

“The results blew me away. I have never seen an effect as powerful as this.” Dr. Benjamin Natelson
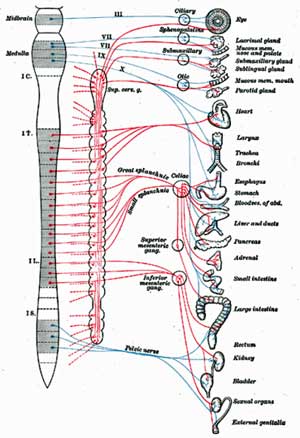
The ‘vagus nerve’ is actually a bundle of different sized nerves. Aptly called the “wanderer”, the tenth and longest cranial nerve enters the brain at the medulla and extends down into the chest cavity and into the abdomen. Eighty percent of the nerve is devoted to relaying information from the body to the brain.
The autonomic nervous system’s Yin to the sympathetic nervous system’s Yang, the vagus nerve regulates the parasympathetic nervous system. It affects everything from the swallowing to digestion to speaking to blood pressure.
Reduced heart rate variability (HRV) findings suggest an underactive vagus nerve may not be keeping the sympathetic nervous system (fight/flight system) under control in chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM). Reduced HRV has been associated with increased pain, cognitive problems and poor sleep in FM and/or ME/CFS. Estrogen, interestingly, appears to accomplish it’s anti-pain functions via the vagus nerve.
Stimulating Health?
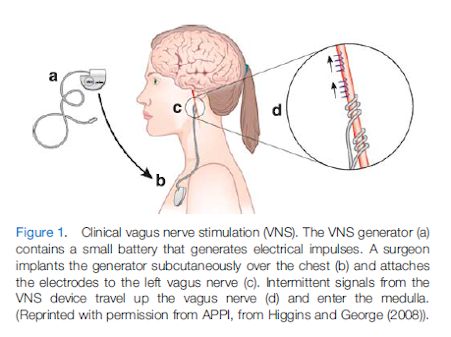
Could stimulating the vagus nerve turn down the flight/fight response in fibromyalgia and reduce pain, improve cognition and sleep? Perhaps. Right now VNS usually requires a surgical procedure to implant an electrode in the neck that’s connected to a battery near the collarbone. That’s no small order, but then again treatment resistant fibromyalgia is no laughing matter either.
Most brain stimulation techniques (ECT, rTMS, tDCS) stimulate the brain from the top down but vagus nerve stimulation (VNS) stimulates it from the bottom up. VNS stimulates the cranial nerves in the brain stem that connect directly to the limbic cortex and the monaminergic nuclei. These regions of the brain regulate mood, emotion and autonomic nervous system functioning among others.
VNS upregulates the activity of serotoninergic and noradrenergic neurons in the brain, which generate neurotransmitters (serotonin and noradrenaline). When stimulated in this manner these neurotransmitters are believed to turn on pain inhibiting pathways in the brain.
The results of his small phase I/II vagus nerve stimulation trial in FM were positive. We didn’t know how positive though, until recently, when Dr. Natelson talked about the study in a two-part radio interview with Dr. Paul Christo.
The Patient
First Dr. Christo introduced a woman, Jean Hasse, with a severe case of fibromyalgia and ME/CFS who’d been in the study. A former high school science teacher, Hasse’s journey with FM/ME/CFS began when she experienced knee pain during pregnancy. The pain spread to her ankles, then to her hips, then into her smaller joints and finally everywhere including her skin. She couldn’t move or experience touch without pain, had severe brain-fog, and was diagnosed with irritable bowel syndrome. She ended up leaving her job and was bed bound most of the time.
Cymbalta didn’t help. Lyrica did but also caused her to gain a lot of weight. Relaxation techniques including tai-chi helped keep her calmer but didn’t substantially reduce her pain. Tramadol helped but she was up to 16 tramadol a day prior to the VNS.
Jean described a fairly touchy surgery done by a neurosurgeon in 2008. The stimulator was turned on about a week after the surgery. Every time it went on (every ten minutes) her neck muscles tightened and she coughed. It took her about six weeks to adjust to the stimulator and the side effects have almost all disappeared.
Her brain fog started disappearing first. Her short term memory problems disappeared. Next the severe radiating joint and nerve pain began to disappear. It happened gradually; by a year later she felt she had been “reborn”.
She still has pain; she’s still taking Lyrica and tramadol but before the surgery she was taking 350mgs. of Lyrica – now she’s on 75. She was 16 tramadol a day and now she’s taking two. She was able to go back to school and get a master’s degree and is now working. She’s also hiking and exercising.
She said for those in pain – not to give up hope.
