gel form
D3 daily with omega fish oil, multi vitamins, b complex 2.5 litres of water…I have contacted numerous M.S. patients they are well this treatment is for life, I also follow a high fat intake food diet ketogenic avoiding any foods I cannot tolerate I eliminate them entirely, nothing with
sugar…’cause I am over 10,000 i.u. of D3 I do not eat any dairy only once a week I ear Edem cheese which has vitamin K in it…They do these bloods or urine 24 hour calcium, blood calcium, vitamin D, ‘parathyroid PTH parathormone’ I am off all prednisone all pain meds this
is all I take, black coffee next is off the list it makes my heart go bananas so I am better once off it 🙂 Numerous youtube videos on Dr. Coimbra from Brazil, neurologist trained prior in Florida he is reversing illnesses one does not need vitamin D2 with D3…I buy this product
online 10,000 i.u. D3 ‘Healthy Origins’ clinically studied 360 soft gels or you can get pure oil D3 but gel forms easier to take, it must have fish oils to work Omega, Cod liver oils etc, I get my calcium from vegs/fruits tolerated types…Water flushes out access calcium vital daily 2.5
litres…A woman on youtube called Stephanie on ketogenic foods I follow, I no longer eat any breads or gluten free b.s. garbage, make your own with coconut oils, coconut flours etc etc see Stephanie diets, last there is no toxicity high dose D3 as long as you cut our
dairy…Magnesium, b2 b12 monitor or take vitamins, meats, chicken, fish plus eggs bacon high in fats ‘eat fat’ it is vital, check out eat fats videos youtube ‘sugar is a toxin’ ketosis runs away from Glucose 🙂
Forgot to mention M.S. lesions gone in patients try looking up ‘MS Cure’ but it is a treatment life long not cure 🙂 numerous groups MS on Facebook now 🙂
Correction I take 50,000 i.u. daily vtamin ‘hormone’ D3 which is actually called Cholecalciferol 🙂
As a sufferer ME/CFS along with IBS, I’m not surprised that more women than men are affected by irritable bowel syndrome. With four types of IBS distinguished so far, I don’t believe that “low” serotonin levels, for many (especially women), is the cause of their IBS; in fact, quite the opposite. Serotonin and estrogen have many systematically interrelated functions. Serotonin and histamine are both increased by estrogen. The reason that irritable bowel syndrome is more commonly found in women, than in men may be because of the hormone estrogen and serotonin, not for any psychological reasons. Estrogen and excess serotonin releases histamine in the gut activating the immune response causing diarrhea-predominant IBS.
In the words of Dr Ray Peat, “Irritable bowel syndrome can be treated effectively with anti-serotonin agents. This syndrome is very common in women, with premenstrual exacerbations, when estrogen is highest.” (1)
(1) http://raypeat.com/articles/articles/serotonin.shtml
As the Managing Editor and Publisher of Dr. Pimentel’s book, “A New IBS Solution”, I thought this might be of interest. We’re currently working on a 2nd Edition which is going to include a new Dietary/Menu Section, Associated Conditions with SIBO, the latest Research/Data and a Directory of Physicians that specialize in treating SIBO. As our goal is to make the 2nd Edition as comprehensive and complete as possible, I would welcome any suggestions/feedback.
I have been diagnosed with “leaky gut” – increased intestinal permeability. This is claimed to be caused by intestinal bacterial overgrovty (SIBO) in 75% of the cases. I was suggested the antibiotic rifamaxin, perhaps in combination with neomycin. Anyone with ME that has any experience from this treatment? What symptoms does improve?
I have a slow bowel. Defecate only once a week in average. Unfortunately I have not found any medication for speeding up my slow intestines that I tolerate. I have heard about some kind of medicine that increases serotonine. Anybody know what that could be?
My IBS started two years before my ME/FM that I have had for fifteen years. My experience is bile is the culprit. The diarrhea will not stop until it becomes bile only. What turns the liver on to produce massive bile that is like pure acid would be a good study. The only treatment that works is Olestyr/Cholestyramine which neutralizes the bile. It is dispensed in packets, and really works for me.
Good blog Cort. As an IBS sufferer for over 40 years, I can say, “there is nothing usual about it,” and when in the throws of an attack, there is NO THINKING IT AWAY! I can yell, kick my legs (often literally when awaiting the explosion set to occur), because I write a great deal about meditation, calming the mind, and providing optimal feedback to the brain. I do all these things, and they all help me cope, but not one has cured my IBS, or other comorbid disorders. There are many forms of stress that affect the bowel and they are not all psychological.
A study in 2009 suggests in some, IBS could be related to immune problems, sound familiar? http://www.ncbi.nlm.nih.gov/pubmed/19174797
Two 2014 studies of note. http://www.ncbi.nlm.nih.gov/pubmed/25150006
http://www.ncbi.nlm.nih.gov/pubmed/25063707
Mast cells were identified in another study in 2011. http://www.ncbi.nlm.nih.gov/pubmed/21427712
INTERESTING! I never thought the possibility that IBS could be just psychological.
I’ve been diagnosed with IBS recently and am now living on a low FODMAP diet. Life haven’t been easier since then.
By the way can you recommend any good IBS resource site? I’ve been looking for quite a while now, and so far I’ve seen this site helpful— casadesante.com
Do you have any other recommendations? Thanks & great post as always!
Sorry. Men are used in research more than women it’s a fact. Women and medicine have been neglected for many years.