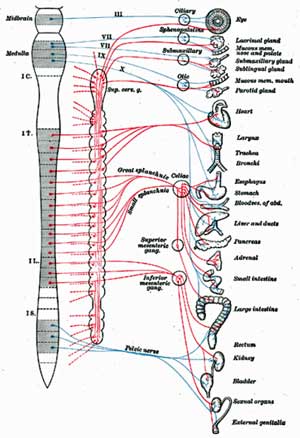
We know that increased activation of the sympathetic nervous (fight or flight) system is present in fibromyalgia but is it contributing to the pain there? Martinez-Lavin (“When Stress Causes Distress”) has been hypothesizing that it’s been a key pain driver in FM for years.
He’s shown that levels of norepinephrine – the neurotransmitter that turns the SNS on – are positively correlated with pain in FM. The higher the NE levels – the higher the pain level. He’s also shown that FM patients in severe pain tend to have alterations in some genes that control sympathetic nervous system functioning. The authors of this paper suggest that these findings suggest fibromyalgia may be similar to several to types of chronic regional pain syndrome (CRPS).
Other studies have associated increased SNS activity with poor sleep and reduced cognitive functioning in chronic fatigue syndrome (ME/CFS). Increased SNS activity has also been associated with increased fatigue in cancer survivors.
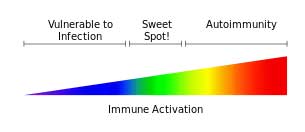
That may not mean that NE levels need to be particularly to cause pain. They may simply need to be high enough to send overly sensitive pain receptors into panic mode. Both Younger and Miller believe a similar scenario may be playing out with the immune system and the brain in chronic fatigue syndrome. They hypothesize that the brain has become so sensitive to cytokines that even normal levels may be causing it to overreact.
No one, however, has directly attempted to correlate SNS functioning with pain in FM – until now. These researchers assessed pain levels and examined a wide variety of autonomic nervous system measures in people with FM.
They also wanted to attempt to track down where the breakdowns are. Do they occur in the brain or in the system that controls sympathetic nervous system activity in the muscles (baroreflex) – or both?
The Study
The Brain
Heart Rate Variability (HRV) – The heart rate is regulated by a variety of electrical frequencies which provide a window into autonomic nervous system functioning. Low frequency (LF) electrical signals are regulated by the sympathetic nervous system branch of the autonomic nervous system. High frequency (HF) signals are regulated by the parasympathetic nervous system.
The Body
They also looked at sympathetic nervous system functioning in the body by examining baroreceptor activation and muscle sympathetic nerve activity (MSNA).
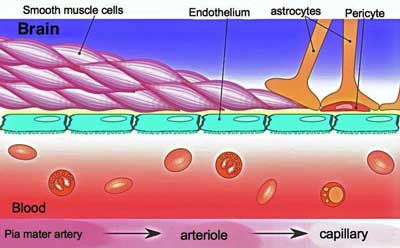
Baroreflex – Baroreflex receptors are stretch receptors found in the large blood vessels in the heart. As increasing blood pressure causes the walls of the blood vessels to stretch baroceptors send signals to the nucleus of the solitary tract (NTS) in the brainstem. The NTS then sends a message to the smooth muscles lining the blood vessels telling them to relax, thus lowering blood pressure.
Muscle Sympathetic Nerve Activity (MSNA) – MSNA refers to the activity of the small muscles in the walls of the blood vessels that control how large or narrow our blood vessels are. When your blood pressure drops these muscles tighten up the blood vessels in order to keep driving blood to the tissues. Increased MSNA activity (tightened blood vessels) also plays an important role in our ability to stand without blood pooling in our legs. These small muscles are entirely controlled by the baroreflex response.
Results
Brain
An increased heart rate had no effect on pain levels but an imbalance between sympathetic and parasympathetic modulation of the heart rate did. This study found that an increased LF/HF ratio (high sympathetic nervous system activity) was associated with increased pain in FM.