The Study
Pain Med. 2011 Sep;12(9):1406-13. doi: 10.1111/j.1526-4637.2011.01203.x. Epub 2011 Aug 3. Safety and efficacy of vagus nerve stimulation in fibromyalgia: a phase I/II proof of concept trial. Lange G1, Janal MN, Maniker A, Fitzgibbons J, Fobler M, Cook D, Natelson BH.
Dr. Natelson is no spring chicken. He’s been treating FM and ME/CFS for a long time. He said “The results blew me away. I have never seen an effect as powerful as this.”
By the end of the trial five of the eleven fibromyalgia patients no longer met the criteria for FM. The biggest improvement occurred during the first three months, but improvement, interestingly and encouragingly, tended to increase over time.
The trial was not placebo controlled or randomized but Natelson argued, it was unlikely the improvement were due to a placebo effect for three reasons: patients tended to continue to improve over time, more patients tended to respond over time and placebo effects rarely last a year.
Natelson said about half of the patients in the person trial had similar, life-changing results to Jean’s.
The Catch
The catch is the cost. Vagus nervous stimulation is approved for epilepsy but not for pain. Even though it’s approved for depression insurance companies won’t pay for it. It would probably cost you a cool 30-40K to get one implanted on your own.
Other options are being developed, though. Gammacore’s transcutaneous vagus nerve stimulator worn on the ear is being investigated in Europe. A UK trial is investigating its effectiveness in irritable bowel syndrome. An multicenter European trial for migraine will begin soon. It’s available in the U.S. only for research at the moment.
Nemos has produced an earphone stimulator approved in Europe for epilepsy. It’s conducting a trial in the U.S. for chronic pelvic pain syndrome.
TENS units can be used to stimulate the vagus nerve via the ear. Check out a description of how to prepare them in the Resource section of the Health Rising Forums.
Thus far, transcutaneous vagus nerve stimulators have been effective in tinnitus, in reducing sympathetic nervous system activity, in reducing depression, in improving cognition. It’s a growing field.
Wrapup
Vagus nerve stimulation was stunningly helpful for about half the FM patients in Dr. Natelson’s study. While the patient interviewed by Dr. Christo was not pain free, the VNS allowed her to move from being bedridden to return to work, and hike and exercise, and largely to lead a normal life. She said you’d have to hold me down and tear it out of me to have her give it up.
The fly in the ointment with VNS is availability and cost. The procedure is very expensive and is not covered by insurance. Despite the success of Natelson’s trial, clinicaltrials.gov does not list followup trials.
Cheaper alternatives in the form of transcutaneous vagal nerve stimulators for the ear have been developed and are being tested. Some are available in Europe and some studies are underway in the U.S. Transcutaneous VNS may be not be available for many at the moment but it’s a developing technology and if it’s as effective as the surgical procedure is, it will show up at some point. This is a treatment option to keep an eye on.
Stay tuned…
Contact Dr. Natelson for future studies here.
Health Rising Forums
Taken the pain poll on the Health Rising Forums yet? Tell us “Where it Hurts” here.







Thanks, Cort, had not seen that approach. I am not too big on any surgery but will now follow research on external stimulators.
I think it’s pretty new in Fibromyalgia. I don’t think anyone else has tried it.
Cort – an external Vagus nerve stimulating instrument is available from dr Nemechek, no surgery required.
In the meantime there are Vagus nerve imbalance trigger points that you can do for free (infraspinatus trigger points-3 of them-you’ll find them in a band of muscle on the back of the shoulder blade) I use a tennis ball against a wall, when you find the correct points your arm goes numb temporarily. I’m pretty sure an acupuncturist can find these trigger points as well. SI 11
The tennis ball sounds good. I didn’t enjoy my expensive and not helpful acupuncture treatment a while back so will pass on that.
As Cort said, the diving reflex of cold water on your face. …I’ve used an ice cube or ice water in a glass on my cheek after overeating to stimulate the vagus nerve in the stomach and feel less full…works.
It works I had this nerve stimulators implanted in my back for chronic back pain and for pain in my legs,hips, thighs, and butt. and it help a lot it’s not a cure for chronic back pain but it is a helpful pain tool which helped me at least 80% with the pain. and I stop taking a lot of pain medication I was on that made me tired and sick all the time, I also suffer from fibromyalgia, and have notice my symptoms from that are not as severe as they use to be sense I had the stimulators but in, my stimulator runs up my spinal cord. I am happy with my decision to have this procedure done, it has help me a lot, I can do things again I haven’t been able to do In years like walk to the corner, play with my grandchildren, cut the grass, walk through Wal-Mart ok maybe not all the way yet butt I’m getting better. Thanks for reading my story.
