A Different Approach
Younger’s been taking a very different approach to chronic fatigue syndrome and fibromyalgia than most researchers and he spoke about it in Pandora’s first webinar of the year.

Younger and some other ME/CFS and FM researchers are taking a very different approach to these illnesses.
We know that people with ME/CFS and FM regularly leave their doctors appointments with disappointingly normal results. But what if normal results actually spell trouble? What if the results are normal but the patient is not? What if the body is configured so that “normal” levels of a factor are, in fact, a real problem?
This idea has become something of a theme in ME/CFS research and it fits in with fibromyalgia findings as well. Miller’s basal ganglia work in ME/CFS suggests that dopamine depletion in the basal ganglia in the brain may be allowing small amounts of inflammation to cause “sickness behavior”. Gordon Broderick’s models suggest that the strange immune networks found in ME/CFS may be causing small concentrations of some immune factors to have immense results. Younger believes a constant state of activation is causing the microglia in ME/CFS and FM to respond to low levels of inflammatory factors.
The central sensitization found in fibromyalgia practically calls out for a situation like this. The difference with Younger’s research is that he thinks he’s found a substance in the blood that can help explain the central sensitization. If he’s right then he’s made a major breakthrough.
The Study
How to tease out normal test results that are not causing problems from normal tests results that are causing fatigue, pain, etc.? The answer is to disregard absolute levels of a factor and see if you can correlate fatigue levels with the levels of inflammatory factors. Younger had his participants measure their fatigue levels and take blood samples for 25 days and then he ran an analysis to determine which of fifty or more inflammatory factors correlated with fatigue.
Results
He found large fluctuations in day to day fatigue. Energy levels would spike up one day and then crash for a couple of days. Then another relatively good day would come along followed by a crash. Fatigue was always present – but the fluctuations were large.
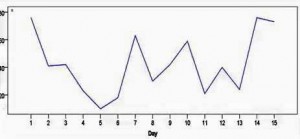
Fatigue levels that changed from day to day brought up the question: if fatigue can be reduced one day – why not the next?
He found some real hope in these fluctuations. If a person is physiologically strong enough to have a relatively good day then their body should be physiologically capable, after all, of having more of them. If you can figure out what is happening when everything is going right – and then duplicate that state – you should be able to maintain it.
(One wonders what’s going on a very different timescale with the relapsing/remitting group of patients – the patients who get a lot better, sometimes for years, and then suddenly and often dramatically relapse. What switch got turned on or off in them? )
Twenty-five days of blood draws sounds like murder. One can envision needle marks up and down one’s arm but Younger only needs a couple of drops each time and he uses really small needles which leave no marks.
Leptin – A Unlikely Candidate Shows Up
Younger first tried his twenty-five day fatigue measurement and blood stick trial on three women with fibromyalgia. Of the fifty or so inflammatory markers one popped out in all three women: leptin – a hormone associated with appetite regulation which on the face of it would seem to have little to do with fatigue or pain. Leptin levels are three times higher in women than men, however, and leptin promotes an inflammatory response: two factors that could explain why it’s having an impact in these disorders.
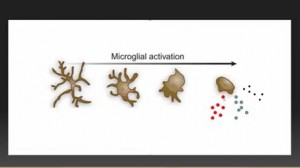
Leptin promotes the activity of the main immune agents in the brain – the microglia. Once activated the microglia change dramatically: they pull in their arms, assume a rounded shape and start pumping out inflammatory cytokines that produce the similar symptoms (fatigue, pain, sleep problems, cognitive problems, etc.) to those found in ME/CFS and FM. Younger believes the microglia in ME/CFS and FM are activated all the time.
Primed For Action
“It’s like you keep getting the flu without having an infection”
Animal research is showing that besides being in a resting or an activated state the microglia can also exist in a “primed” or hypersensitive state – ready to flood, at the slightest hint of danger, the body with fatigue and pain-causing chemicals. They can be put into this hair-trigger state in a number of ways: aging, immune insults, pathogens, taking opioids over long periods and chronic stress all appear able to put the microglia into a hypersensitive state.
The microglia can get so tweaked that they can begin to react negatively to endorphins, the body’s own feel-good chemicals, that get pumped out during exercise.
