



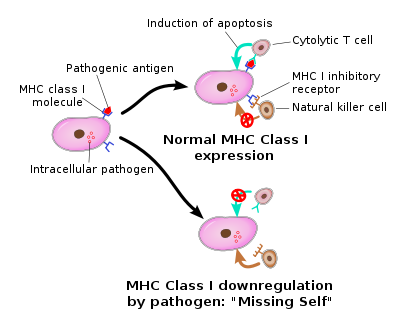
Natural killer cells appear to be the ground zero for the immune dysfunction found in chronic fatigue syndrome. These cells are, as their name implies, killers. They’re called “natural” killer cells because in contrast to cytotoxic T-cells which need to be activated to fight infections, NK cells are always “on”; they’re always prowling the bloodstream for damaged or infected cells. Apparently, when you constitute the first line of immune defense in the human body, you don’t take time off.
Unfortunately, in ME/CFS NK cell’s bark is worse than their bite. Studies have consistently shown that the NK cells in many ME/CFS patients appear to be lethargic and burnt out. They simply don’t kill as many infected cells as healthy natural killer cells do.
The NK cell dysfunction in chronic fatigue syndrome has been evident for years, but an even more insidious problem may be present. Several studies now suggest that the powerful killers featured in the adaptive or late immune response – the cytotoxic T-cells – have the same problem in ME/CFS as do the NK cells.
If that’s true, then both the early and late immune responses are inhibited in ME/CFS.
Novel Antiviral / Anticancer Agent Found
- Science DOI: 10.1126/science.aaa7516. The protein LEM promotes CD8+ T cell immunity through effects on mitochondrial respiration. Isobel Okoye, Lihui Wang, Katharina Pallmer, Kirsten Richter2, Takahuru Ichimura,…..Philip G. Ashton-Rickardt1,3,‡
Unfortunately no readily available drugs are able to improve NK or T-cell functioning. A recent breakthrough could change that, though. Imperial College researchers in London uncovered the presence of a novel protein that appears to dramatically boost both antiviral and anti-cancer defenses.
It took a large team six years. First, they found a strain of mice with dramatically enhanced T-cell responses that was able to more quickly fight off viruses and cancer. Using sophisticated gene screening they uncovered the gene responsible for the mice’s extraordinarily effective immune system. Then they found a heretofore undiscovered protein that the gene was producing. They called it “lymphocyte expansion molecule” or LEM.
In a wholly unexpected finding researchers uncovered an novel protein that regulates important aspects of the immune response
Interestingly, given the current interest in the mitochondria in ME/CFS, that protein turned out to be a mitochondrial booster. LEM effectuates cytotoxic T-cell responses by turning on the mitochondria in cytotoxic T-cells.
With the aim of bringing gene therapy to improve immunity to the market the London team has filed two patents on ways to enhance LEM in humans. Mouse trials will begin quickly and they hope to begin human trials within three years.
The findings may eventually result in a new approach to fighting viruses and/or cancer.
“This study has identified the novel protein LEM and unlocked an unexpected way of enhancing the ability of our immune system to fight viruses or cancers. This is based on the ability of the protein LEM to regulate specific energy circuits, and particularly mitochondrial respiration, in a subset of white blood cells known as cytotoxic T cells. This discovery has immediate consequences for the delivery of innovative therapeutic approaches to cancer.” Claudio Mauro, Ph.D.
ME/CFS Connection?
The relevance of this finding to ME/CFS is unclear. The news accounts of the study focused on LEM’s ability to increase T-cell proliferation. A recent study suggested that T-cell proliferation is inhibited in ME/CFS, but the biggest concern in ME/CFS is reduced cytotoxic T-cell functioning. The reference in LEM studies abstract to increased “effector” functioning, however, could suggest cytotoxic T-cell killing ability was enhanced as well. If that’s true the protein could have direct relevance for ME/CFS.
NK Cell Connection?
We don’t know that LEM has the same effects on NK cells as it does on T-cells. Both cells, though, employ the same type of killing machinery to remove infected cells and, perhaps importantly, similar “signalling cascades” to control the “effector functions” in T-cells.
