

(Thanks to Dr. Courtney Craig for allowing Health Rising to publish her blog on the possible benefits of ketogenic diets for people with chronic fatigue syndrome and fibromyalgia. Please note the title was changed and the links at the end of the blog were added by Health Rising.)
Being a ME/CFS patient in remission is a deeply humbling experience. Even though I think I have the illness under my thumb, there’s no doubt that something could happen to quickly turn the tables the other way.
I was reminded of this back in January.
First came the flu, with laryngitis so severe I could no longer teach my classes (or record podcast episodes!). Then came pneumonia. After 4 weeks came a secondary cold, then another. Next a rib strain so severe from coughing, it sent me to the ER because I was certain I had a fracture.
My immune system was hurting, and musculoskeletal injuries frequently set me into relapse because of the cytokine storm. By late February I was getting better. But my crushing fatigue was back, my sleep was disturbed, my muscles were weak. I was having trouble getting around on the subway.
Unfortunately, I was feeling like a ME/CFS patient again.
This relapse was a doozy! Despite throwing everything I knew at it, I was losing the game against relapse. Even intermittent fasting wasn’t doing the job.
I needed a serious immune and mitochondrial reset. So I shifted my usual paleo-diet around, and astonishingly I bounced back very quickly. I no longer felt like a ME/CFS patient. The illness was back under my thumb.
How’d I do it? I started consuming about 80% of my calories from healthy fats. Sounds crazy right? This is something I do periodically when the fatigue rears its ugly head. It’s also advocated by doctors like Dr. Terry Wahls for MS patients, Dr. Andreas Eenfeldt for weight loss, and Dr. Thomas Seyfried for cancer.
I flipped a switch on my metabolism. I stopped relying so much on glucose for metabolism, and instead encouraged my liver to break down those dietary fats into ketones—a much “cleaner” energy source.
The biohacker in me closely monitored this process with some inexpensive tools. Ketostix’s measure ketones in urine and a glucometer measures blood sugar and blood ketones.
Ketogenic diets have profound effects on the mitochondria, the brain, and immune cells, so why shouldn’t they be considered for ME/CFS and Fibro?
Periods of fasting are an excellent way to maintain ketosis but more intense fasts may be required in some people to achieve benefit. It’s a great way to do some cellular spring cleaning.
Ketogenic Diets

You probably haven’t heard about the ketogenic diet. It hasn’t garnered the media attention like Atkin’s, South Beach, or Paleo. The ketogenic diet, however, has been around since the 1920’s, and is one those in the ME/CFS and Fibro community might want to get to know.
First popularized in the 1920s as an effective treatment for intractable epileptic seizures, the diet is still used today for epileptics that fail medications. It has also been widely studied as an adjuvant in cancer and other neurological disorders such as Parkinson’s, ALS, and Alzheimer’s. A Cochrane meta-analysis highlighted the safety and effectiveness of this diet for controlling seizures (1).
Implementing a ketogenic diet is quite different than other big name diet plans. In order to become “keto-adapted,” the dieter must flip a switch on their metabolism. Instead of burning carbohydrate (glucose) for fuel, the cells must switch over to burning fats in the form of ketones. The downside of burning carbohydrate as fuel, is production of cellular stress and free radicals. Ketones provide a “cleaner” energy for cells and are less damaging to cell membranes. This could be compared to a car burning diesel (carbohydrate) versus a car burning unleaded gasoline (ketones).
This is not to say glucose is completely absent in someone who is keto-adapted. Dietary protein can also be a source of glucose for vital organs that require constant supply, such as the brain. Too much protein however, can cause blood sugar surges that stimulate insulin and “undo” the keto-adapted state.
A ketogenic diet can be initiated with a 12-72 hour fast. Then the diet is maintained by consuming 75-90% of calories as fat, with the remainder coming from moderate amounts of protein and very little carbohydrate.
The ketogenic diet is one that should be considered when dealing with ME/CFS, and perhaps even Fibromyalgia. A body of research in animals and humans have highlighted some of the mechanisms by which dietary ketones promote cellular health.
Here I highlight 3 compelling reasons why the ME/CFS and Fibro community should get to know ketosis.
