The ME/CFS/FM Experts Panel is back! The panel is a group of ME/CFS/FM doctors who’ve agreed to look over a patients case in detail and provide their recommendations. It was Carly’s turn this time.
It’s not fun being Carly right now – and it hasn’t been fun for quite a while. She was completely healthy until age 16 when she came down with a flu she never recovered from. Eighteen years later, she still experiences constant fatigue and flu-like symptoms.
She has endocrine issues, gut bacterial problems and most recently a positive PCR test for parvovirus. Her system is so unstable that she can’t handle medications that help her. On a scale of 1-10 in functionality – she reports she’s at a three.
Basic Details
- Gender – female
- Prior State of Health – excellent
- Duration of Illness – 10-18 years
- Current Age – 34
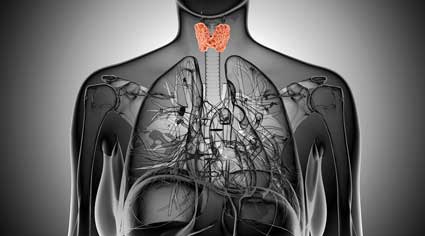
- Co-Morbid Disorders – Hashimotos, Thyroid problems, ME/CFS
- Functional Level (1-10 – 10 being the highest) – 3
How It Started
Carly’s Story “It began with the flu overnight. I was completely healthy before that point although there was a period in which I was more stressed prior to the infection. I was age 16. I was very healthy prior to this infection. I picked up but never regained my energy and had to pace myself to attend college and university. But I wasn’t terrible and had no awful symptoms – just fatigue and bouts of flu again. Five years after university I crashed completely and there had been scary symptoms appearing for the final year.
I had taken antibiotics and I believe my thyroid was failing but that wasn’t picked up in the tests.
Eventually very high antibodies to thyroid showed showed up and I was border-line lupus but never positive. (Using diet I have now reduced my thyroid antibodies from 3000 to 43 myself.)
I was in bed for a couple of years. I was very sick and very anxious. I needed full care.
Then, I was housebound and now I am a bit better but for all my efforts (which are great) I cannot get out much and have constant symptoms which change a lot. I seem to respond oddly to medication I need like thyroid meds despite trying every option available. It is the only thing which makes some difference to my very low energy levels. But I get many symptoms trying to force the medication too.
It’s a constant roller coaster with no baseline. I’ve been in a roller coaster pattern for 13 years and cannot stabilize at all. I recently discovered I have active parvovirus b19 virus (PCR test) but have negative IgM. I have some IGG positive levels. I believe the parvovirus is affecting my endocrine system badly. I do not know why my immune system is compromised and cannot fight this virus or what else I could have.
Carly has recently created a new wellness website – Living Brightly – where she explores how to live a purposeful life in the midst of illness.
Symptoms
What sleep issues, if any, do you have? What are your sleep and napping patterns?
I sleep mostly fine. I can wake with an adrenaline rush if my thyroid gets too low or too much to handle. I nap during the day for an hour, but I cannot work or go out much due to energy. I sleep about 9 hours at night – and I’m in bed a lot more.
Where do you feel pain and how severe is it?
Pain is better since I went gluten free and cut inflammation down with diet and work. Pain is fine really although I do get days where I feel like I’ve been run over and hurt, but that isn’t what limits me – it’s the heavy constant fatigue, and weakness and basically feeling as though I have the flu. All the work I’ve done has helped massively in areas, but has made no difference to my ability to have a normal life so we are missing something major.
What happens when you try to increase your activity level, such as starting a walking program or doing yoga?
If I do too much I will feel sick and it’s almost like my body goes into shock. It’s not a case of pushing through. Wish it was. I often will go to sleep after. But I feel no better doing or not doing it. It’s just pushing myself makes my body unable to cope further.
Do you have sinus symptoms? Have you ever been treated with Diflucan?
No and no.
Do you have any place in your body that seems “infected”—sore throat, cough, sinuses, etc? and what are the symptoms?
Not really I do get sore throats but again not major. Just general flu weakness really.
Testing
Endocrine and Hormone Tests
- Thyroid tests fluctuate
- Current TSH -1.8
- Current T4 15 (9-19).
- Thyroid antibodies have dropped from 2000 to 40 with diet.
How was adrenal insufficiency diagnosed?
Cortisol saliva tests and trial and error over the years. Cortisol is flat all day. A recent consultant suspected Addison’s but we didn’t test as knew likely to be officially negative and would restrict treatment . I don’t have Addison’s I don’t think but the HC (she’s taking 15 mgs) is a life saver although I feel worse on higher amounts. I believe it allows the thyroid hormone to get through to the cells.
Do you know morning salivary cortisol levels?
Not I had it checked for a few years. It’s generally just below the range.
Have you ever had these tests done? – FSH, LH, estradiol, prolactin and progesterone levels.
Probably but were all normal. Tried prof cream in past. Was fine but didn’t impact health.
Thyroid – Re – thyroid – it varies so much. My temp can be very low or very high. I cannot tolerate any thyroid medication at the moment at all. I think my own thyroid is improving but not enough to explain the weird symptoms I get when I take meds. Thyroid meds give me enough energy though to have a walk – but then the side effects begin.
Any symptoms related to your periods or possible estrogen/progesterone issues?
Yes. I always had awful periods from before the illness – but always regular and normal flow, etc. They have been better of late. I sometime get some spotting a few days prior. If I don’t take hydrocortisone I would faint and be sick during my periods so that’s related to weak adrenals obviously. Now, with the hydrocortisone I feel better but I still have to lay down/ go to bed during my period each month.