The Hypothesis
Leptin sensitizes the microglia. Hitting the microglia with leptin and then exposing them to a potential danger causes to them to start spewing out inflammatory cytokines like there’s no tomorrow. Younger’s hypothesis is that leptin in ME/CFS and FM is tweaking the microglia in the brain putting them in a flu-like fatigued, painful and cognitively challenged state all the time.
Next Step
First there were three – then there were ten. Younger’s next good-day, bad-day trial had 10 women with ME/CFS and more immune factors. Interestingly he excluded women with positive ANA’s (sign of autoimmune disease) and ESR and C-reactive protein (CRP) – two signs of inflammation.
In six out of the ten leptin levels strongly predicted how bad or good they felt every day.
The Great Graphic
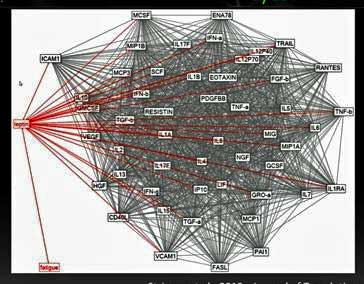
An entirely different type of analysis (thankfully :)) showed leptin popping out again. This analysis found that only leptin was directly associated with fatigue.
Dr. Klimas has done and is doing a different kind of good-day/bad-day study, but leptin didn’t pop out. I asked Gordon Broderick why? They simply hadn’t testing for it before – and why would they? Nobody suspected that leptin – a hormone usually associated with appetite and obesity – would play a role in ME/CFS. Leptin doesn’t even make much sense within an immune context – the immune factors it affects aren’t believed to play a role in fatigue. The only thing that makes sense with leptin within the context of ME/CFS is the microglia and leptins association with the microglia is just beginning to be understood.
Tight Fit Leaves Younger Confident
Younger’s “leptin” studies have included all of 13 people with chronic fatigue syndrome or fibromyalgia but the results were so unusually “tight” that he “very confidently” said – right now – that leptin plays a major role in producing fatigue in ME/CFS.
Younger’s “leptin” studies have included all of 13 people with chronic fatigue syndrome or fibromyalgia but the results were so unusually “tight” that he “very confidently” said – right now – that leptin plays a major role in producing fatigue in ME/CFS.
His hypothesis is that leptin is sensitizing the microglia to trick the brain into thinking an infection is present in ME/CFS. Encouragingly he doesn’t think any damage is being done to the brain – it’s just being tricked into producing these inflammatory products. This process is not producing sore throats or runny noses – that’s an entirely different process; Younger is referring to brain produced symptoms such as fatigue, pain, cognitive, sleep and other issues.
[Why it’s doing this in ME/CFS and FM patients is question Younger did not go into. Leptin was not correlated with fatigue in the healthy controls; i.e. it’s not causing fatigue in them. It may be that an infection or stress or whatever has put the microglia in ME/CFS and FM patients in such a sensitized state that leptin is sending them over the edge. Or it may be that leptin is interacting differently in ME/CFS and FM patients than it is in healthy controls. One wonders how leptin fits into Broderick’s immune networks….]Treatment
Turning Off Leptin
Younger cautioned that he’s not recommending any potential leptin antagonists. If leptin does turn out to be it in ME/CFS and FM there are a number of ways to block it. The problem is that wiping out leptin could have major implications on our ability to fight cancers and block infections. Besides – you’d feel like you were starving all the time.
There are some ways, though, you may be able to safely reduce your leptin levels – at home.
Reducing Leptin Levels
- Fasting – for a few days reduces leptin levels dramatically (not recommended for ME/CFS/FM).
- Meditation/Mindfulness Practices – Since stress increases leptin levels anything that reduces stress should reduce leptin levels
- Losing weight – since leptin is produced by fat cells reducing the number of fat cells in your body should reduce your leptin levels
- Low glycemic diet
Calming Down the Microglial Cells
A better approach would be to calm down the microglial cells so that they’re not over-reacting to the leptin in the first place. A long list of potential microglial inhibitors are available and a really intriguing one was just added to the list; the antiviral ganciclovir (valganciclovir or valcyte) was just found to knock down microglial activity.
Younger has a grant to study nine botanicals in Gulf War Syndrome.
