

The question Dr. Bateman tackled in her recent Solve ME/CFS Initiative video was “Can Fibromyalgia and ME/CFS research help you sleep?” (Section in [ ] represent my additions.)
Sleep, of course, is one of the biggies in ME/CFS and FM — one of the four legs of the table Dr. Bateman focuses on in her practice. She’s gone to great lengths to improve sleep, stating (perhaps with a little sigh), “In the last twenty years I have tried everything possible to help my patients sleep”. It’s a key issue – and Dr. Batemen is talking on it. Why now?
Because as part of her work for the IOM panel, Dr. Bateman dug deeply into a lot of the chronic fatigue syndrome research and that’s prompted some new ideas on these disorders and sleep.
First she tackled some basics.
Sleep Disrupters
Medications That Disrupt
First came a quick overview of medications – some in common use in the FM and ME/CFS communities – that can disrupt sleep. They include stimulants (caffeine, drugs), antidepressants, opioids, benzodiazepines, dopamine increasing drugs, decongestants, and taking multiple drugs. If you’re taking any of these and experiencing really poor sleep, they could be contributing (not causing), but contributing to it.
Sleep Disrupting Conditions Associated With FM and ME/CFS
Some conditions often found concurrent with FM and ME/CFS also make it difficult to get into restful sleep. Pain, for instance, can make getting to sleep and staying asleep more difficult. Frequent urination, a snoring spouse, pets that wake you up, and racing thoughts are all outside conditions or problems that can be addressed.
Primary sleep disorders such as sleep apnea, restless leg syndrome, narcolepsy, etc. are common enough in ME/CFS and FM for Dr. Bateman to assert that everyone with these disorders should have a polysomnography or sleep study done. If they are found, that could be some good news, because they are treatable and once they are treated you should feel better.
- Check out how one person’s life was turned around by a sleep study.
The ME/CFS and FM Sleep Gestalt
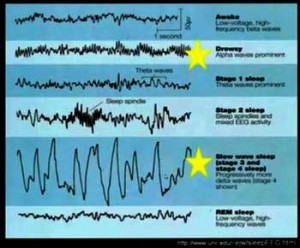
Polysomnography studies display a general sleep pattern which, if it is not diagnostic, is still very different from what is seen in sleep disorders. In general, people with ME/CFS and FM have delayed sleep onset, experience fragmented sleep, increased light sleep (increased alpha waves), and decreased deep sleep (decreased delta waves).
This is the ME/CFS and FM sleep gestalt. Dr. Bateman felt clues to the sleep problems must lie in the scientific literature – not just in the sleep studies, but in other studies that explain what’s going on this illness. Back into the literature she went to try and understand sleep and ME/CFS and FM.
The new insight Dr. Bateman brought in this talk was her realization that the research findings reveal fundamental problems that are guaranteed to disrupt sleep. ME/CFS and FM are not sleep disorders per se – they are disorders that naturally disrupt sleep. The best way to address sleep in ME/CFS and FM is to address these core problems.
This is why, while they can be helpful, drugs rarely if ever return an FM or ME/CFS patient to fully refreshing sleep. The only thing that will do that is fixing FM or ME/CFS.
A Very Sensitive Nervous System
Research has shown that central sensitivity, which occurs when the brain interprets normal stimuli as being painful, is present in FM. Since increased pain levels can cause increased alpha waves, the pain people with FM are experiencing could easily be contributing to their difficulty sleeping.
While central sensitization is not something researchers commonly associate with chronic fatigue syndrome, the symptoms of a brain overwhelmed by stimuli (odors, bright lights, noises) are clearly present.
[An FM study recently indicated why a similar sensitization to stimuli may be occurring in FM. See Sensory Distress: The Other Side of Fibromyalgia. Another study indicates the brains of ME/CFS patients have trouble disengaging themselves from innocuous stimuli. Long after healthy people’s brains have checked out the stimulus, determined it’s not relevant, and moved onto something else, the brains of ME/CFS patients continue to keep an eye on it. That’s not a recipe for rest.]The fact that pushing an ME/CFS patient too far causes their stimulus overload to get worse indicates central sensitization plays a key role in both ME/CFS and FM.