Immune and Pathogens
- Positive for Parvo B19 PCR and IgG, Negative for IgM.
- Gut bacteria – beneficial bacteria lactobacillus specius = no growth; bifadobacterium – low at 2 (suggested should be 4); geotrichum species =2 – which is slightly in ‘potential pathogen’ range. Low levels of good bacteria in gut despite probiotics, excellent diet, supplements etc.
- Pathogens – negative – Cryptosporidum, Giardia iambia, entamoeba, campylobacter, enterohemorrhagic escherichia coli
Have you ever been tested for HHV-6 and CMV?
- CMV – IGG antibody negative. No results for the other one.
- EBV – IGG negative.
However, with the Parvo virus the IGM antibody was negative yet positive in PCR.
Have you ever taken antivirals? If so which ones and for how long?
No, just on a herbal one called Botanical shields but have not looked into virus field before recently so have not done anything.
Autonomic Nervous System
What is your BMI, blood pressure and pulse? BMI – low but weight good for me and stable. Nutrition is excellent. I’m on a nutrient dense paleo-style diet.
- BP – low, but helped with the hydrocortisone.
- Pulse – varies depending on the dose of thyroid medication I am on. 60-70-ish is normal. It can go high though, and a bit lower.
Have you been tested on a tilt table?
No, I assume I would fail this test. POTS highly likely. Never wanted to put myself through it as Doctor said there’s no treatment anyway. My BP often drops upon standing. Always did before the HC.
Do you know your resting blood pressure?
Varies but approximately 100/65. It can be higher though, at times, but vernally always had low blood pressure. It was super low when I was much sicker.
Have you been tested for small intestinal bacterial overgrowth (SIBO?)
No. I have had gut testing though and no parasites or stomach issues showed up. I don’t feel I have gut issues other than immune wise. I have very low good bacteria of lacto and bifidus levels despite taking good probiotics, though.
Others
- MTHFR and other mutations being treated.
Medications Taking
- Thyroid – natural desiccated thyroid – can barely tolerate 1/4 grain so cannot get stable. I think thyroid function is improving but this is complicating things as I feel I do need more but cannot tolerate it due to side effects. I get an energy boost from it but then suddenly I experience higher temperatures (but also low at times) and feel nervous, dizzy, tense and shaky, have ear pressure, jaw ache, blurry, bloodshot eyes, weak muscles. I feel exhausted when I take more than 1/8th grain. But then without any I feel very weak and cannot get out of bed and start to feel quite unwell, too.
- Hydrocortisone – 15 (mgs?)
Have you tried IVIG?
- No – this is what I need to explore though.
Recommendations
Dr. Kaufman (Infectious Disease Specialist)- Parvovirus
For Dr. Kaufmann is an infectious disease specialist associated with the Open Medicine Institute. He formerly focused on HIV/AID – but reportedly got interested in ME/CFS because he needed a real challenge (:)). For him he answer was simple – the parvovirus is the standout finding. Forget the IgM abnormalities, a PCR positive parvovirus tests means Carly has an active infection. He said
“She needs to be treated with IVIG if she is Parvo PCR positive. That is the only effective treatment. Being PCR positive is clearly abnormal regardless of IgM status.”
Dr. Ken Holtorf, MD- Lyme, Immune, Mitochondrial and Endocrine Enhancement
Dr. Holtorf would take a deeper look at her immune functioning and check out Lyme (“sounds very tic-borne illnessish”). (He recently asserted at the LDN conference that Lyme is much more prevalent than many suspect. )
He would also check out clotting factors in her blood. At the LDN conference he noted how often heparin (I believe it was) was effective in his patients (see the Berg studies). Dr. Holtorf is also an endocrine specialist and recommended a series of endocrine tests plus possible trials of low dose naltrexone, a little Ritalin perhaps for the fatigue and mitochondrial support. The next steps after that would depend on the lab results.
“As a starter, I would want to order a natural killer cell function (Quest)(can also do a CD57 from Labcorp), a C4a (Quest), Eosinophil cationic protein (ECP) and vascular endothelial growth factor (VEGF), HHV6, Thrombotic marker panel (d-dimer, thrombin-antithrombin complex, Prothrombin 1& 2, soluable fibrin monomer (SFM) and plasminogen activator inhibitor-1 (PAI-1) along with a Lyme culture from Advanced or an antibiotic provacated Lyme WB from IGeneX, a TH1-TH2 cytokine panel and a nagalse level. Sounds very tic-borne illnessish.
Would bet there would be significant positives, as something infectious is driving her immune imbalance TH1-TH2 shift, autoimmunity and autonomic dysfunction. Lots of options after get these results back. Consider treating underlying cause along with immune modulators, heparin, etc For the thyroid, would stay off gluten and continue high dose probiotic, of course, and try a course of low dose naltrexone (if not on a narcotic) and low dose allergen.
Would check thyroid panel and SHBG to titrate up (likely straight T3 would be best choice), following labs, symptoms, thyroflex, body temp, etc. Follow cortisol and ACTH and adjust her cortisol level.
Can try a little Adderall in the meantime to see if helps the fatigue while figuring out underlying causes. Would start on a combination of ozone and UVI along with IV silver and nutrient with glutathione therapy (maybe IVIG and/or Regenapep. Cell therapy could be of benefit. Again, many options depending on above lab results.