Mitochondria
By their very nature as ATP-churning, energy machines, mitochondria produce an enormous quantity of free radicals. These radicals must be “quenched” by antioxidants to reduce the damage to the delicate organelle’s scaffolding. Glutathione, selenium, coQ10, and others play a key role in combating the free radical onslaught.
Mitochondrial dysfunction is widely recognized as a contributor to ME/CFS and Fibromyalgia symptoms. Indeed, many studies have determined that patients have depleted antioxidants, leaving mitochondria particularly vulnerable (2,3).
Ketogenic diets have been found to reduce free radical damage and thereby improve mitochondrial function. Also, ketogenic diets have been found to increase glutathione synthesis–the most important antioxidant for the mitochondria (5). In a recent study, fibroblasts from fibromyalgia patients were found to have decreased mitochondria per cell. When patients were given the metabolic drug metformin and prescribed caloric restriction (a means to achieve ketosis) the fibroblasts showed a more resilient response to free radical damage (4).
Immune
New studies are emerging demonstrating the role of ketosis in regulating the immune system. In animal models, a 72-hour fast that increases blood ketones, stimulates hematopoetic stem cells. These are cells that will differentiate into various types of white blood cells (6).
A blockbuster ME/CFS study is now underway studying the effects of the B-cell depleting drug Rituximab (7). This cancer drug may provide relief for a subset of patients through similar mechanisms as ketosis—out with the dysfunctional immune cells, in with new. Rituximab has also been studied in autoimmune diseases such as RA. Fasting studies in RA patients demonstrated reduced joint pain and inflammation, which suggests a similar mechanism (10).
Promoting a ketogenic state during the use of Rituximab may make the drug better tolerated and promote a more robust immune response. Ketogenic diets, achieved through fasting, are being studied as a cancer adjuvant to lessen the toxic effects of traditional chemotherapy in various cancers (10).
Neuroinflammation
The topic of neuroinflammation in ME/CFS is starting to gain traction as new research emerges. A Japanese group detected neuroinflammation on PET imaging (8). Newcomer Jarred Younger detected high levels of the pro-inflammatory molecule leptin in a cohort of patients (9). The effects of leptin occur in the brain and may promote “sickness behavior,” or more commonly, malaise. Animal models of ME/CFS have also demonstrated neuroinflammation driven by inflammatory antiviral molecules, like IFNγ. Increased IFNγ has been a consistent, yet non-specific, finding among ME/CFS research (2).
Ketones have demonstrated their ability to down regulate IFNγ and reduce leptin (10). Other pro-inflammatory cytokines have been shown to reduce in a ketotic state; IL-6 and IL-1β. Finally, ketogenic diets increase the production of BDNF in the brain, which stimulates neuronal stem cells and repairs damaged neuronal connections–a potential perpetrator of the dreaded brain fog (10).
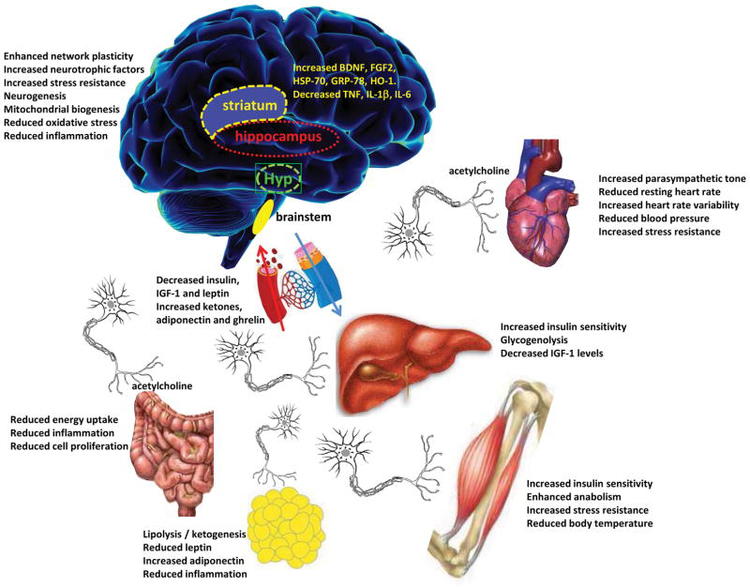
Summary Of Ketogenic Diet Effects
- Increases glutathione production
- Increases BDNF gene expression
- Increases mitochondria concentration
- Stimulates hematopoetic stem cells
- Reduces inflammatory molecules (leptin, IFNγ, IL-6, IL-1β)
- Reduces oxidative stress at the mitochondria
____________________________
Dr. Courtney Craig D.C. was first diagnosed with CFS as a teen in 1998, and recovered in 2010 utilizing both conventional and integrative medicine.