[Dr. Bateman’s conflating of the “wired and tired” phenomena and central sensitization suggests an overwhelmed nervous system that lacks the resilience to calm down is present. An “exhausted” nervous system was believed to be present in neurasthenia – probably the name for FM and ME/CFS in the first part of the 20th century.]Dr. Bateman: Can ME CFS and Fibromyalgia Research Help You Sleep? The Solve ME/CFS Initiative Webinar
Treating Central Sensitization to Improve Sleep
The sleep problems present (fragmented sleep, inability to attain deep sleep) are suggestive of a nervous system that’s too on edge to calm down enough to attain deep sleep. What to do about it? Dr. Bateman suggests some basic approaches to down-regulate the central sensitivity present and quiet those intrusive alpha brain waves.
- Pacing – Since too much activity puts the central nervous system into overload, you should over-exert yourself as little as possible; that is pace, pace, pace to avoid putting yourself into a PEM state that’s going to disrupt your sleep.
- Wind your system down before sleep – by putting yourself in a quiet, dark environment. Since bright screens activate your brain, looking at a computer screen or TV right before sleep might not be a good idea.
- Take calming drugs before sleep, if necessary – Drugs that calm the central nervous system such as Neurontin, Lyrica, low dose naltrexone, Klonopin, low dose amitriptyline, doxepin elixir, and cyclobenzaprine can help. Notice that none of these are sleep aids, per se – they are all calming agents that help relax an edgy brain.
Autonomic Nervous System
All the studies suggest that the “fight or flight” mode of the autonomic nervous system (the sympathetic nervous system) has been turned on in both ME/CFS and FM. They indicate that even during sleep the sympathetic nervous system is revving away producing increased an heart rate and decreased heart rate variability (HRV).
Reduced heart rate variability – Your heart rate should normally be shifting continuously up and down in response to what’s happening in your body, but in ME/CFS and FM it tends to lack flexibility (low HRV), and instead appears to be driven by an unrelentingly turned-on sympathetic nervous system.
[Low HRV is not good news; it’s associated with, among other things, increased mortality. An Australian study failed to correlate any traditional sleep measures (sleep architecture and others) with poor sleep quality, but found that reduced heart rate variability did. It appeared that autonomic nervous system dysfunction was preventing ME/CFS patients from relaxing into deep sleep.]Rebalancing Autonomic Nervous System Functioning
What are we to do? Do things that turn off the fight or flight response, reduce norepinephrine levels, and allow the “rest and digest” or “parasympathetic nervous system” to calm the body and mind enough for you to enter into deeper sleep.
Dr. Bateman recommends deep breathing or relaxation exercises and/or yoga. She noted that long deep breaths with longer delayed exhalations release chemicals from the parasympathetic nervous system that turn down the SNS. [Dr. Cheney and most respiratory therapists recommend long inhales followed by even longer exhales with the lips pursed to increase oxygen level.] [Fred Friedberg, a psychologist with ME/CFS who has benefited greatly from meditation practices, recommends doing simple meditations before sleep to help you enter deeper sleep. He has found patients who employ these techniques can sometimes cut back or even eliminate their sleep meds.
If something is occupying your mind before you sleep, Johannes Starke recommends writing it down on a piece of paper and telling your brain not to worry about it anymore. Envisioning yourself in a beautiful safe place may help as well. I find the simply stating the word “relax” again and again can be helpful. All these practices, of course, take practice to work. ]
The High, High Sympathetic Overdrive Subset
Dr. Bateman has found that patients with really high levels of sympathetic overdrive such as POTS patients, in particular, can benefit from very low-dose propranolol (LDP) (10-20 mg). She uses LDP to reduce the heart rate and help patients relax, allowing them to go to sleep.
At Home Test of Sympathetic Overdrive – when you lie down if you feel your heart pounding in your chest — beating hard, not necessarily fast – Dr. Bateman suggests you’re probably in the sympathetic nervous system overdrive category and might want to try the LDP protocol before you go to sleep.
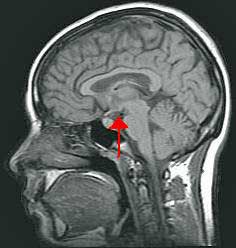
HPA Axis Contributions to Poor Sleep
Cortisol helps the body release energy. You want to have more cortisol in the morning to get your energy flowing, and less at night to allow you to calm down. People with ME/CFS, though, have reduced cortisol production in the morning (trouble getting started) and increased cortisol at night (trouble going to sleep). (How much better it would be to have higher cortisol levels in the morning (raring to get at the day!) and lower cortisol levels in the evening (sleep like a rock).
