



The first intimations that chronic fatigue syndrome might be associated with gynecological issues came early in the history of the disorder. In 1988 Dr. Komaroff co-authored a paper finding increased gynecological complications (endometriosis, ovarian cysts, polycystic ovaries, uterine fibroids, menstrual abnormalities and galactorrhea), in 149 women with ME/CFS. Similar findings (early menopause, hysterectomy) have been reported in fibromyalgia as well.

The gender imbalance has always suggested somethings up with the female hormones in ME/CFS. Three studies do as well.
The gender imbalance, the two-peak incidence pattern in ME/CFS occurring during times of hormonal fluctuations, the significant symptom reductions some women experience during pregnancy and the high rates of gynecological disorders found other functional syndromes all suggest female hormones must be involved in some way in both ME/CFS and FM.
That stimulating finding, however, went without followup for 23 years until in 2011 a CDC study found increased rates of endometriosis ovarian cysts, irregular periods, gynecologic surgical operations, and pelvic pain in women with ME/CFS.
The CDC jumped on their results. There would be no 20 year wait for another gynecological study. Three years later they had another study out.
In the 2014 study 84 women diagnosed with chronic fatigue syndrome and 73 healthy controls took a gynecological history survey of 12 conditions (age at menarche, duration of menstrual cycle, excessive menstrual bleeding, bleeding between periods, missing periods, endometriosis, lower abdominal pain unrelated to menstrual periods, currently menopausal, age at menopause, gynecological surgical operations, hysterectomy, oophorectomy). The women came from a population sampling effort in Georgia using the empirical definition.
Remarkably, every one of the 12 gynecological conditions assessed was significantly increased in the ME/CFS group. Abdominal pain unrelated to menstruation, currently menopausal, excessive menstrual bleeding and age at menopause, were the most highly significant findings (p < .007), with a history of hysterectomy, endometriosis, gynecological surgeries and bleeding between periods coming in “second” with high significance factors (p <.004).
These were not small differences. Women with ME/CFS were four times more likely to have had a hysterectomy than women without ME/CFS. They also tended to have hysterectomies and/or oophorectomies (removal of the ovaries) at an earlier age plus the average age of menopause in ME/CFS was a full 10 years earlier than that of the healthy controls.
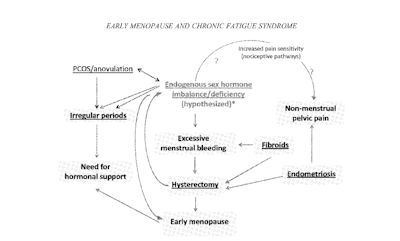
A covariate model employing BMI, hysterectomy and age at menopause suggested that early age at menopause – possibly signifying reduced hormonal production – was a particularly significant factor. In fact over sixty percent of the early menopause found in the ME/CFS women, was associated with hysterectomy; i.e. the hysterectomy appears to have triggered early menopause. Hysterectomy often, through later ovarian failure, reduces sex hormone production.
The three gynecological history results suggest to the CDC that reduced levels of female hormones (estrogen/progesterone) may play a role in ME/CFS. Early menopause, hysterectomy, menstrual bleeding and disturbed menstrual cycles are all associated with sex hormone depletion. Given that it was not surprising to see that the women with ME/CFS were significantly more likely to have been prescribed hormones than healthy controls.
The possible effects of reduced sex hormone production are manifold. Estrogen and progesterone are neuroprotective agents that effect sleep, cognition, inflammation, bone, muscle and joint health and pain sensitivity.
The Chicken Or The Egg?
Does chronic fatigue syndrome lead to hysterectomy and other problems or the opposite? Which is begetting which? It’s impossible to infer cause in these kinds of studies, but when both hysterectomy and ME/CFS and/or fibromyalgia were present, hysterectomy (ME/CFS (73%) / fibromyalgia (91%)) usually came first.
There’s no telling how important hysterectomy is to the development of ME/CFS or FM. It is, of course, a surgical procedure – a traumatic event – that also happens to affect sex hormone production. It’s possible that hysterectomy and the sex hormone depletion it causes presents a kind of one-two punch that sets some women up for a major system reset at some point.