Trained as a doctor of chiropractic and nutritionist, she now provides nutrition consulting and blogs about what she’s learned at www.drCourtneyCraig.com/blog.
- Check out more of Dr. Craig’s Health Rising blogs here
Dr. Craig offers online nutrition consultations to patients worldwide looking to change their diet. Get the details in a free 15-minute call.
________________________________
Health Rising
- Check out resources on ketogenic diets including recipes in the resource section of the Health Rising Forums
- If you’ve tried a ketogenic diet please tell us how it went in our review section.
Trending on the Health Rising Forums:
- How well informed was the last doctor you saw?
- Do you think having more money would improve your health?
- If you could do it all over again – what would you do differently?
_____________________________________
1 Levy RG, Cooper PN, Giri P. Ketogenic diet and other dietary treatments for epilepsy. Cochrane Database Syst Rev. 2012 Mar 14;3:CD001903. http://www.ncbi.nlm.nih.gov/pubmed/22419282
2 Maes, M, et al. Increased plasma peroxides as a marker of oxidative stress in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Med Sci Monit. 2011 Apr;17(4):SC11-5.http://www.ncbi.nlm.nih.gov/pubmed/21455120
3 Cordero MD, et al. Oxidative stress and mitochondrial dysfunction in fibromyalgia. Neuro Endocrinol Lett. 2010;31(2):169-73. http://www.ncbi.nlm.nih.gov/pubmed/20424583
4 Alcocer-Gómez E, et al. Metformin and caloric restriction induce an AMPK-dependent restoration of mitochondrial dysfunction in fibroblasts from Fibromyalgia patients. Biochim Biophys Acta. 2015 Mar 14. pii: S0925-4439(15)00069-1. [Epub ahead of print] http://www.ncbi.nlm.nih.gov/pubmed/25779083
5 Swann JW. How Does the Ketogenic Diet Work? Epilepsy Curr. 2004 Jan;4(1):20-21.http://www.ncbi.nlm.nih.gov/pubmed/15346140
6 Cheng CW, et al. Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cell-based regeneration and reverse immunosuppression. Cell Stem Cell. 2014 Jun 5;14(6):810-23.http://www.ncbi.nlm.nih.gov/pubmed/24905167
7 Fluge Ø, et al. Benefit from B-lymphocyte depletion using the anti-CD20 antibody rituximab in chronic fatigue syndrome. A double-blind and placebo-controlled study. PLoS One. 2011;6(10):e26358.http://www.ncbi.nlm.nih.gov/pubmed/22039471
8 Nakatomi Y, et al. Neuroinflammation in Patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: An 11C-(R)-PK11195 PET Study. J Nucl Med. 2014 Mar 24;55(6):945-950.http://www.ncbi.nlm.nih.gov/pubmed/24665088
9 Stringer EA, et al. Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: evidence of inflammatory pathology. J Transl Med. 2013 Apr 9;11:93.http://www.ncbi.nlm.nih.gov/pubmed/23570606
10 Longo VD & Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell Metab. 2014 Feb 4;19(2):181-92. http://www.ncbi.nlm.nih.gov/pubmed/24440038






Mm, nice article. I’ve tried a few times recently to go ketogenic. Each time, though, after many weeks of trying I just felt even more exhausted, with terrible dark circles under my eyes and no improvement in brain clarity.
I have Reactive Hypoglycemia, though, which means too much insulin, with the insulin preventing fat-burning. I recently read somewhere that protein invokes even more insulin production than carbs; perhaps I need to cut down the protein right down as well.