This part of the study is pointing not at the heart but the brain. It’s the brain, in particular, the hypothalamus and related “autonomic control” areas that regulate electrical activity in the heart. The altered LF/HF ratio suggests that problems with “central” or brain driven autonomic nervous system regulation are present.
Body
In this study, reduced baroreceptor activity was associated with increased pain in FM. Increased MSNA activity – a reflection of the reduced baroreceptor activity – was also associated with increased pain.
The authors suggested that problems with baroreceptor firing may be impairing the NTS’s ability to inhibit sympathetic nervous system activity in the blood vessels. Other studies have suggested that increased baroreflex activation triggers anti-pain signals, something that’s not happening in fibromyalgia.
The study indicated both the brain and the baroceptors were not regulating the SNS properly and that sympathetic nervous system activity was enhanced both in the heart and the blood vessels.
Treatment Suggestion
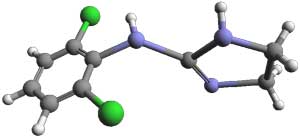
The authors suggested Clonidine, a sympathetic nervous system suppressing drug. Clonidine also reduces blood pressure, the heart rate, glutamate release and substance P levels and has antihistamine effects. These are all potentially good things for ME/CFS or FM.
Clonidine is used to treat a wide variety of disorders including high blood pressure, neuropathic pain, ADHD, night sweats, anxiety, alcohol and opioid withdrawal, restless leg syndrome, migraine and sleep disorders.
Clonidine seems like a good fit for either FM or ME/CFS and Dr. Peter Rowe has found it helpful with some of his young ME/CFS patients.
Wyller’s big 2013 ME/CFS study, however, found that low dose Clonidine not only did not help, but actually increased fatigue and decreased activity levels in his pediatric ‘chronic fatigue’ patients. Wyller’s vague definition of chronic fatigue puts a question mark on many of his results, but this study’s failure raises also questions about Clonidine’s effectiveness in ME/CFS. Clonidine certainly is helpful for some – a smaller study had positive results – but perhaps not many.
- Tried Clonidine? Tell us how it went in the Treatment Review Section of the Health Rising Forums here.
Head-Shaker
Some intriguing work in rheumatoid arthritis (RA) might help explain why. The type of autonomic nervous system dysregulation found in ME/CFS and FM – increased sympathetic nervous system and decreased parasympathetic nervous system activity – also occurs in RA.
First some background. Pro-inflammatory cytokines in the body are able, via the vagus nerve, to upregulate sympathetic nervous system activity in the brain. The brain then turns up SNS activity in the body. A major immune regulator, the SNS then upregulates Th2 immune (antibody formation, inflammation) functioning and inhibits Th1 immune (intracellular pathogen) functioning – an immune pattern believed present in ME/CFS.
The ability of the SNS to enhance inflammation in this manner may explain why stress can cause flares in RA and other immune mediated diseases.
Nothing, however, is ever simple in the immune system. Animal models of RA show that an intriguing time and disease dependent pattern of SNS/immune activation is also present.
Prior to the onset of arthritis SNS activation increases inflammation but after arthritis onset SNS activation actually appears to decrease inflammation. Some sort of immune network shift (aka Broderick) has clearly occurred.
This seemingly paradoxical shift suggests the decreased SNS activation Wyller achieved in his study might have inadvertently increased his patients inflammation and fatigue. (For myself energy and tension reducing treatments work for a bit, but ultimately leave me feeling fluish, It’s as if the tension is there for a reason.).
This doesn’t mean that SNS activation is “good” but that it may not be all bad. It certainly means that our systems are very complex. SNS de-activation may help in some and not help in others.
New Treatment Approach Proposed
Multiple inflammation producers appear to be present in both RA and ME/CFS. Increased SNS activity, low levels of the immune regulator cortisol, and reduced vagus nerve activity all may serve to increase inflammation in these disorders.