The problem does not appear to be in the adrenals or pituitary, but in the hypothalamus – the upper part of the HPA axis that regulates hormone production (thyroid, cortisol, vasopressin, estrogen, progesterone) in the body. Receiving information on hormones, electrolytes, temperature, blood pressure, light, and emotions, Dr. Bateman called the hypothalamus the control center of the brain. It also happens to regulate autonomic nervous system functioning.
How do you help the hypothalamus help you sleep? It’s about reducing HPA axis activation and that means staying even-keeled emotionally, reducing light levels, being properly hydrated, etc. before you sleep.
Drugging Oneself to Sleep
Then there’s the drugging yourself to sleep option. Dr. Bateman warned against the idea that fixing the sleep problem in ME/CFS and FM will cure either disorder. Taking sleep drugs may help with your sleep but will not cure these disorders because they don’t address a) the underlying causes (central sensitivity, autonomic and hypothalamic dysfunction) and b) they often leave one tired the next day. Sometimes they are necessary, though.
Using medications skillfully
- If you can’t get to sleep – use low dose short-acting sleep drugs.
- If you have frequent awakenings – use longer-acting drugs in low doses.
- If you have early awakening – the meds you’re taking to help you sleep may be losing their effectiveness from overuse.
From the Question Period
Diet and Sleep?
Eating carbs before sleep? Some people do well eating carbs before sleep others get worse. Generally, avoid heavy meals before bed. You don’t want, Dr. Bateman said, your body working on anything – including digestion – while you’re asleep.
Melatonin
Melatonin regulates day/night cycles. If you don’t get outside, your brain can get confused about day/night cycles. You want to have light exposure and dark at their natural times. Melatonin can restore that, but it probably works the best when it’s not used all the time. She said it’s a hormone, but it’s “pretty safe”.
Supplements that help you to relax and prepare for sleep are great. Just don’t overdo.
Conclusions
Except for the propranolol suggestion, there’s nothing new here treatment-wise. Instead, Dr. Bateman focused on research findings outside of sleep studies that help explain why sleep can be such an issue in ME/CFS and FM. Those findings led her to focus on basic approaches to sleep we all know about, but probably don’t put into practice as much as we should.
We are where we are. The big answers to sleep and ME/CFS and FM will require more research. With that in mind we await the publication of the most exciting studies, in my mind, to come out of the Stanford ME/CFS Symposium – the Zinn studies.
Sleep Survey
Dr. Bateman suggests that everyone with ME/CFS or FM get a sleep study done, but our recent sleep survey found that most people (about 68%) had not done one. Almost 35% of the people in the survey, however, indicated they had been diagnosed with a sleep disorder that a sleep study would have picked up.
That suggests a significant number of people who have not had a sleep study may have an undiagnosed sleep disorder as well as FM or ME/CFS.
The survey also indicates that most people have tried good sleep hygiene practices. Some (6%) find them very effective or somewhat effective (32%) but most (62%) found them not very effective.
The full results of the sleep survey are coming up shortly.








I have tried melatonin years ago & found it did relax me but didnt quite push me over into sleep-
just made me sleepy. Last year after a number of personal challenges & 6 years of ME to cope with i tried it again. This time I had a very bad experience. I became extremely depressed
within 3-4 days. I had never experienced depression to the point where i felt unable to function
before. It was very alarming. I’ve had the blues inevitably with this illness & all the loss it involves
but have always emerged quite quickly thanks to a number of years of involvement with buddhism.
Luckily for me I came across an article warning of the possibility of melatonin related depression.
I stopped taking it & was fine withing a couple of days.
melatonin is not in my view completely safe…
.
Isn’t that something!
I tried melatonin once years ago and it just made me vague, without helping sleep, a bit like you, Grace.
Many years later I had test for it and found that I already had near- toxic quantities already. Taking more for me is definitely a no – no.
A naturopath commenting on-line to my experience said that melatonin also acts as a detoxifier and it may be why some of us have too much of it.
It is yet another thing we shouldn’t take willy-nilly. Most doctors don’t seem to be aware of this and it is treated as some kind of panacea for sleep.
