“the present findings offer clinical implications that may serve to guide future studies of the pathophysiology and management of a variety of persistent pain conditions.” Loggia et. al.
Chronic pain was thought for many years to be mostly a neuronal problem. Over or underactive neurons in the spinal cord or neuronal pathways in the brain were creating problems with pain processing – causing an overly robust pain response.
A new player, the microglia, entered the pain field about ten years ago. Among other activities the microglia direct the immune response in the brain and spinal cord. In the past ten years numerous animal studies have incontrovertibly determined that over-active microglia play a critical role in producing chronic pain states.
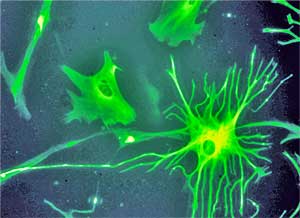
Nerve injury can cause glia cells to proliferate producing perhaps an infrastructure for producing pain.
Studies indicating that a nerve injury causes the microglia to proliferate tremendously suggest that an initial nervous system insult could, in some people, produce a kind of microglial infrastructure for pain and fatigue. By pumping out pro-inflammatory factors that activate pain producing pathways, the microglia could be the spark that keeps the fire, to speak, burning in the brain. Microglial activation by itself is able to induce allodynia in laboratory animals. Animal studies suggest that reducing microglial activation could delay or even prevent the formation of nerve pain.
Despite the great promise that microglial (and astrocyte) activation has shown in helping to explain how chronic pain occurs no one has been able to validate the role they play in producing chronic pain in humans.
The problem has been technological; until recently the technology to detect microglial activation without an autopsy simply wasn’t available. The development of molecules or ligands that bind to proteins associated with microglial (and astrocyte) upregulation is enabling researchers to get a hand on microglial activation. (Astrocytes – a form of glial cell – may be as important as the microglia in the production of chronic pain).
The molecule used in this study – TSPO – is increased in a wide variety of neurological disorders including multiple sclerosis, HIV encephalitis, ischemia and some types of arthritis. TSPO, a microglial inhibitor, is believed to reflect the brain’s attempts to rein in the microglia. Last year we saw Japanese researchers using a different molecule to assess microglial activation in ME/CFS.
Jarred Younger has noted that the technology is not perfect. Last year we saw Japanese researchers using an older version of the same molecule to assess microglial activation in ME/CFS. (They are using the newer molecule in their present study – thanks to Simon McGrath for reporting that). Younger is attempting to use scanning techniques that can assess the degree of neuroinflammation present by measuring the temperature of the brain.)
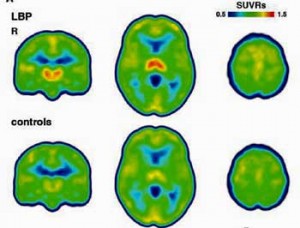
In this study – the first of its kind done in humans – U.S. researchers examined microglial activation across the brain and cytokine levels in the blood in nine people with low back pain and nine healthy controls to determine if and where microglial activation might be causing pain.
Evidence for brain glial activation in chronic pain patients Marco L. Loggia,_ Daniel B. Chonde, Oluwaseun Akeju, Grae Arabasz,Ciprian Catana, Robert R. Edwards, Elena Hill, Shirley Hsu, David Izquierdo-Garcia,Ru-Rong Ji, Misha Riley, Ajay D. Wasan, Nicole R. Zurcher, Daniel S. Albrecht, Mark G. Vangel, Bruce R. Rosen, Vitaly Napadow and Jacob M. Hooker BRAIN 2015, doi:10.1093/brain/awu377
Results
“Demonstrating glial activation in chronic pain suggests that these cells may be a therapeutic target, and the consistency with which we found glial activation in chronic pain patients suggests that our results may be an important step towards developing biomarkers for pain conditions,” Marco Loggia
Microglial activation was found most prominently in the thalamus and the somatosensory cortices. Consistently upregulated microglial activity in the thalamus suggested that this important relay center for pain and other sensory signals played a particularly prominent role in the production of chronic pain.
The Japanese research effort found evidence of neuroinflammation in ME/CFS in several of the same brain regions ( cingulate cortex, thalamus) plus some new ones ( hippocampus, amygdala, midbrain, and pons). With microglial activation in the thalamus associated with reduced cognition and increased pain in ME/CFS, inflammation in the thalamus may play an important role in both ME/CFS and low back pain.
One study has found increased thalamic activity in ME/CFS and depressed patients with ME/CFS patients demonstrated more thalamic activity. Several studies suggest the thalamus may play a role in fibromyalgia as well.