I’ll try again…
Yes, the article says:
“…Dietary protein can also be a source of glucose for vital organs that require constant supply, such as the brain. Too much protein however, can cause blood sugar surges that stimulate insulin and “undo” the keto-adapted state…”
A friend of mine was on a high-fat, ketogenic diet for about 8 years because of seizures, and he seems to have ended up pretty healthy and well-developed physically. There does not seem to be any of the horror threats from many dieticians, about the heart and the arteries and so on, come true.
Many people seem to thrive on Atkins and on this even more severe diet.
I think we are all different, and one of the biggest causes of failed treatment approaches in all branches of medicine, is the “one protocol for all” approach. I think probably every health condition needs to be approached bearing in mind WHAT group of different types the patient belongs to. Even the very simple theory underlying “the blood type diet” might explain a lot.
Logically according to that, people who do well on Atkins etc will be blood type O. People of other blood types may be those for whom Atkins and Ketogenic is not good.
I would also be interested to know whether there are any particular blood types NOT represented among fibro victims, and CFS victims. Are us type-O’s more prone to fibro? I wonder?
Good point Phil
Meta analyses has not supported blood type diets. Nonetheless I’m A+
My daughter is B negative and she has fibromyalgia. it would be interesting to do a survey to see
How do I eat a diet 75-90% calories as fat – specifically in meals…
Steve, I’d encourage you to get Dr. Terry Wahls book, The Wahls Protocol. She has 3 levels of diet in her book – with the third one being a ketogenic diet. She lays out all the details of this diet. (Disclaimer: I don’t agree with her personal beliefs, so I’m not advocating 100% of her book, but her medical and diet information is ahead of the game. That’s just my personal opinion, which may not be worth much. I just think her material makes sense, and as for your question, her book would probably give you the information you are needing. She also has a facebook page where a lot of information is shared. Dr. Wahls has MS, but has greatly improved with the ketogenic diet. Many who follow her, and have been helped as well, have other autoimmune issues – not MS. Another page on facebook run by a woman who utilizes Dr. Wahls ketogenic diet protocol (and shares yummy recipes) is called “MS Saved My Life”. I deal with CFS – not MS, but I love keeping up with her page.
75-90% of calories from fat does not quite mean your whole plate full of food is fat. Cheese for example is roughly 1:1 grams of fat to protein, but because fat is more caloric than protein it works out as around 2:1 in calories for a 1:1 by weight. So most fatty cuts of meat would provide this. With perhaps the extra fat provided by having a salad with olive oil for example.
I recall reading a study that ketosis (which I’ve used extensively) was detrimental to glutathione. Can you please elaborate your opposite claim?
Good question, David. Helpfully, Craig’s claim is footnoted. I read the cited source–it is a commentary in the journal Epilepsy Currents regarding a study of neuronal excitability in rats. (Of course, we all know how excitable the dentate gyruses of Sprague–Dawley rats can be in response to angular bundle stimulation! Am I right, people?)
Neither the study, nor the commentary, mention glutathione.
I haven’t checked Craig’s other cites, but this misrepresentation alone should inspire you to read the original source materials before blindly accepting any of his bolder claims. (Of course, this is good practice with any author, in any subject of importance.)
Hi Dr. Craig, how long would you suggest a person stay on a ketogenic diet to give it a fair trial. Of course I’m talking about a ME/CFS patient.
thanks, David
Good question. Also – if side effects occur – when should you stop and when should you keep going?
Any dietary change should be given a good 30 days or so to adequately assess. As some other commenters have mentioned, side effects may result with inadequate water intake, salt, and nutrients. It will be a different experience for everyone, so that’s why monitoring urinary/blood ketones is such a valuable metric. Working with a healthcare provider is also advised!
Where can I find a detailed ketogenic diet plan?
Where can I find a detailed ketogenic diet plan
Why do I keep repeating myself?
I don’t know 🙂 🙂 🙂
There are links to recipes and diet plans at the bottom of the page in the Health Rising section.
The eBook Ketoclarity is a good place to start but there are also many other online resources.
Dr. Terry Wahls has good information detailing a ketogenic diet.
The number one killer of Americans is heart disease. 75-90% of calories as fat?? What is that doing to our hearts and circulatory systems? The Atkins program was originally based on the ketosis principle. Atkins was grossly overweight and had cardiac issues before his death from head trauma.