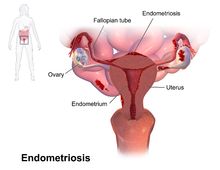
Immune sufficiency or autoimmunity may play a role in most common reason for hysterectomy – endometriosis.
The question is why early hysterectomies – the removal of the uterus and sometimes other organs – were so common in this group. Hysterectomy is not an uncommon procedure later in life – one in three women will ultimately undergo a hysterectomy at some point – but not so common earlier in life. It turns out that woman have hysterectomies for a variety of reasons – many of which involve pain relief. The most common reasons for hysterectomies are endometriosis followed by chronic pelvic pain, uterine fibroids, cancer and others.
The putative causes of endometriosis and chronic pelvic pain hover around those considered for ME/CFS. The roles autoimmune disease, allergic reactions, and toxins are being examined in endometriosis. The roles stress-driven HPA axis dysfunction, neurogenic inflammation, and myofascial pain syndrome are being examined in chronic pelvic pain syndrome.
Pain Sensitization
Since increased pain sensitization appears to be a factor in all these disorders, it may be notable that increased pain is one possible outcome of female hormone dysregulation. High rates of pain associated with endometriosis and CPS could be driving higher rates of hysterectomies in these women. The high rates of abdominal pain that is not associated with menstruation found in the CDC’s CFS group smacks of the increased pain sensitivity occurring in three other disorders comorbid with ME/CFS – vulvodynia, irritable bowel syndrome and interstitial cystitis.
Hysterectomies appear to set up women with fibromyalgia, for increased pain sensitivity. Pain sensitivity, stiffness and fatigue were substantially increased in a large study (n=813; 327 with hysterectomies) of women with FM and a history of hysterectomy. The authors noted that the increased pain following a procedure designed to reduce pain suggested that misdiagnosis may be driving many women with FM to get unneeded and ultimately harmful hysterectomies. Their pelvic pain was due to fibromyalgia – not to structural problems. (In fact, studies finding increased rates of surgical procedures in FM relative to other rheumatological disorders, suggests that all too often FM pain is misdiagnosed as some sort of structural problem that surgery can fix – but which it ultimately makes worse.)
The estrogen – pain sensitization may be a critical one. It was recently assessed in irritable bowel syndrome, another female dominated disorder (2x’s number of females/males). Estrogen receptors regulate both the transmission of pain signals from the body to the spinal cord and the filtering of pain signals at the dorsal horn of the spinal cord. In both cases they do this by modulating the activity of the ion channels, covered in a recent blog. Depending on the type of estrogen receptor in play, estrogen can either upregulate or down regulate pain sensitivity. In general, though, the ovarian hormones appear to have pain reduction properties.
Estrogen also appears to reduce sympathetic nervous system activity. Rice reported reduced estrogen levels may be tied to the increased levels of sensory nerve fibers he’s found in fibromyalgia patients hands.
Estrogen is in the mix. Some of the findings are tantalizing but there’s no clarity as yet to what role it’s playing.
Natural Killer Cell Connection?
Natural killer cells serve dual purposes in the placenta: in their latent state they support placental growth, but if their cytotoxic properties are turned on, they can inhibit it as well. It’s intriguing, given the number of gynecological abnormalities CDC studies have found in women with ME/CFS, that natural killer cells are the most abundant immune cell during embryo implantation and early placental development. Could reduced NK cell functioning somehow be a factor in the gynecological problems in ME/CFS/FM?
Treatment
The treatment implications of these findings are obscure, at least to me. Anecdotal reports of ME/CFS patients responding to hormone replacement therapy do occur but they are hardly a mainstream therapy. Personally, I know of one person who responded very well to progesterone (and poorly to estrogen.) She gloamed onto the progesterone possibility by trawling the forums of other disease groups. Stories of the opposite reaction to female hormones can be found as well.
Dr. Klimas is reported to support low dose estrogen in women going through menopause who do not demonstrate increased cancer risk. Why? Because she’s found that menopause can greatly exacerbate ME/CFS symptoms and therein lies the rub. Several factors suggest female and perhaps male hormones are involved in ME/CFS and probably FM, but exactly what role these complex factors play and how to manipulate them successfully, is another question entirely.