It is a hormone. A couple doctors are pretty careful about it and others are not. Below is from our page on melationin
Dr. Teitelbaum is on the low end of the totem pole on melatonin use – recommending that patients take only .5 mgs/daily. Several doctors note that we still don’t know a lot about melatonin – a hormone that affects many parts of the body – and Dr. Bested recommends melatonin only be taken under a physicians direction.
It has been suggested that OTC melatonin is way too much. I agree with Dr. T. I also agree with Dr. B. I don’t think anyone should take any HORMONE unless they are having their levels checked, especially in FM and CFS. One little thing can throw everything out of whack.
Back to basics. Can one have CFS and a very normal immune system? I have always said NO. I also believe it’s quite possible the original pathogen may be long gone and the dysbiosis in the gut, where the immune system resides, is damaged also from the undesirable proliferation of fungi and negative microbes that release toxins as a result of a high refined carb diet (high fructose corn syrup) in everything and un-natural wheat, which is also in everything, if you actually look at labels. Therefore, I also believe comprehensive stool testing would be very enlightening but they’re never done. Not very romantic I suppose. And, are genetics a factor? Of course.
Not to mention, the toxins from the bad microbes in the gut to the blood stream no doubt pass the blood brain barrier as well as through out the body harming all cells from the blood to the brain, nervous system, immune system, etc, and of course disrupting sleep!
If we had a toxin neutralizer, problem solved. Come on Dr Lipkin, Right, Cort? RP
I wouldn’t be surprised if toxins play a huge role in ME/CFS and FM. Go Lipkin! 🙂
TOXIN NEUTRALIZERS: toxins can be metabolic, heavy metals, petrochemical and pesticide exposures, etc. Make sure that genetics are known and carefully worked with so that toxins dislodged are truly removed from the system, not just pulled out and recirculated (detox hell).
Depending on other substances being ingested, personal situation and the toxins involved:
1. Zeolite in capsules or liquid; many forms of this
2. Food grade Diatomaceous Earth, can be bought in bulk and can be a good calcium supplement if balanced with other things
3. Activated charcoal capsules (Dr. Klimas likes this one for mycotoxin/mold exposures)
4. Modified Citrus Pectin: PECTIPURE formula sold by many vitamin suppliers like Swanson, NOW, etc. for best price. I like this best because it pulls out all the bad stuff and does draw out important nutrients, as charcoal and maybe the others do
5. Fulvic acid and related earth-based products such as the Indian Shilajit, if these are from guaranteed pure and safe origins
6. Bentonite liquid clay, Redmond clay powdered, etc.; same caveats
7. Essential oils applied on skin if in a safe or diluted enough form
8. Sodium bicarbonate body scrubs or soaks
9. Epsom salts baths if the SUOX or other sulphur methylation pathway is not an issue; to find out requires the Dr. Yasko test; 23andme does not test for this
10. FIR sauna only if an environmental doctor approves and knows the system can handle it
Research these for appropriateness. Some of these are very good nontoxic, non-drug antacids that can add some minerals to the body.
TOXIN NEUTRALIZERS: toxins can be metabolic, heavy metals, petrochemical and pesticide exposures, etc. Make sure that genetics are known and carefully worked with so that toxins dislodged are truly removed from the system, not just pulled out and recirculated (detox hell).
Depending on other substances being ingested, personal situation and the toxins involved:
1. Zeolite in capsules or liquid; many forms of this
2. Food grade Diatomaceous Earth, can be bought in bulk and can be a good calcium supplement if balanced with other things
3. Activated charcoal capsules (Dr. Klimas likes this one for mycotoxin/mold exposures)
4. Modified Citrus Pectin: PECTIPURE formula sold by many vitamin suppliers like Swanson, NOW, etc. for best price. I like this best because it pulls out all the bad stuff and does draw out important nutrients, as charcoal and maybe the others do
5. Fulvic acid and related earth-based products such as the Indian Shilajit, if these are from guaranteed pure and safe origins
6. Bentonite liquid clay, Redmond clay powdered, etc.; same caveats
7. Essential oils applied on skin if in a safe or diluted enough form
8. Sodium bicarbonate body scrubs or soaks
9. Epsom salts baths if the SUOX or other sulphur methylation pathway is not an issue; to find out requires the Dr. Yasko test; 23andme does not test for this
10. FIR sauna only if an environmental doctor approves and knows the system can handle it
Research these for appropriateness. Some of these are very good nontoxic, non-drug antacids that can add some minerals to the body.