Younger’s ME/CFS and FM Studies
New Immune Monitoring Study
The NIH is funding a much bigger 25 day immune monitoring study that will start in a couple of months. You should be within in an hour of Birmingham, Alabama to participate in this study..
Leptin Study
People will be given an injection of leptin to see if it causes more fatigue. Since leptin leaves your system quickly, if it does increase fatigue it will only increase it temporarily. This study probably begins in one month. This is an ME/CFS study, but if you have fibromyalgia and haven’t been assessed for ME/CFS you may be eligible.
PET Scan Study
To assess neuroinflammation in ME/CFS. The study will probably be done at Vanderbilt University in Tennessee.
Low Dose Naltrexone for ME/CFS
This study will probably start later this year.
Neuroinflammation, Pain and Fatigue Lab
The lab at the University of Alabama at Birmingham is growing rapidly with twelve people now working in it. Sign up for updates here.
Support the Research
Donate to Younger’s leptin ME/CFS research in a tax deductible manner by funneling it through Pandora, a non-profit organization here. A hundred percent of your donation goes to Younger’s research.
- Dr. Klimas is next up on Pandora’s webinar program.
More on Dr. Younger’s ME/CFS and FM Work
- New Chronic Fatigue Syndrome and Fibromyalgia Lab Opens: Jarred Younger Talks
- Successful Low Dose Naltrexone Fibromyalgia Trial Points to Safe, Low Cost Therapy; Implications for Chronic Fatigue Syndrome








Interessant ! Je suis EM sévère, et mon taux de leptine est 3 fois supérieur à la normale … Même si je ne pense pas que ce soit la cause ,mais une résultante !
Interesting ! I am severe ME sufferer, and my leptin levels is 3 times higher than normal … Even though I do not think this is the cause, but a result !
Ha! Younger’s study in which he gives people leptin and sees what happens should at least partially decide that answer….
It’s a great question 🙂
Very interesting stuff. More and more clearly, microglial activation appears to key to our disorders.
Want to point out that ganciclovir is not the same drug as valganciclovir, though they are closely related. Valganciclovir is a pro-drug that is converted to ganciclovir in the body. Presumably, therefore, it would have similar effects on the microglia.
By the way, did you notice that this article about ganciclovir and microglial inhibition (Antiviral drug ganciclovir is a potent inhibitor of microglial proliferation and neuroinflammation
Journal of Experimental Medicine, 2014, vol 2, p 189-98.) was submitted in MARCH 2012 and published in FEB 2014?!
Also, I found reference from 2005 (Nature Medicine 11, 146 – 152 (2005) Experimental autoimmune encephalomyelitis repressed by microglial paralysis) that clearly demonstrates that ganciclovir is a microglial inhibitor. That was 10 years ago.
Not sure what my point is.
Thanks for your work.
The link said a list of drugs and botanicals but no botanicals were listed. I would be interested in seeing a list of botanicals.
Sorry about that Mary – I just put the botanicals in now – http://www.cortjohnson.org/treating-chronic-fatigue-syndrome-mecfs/drugs-for-chronic-fatigue-syndrome-mecfs-treatment/microglial-inhibiting-drugs-combat-neuroinflammation/
yes, I mentioned the ganciclovir study to Cort a week or so ago 🙂
I also asked if Cort could mention it to Younger since he knows him. I emailed Younger’s clinic weeks ago but no response.
Any chance Cort? We need to push these researchers a bit.
There seems to be strong evidence that ganciclovir inhibits microglia, SO WHY NOT STUDY IT IN CFS?
More action, less talk and theorizing.
🙂 I am going to do a blog on this very bit of interesting information you found…Valcyte’s a pretty heavy duty drug – it may take awhile to get a study – but it should get more people thinking about the microglia..
One point. As far as I know, outside of liposuction, dieting doesn’t reduce the number of fat cells, just reduces their size.
This is fascinating and really promising. Great work! Thanks, this is just what I needed today.
Often, the hardest things to discover are the most obvious. Younger looked at what was there and what fluctuated with fatigue. Seems to a be a no-brainer (no pun intended).
I would bet that if significant, this is only part of the picture. But a good start. What seems kind of contradictory is that leptin increases in pregnancy. Since many CFS/ME patients feel better during pregnancy, I wonder what makes the difference.