Can try pyridostigmine, testosterone or Myopep for the weakness or DDAVP nasal spray for the low BP and Isoprinosine as a broad spectrum antiviral immune modulator. Mitochondrial support usually worth a try and a basic. Sleep sounds OK but Xyrem may be an option for a deeper sleep if others have been tried such as melatonin.”
- Learn more about Dr. Holtorf here
Courtney Craig – Chiropracter and Nutritionist
Courtney Craig and Dr. Holtorf both agree that a gluten-free diet is indicated given the possible diagnosis of Hashimoto’s. Courtney Craig recommends various supplements, a very low carbohydrate diet, and intermittent fasting to, among, other things – improve mitochondrial function
“I’m glad to see Carly has already adopted a nutrient-dense, Paleo diet. Given her Hashimoto’s diagnosis, a gluten-free diet is indicated. Several studies have demonstrated high prevalence of thyroid patients have celiac disease or non-celiac gluten sensitivity. Many improve with gluten avoidance (1,2).
To support overall thyroid health, I would suggest adequate dietary selenium and iodine. Good sources of selenium are Brazil nuts and shellfish. Sea vegetables are rich in iodine, as is sea salt. Dietary strategies to address the adrenal fatigue may include a very low carbohydrate diet to stabilize blood sugar. Getting adequate protein in the morning supports adrenal function by stimulating cortisol production upon waking.
It’s also important to consume abundant vitamin C, with low-sugar citrus and/or supplementation, for the biochemical conversion of adrenal hormones.
Lastly, electrolytes are essential for adrenal function. Increasing dietary salt intake throughout the day in addition to adequate magnesium can be beneficial. Supplementation with a multi-mineral has been shown to improve many CFS symptoms, including autonomic dysfunction, anecdotally and in some small studies (3).
To support immune health, in addition to a nutrient-dense diet, I like to recommend periods of intermittent fasting. Studies show 16-18+ hour nutritional fasts can stimulate mitochondrial health and effect immune cell function (4,5). These effects can be safely obtained by eating during an 8-10 hour window and consuming adequate water and electrolytes.”
- Learn more about Courtney Craig D.C here
- Check out Carly’s new wellness website – Living Brightly – where she explores how to live a purposeful life in the midst of illness.
1 Sategna-Guidetti C., et al. (2001) Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study. Am J Gastroenterol. 96(3):751-7. http://www.ncbi.nlm.nih.gov/pubmed/11280546
2 Guliter S., et al. (2007) Prevalence of coeliac disease in patients with autoimmune thyroiditis in a Turkish population. World J Gastroenterol. 13(10): 1599-1601 http://www.wjgnet.com/1007-9327/13/1599.pdf
3 Maric D., et al (2014) Multivitamin mineral supplementation in patients with chronic fatigue syndrome. Med Sci Monit. 20:47-53. http://www.ncbi.nlm.nih.gov/pubmed/24419360
4 Cellular Spring Cleaning: Intermittent Fasting for CFS. 8 May 2014. http://www.drcourtneycraig.com/blog/intermittentfasting
5 Longo VD, Mattson MP (2014) Fasting: molecular mechanisms and clinical applications. Cell Metab. 19(2):181-92 http://www.ncbi.nlm.nih.gov/pubmed/24440038 ______________________________
If you have any suggestions for Carly please pass them on.
Check out Health Rising’s new ME/CFS, FM and Chronic Pain Forums here











I suggest Carly look into Wilson’s Low Body Temperature Syndrome a condition that is managed with compounded T3 alone to raise body temperature and relieve fatigue.
http://www.wilsonssyndrome.com
To help with low blood pressure be sure to consume lots of water and salt. When feeling worse try drinking salt in warm water.
For gut issues look into the possibility of Small Intestinal Bacterial Overgrowth (SIBO)
http://www.siboinfo.com
To improve adrenal issues and raise cortisol levels try LENS neurofeedback (it worked for me)
http://www.ochslabs.com
I love the variety of approaches available. I have to remember to consume water and salt together – it definitely helps me. Thanks for the reminder 🙂
Please, if you have an idea what’s happened or happening to Carly or how to possibly fix it – put it forth.
Hi Cort,
I hope someone will filter all this information for Carly. Such a diverse load of ideas will no doubt cause some stress for her. It does highlight the truism…..’for a carpenter the answer is always a nail’. However, I do feel for the practitioners trying to come to grips with the vagaries of the human body!
I hope there is a possibility that we shall hear some kind of follow up on Carly and her quest to find some relief, or heaven forbid….a cure. Fingers crossed. I wish her well.
Linda
Yay Carly – hope this helps – love Steve OHC x
Hi Carly.
What a conundrum you present to the medical fraternity. My hopes are that you find a way to a better state of health, to have made it this far it seems you probably have a supportive environment.
I can only suggest one thing….heard on an interview and stuck very permanently in my mind….about a child whose health was deteriorating and it was suspected that the high amount of probiotics being given were missing their mark due to other complications in the intestinal tract. The practitioner suggested, out of pure desperation, for the parent to consider a high dose of probiotics administered as a suppository so that they were not compromised by gut bacteria. The effect was noticed within a day or two and continued to assist on an ongoing basis.
I wish you well and hope the wealth of ideas being offered to you will be filtered by someone on your behalf.
(My 13 y o daughter had a similar kick off…..virus…never recovered….6 years later still searching and hoping a deterioration is not on the cards. She is semi functional at present.)