At the least, this study should alert physicians that some ME/CFS and FM patient’s flares may be due not to these disorders, per se, but to the entrance of early menopause – something they can do something about. At the most it will spur more research into the role sex hormones play in the genesis and perpetuation of ME/CFS and FM.
“CFS can take a tremendous toll on women’s lives at midlife and on our society and health care system. Being aware of the association of CFS and earlier menopause can help providers assist women in sorting out symptoms of CFS from symptoms of menopause,” Dr. Margery Gass
For now, hormonal treatments appear to be used as secondary factors to reduce symptoms, but who knows what the future may hold. If Broderick’s model is correct, hormone therapy in some form, may someday be part of a one – two- three punch protocol, designed to shift and ultimately tilt the system back to homeostasis.
Glaser restored T-cell cytotoxic activity and knocked down herpes simplex replication in stressed mice, using a beta blocker called nadolol and low dose mifeprestone, a natural killer enhancer used in abortions. The combination of a gynecologically active drug focused on natural killer cell functioning, and an autonomic nervous system affecting drug to fight off herpesvirus infection is, of course, intriguing. It may speak to the type of multi-systemic drug combination that ends up being effective in ME/CFS and FM.
Repurposing II: A Natural Killer Cell Enhancing Drug and Chronic Fatigue Syndrome
The women in this study were a) from a randomly sampled population and b) identified using the empirical definition. The findings, may not, therefore, reflect those of patients seen in ME/CFS clinics. (Komaroff did, however, find increased rates of gynecological problems in a non-population-based study.) Hopefully, we’ll know more about the gynecological connection to ME/CFS as the CDC’s Multisite and the Chronic Fatigue Initiative’s epidemiological studies start rolling out.
Inquiry of the Day – What kinds of gynecological disorders, if any, have you been diagnosed with? Let us know on the ME/CFS and FM Gynecological Disorders poll on the Health Rising Forums






I’m not surprised of this possible correlation.
I always suffer worse fibromyalgia pain during the week before and during menses.
My doctor, hoping to reduce flare ups, prescribed low dose birth control pills so that I wouldn’t have a period, however, that caused me to have menopausal symptoms, the worst of these being night sweats which was causing extreme sleep problems. The sleep problems became much more bothersome than the fibro flares so I went off it.
I also have an issue with poly cystic ovary disorder.
Will be interesting to continue to watch what, if anything, this research brings to light.
Sadly, I’m not surprised with this news. I always wondered how much my hysterectomy played into my CFS development. Endometriosis is a painful disease.
Unfortunately, in my small town, endo sites are ‘burned’ off and since it had spread throughout my pelvis, my bladder was burned. I finally resorted to a total hysterectomy. Endo growths were found on my bladder, appendix (removed), both fallopian tubes, one ovary, uterus and the cul de sac. Painful adhesions formed (scar tissue) which brings its own kind of pain. Less than 2 yrs later I was in a brutal car accident from which I still need physiotherapy. But, I still have hope things will improve re: CFS and that I’ll be ‘better soon’
Cort: how can I do the poll?
I sent an addition to my first message (Rita Macoritto) but I’d rather you use the name ‘better soon’ ! Thanks
I had a partial hysterectomy at 28 for endometriosis and I never had regular periods and my 2 children that were full term were both induced at a month overdue. I have been a fan of hrt for about 14 years as it seems to really treat the fibromyalgia symptoms. Every time I do not do hormones for awhile I have a bad flare that lasts months. I am now 60 and have hasimoto thyroid and have went without hrt for part of the year and am having a bad flare.
Also, Dr. Klimas offers Low Dose Estrogen. I tried that but unfortunately it caused the endometriosis to re-activate and took 6 months to disappear after stopping the hormone replacement. It seems you can never be sure if all endo cells are eradicated (laser treatment) and since estrogen feeds those cells, hormone replacement in the case of endometriosis is quite controversial.. So, although I’m very deficient in estrogen, I DO NOT want endometriosis back. CFS is hard enough
We’re such a complicated group! I guess humans are just complicated and when you throw a wrench in the system – it just gets more complicated (lol)
I have endometriosis following ruptured ovarian cysts (endometriomas) and was on continuous oral contraceptives for years to suppress my menstrual cycle to prevent more cysts. I gradually developed ME/CFS during this time. I definitely see a connection in the severity of my symptoms with my level of sex hormones.