The authors propose upregulating the activity of the other side of the ANS – the parasympathetic nervous system – to bring down inflammation. The cholinergic anti-inflammatory pathway associated with the vagus nerve is a fairly recent discovery. A drug called GTS-21 that’s been tested in healthy controls, schizophrenia and Alzheimer’s is a possibility. Electrical vagus nerve stimulation is another. It’s being used in several diseases and was effective in re-balancing the immune system in refractory epilepsy.
Other Possibilities
Studies indicate that mind/body practices such as yoga (introductory postures), Tai Chi, Qi-Gong, mindfulness and meditation techniques can help to rebalance the autonomic nervous system. Several studies suggest QiGong and similar practices may be able to reduce pain to some extent in FM. The techniques Dan Moricoli used (pacing, light exercise, yoga, meditation) in his recovery all tend to suppress SNS activity and increase PNS activity.
A Naturopath proposes not over-doing exercise and the following to rebalance the ANS.
- Supplementation – The minerals calcium, magnesium, selenium, manganese and zinc are known for their calming effects, as are the amino acids GABA, and L-taurine and the herbs valerian, passionflower, skullcap and hops.
- Destress – Try to reduce the stress in your life as much as possible. This can include physical stresses such as noise pollution, environmental toxins, electromagnetic pollution and spinal misalignment.
- Think positive –Try to promote your parasympathetic nervous system through the use of meditation, affirmations, and through watching, listening to, and reading uplifting books and other media.
- Release negativity – Aim to steer clear of negative emotions such as fear, anxiety and blame.
- Cultivate inner peace – Let go of the need to control and choose contentment and peace.
- Breathe deeply – This activates the parasympathetic response and turns the sympathetic nervous system off.
- Meditate – Make time to still your system and just be – even if for only a few minutes a couple of times a day.
Conclusion
Autonomic nervous dysregulation is contributing to the pain found in fibromyalgia and may be affecting immune activity as well. Various ways to rebalance the autonomic nervous system – from drugs, supplements, electrical vagus nerve stimulation and mind/body practices – have been proposed.
- What’s on your Bucket List? Tell us on the Reverse ME/CFS/FM Bucket List thread in the Health Rising Forums here.







“it’s as if the tension is there for a reason”- i have often had this thought also because i find when i take a supplement that lowers inflammation -ie-pain-my energy drops even lower.(if that’s possible.ha!)
I wonder if the auto immunity to the blood vessels as theorised by fluge and Mella is what is happening to create this cascade??
I wonder if the auto immunity to the blood vessels as theorised by fluge and Mella is what is happening to create this cascade??
Could be – I just think the blood vessels have to be involved. We shall see, though.
Yes, as we have discussed, it might even be restricted flow at the point of the myofascia that is the problem. But if the blood vessel walls themselves can be stiffened up by stress, that would be enough to explain a lot – but it does not satisfy me as a cause of POTS-like symptoms in certain positions and not in other positions. If the blood vessels through the entire system were restricted as hypothesised above, then surely bicycling 30 miles in 1 hour 50 minutes (which I can do without a problem now) should be just as debilitating as 2 minutes of window cleaning or 5 seconds of squatting, or climbing 2 flights of stairs – all of which still leave me gasping for breath, heart pounding, and related muscles on fire with pain? Other things I can do without a problem, is leg-press 2.5 times my body weight, and have some pretty competitive arm-wrestles with some quite strong guys.
This contradiction of strengths and weaknesses is especially frustrating because it gives rise to assumptions of malingering and “attitude problems”.
I have always regarded chronic daily flight-or-fight stress response in a sedentary job, as what did the original harm to me.
The role of blood flow and blood vessel contraction in this study is very interesting, it fits with what I have recently hypothesised about POTS- type effects in fibro, once I had learned about the existence of POTS!
In my experience, it is certain postural triggers that cause problems to onset most rapidly; it is as if blood flow is permanently impaired at some particular locations and going into particular positions, like squatting, creates abnormal overload for the fibro sufferer versus a normal healthy person. But there is also an ever-present risk of overload of the whole body or nervous system, possibly due to the cumulative restrictions in the entire cardio-vascular system.
i have also mused on whether the myofascia is implicated; especially in the locations of permanent abnormal restriction. I am sure the tension effects go beyond the blood-vessel walls.