Other areas of increased microglial activation included a variety of brain regions often associated with ME/CFS and fibromyalgia including the insula, prefrontal cortex, cingulate cortices, the supplementary motor area and the basal ganglia.
Treatment
“By showing that levels of an inflammation-linked protein are elevated in regions known to be involved in the transmission of pain, the study … paves the way for the exploration of potential new treatment strategies and identifies a possible way around one of the most frustrating limitations in the study and treatment of chronic pain — the lack of an objective way to measure the presence or intensity of pain.” Mass General Hospital
The authors – from Harvard and Duke Universities – asserted that now that microglial activation has been associated with chronic pain production in human that clinical trials of microglial inhibitors should begin immediately. Known microglial inhibitors have been FDA approved for other conditions.
The authors pointed to low dose naltrexone fibromyalgia studies as evidence that microglial inhibition works
The first drug they pointed to, interestingly enough, was none other than low dose naltrexone, a known glial cell inhibitor that two Younger studies have shown can reduce pain in fibromyalgia. They noted that two other putative microglial inhibitors (propentophylline, minocycline) have not panned out in two chronic pain trials but, pointing out that it’s easier to prevent microglial activation than knock it out, they asserted that the trials may have been too short (8 days to 4 weeks) to show efficacy.
This study should start the ball rolling on increased efforts to reduce chronic pain by reducing microglial activation. A surprising finding that the patients with the highest TSPO levels had reduced pain added TSPO enhancing drugs to the list of new possibilities for reducing pain. Younger’s Neuroinflammation, Pain and Fatigue Lab is currently testing how effective botanicals are at reducing microglial activation in Gulf War Syndrome. Younger has elicited some surprise at how effective some of the botanicals may be. (Subscribe to his newsletter for updates).
More on Possible Microglial Inhibitors
- Check out a long list of putative microglial inhibitors
- New Chronic Fatigue Syndrome and Fibromyalgia Lab Opens: Jarred Younger Talks
- Palmitoylethanolamide (PEA) – A Medical Food for Fibromyalgia and (ME/CFS)?
- Drug Repurposing I: Antibiotics to Reduce Microglial Activation in ME/CFS and Fibromyalgia?
The microglial field – already a hot one – should heat up more now that pain has been linked in human studies to microglial activation.
Many labs are engaged in finding ways to accurately assess microglial activation and neuroinflammation. At least three studies testing marker of microglial activation (GEH120714 (18F)), ([18F]DPA-714), [C11]PK-1195 PET) are underway. Ultimately scanning techniques should be able to pinpoint patients for whom reducing neuroinflammation makes sense.
The authors asserted that treatment trials using microglial inhibitors should begin now. Only minocycline, however, shows up in a search of the Clinical Trials database. As noted earlier, Younger is examining the efficacy of botanicals in a Gulf War Illness study.
With microglial inhibition, Dr. Pridgen’s antiviral approach to Fibromyalgia, immune therapies and brain stimulation all on the table now, researchers are getting more creative in their approach to reducing chronic pain.
- Drug Combo in Pridgen Antiviral Fibromyalgia Trial Identified
- Symposium Calls For Use of Immunotherapy To Treat Chronic Pain








Bring on the research!
Cort, do you have a study reference for this “Animal studies suggest that reducing microglial activation could delay or even prevent the formation of nerve pain.”?
Imagine millions of people awakening from their nightmare lives of pain and running back into life.
Here are the studies cited in the paper but I imagine there are more recent ones out there. They state “Although a plethora of animal studies has demonstrated that glial cells are involved in the establishment and maintenance of persistent pain, no study has previously demonstrated in vivo glial activation in humans suffering from chronic pain.”
Note that it’s going to be more difficult to turn off the microglia once they’re activated than stop them from turning on in the first place.
Ledeboer A, Sloane EM, Milligan ED, Frank MG, Mahony JH,
Maier SF, et al. Minocycline attenuates mechanical allodynia and
proinflammatory cytokine expression in rat models of pain facilitation.
Pain 2005; 115: 71–83.
Raghavendra V, Tanga F, DeLeo JA. Inhibition of microglial
activation attenuates the development but not existing hypersensitivity
in a rat model of neuropathy. J Pharmacol Exp Ther 2003; 306:
624–30.