After discussing this study with my husband, a doctor- he brought up the idea that if ME/CFS does indeed have lowered NK cells or lowered NK cell activity, that could play a role in the development of gynecological disorders because NK cells are thought to play a significant role in regulating the reproductive system.
I believe there are studies linking defects in NK cell functioning to the development of endometriosis.
I’m sure this ties back into the sex hormones as well, but that function is less clear.
Its also worth a mention that Dr. Chia has a study finding enterovirus in ovarian tissue of women with gynecological problems and ME/CFS. But that bears more study to determine significance.
I had completely forgotten all about NK cells/gynecological intersection. Check this out from a blog on mifeprestone which induces abortions by enhancing NK cell problems.
http://www.cortjohnson.org/blog/2014/06/29/repurposing-ii-natural-killer-cell-drug-chronic-fatigue-syndrome/
Would it be relevant to give men with CFS testosterone injections and note any changes?
Gordon Broderick’s models suggest that testosterone is protective in men. Iv’e heard that some practitioners do use testerone effectively in some patient. I believe they use creams but I’m no expert.
I suffered from “female” problems since the onset of menses at age 9. On my maternal side every female except my mother had a hysterectomy by age 39, 39 being me. I was a hold out. I had Cervical Cancer at 33, but didn’t want a hysterectomy then, even though my menses were more painful then giving birth and I had to wear preemie diapers to contain flow. I don’t want to describe flow because it was too disgusting and gory for 7 long days. I got pre-cancer at 39, along with endometriosis, ovarian cysts, and fibroids. But my “female” problems which later were diagnosed as PCOS was before Fibromyalgia.
In fact other than my PCOS, I was never sick, other than a strept infection at 12. Then at 32, 1990, I got Fifths disease, Human Parvo Virus 16, next I got an aggressive strain of HPV cancer a few months later, only took 4 months to go from abnormal to cancer, after monogamy for 11 years, 10 rounds of chemo. Then 5 months later I felt sicker than I ever felt before.3 years later they called it Fibromyalgia and said it was non-progressive. But every year a new symptom, spiraling and spiraling, till I was getting symptoms faster than researchers could discover they were Fibromyalgia symptoms. Non-progressive.
I had right ovary removed at age 17 and partial left ovary removal at age 18. Right ovary and fallopian tube wrapped around the ovary and destroyed it and caused intense pain. Partial left ovary removal due to having pain. Only ovary killed by scar tissue at age 25 and was in some degree of menopause as a result. Had hysterectomy and uterine fibroid removal at age 51.
The poll results are in line with the findings in the study thus far.
http://cortjohnson.org/forums/threads/the-fm-and-me-cfs-gynecological-history-poll.2427/
Hysterectomy – 15 vote(s) 34.9%
Oophorectomy (removal of ovaries) – 8 vote(s) 18.6%
Endometriosis – 18 vote(s) 39.9%
Excessive Bleeding – 24 vote(s) 55.8%
Abdominal pain not related to menstruation – 21 vote(s) 48.8%
Irregular Periods -15 vote(s) 34.9%
Other- 26 vote(s) 60.5%
None of the above – 4 vote(s) 9.3%
It would be really interesting to find out for how many people a hysterectomy helped reduce their symptoms (???)
I have had ALL the gyno problems including a rare ovarian tumor and endometriosis. All which resulted in removal of the uterus and both ovaries by age 37…all 3 in 3 separate surgeries over the course of 13 years. I have had CFS/Fibro before these surgeries and problems and I still have CFS/Fibro after…25 years after the last ovary was removed. I have been on HRT consisting of Estrogen and Testosterone since…I still suffer from CFS/Fibro…no difference…The only time I was completely CFS/Fibro symptom free was the 8 months I was on LUPRON for the Endometriosis. LUPRON is a GNRH agonist.
My uterus ruptured at the end of my pregnancy.