I have insomnia, CFS and Ehlers Danlos Syndrome (a connective tissue disorder). I’ve been on Ambien for seven years now and worry about the connections suggested between this drug and Alzheimer’s.
What on earth are we to do?
Ambien is zolpidem, which is not a benzodiazepine and there is at least one study that suggests it may actually help memory consolidation. I don’t believe there is any data linking it to dementia. I’ve been taking 10 mg in four divided doses through the night for fibro for 15 years. While it is not quite as effective for me now and and while I am a bit drugged for an hour or two in the morning, I haven’t noticed any negative memory effects. I wouldn’t worry about prolonged Ambien use.
I’ve had fibromyalgia for 30 years and I had extremely severe insomnia for 16 years. I was on heavy sleep medication and getting physically worse and worse. As I was declining physically I was also waking up every two hours, unable to go back to sleep without sedation. I really thought I had reached the end of my life, especially as the sleep medication was stressing my body and making matters much, much worse. I tried to get help from an integrated sleep clinic but all they could offer was CBT. I knew my problem was not in the mind and that trying to access it through the mind was ridiculous.
Then somehow, as by a miracle when I was just about giving up, I discovered the world of Chinese herbs. For the first few months they helped me get much deeper and longer sleep. I had real trouble going to sleep so would take some Western medicines for that, however would then sleep 5-6 hours and another chunk of 2-3 hours after taking some more herbs. While on these herbs, I was able to cut down the Western medication to a bare minimum (a process I’d already started in the spring since they made me so sick). I was gradually feeling better. This was so exciting to me that I decided to take matters in my own hands, so started to study the world of Chinese medicine. I also worked with a Chinese practitioner for a while but have mostly found my own solutions. I have an aptitude for this way of thinking, which sees the body as a combination of matter and energy. So not only do I now understand why I have insomnia and how it all hangs together (what a relief), I have also been able to address the root problems that are causing it. It has been quite a roller coaster in the past few months but I’m starting to clear the root problems and once that’s taken care of, I expect my sleep will become normal.
I never found Western herbs useful, however the Chinese ones that have a sedative effect can be extremely powerful if used in the right combinations. Getting this right is tricky and I would of course recommend that people see a practitioner. Because of a tight budget and a feeling I could solve my own problems, I have mostly worked on my own and worked out a formula for the sleep that suits this kind of illness pattern. Though so many of these herbs are effective straight away and thus take care of some of the acute need for sleep, they also treat you long term. However, in order to cure the insomnia you will also have to address all the other issues in the body. For me, it has been a case of improving the digestion and opening up a lot of stagnated energies that have been troubling my heart. There have been massive improvements since I started all this in the summer, but I still need to clear my gut. At this speed, however, it shouldn’t take too long.
I appreciate that people think Chinese medicine is unscientific or strange, but it’s extremely deep and comprehensive and very logical. It’s a different way of looking at disease, and it makes 100% sense to me. I have been documenting my increasing insights and progress in a blog but it’s not easy for laypeople to read. Eventually I will try and summarise it all in a language more people can understand. However, if you want to check it out, the blog is called The Alchemy of Health.
Even if you don’t believe in this kind of approach, I would suggest you at least use the wonderful sleep herbs available for immediate relief. You can ask for a made up powder at Activeherb. They will also tell you if the formula is alright or not from a practitioner’s point of view. The herbs I’m currently using for my sleep are Fu Shen, Suan Zao Ren, Yuan Zhi, Wu Wei Zi, Bai Zi Ren with added Gan Cao. You could add Dan Shen too. This are herbs you can take a lot of without any fear of problems. These herbs are for people with pink or slightly red tongues with a thick yellow greasy coating. There are other sleep formulas based on these herbs that deal with different illness patterns. If you have a very red tongue you can try Tian Wang Bu Xin Dan and if you have a very pale tongue you can try Gui Pi Tang (two wonderful formulas that you shouldn’t use for too long, though). You can also get them as pills. As I said, you’d normally also take other herbs to treat the digestion, which is at the heart of fibromyalgia problems. The nervous system will calm down as a result. I have no more palpitations! :). I hope this helps someone out there. You need not suffer.