What’s particularly convincing is a seeming explanation for why doing the same physical activity on different days could produce such different results. Also, that leption responds to emotional stress, a frequent trigger for symptoms.
Could the different results from physical activity be related to the intensity of the physical activity? Both Cort Johnson and I believe that strict pacing of physical activity has been very beneficial for us. The post-exercise malaise syndrome is triggered by physical activity beyond a certain threshold, but not below that. Possibly heart rate is a guide – keep it from going anaerobic?
Trying to run for 1 minute will cause me pain and stiffness for a week. But I can walk for hours with no ill effects. A daily routine of varied exercise of strictly moderate intensity has become very good for me – for years I was always overdoing it, if even for only 1 minute, almost every time I took some exercise.
Interestingly, I have also been low-Glycaemic diet for a year now and have lost 30 kgs although that loss has plateaued at a level that is still far too high for my height.
It actually does not seem far-fetched to me that a hormone involved with appetite regulation might play a role, because appetite is one thing that has always been messed up with me. I have assumed hypoglycaemia – carb cravings – because I could have indigestion from eating too much, and hunger pangs, simultaneously. Going on the Atkins (very low glycaemic) diet burns off this withdrawal symptoms type of craving after the first 3 days of severe withdrawal symptoms. But it certainly did not reduce fibro pain related to post-exercise malaise sydrome – what has slowly been doing that for me, is careful pacing. It is taking months for the very long-established pains in the shoulders, elbows, legs and neck to go away, but they are going away. I have just become able, for the first time for years, to squat down on my haunches without unbearable pain.
How great that you have found such improvement from pacing and diet. I agree about a low glycemic diet. I had similarly great results before other cfs/me-related health issues forced me off of it. I was on one with lower fat meats and also have hypoglycemia.
Pacing works for me with only a few activities, like walking. But my frequent, long and severe setbacks too often revert my progress. I haven’t gotten very far before reversals. I am on the severe side of the illness, though.
As for the difference day-to-day, it’s a good thought about the intensity, but unfortunately it doesn’t apply. Small things like being able to lift my Brita water pitcher vary by the day. One day, I lift the pitcher from counter to table, with no problems. Another day, I can barely lift it. Even with other factors, like physical activity, being the same. It’s bizarre, because I know it’s not deconditioning.
With movements like the squat, how would one pace if even one squat produces days (or weeks) of pain? How did you figure out that you were overdoing it, even if for one minute? Heart rate?
I think you are exactly onto the important questions about this.
“…how would one pace if even one squat produces days (or weeks) of pain…”
Exactly! This is a terrible dilemma.
I did careful squats IN WATER, or with my weight supported by a pulley on a gym exercise machine.
“…How did you figure out that you were overdoing it, even if for one minute? Heart rate?”
For me I think the indicator is a rapid descent into breathlessness. It is humiliating to be absolutely fine, with an impressive level of moderate output for long periods of time, but increasing the exertion turns one into a panting, heaving, flushed and sweating “couch potato trying to play athlete” within one minute. But one single squat, which does not take more than a few seconds, also did this to me. Yet I can do a seated leg-press of 3 times my own (high) weight! It is also humiliating to be a “big man” with known STRENGTH and yet NO STAMINA when the going gets tough.
Why such strong leg muscles and yet inability to squat? I believe that myofascia tension and lost elasticity causes important blood flow to be shut off by squatting. I believe this is also implicated in the inability to sustain any effort above a certain threshold for long eg running. It is like a car with a large V8 engine, having a carburettor with a constricted throttle passage – that is the tight, stiff myofascia constricting blood flow at the immediate interface with the muscles themselves. The big arteries are probably OK. At low power requirements, I can tick over lazily all day.
Something else that overloaded me, was climbing any stairs or inclines. However, taking it SLOOOOW was the solution.
I am extremely sympathetic with anyone whose threshold is so low that they can hardly do anything; I wonder whether my conclusions about myself are relevant to those far worse off, or whether they too somehow need to “pace” at incredibly low intensity. I see it as a vicious circle, where the more inactive you are, the further your threshold falls. I believe I am moving my threshold up by doing a LOT of paced activity.