My problems started after the birth of our daughter. My GYN said hormonal change, D and C and then all the infections started, every itis yeast and all of them. A hysterectomy at 35, fibroid tumors were found and scar tissue from all the infections. I was fine then for quite a few years. I had a year of unrelenting stress, sick parents in another state, daughter’s wedding, knee scoped and PT so I could walk down the isle. I in typical A personality style decided to paint the whole house and hurt my knee. My husband’s mother died and then I had the flu shot. I got the flu and it is not completely over yet. I can live a normal life now with pacing and some times acting, thanks to Dr. Klimas and Dr.Rey. I go for my yearly check up in June, I have sent several vials of blood so we can see how I am doing on paper.
I just read Suzanne Somers latest book :”Tox-Sick”. She interviews the very best doctors. I know we are all very toxic and I have cleaned up a lot of things. We have some very good local farms here and do a plant based diet. We now have Earth Fare and Whole Foods is being built. All of that has helped a lot. I still do Rich Vanks protocol for the methylation pathway. I highly recommend the book, one of the best I have read and I have read a lot. I could not put it down.
I was plagued by gynae problems from an early age. Typically, I was told that ‘all women’ have pains and I was making a fuss. After five years of increasingly agonising periods I finally paid to see a gynae surgeon privately. He carried out a laparoscopy and found, at just 21 years old, that I had prolapsed womb, prolapsed ovaries and endometriosis ‘everywhere’. Over the next ten years I was continually in and out of hospital for various gynae ops including suspensions, ovarian cysts, ectopic pregnancies (2), miscarriages, oopherectomy and finally at 31, my 13th gynae op – a total hysterectomy. At 35 I had breast cancer and then diagnosed with ME a few years later. My thyroid was found to be under active and have also been diagnosed with lupus, sjorgrens and UCTD – all I gather are considered autoimmune. Will be very interested in any further research into the gynae aspects/links with ME.
Wow….you are so in the hormonal subset…..the gynecological aspect of ME/CFS obviously needs MUCH more attention..
I started having painful periods at 15, and was diagnosed with endo at 29 (all in your mind, the doctor said…) Extremely painful periods, and as the years went by, significant fatigue. Many, many endo patients complain about fatigue. I went through several hormonal treatments and surgeries, but the endo returned, again and again.
I got ME after a flu when I was 39. Some of the surgeries were after I became ill with ME.
Menopause has been hard, with hot flashes, and I tried hrt, but there is a challenge… estrogen makes the endo lesions grow. Women with endo should, generally, not use hrt. Most women with endo experience a relief in symptoms at menopause. So I got the hot flashes, but less pain.
Hrt may have caused a slight improvment in ME fatigue, but I had to stop hrt because of a return in symptoms caused by adhesions and lesions on bowel and bladder.
Rather fatigue than pain…
What surprises me is that the author appears surprised to find that gynaecological problems are increased. It is my belief that almost everyone “diagnosed” with ME/CFS has a Multi Endocrine disorder. Most commonly caused by either Lyme Disease or Hypopituitarism (possibly as the result of a head injury).
Both of these conditions affect the whole endocrine system. So sufferers will have secondary hypothyroidism, hypoadrenalism, sex hormone imbalance and many other associated hormonal imbalances and vitamin/mineral deficiencies.
Secondary hypothyroidism, although acknowledged by the medical profession, is rarely diagnosed as the patient’s TSH rarely rises. Their glaring endocrine symptoms are ignored.
Is it a coincidence that “fibromyalgia” (a symptom not a condition), ME, CFS, hypothyroidism, hypoadrenalism all have the same symptoms? Of course it isn’t.
The only coincidence is that the medical profession as decided that ME, CFS, Fibromyalgia are mysterious undiagnosable, untreatable conditions. They are quite prepared to diagnose you with either one with no evidence at all. Yet will dismiss the treatable endocrine conditions on the basis of incomplete testing and ignore all symptoms. Why? Because it’s cheap (no tests) and because the drug companies prefer it that way – sufferers are then treated with a cocktail of other drugs to control their symptoms.