I also have had a very good experience with Chinese medicine for different symptoms of rheumatoid arthritis, fibromyalgia and cfs. I found out that in many states the schooling requirement for acupuncturists is only 2 years; in China it’s 5 years. That said even some Chinese acupuncturists try to cut corners. I’ve been advised never to go to a practitioner unless they will spend at least 45 minutes per session with a patient since some chronic ailments require that amount of time to treat properly. My Chinese-born and trained acupuncturist told me at the beginning that with the numerous problems I have it would take a very long time to get them all under control and he was definitely right but I’ve stuck with it and feel significantly better, about 90% of what I did before the cfs train-wreck destroyed what was left of my health. Thanks for your post V-M.
Yes, I have a deep seated mistrust of doctors in general and since I have a postgraduate background also of Asian studies and studying Chinese, I felt I should try and get my head around it by myself (an ambitious intent, but…). In the end I did work with Dr China, a chain of Chinese doctors (from China), for a while and as I was able to dissect the individualised formulas she gave me, I also learnt a lot about what a practitioner would recommend. Working with her got too complicated because I had to communicate via an assistant and was doing it mostly on the phone due to the distance. I believe it was all useful but then I felt confident to find formulas and modify them to suit my needs based on a lot of information found on the internet. Upon learning to understand my pattern, I realised that in spite of my shitty feeling and disability, my pattern wasn’t quite so complicated. I’d clearly kept it in some kind of check. I fully appreciate that many people, especially with ME, have a very difficult and complex pattern that takes a long time to heal. However, I am absolutely certain it is possible to get a lot better. My tongue has gone from extremely gunky with terrible sores to a healthy pink with only little left of the pathogens. I feel pretty full of energy, almost a bit too much so as the healing process isn’t entirely straightforward!
As I said below, I don’t think acupuncture is effective enough and should possibly only be considered as a complement to herbs. Herbs address the problem from two sides, energetic AND physical, and it will be 24/7. And yes, you do want to find a good practitioner, preferably a Chinese one though a Western one is probably fine too if they have good references. The time they spend with you isn’t necessarily an indicator but you have to feel that it’s right for you, depending on your psychological needs and complexity of syndrome (time is money too). I had a very intuition that the answer was in these herbs, and am ecstatic to have come off all the terrible medications that only make you worse. People often say they would prefer Western herbs but there is no in-depth tradition that also sees the herbs as a way of treating the energies (certain herbs enter certain meridians, etc). Here’s a little “declaration” I wrote >http://chronicillnesshealthissues.blogspot.co.uk/2014/10/converting-to-chinese-medicine-and-why.html
I’ve not had Chinese herbs for my sleep (I’ve been diagnosed with severe sleep apnea too) but have received the acupuncture treatments for that which helped a lot.
I have to say I don’t believe acupuncture is as good as the herbs for these kind of disorders. For one, you’re not usually getting it often enough. The herbs, on the other hand, you take two or three times a day. I hope you’ll give it a go even if you stick to a ready made formula!
Ambien is zolpidem, which is not a benzodiazepine and there is at least one study that suggests it may actually help memory consolidation. I don’t believe there is any data linking it to dementia. I’ve been taking 10 mg in four divided doses through the night for fibro for 15 years. While it is not quite as effective for me now and and while I am a bit drugged for an hour or two in the morning, I haven’t noticed any negative memory effects. I wouldn’t worry about prolonged Ambien use.
This article describes me perfectly. I have severe ME and pots. For the last 9 months or so I have been deteriorating big time. So has my sleep. I now cannot sleep for more than 10 mins at a time. Traditional sleeping tablets have no effect. One off high dose pregablin or low dose mirtazapine does occasionally help. I do not believe I have a co morbid sleep disorder. But I do have the snoring spouse who snores so bad she has sleep apnea!
Really good article.
“Notice that none of these are sleep aids, per se – they are all calming agents that help relax an edgy brain.”
***************
They may not be sleep aids, per se – but amitriptyline and doxepin are both potent antihistamines. The tricyclic antidepressants are third generation antihistamines. The discovery of antihistamines was followed by their use as tranquilizers. The most potent antihistamine, doxepin, is about 4 times more potent than amitriptyline, about 800 times more potent than diphenhydramine (Benadryl), and about 8,000 times more potent than desipramine.
Tricyclic antidepressants, Doxepin hydrochloride and amitriptyline hydrochloride may be the most potent antihistamines known, and the antihistaminic potencies of these and the other tricyclic antidepressant drugs may relate directly to their ability to cause sedation and drowsiness in patients.