I love this. So happy you are providing this Expert Panel for our education. My only problem is I cannot find where some of these doctors are located. Case in point, Dr. Holtorf. I followed the link to the clinic mentioned and could not find an address there either. Yes, it could be that brain fog is the reason. It would make it so much easier if the doctor’s locations were beside their name in the article above. I’d love to know if one of these experts is near me! Thank you!
Nita,
If you click on the link in the story above that says “Learn More about Dr. Holtorf here” and then click on the link to go to his website, all the clinic locations are listed under the ABOUT menu at the top of the page.
Why, I’ve been sic/ME since the white Bronco was doing a slow speed chase with ( brain fog )
Can’t remember who was driving.
Anyway, I live just north of San Antonio Texas.
And all this time I’ve been trying to find a dr. With knowledge of M E .
I m ow it’s hard to believe. But remember that I can only read or think intermittently.
I have two questions
1. Have you ever heard of an M E patient not being able to say anything understandable and also talking from somewhere in there head ( I’m not trying to say anything)
2. How do i find these AWESOME doctors. I’m still being treated like a liar or just a bad person.
Thanks , your path has helped me alot .
She mentioned antibiotics but not what kind and for how long. I was on doxy for thee years and I believe that is what destroyed my gut microbiome, your first immune line of defense.
Based on my experience I would definitely not suggest intermittent fasting with weak adrenals. They need lots of C and protein throughout the day. She could try Thorne adrenal exract as well but it hyped me too much. Works for some instead of hydrocortisone.
I would be curious about any mercury or mold exposure. Dr, Kogelnik talks about the two issues, one is something punches a hole I your immune system, two is what you deal with opportunistically once you immune system is shot. I agree with the recommendation of one Dr. above, the NK cell function test was my first solid evidence of immune dysfunction.
perhaps a faecal transplant for the gut bacteria. I also tend to fall asleep if I do too much activity and benefited from being gluten free. I have found n-acetyl-cysteine helpful and ATP if I have to do something, although the effect is short lived. I am considering if my ongoing problems could be due to histamine intolerance and if quercetin and vitamin C could be helpful.
Carly is my sister and this gives us a lot to go on so thank you all so much, please keep all the ideas coming! As well as links to doctors who can/will help.
Many many thanks
Donna
This is a real different story then Dan, isn’t it?
Hi there,
Wow. I have a friend who has now been diagnosed with 20 different conditions and diseases, including Lyme, POTS (she has been advised to increase the amount of salt in her diet and literally takes a small handful of sea salt (sel de mer is full of vitamins) on a daily basis.
Obviously, it is important to at least come to some conclusions as to what is actually going on. As mentioned above by the first doctor – the parvovirus might still be lurking…but…due to the amount of antibiotics I am guessing that Carly has taken, I am wondering if she is experiencing a candida overgrowth and needs to go through the process of supplements, restricting foods that are actually feeding the candida as well.
Considering that LDN is being used for 174 different auto immune conditions, and (according to the chemist here in the UK who compounds it, and whom I met at an LDN meeting), ‘LDN is safer than aspirin’. It is definitely worth a try – however – what many doctors and patients do not know is that it can take up to 6 months to kick in…so it would be important for her to stay on it for half a year in order to determine whether or not it is starting to make a difference.
Candida overgrowth can cause all sorts of bodily hell! I read if you have been on antibiotics for more than 20x in a lifetime, then there is a very good chance of this happening.
What about investigating to see if there is a functional medicine doctor in the area? They will also test for many things that you wouldn’t normally get from usual western culture of medical treatments and investigations.. I would also be looking into Mast Cell Disease.
Very complicated indeed. Please keep us posted Carly (and Cort!).
Also, Carly, an idea would be for you to use the Health Rising FibroMapp app – because it can be personalised – and you can start tracking everything from pain to meds, fatigue, sleep, a journal and much much more. All the data is collated – and you might see patterns starting to emerge in order for you and your medical peeps to determine if there is anything going on that is causing flare ups. The app is available on the Health Rising website.
Wishing you success in getting to the bottom of what is going on so that you are able to move forwards and have a much better quality of life.
A.x
my son has had CFS for20yrs. His recovery started when we realisedthat candida overgrowth in his small intestine was causing most of his symptoms. I would suggest that Carly reads Dr Orian Truss’ work which can be found in the Journal of Orthomolecular Medicine online also his two books The Missing Diagnosis 1 and2 He found over 50 yrs of experience that candida produces many other symptoms via its toxin acetaldehyde long before it produces gut or vaginal problems. My son had many of theseIf you have had antibiotics and have CFS you almost certainly have candida. Candida forms biofilms, which
protect it from the immune system and antifungals. Thorne product SF722 is an antifungal and also detaches and dissolves biofilms. It cleared my son’s candida in a week.Truss’s paper on his ‘acetaldehyde theory’ doesn’ cover all the negative effects of acetaldehyde, it also inhibits B ,vitamins and inhibits the conversion of T4-T3 and causes peripheral thyroid resistance which may explain intolerance of thyroid hormone, theT4 just makes you toxic.Try T3 to get over this. Adequate cortisol levels are essential for cellular uptake of thyroid. If you rid yourself of candida you will see the other problems more clearly. Getting thyroid and adrenal hormones, both cortisol and DHEA.right for you is essential if these aren’t right nothing is right. Also check estrogen and progesterone levels via saliva tests, if you have an excess of estrogen this interferes with the thyroid hormone and you will seem to have too little. Using bioidentical progesterone
Cream gets over this, in my personal experience, see Dr John Lee’s work on this.