Estrogen inactivates microglia:
http://www.pnas.org/content/110/9/3543.full.pdf
Life with ME/CFS becomes pretty unbearable the week before and during menses. I have regular episodes of unexplained pelvic pain during the other weeks. Have been diagnosed with uterine fibroids and partially blocked fallopian tubes. Had a total of 5 miscarriages which were suspected to be the result of natural killer cell overactivity. I’m convinced that at age 43 I am close to going into early menaupose. Above all, my body and my gut feeling tell me it is my sex hormones that wreak havoc with my health as hormonal fluctuations invetably lead to severe ME crashes. Haven’t tried any medications for it though; sometimes medicines can cause more problems than they solve. Hysterectomy is not an appealing option and would not even contemplate one. So there we are…
Indeed, there we are..Good luck finding a way through this…
I had, and still do have at the age of 60, galactorrhea, which is a condition that one or both breasts produces milk, or a milky discharge. This disorder has been with me since the birth of my daughter, when I was in my twenties. However, having galactorrhea has helped me in my quest to find answers regarding my ME/CFS. I delved into research to find out what caused galactorrhea and discovered that this condition is often the result of too much prolactin. Prolactin is the hormone responsible for milk production. It is also an immune system stimulating peptide hormone. The secretion of pituitary prolactin is under the inhibitory control of the hypothalamus, and the most important inhibiting factor is dopamine. Dopamine agonists (helpers) such as bromocriptine and cabergoline are often used to treat galactorrhea. Progesterone is linked to the neurotransmitter dopamine. Chasteberry or (Vitex agnus-castus) also appears to inhibit prolactin secretion by raising dopamine levels.
Since, I believe my case of ME/CFS is caused by an over-stimulated immune system (autoimmunity) and since prolactin is involved in causing an over-stimulated immune system, this led me to understand that dopamine was a major player in my illness ME/CFS. Raising dopamine levels with tyrosine and other agents has had a very positive effect of controlling many of my ME/CFS symptoms. Dopamine is the major neurotransmitter that puts the brakes on immunostimulating prolactin.
Rachael, do you have any side effects with the tyrosine such as tachycardia? I’m wondering if it would be contraindicated in those of us with POTS. Do you mind sharing which Me/CFS symptoms the tyrosine helps you with. Thanks
Tyrosine helps control my POTS. I used to have a resting heart rate of about 100 bpm (tachycardia) and blood pressure was always low about 95 over 60. Tyrosine lowers my heart rate to about 80 bpm and raises my blood pressure to about 140 over 80. I know that many may consider 140/80 to be high bp, but I feel so much better and that’s all that matters to me. Tyrosine not only helps me with POTS, but also eases symptoms of malaise and gives me more energy. It seems to dampen my hyper-immune response. I only take a very small amount of tyrosine every morning from an open capsule, along a small amount of MSM (methylsulfonylmethane) and a salmon oil capsule. t was trial and error until I found the amount of tyrosine that worked for me, but be careful if you are planning on using tyrosine because it the ability to raise blood pressure, quite substantially. If I feel over-stimulated at bedtime, I take sedating antihistamines to counteract this effect.
So sad that we who are too sick to be on any forums (or social media for that sake) are excluded from the polls. Health practitioners and researchers exclude the sickest amongst us, now also the online community. Sad.
I feel so badly you feel excluded. I have so many of the symptoms I feel I don’t know exactly where I fit. That I would overwhelm the poor researchers. Here at least I can feel we don’t get hokum. I don’t like to get in P!$$!Ng Contests that my Fibromyalgia, CFS, ME is worse than anyone else because it’s probably not. But here I am validated instead of made feel like a hypochondriac. I feel strong among the many who the same fight as me instead of weak among those who look right through me. I can state a symptom and hear others echo it, instead of meeting disbelief. I believe there are very good intentioned, talented, people willing to work with syndromes which seem to offer no glory for the wunderkinds who crave a quick fix and quickly is frustrated and tired of us. So I have just all kinds of great things to contribute as I lay about on my giant 6 foot bean bag. If there’s never a cure, never relief of body, here my frustrated Fibromyalgia spirit found an Oasis. I am sure there are many sub categories you may fit into, after all, with “us” is there any just two alike?