You’re always so fast with the new research, Cort, and this looks really interesting
Clarification:
“The molecule used in this study – TSPO – is increased in a wide variety of neurological disorders including multiple sclerosis, HIV encephalitis, ischemia and some types of arthritis. TSPO, a microglial inhibitor, is believed to reflect the brain’s attempts to rein in the microglia. >>Last year we saw Japanese researchers using a different molecule to assess microglial activation in ME/CFS.”
This study used 11C-PBR28 as the radioactive tracer binding to TSPO; the Japanese studie used the ‘older’ 11C-(R)-PK11195 radioactive tracer, also binding to TSPO, but less sensitive than the PBR28 one. Interestingly, the Japanese group said it was planning to repeat its ME/CFS study using the new PBR28 tracer.
Cool – that’s good to hear.
Thanks. Interesting times.
Possibly a dumb question or two, but I didn’t think it was clear from above: in these studies with humans did the researchers establish that treating those who had this problem actually resolved the pain or have they not got to that point yet? And is pain the only thing that inhibitors can deal with – there is much talk of ‘sickness response’ in association with ME/CFS – would all such responses be helped e.g. general pain, cognition, fatigue and muscle pain specifically etc.?
And, if you inhibit or reign-back the activated microglia with drugs – what effect might this have on normal microglia function in say the presence of a subsequent infection? For how long might these drugs be required to be taken before, I presume, microglia are corrected?
I guess we might only know some of the answers from new trials. Younger spoke of ‘sensitized’ microglia and of course Leptin, but they are all on the same page I suppose.
Russ
Linking neuroinflammation in the brain to pain or fatigue or whatever was the first step. Turning down microglial activation is next.
I think they just want to normalize microglial functioning – so that it just reacts to infections (and not other things.) Of course an infection IS present maybe you don’t want to turn down the microglia (or do you?)
They’re going on the assumption I think that some sort of insult got the microglia into this steady state of hyperactivation.
It will take clinical trials and Younger is on the same page (except he doesn’t quite trust these tracers).
This would certainly explain the wide range cytokine blood level abnormalities I would think due to the kind and rate they cross the blood brain barrier. With microglia doing what they do best to defend CNS immunity, this new information will no doubt be groundbreaking in understanding the brain and responses involved in pain. What a great report Cort. TY. My own pain specialist (anesthesiologist) has told me from the get go that most pain specialists see fibromyalgia as a microglia problem. I can’t wait to see more to come.
That’s so cool that pain specialists – the ones in the know – see FM as a microglia problem 🙂
It looks to me that microglia is a hot topic for many different disorders, FM, ME/CFS, depression and anxiety. I hope it is not a new XMRV hype. I don’t believe the microglia is the cause for all these problems. If we can objective see with PET scan that they are activated it is just a start. We must know why they are activated. I don’t believe in ‘hypersensitive’ that is really simplistic thinking.
I believe we will have to resort to very individualized treatments, depending on how, and why the microglial became so turned-on in the first place. I hope that an emphasise will be placed on the need for identifying subgroups. Some sufferers may benefit from anti-inflammatory, or antihismanic interventions because their microglial activation and ME/CFS or FM symptoms (brain inflammation, sickness behaviour, pain) are the direct result of being allergic and up-reglated towards autoimmunity. In others microglial activation may have been caused by a virus, or bacteria that couldn’t be defeated by an individual’s immune system (down-regulated); it keeps trying, but isn’t winning the battle. These people may require a completely different treatment, such as antivirals, or antibiotics to finally eliminate the invader, thus calming activated microglial cells.
Sounds right to me – knock down whatever is still disturbing the system and go after the microglia…I don’t think it’s ever going to be simple.
Great info! Thanks for the link to Younger’s newsletter.
Andrew Lloyd in Sydney also thinks microglia are a key player in CFS.
If microglia is the key for many neuropsychiatric conditions. Is ME then a psychiatric disorder? Can the location of the ‘ínfection’ in the brain explain the different symptoms in people with CFS? What causes this activation of the microglia? I don’t believe in the ”primed” story.
Well microglia could play a role, but a different role, in both cfs and depression.
M.E. stands for ‘Myalgic Encephalopathy’.
Encephalitis is an inflammation of the brain:
http://umm.edu/health/medical/altmed/condition/viral-encephalitis
M.E. may turn out to be the best name!!!
there are quite a few drugs (existing or in development) that can work on microglia.
The one in the link below has promise. I suggest a concerted effort in this area is required.
http://news.uci.edu/press-releases/cancer-drugs-block-dementia-linked-brain-inflammation-uci-study-finds/