All the other risks of ketosis also need to be taken into consideration.
Apperantly changing the fat americans use to eat for carbs is what lead to that overweight epidemia.
Science no longer supports a connection between high intake of saturated fat and heart disease. This article covers it: http://well.blogs.nytimes.com/2014/03/17/study-questions-fat-and-heart-disease-link/?_r=0
I also remember a recent TIME cover stating, “Eat Butter.”
Thanks Johannes
I tend to agree with Michael Pollan who says to eat real food and not much of it. I know there are conditions that are helped by a high fat diet but I still can’t buy into the animal protein. The article mentioned inflammation and I was wondering Cort if you’ve ever done a survey of your readers who have had their C-reactive protein tested? I recently had mine and it’s .5 which is low. I’ve read about CFIDS or Fibro maybe being an inflammatory process – does the C-reactive protein show whether that’s the case? Would a latent virus increase the C-reactive protein?
It’s my opinion that Dr. Atkins did not continue to follow his own diet…
dr craig, can a person who has hashi’s on top of me/cfs/seid do a ketogenic diet?
Yes, ketogenic diets are also being studied for autoimmune conditions. Dr. Terry Wahls advocates this type of diet for multiple sclerosis in particular.
please don’t allow false information about Atkins death to go unchallenged – as the statement from his widow and doctor make clear the weight gain was fuid retention and his heart healthy before a viral infection http://usatoday30.usatoday.com/news/health/2004-02-10-atkins-statements_x.htm
An Atkins diet made me so ill so I didnt stay on it and fat would now have me running for a toilet but you can always get some of the fat in the form of oily fish and have your HDL/LDL and homocysteine levels measured
As someone who has CFS and has been on the ketogenic diet for about 6 months I could not recommended it highly enough. It hasn’t cured me but it has made a drastic improvement to my life. There are less crashes, my energy is more even throughout the day, my moods are better, complexion is clearer, less brain fog I could go on forever.
For people worrying about fat consumption there is plenty of scientific evidence which is now showing that healthy fat isn’t the cause of heart problems and sugar and carbohydrates are to blame. If you are interested in starting the diet go to http://www.reddit.com/r/keto they have plenty of links and resources and people in all stages of trying the diet. They really helped me and pretty much any question you have can be answered there!
A word of caution though it is really important to do the diet properly, it’s very easy to not be getting your essential nutrients and you need to drink plenty of water.
Otherwise definitely try it! I’m staying on this diet forever!
Ketoer, I’m so glad you feel so much better – perhaps I’ll try this. I checked out the site you gave though and it said there is no evidence of heart disease being linked to animal fat. Really? I thought there were numerous studies linking animal fat with not only heart disease but cancer. I have read about the benefits of healthy fats such as coconut, olive, avocado oil, nuts etc but I can’t imagine that eating a large percentage of animal fat would be good for anyone. What percentage of your ketogenic diet is animal vs plant fats?
It’s surprising and with everything we have been told our whole lives about fat it seems almost naughty eating so much. But I always remember my whole life thinking why would eating fat be so wrong all animals naturally go for the fattiest parts of an animal. It’s only recently that humans have decided to eat all the lean parts. Fat is absolutely essential to the human body many of the cellular processes rely on fat.
From the research I’ve read it seems that eating high carb in combination with high fat is where all the problems start occurring which people attribute to fat. Also the myths we have been told about cholesterol just aren’t true. It is important in the body and it’s function is to repair and protect arteries.
I realise it sounds like i’m just pulling these things out of my head but I have carefully looked into this. I used to be someone who’d say it’s not healthy to cut out a whole food group. But another good place to start looking is if you look into Gary Taubes work. He has a few lectures on youtube, has written some books and has appeared in various documentaries.
Generally keto percentages are 60-75% fat, 15-30% protein and 5- 10% carbs. The carbs of course are in vegetable form. You can go higher in fat but most people don’t go as high as 75-90%, as the article says, I’m not sure it’s necessary. But for my diet I’d say maybe 60% of my fat intake in from animal products. I eat a lot of nuts, olive oil and coconut oil but I find it’s much harder to eat those in large quantities than fatty cuts of meat or buttering vegetables.