A lot of the medical advice I got all along – since more than 20 years ago – involved “don’t drop out of life, stay active, use it or lose it”, and so on. But no-one told me about pacing and overdoing it. This is the missing part of the advice – it is true that you must use it or lose it. But you must stay within the threshold or you are harming yourself. I read this advice on this blog, only a few months ago – which was the first time I had encountered it. This blog is amazing.
I hypothesize that some very unfortunate people have been rendered inactive by overdoing it, for too high a proportion of their time, so that their threshold has fallen over time, and they have gone down in a vicious circle of lesser and lesser activity exceeding the threshold and rendering them inactive again. Is it possible to build up again from the bottom? It is your own experiment to conduct – I would love it if my story does result in a breakthrough for others.
“…It’s bizarre, because I know it’s not deconditioning…” – but could it be that you did overdo it in some other activity, even the day before – and not even realised it? I did not even realise it when I was simply trying to run for 1 minute during each of my regular walks! The deceptive problem is, the pain and stiffness and limitation doesn’t really set in until hours later, and especially after the night’s “sleep”. While you are still up and moving, even if you got breathless for a few minutes, you SEEM to have recovered, and simply get on with the rest of the day. It is when you stop and sink into a chair or bed, that the “post exercise malaise” sets in. The longer you are sitting or lying, the worse it feels when you try and get up again.
It is that “getting breathless for a few minutes” that is the sign to me that uh-oh, I am in trouble now for a few days…. So you need to take whatever activity it is that is doing that to you, slower (and if you can’t, you have to do something else altogether like getting a labour-saving device).
I also hypothesize that chronic stress is what causes the problems in the myofascia to begin with, so if you cannot resolve the chronic stress, it may be very hard to restore condition. I hold that I owe a lot to a total career change. I have also adopted a “middle finger” life strategy regarding “friends” whose “kind” advice is that I am a hypochondriac. I refuse to let myself miss them. They are monsters, end of story. They need to reform themselves, not me. They cannot possibly “know” I am a hypochondriac. I can and do know that they are charlatans, with their claim to God-like all-knowing status. In a different time and place in history they could have been something determinably evil – eg in a theocracy or a primitive pagan system or a totalitarian political system.
Phil, thank you. Had a bad few days. Will respond tomorrow.
Your water strategy helped. Even though water makes my symptoms worse, I know that the key is having a person or mechanism take some of the exertion from you. Maybe an OT could help.
I don’t know that the same exact strategies are relevant or that I could make as much progress, but the basic principles you’ve relayed have already helped me see the problems differently. I know that I’ve got some different questions my doc. It helps to get a fresh eye.
Myofascial theory is interesting. I know that myofascial massage, if gentle can help me. What really helped me was spinal alignment in my neck. The problem I described with the water pitcher as an example, the strength returns when my neck is aligned and the base of my head is in the proper position. On days when I lose strength, my neck and head are having problems. Unfortunately, congress keeps cutting and adding loopholes to medicare’s PT coverage.
I can totally relate wrt to those types of friends. I’ve had to cut out some myself. Really painful and stressful, but necessary. It’s hard to cut out stress, because by its nature, stress is often out of one’s control. My biggest problem wrt to setbacks seems to be the infections. Getting one can set me back months or more. Thank you for your detailed help!
I am thrilled if my experiences, passed on, help others – I picked pretty much everything up from others in the first place myself.
I too had some really good spinal manipulation on and off over the years, and the osteopath who does it, has seen me improve dramatically and spread out the intervals with which I visit him – about 6 monthly now. So this too could be a key ingredient for me.
Finding great practitioners whose approach really fits your need at the time, is a Godsend. Looking carefully at their websites and what they say about their experience and approach to different problems, can help you find the best ones. For years I know I wasted money on treatments that were actually pointless – like deep tissue sports massages, for example. Or quick and cheerful manipulations from a practitioner who is not a real guru. Or supplements that are of little benefit for fibro, just because they are the magic bullet of the moment for some friend or magazine writer.
I can understand the stress and the infections are likely related, I was incredibly fortunate that a major career change worked out for me, and is low stress while providing an adequate income.
I also stopped getting throat infections after I got a CPAP machine for sleep apnoea; I think everyone with fibro needs to be sure they have not got sleep apnoea as well because it is probably impossible to make much progress if you do have it undiagnosed and untreated.
I wish you all the best.