I strongly recommend changing everything possible in your life to avoid stress, and seeking therapies like massage and spas and stretches and enjoyable low intensity exercise programs and so on – rather than expect a magic bullet drug to fix you.
Valerian is not recommended for long-term use as it elevates cholesterol. Also, do not purchase GABA. Its large molecular structure prevents it from crossing the blood brain barrier. Instead, buy L-theanine, its precursor.
Clonidine has been shown in previous studies to have an ADVERSE effect on people with ME/CFS
http://www.shoutoutaboutme.com/news/clonidine-study-psychiatry-takes-a-beating-on-this-one/
As I noted in the blog
“Wyller’s big 2013 ME/CFS study, however, found that low dose Clonidine not only did not help, but actually increased fatigue and decreased activity levels in his pediatric ‘chronic fatigue’ patients. Wyller’s vague definition of chronic fatigue puts a question mark on many of his results, but this study’s failure raises also questions about Clonidine’s effectiveness in ME/CFS. “
Clonidine has actually been shown to have and ADVERSE reaction for people with ME/CFS in some previous studies.
So I’m not sure this can be generalized from research on Fibro.
http://www.shoutoutaboutme.com/news/clonidine-study-psychiatry-takes-a-beating-on-this-one/
I agree – that’s why I stated in the blog
“”Wyller’s big 2013 ME/CFS study, however, found that low dose Clonidine not only did not help, but actually increased fatigue and decreased activity levels in his pediatric ‘chronic fatigue’ patients. Wyller’s vague definition of chronic fatigue puts a question mark on many of his results, but this study’s failure raises also questions about Clonidine’s effectiveness in ME/CFS. “
thank you!
I was prescribed Clonidine for FM by my pain clinic several years ago, but it made everything worse and I was so fatigued I could not even function. My pain clinic abandoned Clonidine for FM about three or four years ago, as it seemed to make almost all FM patients worse. They now operate on the premise that the high SNS activity is a compensatory mechanism, and there are most likely some primary vascular problems. A little disappointed to see this being suggested by the study authors – if Clonidine was an answer we would already know that. There are far too many FM patients in the world to not think that clonidine (an extremely common drug) would have not already been tried. IT is a core treatment option for many pain conditions. just my clinic alone ( which is a hospital based clinic run by just TWO doctors) prescribed this to almost 500 patients before deciding it was too harmful to use with FMers.
I keep saying this but no-one listens or everyone is in denial…’internal ionisation radiation injuries’ broken chromosones & translocations worse than what was found in the Gulf War Vets at Wayne State University by Dr Henry Heng…Each time I hear the phycological pure b.s. I explode in a rage…If you got well through Phycological ways you never had CFS period…
Can this be related in any way to the Gupta Amygdala protocol and the way it “supposedly” works? Not saying it doesn’t work by the way, just that the protocol I have read about is very similar to the treatments mentioned in Other Possibilities, above. Appreciate your work Cort.
Sure..The Gupta Amygdala protocol and most of the mind/body protocols I’ve come across reference sympathetic nervous system activation…
So is it too simplistic to suggest that, no matter what the cause, or for the majority of causes, the Autonomic Nervous System is in distress (for want of a better word) and the first thing for a patient (my wife in this case) to try is a treatment that works to return the ANS to a balanced state?
My only questions then would be, “How do we measure the level of distress, so it can be monitored objectively during treatment?” and “What treatments are available that work?”
what about female issues? I had to have a hysterectomy last year do to cramps and bleeding
Hang on there Faith – you are not alone. We are going to do a blog on gynecological issues.
I have been suffering from FM since I was a kid apparently and only diagnosed recently. As far as sleeping goes, I have always “slept with one eye open”. I have never slept well. Always in agonizing pain. I have just stopped getting out of bed all together during the weekends and just started getting as much broken sleep as possible and by Monday mornings I feel sooo much better! It’s unfortunate that as the week goes on I feel the horrible pain all over again.