Thanks for sharing your experience Eva 🙂
Hi I have the same problems as you and I’m very interested in this can you please gi e me some info as to where I can find out how much it will cost and in which countries is it available please thanks janine
I am trying out my new parasym device which stimulates vagus via earclip electrode.
Seems to be doing something!
How great that someone is having such great success and recovery!
There is a great perspective on the vagus nerve by neuroscientist and psychophysiologist Stephen Porges, Ph.D. currently at Chapel Hill. He has worked with autism and has researched the origins of the vagus and come up with data showing that there are actually two branches of the vagal nerve.
Both branches of the vagus support ANS function in health. The more primitive branch, referred to as the dorsal vagal complex (DVC) because of where it originates in the brain, is what triggers the freeze state following traumatic events. It maximizes survival through stillness and decreasing oxygen consumption, allowing a fish or reptile or animal to wait until a threat passes or to “feign death.” In humans, it can become dominant following trauma and can cause prolonged states akin to hibernation (low blood pressure and heart rate, foggy brain, and more). I suspect this is an important player in ME/CFS and FM.
The more recent vagal branch is called the ventral vagal complex (VVC) and is found in mammals. It regulates the social nervous system (cranial nerves, ability to speak and make facial expressions to communicate or warn others off…) and it suppresses fight / flight in health.
I wonder if the vagal stimulation in this research is supporting greater VVC/social nervous system function and enabling a shift out of DVC/Freeze. It may also be suppressing the fight/flight response more successfully as well, as mentioned in your post.
Porges’ research is findable online (although I find his articles very difficult to read). There’s a great summary of his work on wikipedia.
http://en.wikipedia.org/wiki/Polyvagal_Theory
Thanks , Veronique. While I was texting, you answered some of my questions.
So glad it was helpful, Nina. And you raise some great questions re what the triggers might be. I think trauma plays an underestimated role in triggering the freeze response and we’re learning through the science that traumatic events – including very early in life – can shape the way the ANS develops, learns to regulate, and learns to perceive the environment (as threatening vs safe). We’re also learning that trauma has long-term effects not only on thoughts and emotions but also on the body, physiology and biochemistry (including high cortisol in many early on and low cortisol in the late phases). It’s one theory at any rate!
Thanks Veronique…I agree that it’s fascinating and I do wonder if it occurs to me in some ways..It makes sense in several ways. Marian Lemle has put forth a hypothesis that hydrogen sulfide is producing a similar state of “hibernation” in ME/CFS.
Tim Vaughn did a nice blog on the polyvagal theory –
http://www.cortjohnson.org/blog/2014/01/02/immobilized-mecfs-fm-polyvagal-theory-movement-restriction-autonomic-nervous-system/
Hi Cort,
What an articulate and thoughtful post by Tim Vaughn. I am part way through the comments, which raise so many relevant issues. I can’t believe how many topics you cover in your blog!
I find this very interesting as it helps support my theory that the animal brain is failing and that the reptilian brain is becoming dominant. A good reason for the higher centres to evolve. We talk about fight or flight but forget that freeze is the absolute default position. I wonder how long you can go on stimulating something that is dysfunctional without taking other factors into account. The use of coffee is a prime example.
I really enjoyed reading this summary of the vagus nerve having 2 branches and their pathophysiology. I will try a read of Dr. Porges research Very interesting topic.
Wonder why it doesn’t help the ‘other’ half. And a tangential question: Why can’t I take soo very many drugs/classes of drugs… including pregabalin , gabapentin, tramadol…SSRI’s, tricyclic’s…etc. etc. I have extreme, exaggerated reactions to meds that many others with this disease deem not only tolerable but wonder meds. One doc said I was ‘a slow acetylator’. I understand that, in general, this means ‘slow to metabolize’. I also understand that it is far more complex than that. I no longer wish to ‘get well’. I wish to simply stop suffering. When I was a teen I began to pass out…with no prodrome. Just stand up to go do something and …BAM…unconscious. The vasovagal part of this intrigues me. From the web: “The vasovagal syncope trigger causes a sudden drop in your heart rate and blood pressure. That leads to reduced blood flow to your brain, which results in a brief loss of consciousness.” But …what else does it do? Or rather, what causes it…and what is the trigger in CFIDS? And what IS CFIDS /SEID? Is it this disease a symptom of something else yet to be discovered , or is it a distinct clinical entity?
re slow acetylators
http://tmedweb.tulane.edu/pharmwiki/doku.php/fast_vs_slow_acetylators
I do understand how you feel. I have the same problem with many meds, they make me drastically worse. On the other hand some work but usually not for more than a couple of years. Even narcotics stopped working and I’ll never go back on them again. I’m down to 2 meds, cymbalta, but not higher than 30 mg or I get worse and cesamet. (I aslo take thyroid meds)
Any treatment I’ve ever had: physio, massage, acupuncture, Bowen therapy, cranial/sacral and on and on also make me much worse. It is extremely frustrating and a lot of trial and error (more error I must say!)