Thanks for your comments, Phil. I too have found much benefit from pacing, despite being at the severe end of the spectrum. The key for me has been letting go of any kind of “normal” frame of reference in regards to what constitutes exercise. Squats are no go… but very gentle yoga postures, while lying down (& sometimes seated), have been beneficial. Especially using Klimas’ 3 mins on-3 mins off (light bulb moment when I learned of that). Some weeks even that’s too much, and I don’t do it. But it’s felt empowering to find some movement that is safe for my body… and my muscles feel used, which is actually quite lovely
We’re going to have a really intriguing blog on Dan Moricoli’s amazing improvement over time using very simple methods – and very rigorous pacing.
Thanks for your comments, Phil. I too have found much benefit from pacing, despite being at the severe end of the spectrum. The key for me has been letting go of any kind of “normal” frame of reference in regards to what constitutes exercise. Squats are no go… but very gentle yoga postures, while lying down (& sometimes seated), have been beneficial. Especially using Klimas’ 3 mins on-3 mins off (light bulb moment when I learned of that). Some weeks even that’s too much, and I don’t do it. But it’s felt empowering to find some movement that is safe for my body… and my muscles feel used, which is actually quite lovely
Phil,
I love what you said here: The deceptive problem is, the pain and stiffness and limitation doesn’t really set in until hours later, and especially after the night’s “sleep”. While you are still up and moving, even if you got breathless for a few minutes, you SEEM to have recovered, and simply get on with the rest of the day. It is when you stop and sink into a chair or bed, that the “post exercise malaise” sets in. The longer you are sitting or lying, the worse it feels when you try and get up again. “
by night i can do nothing else and have to become a couch potatoe and watch tv only. even reading it out. it’s like my cells begin to really suffocate and lead fills my body. this happens each night with or without any exertion though. perhaps everyday i exert past my limit.
i still have an active middle finger for the arrogant “friends” who think they have answers for me…assumptions which their heartless judgements are based on.
Same with me! I can get through exercise OK – at least the first time – I even feel better! And then over time everything seems to contract! Muscles tighten and stiffen. Exhaustion sets in. I have trouble thinking. Sometimes I have more problems with OI.
Oddly enough that same feeling is more common when I wake up….
Cort,
likewise upon waking. it’s murder! and i have a very enthusiastic cat who wakes at the crack of dawn and gets the party rolling early!
it takes awhile to get into the day. i think for me this also has to do with low cortisol (despite taking HC, i still deal with this). i just added in one cup of green tea to help with it. i know i shouldn’t but i need relief too.
Something else I just thought: every time I have a serious setback, I gain weight for no apparent reason. Every time I recover (somewhat), I lose weight for no apparent reason. Same routine, same foods. Each time, the weight increase or reduction starts a bit of time before I start feeling worse or better. Leptin’s connection to fat is interesting. Maybe the increased leptin is one indication of an already-initiated process.
So this is why LDN works, to help relax the leptin response?
I think that’s the idea: LDN reduces microglial activity which means the microglia are less responsive to leptin and stop pumping out inflammatory mediators that cause fatigue and flu-like symptoms when it’s around.
Of course it will take some more testing to validate it 🙂
I have been on LDN for a year and I have FMS but CFS could be there as well. That just hasn’t been diagnosed. I have slowly ramped from .5mg up to 3mg then jumped to 4.5mg for a while then went back down to 3mg, which I have been at since August. I would only know for sure if it is helping if I stopped it because to tell you the truth, I still feel pretty crappy! I was hoping for more with this drug. Maybe I just haven’t found the right dose yet.
Thoughts?
Been a while since I studied up on LDN but I thought 5mg was the dose to shoot for…. marcie
Hi,
The print button doesn’t print out the whole article; can that be fixed?? Thanks!
Mary
Darn! I don’t have a printer here. Can you tell me where it gets cut off?
Sure, Cort. The last section of this article that is printing is “The Great Graphic”. Nothing after this section will print when using the print button.
Thank you!!!!!!
I don’t have a printer hooked up either, but have you tried selecting the text from the top of the article to the bottom, then right-clicking on the selection and picking “print selection?” The print pop-up box usually also has a “print selection” choice, if you can’t do it through the right-click menu. This method prints the text, not the internet page. Might get around a format glitch.