Linsomw interesting points made. Thyroid treatments are different worldwide. UK standard treatment is thyroxine. Would be interested to know more about what side effects you think you get from natural desiccated thyroid. 25 micrograms at intervals daily according to dose could possibly improve these. Interested also to know more about diet but sounds like one Dr Myhill recommends for ME. Prof Newton at Newcastle does treat POTS patients and is an expert in this area.
If there are errors in the posting I apologise, a vertical banner goes across the text box on the iPad meaning I can’t see all that I’m writing.
Definetely a trial of IVG is the best choice for her,even at the lowest dose,400 mg-k of body weight,it is the only treatment which has antiviral properties even if the virus has turned intracellular,at the same time can shift the immune system from th2 dominant state to a much more ´´calm´´ and functionable level,plus it is the best,if not the only,treatment to regenerate the small c fibers of the autonomic nervous system and so will adress her problems with low BP.
We can not be sure that everything comes from the adrenals,I would suggest a skin biopsy to test for small fiber neuropathy,a biopsy in the lower part of the colon to test for collagenous collitis or another sign of chronic inflammation,plus a test for amyloidosis which can hit your autonomic nervous system in a thousand ways.
Is she complaining for dry mouth,dry eyes,dry skin? Testing only for lupus or sjogren antibodies means nothing,there are many patients who suffer from a rheumatic disease and they are serum negative!!!if she has dry mouth a lip biopsy is the best option,better to find these diseases early than later when systemic inflammation is spread out,fasting is like killing her.
no seak organism needs fasting,what she needs is the basic materials that her body needs to heal itself and sustain life,that can not be only water,she needs protein,injectable amino acids,injectable magnesium,injectable vitamins,injectable carnitine and if not injectable glutathione then NAC if her stomach can tolerate it.
For the fatigue I would definitely suggest provigil and pyridostigmine,also kefir yogurt and if ferritin test below 50 then iron 50-100 mg every day for three months and recheck,has anyone tested vitamin d for her?
It is crucial because in our bodies vitamin D works as an immune modulator…I hope that someone will show interest to her case because she herself says that she is not sure about this test or the other etc…seems confused….needs serious medical guidance,hope she gets better soon and enjoy her life!!!
Thanks for the great comment Savvas.
Mr. Salva Dimitriadis-are you a medical doctor and if so, do you take patients and where are you located? I have similar issues to Carly plus a lot more and think you could help me. I have Lyme disease in addition to CVS and Fibromyalgia and think I am slowly dying.
Dear Sharon,
First of all you have to calm down,you are NOT slowly dying.
Believe me,there are people who suffer much more but i understand how you feel.
Unfortunatelly i am not a doctor,i am a patient like you,i have cfs for the last 8 years and sjogrens for at least 20 years,also small fiber sensory peripheral neuropathy and dysautonomia due to small fiber autonomic neuropathy,believe me you would not be happy having all these to deal with…
If you have lyme disease there is a possibility that you have only this and no cfs,no fibromyalgia,i mean maybe all your symptoms are driven only from the Lyme disease,if i were you i would search for a Lyme specialist and not a cfs doctor,your primary disease is Lyme but if it stays untreated for a long time can cause secondary cfs or fibromyalgia.
I live in Greece and here lyme disease doesnt exist.
Personally i think Lyme can be easier treated than cfs or a rheumatic disease,find in your area a good doctor and proceed as needed,i could write you one thousand suggestions but it is better to hear them from a doctor and discuss the problem with him,there is a solution for everything,try to be possitive,being negative means you are trapped,you dont move and if you dont move my dear then you dont live…
I wish you the best…in everything…
P.S dont forget to smile!!
my son has had CFS for20yrs. His recovery started when we realisedthat candida overgrowth in his small intestine was causing most of his symptoms. I would suggest that Carly reads Dr Orian Truss’ work which can be found in the Journal of Orthomolecular Medicine online also his two books The Missing Diagnosis 1 and2 He found over 50 yrs of experience that candida produces many other symptoms via its toxin acetaldehyde long before it produces gut or vaginal problems. My son had many of theseIf you have had antibiotics and have CFS you almost certainly have candida. Candida forms biofilms, which
protect it from the immune system and antifungals. Thorne product SF722 is an antifungal and also detaches and dissolves biofilms. It cleared my son’s candida in a week.Truss’s paper on his ‘acetaldehyde theory’ doesn’ cover all the negative effects of acetaldehyde, it also inhibits B ,vitamins and inhibits the conversion of T4-T3 and causes peripheral thyroid resistance which may explain intolerance of thyroid hormone, theT4 just makes you toxic.Try T3 to get over this. FAdequate cortisol levels are essential for cellular uptake of thyroid. If you rid yourself of candida you will see the other problems more clearly. Getting thyroid and adrenal hormones, both cortisol and DHEA.right for you is essential if these aren’t right nothing is right. Also check estrogen and progesterone levels via saliva tests, if you have an excess of estrogen this interferes with the thyroid hormone and you will seem to have too little. Using bioidentical progesterone
Cream gets over this, in my personal experience, see Dr John Lee’s work on this.
A couple of suggestions from Dr.Amy Myers ‘ Autoimmune Summit’ (available on line). Myers is a doctor from Arizona who is associated with the USA based Institute of Functional Medicine. She practices in Arizona and has a strong interest in thyroid problems associated with the gut. Functional Medicine has a a very strong interest in gut health generally and has doctors who specialise in this area throughout the USA especially SIBO.
Myers series suggest that :
1. some people who are reacting to the bio identical thyroid hormones, she as Carly is using, may react better to the synthetic ones because they will make fewer antibodies to what is NOT identical to their own cells.