Reduced NK functioning is not the result of low NK cell numbers in ME/CFS. It’s possible, though, that increasing NK cells could be helpful in the same way that increasing cytotoxic T-cells are projected to be. Even healthy humans have trouble generating enough cytotoxic T-cells to fight off infections or cancer. The London hopes this new protein will help patients to get rid of lingering viruses or tumors.
The other major caveat is that the finding was in mice. As Mark Davis put it – mice diverged from humans 60 million years ago. They have four legs we have two. Their hearts beat 400 times a minute. Ours beat 60 times a minute. They’re different. That doesn’t mean they’re not useful; many of the immune discoverers for humans have taken place in mice, but they are different.
There are too many if’s and’s or but’s to determine what relevance, if any, this finding has for ME/CFS. The discovery of a novel protein that plays a key role in the immune systems ability to fight off viruses and cancer is encouraging, however, in and of itself. It underscores how much yet there is to learn about the immune system and what surprises may be in store as researcher dig deeper and deeper into this complex system.
Inquiry of the Day – Health Rising Forums
Have you had your NK cells tested? If so, what were the results? Tell us here...







Excellent article! Thanks Cort.
Thanks Mike. I love how the new gene sequencing technology opened the door for this discovery.
Hi,
Just put my vote in for the NK CELL TEST. Would you call the bottom 10% of the reference range …. Quite low or scary low?
Thanks for all the updates.
Linda
Personally, I would call anything in the ten percent range scary low 🙂
Cort, Where do you find this stuff?
The Forums made me do it, actually…
Cort, Where do you find this stuff. Also, you comment box leaves an error if you stick in a question mark.
How weird – thanks for letting me know.
My comment disappeared after confirmation of submission.
Short version: LEM (by Asian names) has been successfully used in Asian herbal formulas for thousands of years. Searches on various engines will reveal the researchers and medical journals. It is available now to sufferers through licensed acupuncturist-herbalists. Big Pharma may try to mess with it by changing a molecule and patenting that, but it will not be as safe nor have the same effect.
From Cort’s article: “Several studies now suggest that the powerful killers featured in the adaptive or late immune response – the cytotoxic T-cells – have the same problem in ME/CFS as do the NK cells.” (lethargic and burnt out)
**************************
Again, I find, that we don’t all seem to be suffering from the same illness, or immune system problems with ME/CFS. I have the overactive immune system type of ME/CFS described here: Overactive Immune System “In one study, some patients, particularly those with severe CFS symptoms, had higher-than-normal numbers of infection-fighting white blood cells known as CD8 killer T cells, which launch attacks on invading viruses and other disease-causing microorganisms. These same people had lower-than-normal levels of another white blood cell known as the suppressor T cell, which helps to shut down the immune response once the invading organisms have been killed. In such cases, the immune system becomes persistently overactive and produces fatigue, muscle aches, and other symptoms of CFS.” (1) That’s me!
The other type of CFS seems to be the result of deficiencies in Natural Killer Cells described here: “Other studies have indicated lower amounts of so-called natural killer cells in many CFS patients, which might make them more susceptible to viruses.”(2) That’s not me, I never get cold, flues, infections or viruses! We may all have immune system abnormalities, but they certainly don’t seem to follow a consistent pattern. Some of us seem to have immune systems that are on fire, and others seem to have immune systems that barely function. Sometimes, I feel so discouraged by all these opposite symptoms/findings regarding ME/CFS
(1) (2) http://preventdisease.com/diseases/chronic_fatigue.shtml
Rachel, that is me too. I don’t get anything even when I am around people who are sick. My symptoms are fluish – headaches, exhaustion, a lot of the typical (for some) symptoms but that is all the time not the result of another illness.I have a friend with me/cfs and she is almost a polar opposite and gets everything that is around.