Worth a try.
Thank you! It was fixed, so didn’t need to try your suggestion.
I think this might be a very important realization. Ever since I became i’ll I’ve had a problem with getting cripplingly hungry at completely random times with no rhyme or reason.
It’s a weird thing – sometimes it happens to me when I’m clearly full…
Absolutely! I can suffer indigestion and hunger pangs simultaneously.
I get that too. My blood work showed I have a hyperinsulemic (is that a word?) reaction after eating carbs which leads to hypoglycemia.
I have gastroparesis and my blood work shows that my insulin is aggressively released after eating carbs, leading to hypoglycemia after a meal. Just throwing it out there! It is less of a problem when I eat more fat and protein but I still have the symptom.
What is the connection between microglia into a hypersensitive state and the ANS dysfunction?
That’s the question I would have asked him if I had made the webinar.
My heart rate stays around 124 as if I’m always exercising but I still have good and bad days. I’m sure my kept in is all over the charts.
Do you think they will do a study in the future for those with autoimmune disorders (I have Hashimoto’s thyroiditis and possibly rheumatoid arthritis)?
Also, I asked one of my doctors (a psychiatrist that hersellf has fibromyalgia) if I could try LDN and she said that she tried it on one patient, and told me “it doesn’t work” (her words)!
Wow – a doctor relying on a sample size of one to decide if something works – that’s not very encouraging.
I think Younger will probably focus on ME/CFS and FM first but you might want to check Pubmed and see if any research is being done on leptin and autoimmune disorders. Since it’s an inflammatory compound it’s possible there may be some.
Hi Sara,
I have rheumatoid arthritis, and am on medication for hypothyroidism. I am gradually building up to a therapeutic dose of LDN (currently 1.5 mg). Although I have not yet experienced an improvement in my ME/FM symptoms, I noticed a lessening in the stiffness of my hands at a dose of only 1 mg.
I realize everyone is different in their response to various medications, but it seems worth trying LDN for your particular medical issues.
Really interesting. Glad he’s doing a naltrexone study. I’ve been on LDN about 6 months. It’s made a huge improvement in my stamina. remarkable.
Ahmo – are you at the point where you can exercise?
What dose are you on? marcie
Hi
I’m trying to find people who are willing to have their case histories written up for publication in a medical journal. I’ll include my own story as I responded very well. Would you be interested?
the gut (lps, bacteria), stress (emotion), exercise, chemicals can activate primed microglia. But what makes microglia primed in the first place. Or is there another reason why these microglia are active? Primed microglia sounds very vague…
Thanks for the follow-up summary, Cort. We really appreciate it. I’m looking for great things coming from his studies. The webinar was recorded, so if anyone missed it they can view it here: https://www.youtube.com/watch?v=bFwAyrb5p34
Maybe he should speak to Ritchie Shoemaker first. He’s been talking about leptin issues in “CFS”, lyme and mold illness for quite a while now.
http://jackkruse.com/hey-lyme-disease-meet-leptin/
Indeed. We can laud Dr Younger for great work, he deserves it, but Dr Shoemaker beat him to the whole leptin thing several years ago. To say nobody could have anticipated leptin’s role in inflammation in neuro-immune disease is a bit of a slap to Shoemaker and the many practitioners who follow his work and implement similar protocols.
The best part of this is that a large percentage of patients who suffer from ME/CFS and fibromyalgia improve with avoidance of mold and detoxification. A greater percentage, I would say, than with any other single treatment. Which isn’t to say mold is the only factor driving leptin, but I do think it’s the primary one. Yet, for whatever reason, this approach has been marginalized by our community. Hopefully Younger’s work brings it to the mainstream.
This study sounds really great!
I had similar thoughts as I was reading this article.:
“I sure hope Dr. Younger has read Dr. Shoemaker!”
Leptin plays a part in the inflammatory cascade in the immune system that Shoemaker figured out years ago.
Cort, Dr. Ritchie Shoemaker describes in his books the tests he uses to monitor his treatment of mold- illness patients — and one of the key tests is leptin. Going from memory, I believe the higher it is, the sicker the patient.
I wonder if there’s a connection?
Cort, Dr. Ritchie Shoemaker describes in his books the tests he uses to monitor his treatment of mold- illness patients and one of the key tests is leptin. Going from memory, I believe the higher it is, the sicker the patient.