Another thing that’s probably worth keeping in mind is that there is a withdrawal period and it seems like a lot of commenters got stuck at that point. It’s not pretty but when you come out the other side it’s amazing. It’s a great lifestyle change but if not done properly can just make you end up feeling worse.
Thanks Ketoer – I’ve been on a plant based diet for years and won’t support factory farming but I might consider eating a chicken who had a great life and then is suddenly gone. I read that Dr. Wahls recognizes some people won’t eat meat due to their religion etc and she says although she prefers they do, her diet can be done without using animal products. Personally I’m not sure our bodies are designed to eat meat but if others have been helped it’s worth a try and keeping an open mind to everything….
It’s definitely hard eating animals. I try to get as much of my meat free range or from good farms I know. I find I feel much worse if I cut out animal products. But there are plenty of vegetarian ketoers. There’s another keto sub reddit (on reddit.com) dedicated to vegetarians sorry I can’t remember the exact link if you search around you’ll find it. They always share lots of good recipes and advice.
Good luck with it all. I really hope you see some improvement!
Interesting. I’m severely affected and once tried a diet that got me into ketosis, but after three weeks I had to give up as my pain levels got so much worse. I also know of someone else who tried a similar diet and it caused a long lasting relapse
I have tried The paleo diet without carbs, but my night panics got worse and worse. I think it must be related to low blood sugar levels and not properly functioning adrenals. So although I like the theory in this article, it doesn’t seam feasible for me unfortunately.
I have tried a very low carb diet many times but it always makes me worse, my body just cannot function without a small amount of carbs together with fat and protein.
Its because I have such bad adrenals to the extent I am steroid dependent on 6mg Prednisolone daily. My brain and body seems unable to use fat for energy, I end up so dizzy I cannot do anything. I also have Hashimotos and take dessicated thyroid.
By eating just a small amount of no sugar carbs, protein and fat I am able to do quite a lot, around 8000 steps daily since being on the Cowden protocol to deal with borrelia but if I was to stop these carbs I wouldn’t be able to exercise at all so for me it just isn’t doable.
Because of having to take the Pred it does mean its extremely difficult to keep my bs down unless I exercise so I never eat sugar, bread, pasta or rice and yet still in an evening especially my bs is too high so I am going to try and have to do a bit of exercise. This is very difficult because by 7 pm my body is worn out and I need to rest!
Hey fellow sufferers I have tried to lose weight on the Atkins, and would lose weight quickly, but I also within about a 9 day period would have such dehydration that my nerves are crawling in my neck. I tried drinking at least 1/2 gallon a day of water only to deplete my sodium so much that I was having the nerve issues. I started taking sodium pills, and it helped a little, but I also had to stop the diet. Very frustrating because when your so sedentary its hard to lose weight. Before my illness I struggled with weight loss, until I started working out every day, then it dropped off, but that’s out of the picture now. I would love to try this, but its so close to Atkins that I am afraid of the same outcome, I think with the blood volume issue we have, that its harder for us to do anything that makes such a shift in our bodies.
Like any diet it’s not for everybody. We just got this review in the Health Rising Forums:
“I am amazed after looking at the ketogenic diet because I have done this basic diet for over seven years, yet I never called it ketogenic, I called it a hypoglycemic diet. It was recommended by my fibromyalgia specialist, Dr. St. Amand, who is an endocrinologist. I suspected I was hypoglycemic when I was introduced to this diet in 2007, so was very happy to have some specific directions on what to eat.
My symptoms were IBS, bloating, frontal pressure headaches, fatigue and most specifically to HG, an inner shaking or trembling when hungry and an urgent need to eat. I had a couple of episodes of rapid heartbeat prior to the diet also and once became faint and went to the ER.
As I have continued with the diet over the years, I find that if I eat too many carbs in the form of low carb fruits (I do not eat grains except for gluten free oats occasionally) I will become tired and bloated.
This diet has had a huge impact on my ability to function, feel good, and exercise, think, etc. I am thrilled to see the additional science behind why I do so much better eating this way!”