2. there is considerable evidence that GM foods are associated with increased antibody production especially thyroid antibodies because these products contain novel proteins that people and animals have never encountered before. Dr. Myers does advocate a paleo diet such as Carly is using BUT avoiding lot feed meats as these animals in the US are feed mainly on GM. Given the very large amounts of meat Carly will be consuming it maybe worth sourcing meat from grass fed animals. Easier said than done in the US I know but worth thinking about.
3. One of the speakers in this autoimmune series is a dentist who had some similar symptoms to Carly. His talk identifies dental issues especially toxins that can produce weird autoimmune symptoms.
You never know what will prove useful but I appreciate Carly’s cautious approach …..best wishes keep us posted….
Good idea about the hormones and meat. The dental speaker in the summit was Stuart Nunnally. Very informative and surprising what lurks in old dental fillings, under caps, and in the gums where teeth have been removed.
I hope Carly is also avoiding ‘sugar free’ products, esp those that come in fizzy cans…if you get my drift.
Cheers
Linda
Hi all. I am a friend of Carly’s and know her situation well. She has tried all different types of thyroid separately and in combo. Her meat is grass fed and she has extensively studied the teachings of Amy Myers and many others. Her diet is totally pure of with the odd exception of healthier treats (a total food health but basically). She has no stomach issues to speak of but may revisit the yeast issue.
I feel that the bug question is why has she stopped producing antibodies to Parvo? Is it just Parvo or something else stopping her ability to produce antibodies to other infections also? We know that Lyme does this as it is so immune suppressive. She may also have some coinfections that go with Lyme such as Bartonella or Babesia. Other infections to look at might be mycoplasma infections and chlamydia pneumoniae (not the STD). As money is tight she wants to know which avenue to persue first to give her the best chance of improvement. So do we know if she chooses IVIG whether this will be problematic in any way if she also has Lyme as the root cause that is suppressing her ability to make antibodies to the Parvo. Could it cause dangerously high levels of herxing if the IVIG affected other major infections she may have too….such as the Lyme. The doctor’s feedback on this would be so valued. Cort is there anyway you can find out?
Thanks so much 🙂 x Jo
I’ll try.
Both clamydia peunominae and micoplasma have been know to respond to the low risk treatment of 6 weeks on boiotics Rearsestch ADP which is oregano followed by 6 weeks on olive leaf extract repeated for months and with Allergy Research’s Humic Acid according to Antony Haynes of Nutri link.
The problem is that when you become as reactive as Carly it all feels like overload and caution is required also I suympathise with how annoying peoples well meaning suggestions get after you have already tried many most of them.
Just another HUGE thank you to Cort!!
This info is exactly what i need right now as i’ve started with a new doc and we’re investigating much of what is written about here (thyroid, tic-borne stuff, adrenal, etc). This is sooo helpful. I can very much relate to this woman’s story. When i get a bit more energy i’ll read it more thoroughly tomorrow.
Thanks again for posting this!
Kira
Quick question. What is IVIG? (intravenous something?)
Also, don’t want to be a downer but I’ve had lyme/cfs for 20 years and try to research any protocol before trying it. This, from having previously wasted a lot of precious energy and $ on false hope.
Since I have low body temp but as yet undiagnosed thyroid issues, I was interested in the post about Wilson Syndrome. I looked up Dr. Wilson. When I discovered he did not have a medical license, I did more digging and found Wilson’s Syndrome is not recognized by the scientific community or the American Thyroid Assn.
( http://www.quackwatch.org/04ConsumerEducation/News/wilson.html )
That said, his protocol may still be valid. For all I know Big Brother just wants to shut him down for some reason. You would have to decide for yourself.
Hi Kira,
There are a lot of untruths on quackwatch. I checked up on their comments about someone whose books I had read, couldn’t find anything to substantiate their comments.
Have you seen http://www.herbsforlyme.com , seems lyme is thought to be a biofilm infection. Thus is where I found the Thorne product mentioned in my previous post, but it isn’t on there now .
Sandra
Intravenous immunoglobulins – http://en.wikipedia.org/wiki/Intravenous_immunoglobulin
http://www.ncbi.nlm.nih.gov/pubmed/12715326
http://www.ncbi.nlm.nih.gov/pubmed/15750469
She can not choose this or that,she needs treatments simultaneously to adress all her problems,Lyme can be treated with antibiotics,also many other infections,has anyone put her in antibiotics?
High levels of herxing during intravenous immunoglobulin is not so easy to happen because they give you also intravenous methylprednisone and antihistamines before,during and after the procedure.
But yes,it can rarely happen.
Jarisch-Herxheimer reaction would be a good sign,her body will get rid of the bad microorganisms and later on she will feel great.
IVG is expensive,if she tried no antibiotics then it is time to do so but remember,you need to take a good probiotic and antifungal medicine such as diflucan during the period on antibiotics,not nessecary every day,3 times per week is not bad,check before and after the treatment of the liver enzymes is essential.
More on Wilson’s Syndrome:
http://articles.orlandosentinel.com/1991-09-22/news/9109201143_1_wilson-syndrome-wilson-syndrome-denis-wilson
http://articles.orlandosentinel.com/1992-02-08/news/9202081153_1_wilson-syndrome-denis-wilson-medical-board
Hello,
Just wanted to make a comment on IVIG. I have used it for years with success; it has been very beneficial for many patients. It is an immune modulator that has multiple benefits, but have some concerns that it can lower natural killer cell function (It is used by fertility doctors on women with overactive NKC function). While its effect on patients with low NKC function have been studied, that I know of, I have some concern that using it might be a double-edged sword with symptomatic improvement but might be counter productive for long-term recovery. I still use it because I do see improvement with it, but I discuss with patients the potential theoretical downside and monitor NKC function and number.