I wonder if there’s a connection?
really interesting article on inflammation and depression….and guess what MICROGLIA:
http://www.prohealth.com/library/showarticle.cfm?libid=19515
It’s nice that he thinks brain damage isn’t occurring from these inflammatory factors, and I hope so!…but what about the Stanford (Zinn’s I believe) study on right arctuate fisculus (?) and damage. I believe in the subjects they studied there was reduced white matter. Looking forward to Dr. Klimas’ Pandora presentation!
‘internal ionisation radiation injuries’ with ‘broken cromosones & translocations’ are the cause of CS Fibro Lyme Syncope Autonomic Dysfunction Reflex Sympathetic Dystropy ‘labels’ yes Labels given to CFIDS including numerous Cancers & all Auto Immune Disorders none of these Research Lunatics will come up with any answers unless they are trained in Radiobiology injuries anti virals antibiotics will not correct radiation it is impossible to get rid of these from the body this is identical illness to so called P.T.S.D./Gulf War Illness it is also what Chernobyl victims will slowly die from over decades with radiation injuries…Time for Private Commercial Lien Lawsuits under Uniform Commercial Codes of Laws Roman Cannon Laws God’s Laws not Admiralty b.s.merchant sea laws…Time for damages in the Millions of Dollars to the N.I.H./C.D.C.WHO/U.N/Nuclear Industry including Peter White/SimonWessely ‘the weasle’
Canadian scientists say they’ve made a big breakthrough in depression research with a new study that found activation of the immune system causes sickness behaviors that present during a major depressive episode, such as low mood, anhedonia, anorexia, and weight loss. Second, peripheral markers of inflammation are frequently reported in major depressive disorder. Third, neuroinflammatory illnesses are associated with high rates of major depressive episodes.
This finding provides the most compelling evidence to date of brain inflammation, and more specifically microglial activation, in MDE. This finding is important for improving treatment because it implies that therapeutics that reduce microglial activation should be promising for MDE. Researchers are already starting trials to test whether anti-inflammatory drugs may one day serve as anti-depressants.
http://www.ctvnews.ca/health/study-finds-link-between-depression-brain-inflammation-1.2210121
The findings were published Wednesday, January 28, 2015 in the journal JAMA Psychiatry.
Role of Translocator Protein Density, a Marker of Neuroinflammation, in the Brain During Major Depressive Episodes
http://archpsyc.jamanetwork.com/article.aspx?articleid=2091919
L
It is thought prozac is effective in depression and sometimes CFS (has been very good for me) because in reduces microglia activation.
I’ve read a little bit about leptin resistance. I would guess some of us have it, which could explain overeating due to leptin not being available to signal satiety.
My appetite during the day is nonexistent but I am ravenous at night. Could leptin levels vary that way? Regarding those who lack an appetite, could leptin resistance explain it?
I’m just wondering about these things and lack the background to understand the role of leptin and mechanism of leptin resistance. The experts probably don’t understand it either.
I also have little appetite during the day: cannot eat breakfast, eat a light lunch. About 5pm I get hungry, have a few nuts, we have dinner at 7pm. I put lots of veggies on the table, good thing, because as soon as I sit down, I am ravenous and gobble most of them down with a moderate portion of protein. Must moderate protein, I have only one old, diabetic, kidney. Then it is eat, eat, eat until I go to bed. By eating more veggies, mostly dropping ice cream and other dairy and switching the night snacking to popcorn, which I am not crazy about, I have managed to lose 50 pounds over more than four years. I gain every winter, so I have probably lost close to 80, even 90, pounds over that time period. Unfortunately, my ability to exercise has been lost, tho I now just try to sit less over the course of a day. I am always tired, always hurt, have little or no stamina, lots of brain fog. I take one tramadol, one norco a day, hold the opioids down but cannot further decrease, so no LDN. At 77 one might say what else did you expect? But I have friends the same age, or older, without fibro, who can do so much more. As I used to be high energy, fast thinking, I feel the loss deeply. I do meditate, but that is more to accept who I am now and move forward with it. The research is very interesting in light of my lifelong problems with weight.
Leptin is tied to orexin which controls sleep… never hear much about orexin unless your in the narcolepsy community!