Margo: Adrienne Dwello who writes about ME/CFS and fibromyalgia for about.com had an interesting perspective when comparing immune markers in men with Gulf War Syndrome and women with ME/CFS. She wrote, “This raises an interesting question in my mind: Is there a spectrum of these endocrine-immune dysfunctions, and does effective treatment depend on where you fall on that continuum? For example, let’s put men with GWI on one end and women with ME/CFS on the other, since we know that, in general, they have exactly the opposite things going on.” Could one day ME/CFS, in itself, be considered a spectrum disorder and would valid treatment be dependent on where you fall on that spectrum?
http://chronicfatigue.about.com/b/2014/01/17/new-models-of-chronic-fatigue-syndrome-gulf-war-illness.htm
Rachel I know that the internal doc that diagnosed me said he felt that ME and FM were on a spectrum – ME with more exhaustion and FM with more pain but many shared symptoms. I often wonder if it is a system disfunction reacting to assault/trauma rather than discrete virus etc. I really feel I have had this most of my life at least from my early 20’s and now in my 60’s I don’t have the body youth/resilience to counteract it anymore.
Thanks for the info, I will check out the link on a non-brain fog day. It took too long just to compose this. 🙂 Some days remind me of learning other languages when I would mix up yes and no, right left etc. because now I have that difficulty with English!
I can’t wait until they separate out these subsets! That’s going to be great news for each of them. I wonder if the multi-site study is going to help in that regard (???). I don’t know how many lab scores they’re examining…
I never catch anything either. But just had my NK function tested by Dr Vera. She said only one third were working. After reading some posts here that doesn’t sound all that bad, but still seems low enough I should be catching stuff?? Went from missionary/construction volunteer in third world country to mostly housebound/sometimes bedbound after dengue fever. 18 yrs & counting….
I have under active and over active immunity. Problems with t cells. Nk cells below 10 percent and functioning below 10 percent. Heart dysfunction lost my abilty to do aerobic sports at 20 years old. Have had disease since child now 53. The disease got worse. Have white matter in brain. Adhd ect. Got kidney cancer couple of years ago. Have to go biopsy for thryroid no life for over 15 years. No worry’s you lose something you can something. I lost all fear and have had major spiritual awakening. I’m frustrated but blessed to. p
This is not necessarily a new discovery — maybe for the Western scientists, though. If this is the same LEM, it can be found in various fungi/mushrooma in the East, where it has been well documented and used for possibly thousands of years alone or in various healing and /or rejuvenation formulas. Just one quick search turned up an article by well-respected Western herbal researcher and practitioner Dr. Christopher Hobbs, Ph.D., L.Ac, A.H.G. His article cites all Asian source researchers: Izuki, 1986; Mizoguchi, 1987b; Lin, 1987; Acki, 1984a. This stuff will not make trillions for Western Pharma unless they mess with it and create a patent from that. So the person who wants to try it can get it now through some highly qualified, licensed acupuncturist/herbalists in the West, if the practitioner thinks it is a good fit for whatever his system is deemed deficient in. Asian medical journals will of course have much more to report than can be found on Google; they seem to have their own system for research, and the ancient formulas are sometimes carefully guarded among clannish practitioners who want to keep the best stuff “in the family.” Hope others who have used LEM (under the PinYin names) will report their findings.
Becca, I noticed that the LEM referred to the article is “Lymphocyte Expansion Molecule”, Whereas the mushroom derived LEM is “Lentinula Edodes Mycelium”. I don’t understand how, from this article that we can assume that they are the same thing.
Great reporting and thanks for the interpretation – otherwise, Chinese Calculus
I like your post , Jimmy. As so many have, I , too, have lost an array of things to this. disease. And it makes sense to me that along with Natural Killer cell dysfunction, et al …the body is stuck …just struggling in the chaotic biological climate that is ‘us’. I know it is depressing to face, but we may never find a single ‘upstream ‘ causative factor or silver bullet remedy for this. Look at AIDS. Yeah, there are cocktails, meds almost as bad as the disease. But where did all the good news about AIDS go? It simply stopped. I focus a lot now on my attitude about my suffering. And truly transcendence is mostly up hill work for me, especially when really sick. I have not given up on science completely. . But I do need a foothold, an idea of myself as more than this illness. I live pretty much in the moment . I have to…or…this disease wins it all.
True that!!!