Regards,
KH
Thanks Dr. Holtorf
typo: “…with low NKC function have NOT been studied, …”
Thank you all so much. It’s Carly here and I am penning a proper detailed response ASAP as many things I’ve already addressed ( feel like somewhat of a doctor myself at this point
V interesting everyone thank you. Thanks to Dr H for coming back to us. Good to know the Ivig can be helpful but if it lowers NK function presumably that is not the best plan if one has Lyme also? Also steroids are I believe not a good idea if you have Lyme as they suppress immunity but perhaps as it is just for the duration of the treatment for ivig then not such an issue. My gut instinct would be perhaps be to get a clearer idea of Lyme status first and treat for that. If Carly has tick Bourne infections then she may not be producing antibodies well to other infections if her immune system is overloaded. Not just a parvo specific problem. I wonder if by treating tick infections her immune system may pick up and fight the parvo itself. I guess the root question is why did her body stop producing antibodies to parvo? Is it possible to just have a condition where one just doesn’t fight off parvo properly…somehow I suspect not but I am no doctor and may of course be wrong.
Thanks Jo – great question and clarity. Hopefully get down reposnse xx
Oops don’t know what happened but the rest I my text was cut off…. Thanks again everyone will write it out again ASAP x
Oops don’t know what happened but the rest I my text was cut off…. Thanks again everyone will write it out again X
Carly is certainly beautiful. IVIG is something I would like to learn more about. I have read that colustrum is a mild alternative, does anyone know there is any validation to this?
I am THRILLED to see that people are talking about the TH1-TH2 balance, something that was a big game changer for me when I considered it in customizing my personal Lyme protocol. I find that most Lymies do better when the increase TH2.
A note on the sore throat, it could only help if you addressed this. It could be sore because you have a throat or sinus infection, and wherever you can reduce infection, whether in your blood, your gut or your throat, could benefit you greatly.
Good luck Carly!
Generally find that sore throats are more viral
Would check ebv and hhv6 titres and or consider general antiviral therapy
Hi again everyone,
Its Carly here. Hopefully my message won’t get cut off this time 😉
Firstly I want to thank Cort and the Doctors for their valued time and input. It is much appreciated and I think chronic ME needs to be explored much further as for me clearly the diagnosis is useless for many (umbrella term) and conditions are very complex.
The Experts have basically reached the same conclusion that I myself have come to – I feel like somewhat of a doctor myself by now. Haha.
My own conclusion is that at age 16 I contracted an overnight flu virus which was the significant trigger which kicked off the spiral and perfect storm for this all to begin. This then led to autoimmunity kicking in with hasimoto’s thyroid and adrenal problems and caused further spiralling in a system which couldn’t cope and became vulnerable to other infections.
It is certainly a complex jigsaw puzzle and a spiralling system with viral, immune and hormones getting caught up. Once in this mess no ‘normal’ treatment’ such as thyroid medication worked because although they are needed, they cannot be tolerated. There is too much going on and the body is an intricate system which needs to be treated as a whole and for each root cause to be discovered….
I believe that environment and genetics also played a role in this perfect storm. However, although I likely contracted Parvo B19 Virus right here at the onset it has still remained unclear why I originally produced antibodies to fight it, but then stopped – with the major problem being that I still have the virus active today 19 years later. I still have the flu every day basically.
I believe that there is a reason for the compromised immunity perhaps beyond just a system unable to cope. Although of course it would be great if the only thing I needed to deal with was the Parvo infection as the root cause. I am seriously considering the possibility of Lymes Disease now though which scares me a lot. But obviously I already have whatever this is so the only way is up 🙂
I thank you all so much for your comments. It is so appreciated and valued. I hope that by sharing my story and appealing for help I can get further because I know I will get well one day and I have focused all my efforts on a wellbeing lifestyle and path for many years. I embrace all I can do to get well myself and have covered almost everything it is possible to cover such as Methylation, Gut, Diet, Deficiencies, Food allergies, Candida, Detoxing, Mediation, Parasympathetic nervous system, etc etc. Many of your suggestions related to this but I have covered them all including every brand and style of hormone medication over the last 20 years. At least I have got to a point now where I know I have done the foundational healing work, but the fact that I am still so unwell means that I absolutely need to address the root cause and the ‘thing’ which is pulling down my whole system and which always has been.
I would love to form a plan now. I am in the UK so we don’t have insurance here and the NHS is not able to help. Finances are therefore limited and I’ve already exhausted my family’s help over the years with seeing many doctors as you can imagine. Having said that we will do all we can to raise the funds if we can find a clear direction.
It would be great (as many of you suggested) if my case can be acted upon and followed through. I have a wellbeing blog at http://www.living-brightly.com and I will be documenting my journey.
So, firstly I need to find a doctor to work with me who will take all my history on board. More of a researcher I think. I am also very sensitive and have learnt from past experience not to overload my system with drugs as I cannot handle them or the repercussions. I need a gentle approach and one step at a time now. As I say I am in the UK so within Europe would be ideal – or Skype consulations. Or if maybe that I need to work with a number of practitioners to support me and help me manage this and keep it within a framework I feel is right for me as I also believe nobody knows better than ourselves. Travel would be very difficult but my family will support me and get me anywhere if they can.