I’m sorry about that. Building up the Forums is a big emphasis right now. They’re important for the blog and for Health Rising. There’s no better way that I can think to assist the blog than to have a good strong Forums going along with it so for now I’m going to continue to post polls on them frequently. Over time, though, we’ll have more polls on the blogs.
If you go straight to the link for the poll rather than wading through the Forums to find it that might work. It’s rather like reading a blog to me but your experience might be different.
Thanks for posting this, Cort. Interesting to read the commends and consider the earlier studies.
What’s frustrating about this particular study is that it used the Empirical (Reeves 2005) definition, which was discredited in a 2008 article by Jason and does not appear to have been used outside of CDC. Given the problems with the Empirical definition, it is difficult to know what population of patients was actually examined in this study and to evaluate the relevance of the findings to patients that meet the CCC or ME-ICC.
Its important to study this symptom cluster. But its unfathomable to me why articles using the Empirical/2005 Reeves criteria are still being published seven years after they were discredited.
Cort,
I haven’t had ANY.
I’ve been sick for 25 years. I had our third child AFTER being diagnosed – she is fine.
I had NO trouble beyond very minor hot flashes that didn’t last long with menopause.
I DID have a doctor tell me, when I was feeling a bit better while expecting daughter, that ALL his CFS patients went psychotic after delivery.
I changed doctors. What an idiot!
He was a ‘specialist’ – possibly he only got referrals when other doctors were already worried. But I still fume when I think of it.
Other than that iatrogenic bit, I have had NO problems.
I wonder about these papers – self-selected by those who have problems?
Alicia
Chronic candida infections, recurrent cystitis, fertility problems, early menopause and lately lichen sclerosus have been my gynecological issues.
My menopause ended when I was 54 that is when the FM started or at least became a problem it had been there all the way through. I had just put it down to menopause. Yes I had the irregular bleeding so bad prior, I had to go and get my womb lining burned off. Was this the start of the problem inquiring minds would like to know. Not for any other reason than to be able to say that started it. I would so love to know what did. I also have Lupus but it has been well controlled. I was diagnosed when I was 27.
Uterine rupture can happen with Ehlers-Danlos Syndrome (EDS) too. Many people with ME/CFS/FM comorbidly have EDS, which affects collagen/connective tissue. . I have the hypermobile type of EDS (there are at least 5 different types of EDS.) I, too, also have ME/CFS & fibromyalgia.
Developed fibroids in early 40s, (also Hashimoto’s Thyroiditis a the same time.) Sleep problems 47-49 but thought was due to peri-menopause. February 2009 at 49 1/2 went menopausal and that very month the ME/CFS symptoms came on and decimated my health.
Also, I have 2 children, 12 years apart, with my second I was unable to conceive so I went thru 3 rounds of IVF, got pregnant at 36 with my second child. I do test positive for HPV, (probably contracted from my first husband.)
Had a hysterectomy in 2012, afterward a pap smear came up with hi-grade precancerous cells in the vaginal cuff, attributed to the HPV not doubt. Had this treated with laser surgery and am monitored closely.
forgot to mentioned, bc was unable to conceive went through a tuboplasty (due to scarred fallopian tubes) which was major surgery in 1988, my doctor saying classic damage probably from Chlamydia, thanks to my ex.
My goodness, reading this article was almost like reading my medical history! Thank goodness the CDC is looking at these issues again.
I just want to put this out there. There is a drug called Visanne. This may help many.
It is an option. I finally found a gyno that wrote down a list of helpful options. This is one. I still have to be assertive to make sure that I am not doing something that will set me back all the years that I already did trial and error with. Some women don’t like the side-effects, but many including myself are able to bear them. The worse for me is dry mouth and tiredness. I take it before bed. It helps me to sleep, which is good. I keep drinking throughout the day, and that helps too. My main target is pelvic pain and more. It also helps my pelvic pain, and reduces the menstrual amount that occurs during my periods. Before, I only had one free week per month of no pain. The other three weeks was hell. I could write a novel about my experience. However, to make a long story short, consider it another way if nothing else works. It helps manage the pain. I am not out of the woods but I can live more than I did. Finally, after 10 years plus, I can somewhat manage my life better. I pray good things for you all. xo