I followed a ketogenic diet to treat my ME/CFS for 3 months and this is what happened. The first month and a half I saw no improvement. Around the second month I slept more than I ever had since I got sick. I would sleep from 1am till 10am. Wake up, eat breakfast and go back asleep till 2pm. I would spend the rest of the day resting. This lasted for a few weeks and I thought I was just experiencing a bad crash. I was sure the diet was not working. Turns out my body was addressing some serious issues and finally one day the big improvement came. My muscle pain was completely gone and my energy had increased 10%. I stopped the diet (continued paleo) shortly thereafter but I am plan to do another round to get even more improvement. My muscle pain has still not returned 2 months later! This was the only treatment I was doing at the time (except for acupuncture) so I can honestly this made a difference for me. I was not taking ANY supplements at the time (ok so maybe a probiotic).
For those of you that want advice on how to start a ketogenic diet, read Dr. Terry Wahls book the Wahls Protocol. She has a ketogenic diet meal plan along with instructions and descriptions. She uses coconut fat as the source of fat for the diet, which is a shorter fatty acid chain and requires less energy to digest. Another perk is that large amounts of coconut fat contain an antiviral fat called monolaurin.
Finally, I will say that I also did an elimination diet while on my ketogenic diet and was able to identify my sensitivities to nightshades.
The only side effects I noted from the ketogenic diet were occasional increase IBS like symptoms and weight loss (Good for some people ,but I am underweight and have trouble gaining on a paleo diet)
So all in all I would say depending on how sick you are, I was 90% bedridden at the time, ketogenic diet may take some time to help. Also you may get more tired before you feel the benefit as your body starts to heal some damage. Hope this is helpful!!! Good luck everyone.
What an amazing story Sophia. Thanks for sharing it. It brings up the question when to stick with it and when to quit…Man oh man…
I’ve tried and failed the Atkins diet many times. Can’t seem to do any diet that’s extreme in any particular direction, be it low-carb, no-carb, high-protein, high-fat, whatever. They all just make me feel worse, not better. The best explanation (for me) is presented by Diana Schwarzbein, the endocrinologist who wrote The Schwarzbein Principle books. She believes the key is knowing how your adrenals are functioning. People with strong adrenals, she says, can successfully do diets like Atkins and Keto diets. But people with adrenal fatigue need a balance of fats, carbs and protein, and often get worse on diets that strictly limit or greatly emphasize any particular food group. This seems to be true for my body. YMMV.
How would you know how well or not your adrenals are functioning?
I arrived at a low carbohydrate diet as being the best for my health condition years ago. Avoiding all forms of sugar including fruit has been critical for me. When all the rhetoric about low fat diets being best for you was popular I ignored it and followed my “gut” eating liberal amounts of butter, animal fats and oils. After 40 years on this diet a recent Coronary Calcium Scanning Report showed a zero score of of calcified plaque in my blood vessels or arteries.
Persons with CFS do however have cardiovascular dysfunction manifesting itself as low cardiac output. The heart is operating more slowly and stimulates including dietary sugars can aggravate this condition. This is the reason I think this diet works. From time to time I expand my diet to include more carbohydrates and supplements, then my heart fights back and I have to take a break from these things so my cardiovascular system can rest and catch up.
all very well to say there is a “withdrawal period” but I went on for a week after I started felling pretty bad and it only made me feel sicker by the minute. I cant process large amounts of fat, even healthy fats. Some of us do not have great digestive systems.
You, and others, might consider using MCTs (Medium-Chain Trigerides) to jump start your keto-adaption. MCTs, the main type of fat in coconut oil and, maybe, butter, are easier to digest and absorb than LCTs. [LCT=Long-Chain Triglyceride, the predominant type of fat in most foods.]
From http://nutritionreview.org/2013/04/medium-chain-triglycerides-mcts/ :
“In contrast to LCT, MCT are more rapidly digested, and the resulting MCFA are more rapidly absorbed via portal circulation than the corresponding LCFA which are re-esterified and packaged into chylomicrons for lymphatic absorption.”
I.e., they get to skip a big part of the digestive process, and don’t have to be ferried through the lymphatic system. Once absorbed by cells, the MCTs are converted into ketone bodies:
“The energy-enhancing properties of MCTs are attributed to the fact that they cross the double mitochondrial membrane very rapidly, and do not require the presence of carnitine, as do LCTs (Fig. 2). The result is… the production of ketones. Scientists attribute the increased energy from consumption of MCTs to the rapid formation of ketone bodies. MCTs are thus a good choice for anyone who has increased energy needs, as following major surgery, during normal or stunted growth, to enhance athletic performance, and to counteract the decreased energy production that results from aging.”