If anyone has any suggestions who I can work with I would be very grateful? I will contact Dr Holtorf too and ask his opinion.
My next consideration is whether to treat the Parvo Virus with IVIG regardless of the potential of Lymes or further co-infections? I have heard conflicting responses and its hard. I just want to know its safe and the herx reaction would not be terrible? At the moment I am still trying to access an NHS appointment 6 months after diagnosis so you can see how slow it is here. Then I may have no chance of even being given IVIG on the NHS – but I need to decide if I want it first? I think it is necessary to give my immune system a chance to rid myself of the Parvo and perhaps see if that is enough to give it the boost it needs to re-set itself and heal in other areas. It may well be. Fingers crossed. Or it may be that maintenance dose is needed (although no idea again if that would be viable) but to be honest even if I reacted well and felt it was working that would be incredible as nothing I’ve tried so far has ever done that and it would give me a major insight into what I need ongoing. I would love to know if IVIG would be okay though if I and Lyme too? That is my worry as there are risks with it. ….. But it is appealing to know that it could help me a lot even if not the cure as such and I’m leaning towards it certainly. I am also looking at DR Kenny De LeMeir In Belgium who offer IVIG if anyone has experience of working with him? I believe he looks at Lymes too – although my preference is to work with someone who combines natural herbal type treatment for lymes.
So, once Ive decided on IVIG and hopefully a doctor to work with (???) I guess I should test for lymes – even though I know it is very inaccurate? Or perhaps I will do that before IVIG.
SO thats it 🙂 Sorry its so long. It is very complex and feels like a jigsaw puzzle which I am finally beginning to solve. The Parvo Virus detection was major but as yet I have had no treatment which is behind frustrating after being sick for so long. I would love to discuss all my questions with a doctor and that is the main focus now – where to go next with these conclusions which are much clearer? The panel reinforced my own view but at the moment I am no further along in terms of what to do next really.
If anyone has any further suggestions I would be most grateful. I can contact doctors but its difficult to book an expensive appointment without some pre- discussion of their thinking as I don’t have money to waste. Ive consider Dr Amy Myers, Dr De Meleir and and many others but still still to decide what is best and what is possible. I do feel very much alone with this, as Im sure many people in this position do. Im happy to be totally responsible for my recovery path but I also need some real help too- even if just guidance and direction.
Anyway I want to thank you all so much again (and Cort and the Panel again) and one day I will be back with a recovery story! Best wishes to you all and good luck to all those of their own journey. Research is progressing and we can always make a start where possible and keep digging.
Carly x
Hi Carly,
What a journey you have behind you, and ahead of you. I wish you personal strength and many miracles. Cudos to your parents.
As we support our daughter in her sixth year of compromised health (also after a viral infection: at the age of 13) I look forward to reading YOUR recovery story. It would give many of the sufferers and carers much heart.
Live long and prosper!
Linda
Hey again,
So lovely people – who r the best like docs I can work with from the UK please. Loving Horirowitz, cowden, Byron white and klinghart philosophies but need a few more realistic options for my complex case. Esp those who will consult with uk patients. Many thanks Carly xx
Hey again,
So lovely people – who r the best Lyme disease doctors I can work with from the UK please. Loving Horirowitz, cowden, Byron white and klinghart philosophies but need a few more realistic options for my complex case. Esp those who will consult with uk patients. Many thanks Carly xx
I would check with ILADS. I am pretty sure they have a number of doctors in the UK. At their last meeting, I spoke to a few doctors from other countries (it is a huge problem worldwide) so would think they have members in the UK. Can also try ThyroidUK and see if any of the thyroid docs listed have CFS/FM/Lyme experience.
good luck
KH
HI,
Its Carly.
I have spent the past few months since this interview exploring options as I move forward with my journey. Unfortunately this year I have not been well at all and am determined to find a way to recovery. I wanted to firstly thank you all for your input previously and to also say that I am keen to document my progress as I go forward as I think there is a sense of us all here massively appreciating the advise and opportunity, but then feeling quite stuck as to the next move – or perhaps more specifically how to finance the next move… Therefore we are not necessarily seeing an actual outcome.
I thought long and hard about this and I want to be a proper recovery story where people can actually see results. I want to share this ongoing on my blog http://www.living-brightly.com
My sister has long since suggested to me that she sets me up an online fund-raising page but I had resisted it – for many reasons. I even wrote a blog post on my reservations here…..
http://living-brightly.com/wp-admin/post.php?post=3677&action=edit
Eventually however (through writing the above post) I realised I was doing her (and my family/friends) and myself a disservice by not taking this next inevitable step. If I have spent so long exploring root causes and immersing myself in healing, I need to now be brave enough to ask for help (without people feeling in any way obligated) to implement some action. I have therefore after much deliberation gone ahead and let my sister set up a fundraising page for me which I hope it is okay to share here with you in the hope you may even share it for me. Any help is much appreciated.
My Fundraising Page: http://www.gofundme.com/4c2t5b3kk2t?utm_medium=wdgt
With love
Carly x
@Cort
23? years later…. i think her blog said…. but most recent blog date was 2018 that i saw.
Carly mentions ozone treatment—
Cort, what is your perspective on recent developments on ozone treatment?
https://www.researchgate.net/publication/327926030_Ozone_therapy_is_an_effective_therapy_in_chronic_fatigue_syndrome_result_of_an_Italian_study_in_65_patients
Thanks Sunie…I hadn’t seen that.