Here’s an interesting paper, which supports the conclusion that a large fraction of depressions are responses to environmental molecules, and that the tricyclics are effective in many patients because of their antihistaminic properties, not because they act upon the serotonin or sympathomimetic amine pathways.
http://www.orthomed.org/resources/papers/hofdepr.htm
Amitryptyline and doxepin are both pretty “dirty” meds in that they impact lots of body systems. Having tried each for sleep, I will stick with zolpidem, not health food, but cleaner than these two IMO.
This isn’t about treatments, but I’ve found it interesting that I’ve had a sensitive system since childhood. My mom joked that had I been born in today’s times I “would have been diagnosed with something” :-). On and off through the years I’ve been ‘diagnosed’ with both chronic fatigue and depression. About 15 years ago my cardiologist said I have Mitral Valve Prolapse Syndrome (I have MVP), which is that sensitive system, constantly in fight or flight mode, etc. of which MVP is a marker, not the cause. It wasn’t until about 10 years ago that I crashed with fibromyalgia and the pain. What triggered that? Perhaps an upper respiratory infection I had right before; or environmental toxins that I had been exposed to around that time (I do think a course of zeolites did help with that). So in my case I feel I always had the type of system that was vulnerable to developing fibro/chronic fatigue…it was just timing for various triggering events to come together. Had I understood all of this better from the get-go, I likely would have made life choices more in line with the system I was born with rather than pushing my limits until I finally did crash. Education and understanding is so important!
As to the main topic of this article, I remember not sleeping well even in my teens. I do think finding the right medication, or combination of medicines and/or other treatments, is crucial to a more productive lifestyle. I have found, be it pain or sleep, that Jacob Teitelbaum is correct that very low doses of more that one med/supplement are often more effective than higher doses of just one.
Thanks Cort, another excellent article and good video by Dr Bateman. I agree we have to be like detectives in working out what are our precipitating factors that stop us sleeping. I’d suggest Dr Bateman also try the FDA cleared Microtherapy treatment with her patients. This is a great way to improve sleep quality without the side-effects of medication. It is effective and gentle. I have been using the Alpha-Stim for the past 5 years it has improved my sleep and stopped the wired and tired feeling 90% of the time. When it worked for me I wondered if the research was correct so 18 members of our FM & ME/CFS group also tried it and 16 of them found it also reduced their symptoms. I then re-registered as the Therapist (I’d been too disabled to work for 20 years)and set up a clinic in the UK to give others the chance to try this device. I’ve found the device helps 70% of those with FM and CFS that I see. I’m told it helps reduce central sensitisation and hormonal imbalance. I find it’s not so great for those with ‘pure ME’ as I feel there is more viral involvement. The Alpha-Stim ear-clips works because it can lengthen the time in deep sleep and reduce our over-active ‘fight and flight’ response by modulating messages going to the amygdala and hypothalamus regions of the brain.
Please see the following for insomnia studies http://www.alpha-stim.com/wp-content/uploads/2014/09/key-studies-in-insomnia.pdf
There have also been 4 randomised studies on fibromyalgia and the Alpha-Stim.
The last 2 can be seen:
http://www.alpha-stim.com/wp-content/uploads/CES_Research/CES-Improves-Symptoms-and-Functional-Status-in-Fibromyalgia.pdf
http://www.alpha-stim.com/wp-content/uploads/CES_Research/Brain-Processing-taylor.pdf
I’m so glad I gave it a go it has changed my life.
While, some drugs may initially help you sleep, antihistamines and antihistamine based antidepressants have the added bonus of actually curbing some ME/CFS symptoms, through the day, by dampening-down allergic reactions. Antihistamines allow me to take other supplements and medications to control my ME/CFS symptoms, that I normally wouldn’t be able to take because of my body’s constant over-reaction to anything and everything it deems foreign. If you believe your ME/CFS is caused by an overactive immune response sedating antihistamine base medicines may be beneficial.
Comments are great, especially the Chinese herb references, after you’ve learned the
usual Yada regimen
Comments are great, especially the Chinese herb references, after you’ve learned the
usual Yada regimen
Comments are great, especially the Chinese herb references, after you’ve learned the
usual Yada regimen
I’ve had insomnia for 20 years. I was diagnosed with fibro 15 years ago. I’ve had chronic headaches and migraines for 24. I take 10-15 mg of melatonin nightly. I have for 15 years. I take Unisom and Benadryl. I still can’t sleep.