Thanks Nina. For me I always stay positive and do what I can to get better. That said I have always been searching for God. As you continue things just fall into place. Then faith becomes real constantly growing and there is no doubt. To me it’s not a crutch but a reality. I feel very fortunate. The bigger picture is great.
I was thinking recently about this phenomenon of “not getting sick”: I, also, rarely get symptoms of colds or the flu. But I was thinking… what if I actually am infected with these viruses but don’t get symptoms… because my immune system is not fighting the viruses? The effect would be that I would not have symptoms of illness (which are caused by the immune system’s reactions to infection), while the virus would replicate at will and infect the people around me. I’ve not had my immune functions tested so I don’t know its status. I’m just thinking.
Hmmmm. What little bit I’ve read would indicate that what is known as LEM is actually derived at least in part from shiitake mushrooms. Hence I guess the encouragement from researchers in the past to take various mushroom supplements. Wonder if I can get my Internal Med MD who knows nothing of CFS/ME/SEID to do an NK panel or any of the other immune testing panels that indicate specifically elevated cytokine levels as well as the abnormal IL’s being noted. Problem being, there is nothing specific for a non-specialist MD to do with the results, normal or otherwise. This is why I continue to push for MD’s to be taught about my disease and for the curriculum to be finally added to medical universities. Only then can us one million possibly see a “sub”-specialist. Cudos to those of you who have the money and support systems to get to the handful currently available. I called Dr. Cheney’s office in Asheville, NC and an initial visit is between $6-8K, as in beaucoup bucks with no Medicare participation. Again a shame. Those of you who do get to the specialists, please share the details of your test results AND what the MD intends to do about them besides say “Hmmm”. Then I can get an indication if that amount of money spent in a day or two has any real merit. marcie
6-8 K! He just apparently raised his prices….
Don’t waste your money on Cheney. I have a been a patient from years ago and then a couple of years ago.
Nothing but an Echo and only blood tests if you beg for them. His behavior was Bazaar
to say the least and he spoke mostly of himself and his research from the 90″s.
His fees have upped as I don’t feel he is going to be practicing alot longer.
I saw him in Charlotte years ago and he is not the same person.
I don’t know anyone that is better from seeing him. However we don’t have many Dr that specialize in our Malady in the SE. Most of his patients are people who have never gotten better and I think afraid to change Dr.
No one where I live will even accept any of his tests or finding.
Carole
Forgot to say- Lapp would be a much better choice than Cheney.
Carole
Thank you for your insights.
Guys, same acronym but beyond that very different. meaning. Interesting coincidence though.
My NK cell activity got tested when I lived in Japan in 1996. It was 6%. But might be very different today.
After reading the study my observation as well re ‘LEM’. Is this actually related to the mushroom molecule or an entirely different substance?
I know ME patiënts who did have low NK cel activity/function. When there NK cel function were normal again they didn’t feel better.
After reading the study my observation as well re ‘LEM’. Is this actually related to the mushroom molecule or an entirely different substance?
After reading the study my observation as well re Matthias’ ‘LEM’ acronym.
Is there a way to determine if actually related to the mushroom molecule or is an entirely different substance?
I would love to see links to specific data backing up the whole mushroom thing…
Hi Cort: Is there a way to post your articles to Facebook? I wondered if you could put a link somewhere in them so we can post them to FB? I really appreciate all of the excellent articles and updates you send out. I know it must take ALOT of energy to keep us so informed.
Tammi Rhoney
Thanks Tammi :)There is but the formatting sometimes make the buttons disappear. We have a new website coming – it will be much easier.
Cort,
PLEASE follow-up on this! Do you know where I can get in on clinical human trials???
What about IP6 ? It has a good rating on Amazon. Have you ever written on this?
I’m afraid they have 3 years of animal trials and then come human trials but in cancer first. It’s going to be awhile. Never written on IP6 – first I’ve heard of it.
Of course – everything takes a long time.
IP6 is an immune booster.
I have a concern because sometimes cfs/ fibro can lead to cancer. But we have a lot in our arsenal already to choose from – I just wish they took human trials sooner.