…Or ME/CFS, one assumes. The brain doesn’t utilize fat for energy, but the liver converts MCTs into ketones and releases them into general circulation. The brain loves ketones. Many (normal) people report thinking more clearly with elevated ketone levels.
Supplementing your diet with MCTs (from MCT-rich foods, or MCT oil from a health-food store), will provide you a greater supply of ketones without your going into ketosis via dietary restriction. I would think that training your body to utilize ketones for a period of time before dietary restriction might ease the pain of that transition. (Also, I believe that ketone supplements are now available and would be useful for this purpose.)
I’ve occasionally used MCT oil in my food preparations–it is a light, flavorless oil, suitable for dressing salads. I believe I’ve also sauteed with it, perhaps eggs, though I’m not sure what its smoke point is. It is used in “Bulletproof Coffee”, and I’ve used it there, though I guarantee it will cause diarrhea, at least initially. Try a teaspoon at first, then ramp up from there. I’m not the best source of info on this topic, though, so search around the internet.
The problem with MCT oil is that it does not include Lauric acid which is the most abundant MCT in coconut oil. Seems it would be best and probably a lot cheaper to just consume the natural coconut oil and get all of the MCT’s.
http://healthimpactnews.com/2014/mct-oil-vs-coconut-oil-the-truth-exposed/
Reason some people with CFS recover is very obvious they have the less form of EDS the ones with type 4 EDS will not get well…
If you have ME, is it safe to take the KETO tablets to jump start your keto diet?
I was diagnosed with Fybro and CFS back in 1996…suffered for years kept working at my job, then went back to School…began working out…changing my diet here and there…but it wasn’t until I was living in the Arctic eating a total Paleo (northern) Diet that I saw real changes…and once I moved South again and became an “almost” vegetarian( still use Organic heavy cream, free range chicken EGGS and Wild caught Salmon and Shrimp) did I notice the most drastic change in my overall health… I follow Keto with IF (16:8) best thing ever…. NO PAIN…NO FATIGUE…healthy blood and thyroid I’m 56 next month feel better than I did at 36 when all this crap started happening….
Wow.
A move to the Arctic sparks an improvement -that’s a new one! (Who knew?) What the heck were you doing in the Arctic?
Congrats on getting better. I’m pretty much going full keto now.
I would posit that anyone who has success with a Keto diet does not have ME/CFS and your chronic fatigue is caused by something else. The 2-day CPET is the gold standard test to prove post exertional malaise, the hallmark of ME/CFS. This test shows the body is mostly in an anaerobic state and energy is derived from carbohydrates almost exclusively. This would indicate a fat metabolism disorder and Keto would be contra-indicated. You cannot ‘teach’ your body to burn fat if the Krebb’s cycle simply cannot do it b/c of mitochondrial dysfunction at the cellular level. Please expound upon this thought train.
Hi Cheryl,
I just came across this article (which then led me here):
https://www.newscientist.com/article/2121162-metabolic-switch-may-bring-on-chronic-fatigue-syndrome/
I was thinking this might indicate why someone with ME would have difficulty losing weight (sugar not be used by the body is converted to fat, no?) …. and that maybe keto would be effective for such a person…? So much conflicting info!
I’ve skimmed over a few articles and studies but I don’t have the energy/time to really absorb (or sometimes even understand) it all.
I’d love to hear your thoughts, though!
Thank you!
Thanks to Dr. Craig for a great article!
One thing worth noting: for the 25% or so of the population who carry at least one copy of the APOE-ε4 allele, ketosis might not help much, if at all. Research is still unclear on this. But that of course doesn’t mean that fasting, via some other mechanism (lowered mTOR, autophagy, etc.) wouldn’t help.
And, unfortunately, it’s not inconceivable that APOE-ε4 is over-represented in people with ME/CFS/SEID. (This is the hypothesis being tested by Hector Bonilla.)
Thanks again,
Brian