Our bodies are uniquely wired, beginning in-utero, part genetics then part life experience both physically and emotionally.
@Nina……..you may want to research MAST CELL ACTIVATION DISORDER. Also, read Dr Lawrenceville Afrin’s detailed research online through journal of hematology immunology
Cort, you say vagus nerve stimulation has been approved for depression. So why won’t insurances cover it?
I have CFS/ME, Fibro, POTS and treatment resistant major depression, and I wonder if I’d be a candidate. But I can’t afford it if insurance doesnt cover it!
Yes, it’s odd. I thought the two went hand in hand. Dr. Natelson said insurance would not cover it. I cannot remember why. My guess is that it was the combination of the expense and the fact that the efficacy wasn’t extremely high – even though the FDA approved it. It’s on Dr. Christo’s conversation though – in the second part.
there is an inexpensive way to try vagus nerve stimulation – buy a tens machine and ear clips like these https://www.niddvalley.co.uk/item.asp?iID=111 (uk) or these http://www.tenspros.com/Electro-Stim-Ear-Clips-for-Depression-Anxiety-Pain-and-More_p_196.html (us)
fiddly to attach and not going to work as well as the expensive version but perhaps a way to sift out those who would gain the most benefit. If you can develop an inexpensive way to show who would benefit maybe insurance will cover it?
I did actually buy these, must see if it help my tinnitus.
Have you begun trialing this yet? What effects are you seeing?
Has anyone tried the Rezzimax Tuner Pro tool for vagus nerve stimulation invented by Sherik Peck Utah. Sounds amazing. Would like to hear anybody success story with FM
You can stimulate the vagus nerve yourself by gargling, gagging and singing loudly. According to Dr. Datis Kharrazian practicing one or all of these on a regular basis can bring balance to the nervous system and improve function of the brain/gut axis. Check out this video on the subject https://www.youtube.com/watch?v=Am7kr-vP0Ys.
My personal experience is that like many other therapies or treatments, these technques become less effective over time.
Interesting…Thanks
Here are some others from a website – http://eiriu-eolas.org/2013/06/29/its-very-easy-to-deal-with-your-anxiety-using-your-vagus-nerve/
It’s interesting that diaphragmatic breathing is the first technique Staci Stevens teaches to her patients using her heart rate based exercise protocol.
Check out a 7 – 11 diaphragmatic breathing technique.
(1) Inhale diaphragmatically through your nose, with your glottis partially closed, like almost making a “Hhhhh” sound for a count of 7
(2) Hold your breath for a moment
(3) Exhale through your nose (or you mouth), with your glottis partially closed, like almost making a “Hhhhh” sound for a count of 11
This is one breath cycle; go for 6 – 12 cycles and observe the results.
(This is similar to Andrew Weil’s technique- The key is longer exhalation than inhalation. Check out a video in our media section here.
Practice, Practice, Practice
The more you practice the more effective this technique will be.
Eventually, when your newly acquired breathing skill is established and abdominal breathing becomes a habit, you’ll find your body constantly operating at a much lower stress level.
You will also notice (or sometimes you will not even notice it) how your breath responses to stressful situations; your body will be conditioned to automatically control your breath and by this, your stress and anxiety.
I found the article very interesting and I have most of the symptoms mentioned. I am 73 yrs old and chronic fatigue and fibromyalgia have stolen my life.I have had this disease for 40 yrs. I am 95% homebound because I pay horrific price for a little enjoyment. I would consider almost anything to enjoy what time I have to enjoy the rest of my life’s
Hi , Kathleen. I can relate. I, too, would consider almost anything. For me, access/cost is hurdle, one I cannot seem to cross.
Cort, have you seen this article about stimulating the vagus nerve in arthritis? http://www.nytimes.com/2014/05/25/magazine/can-the-nervous-system-be-hacked.html?_r=0
What a great article…I missed that one – thanks very much 🙂
You’re welcome
I do this by attaching a TENs machine to my ears. 15 mins, 3 times a day. Not a cure, but it makes a significant difference (I have ME not FM).
This is the one I bought:
http://www.bodyclock.co.uk/acatalog/First_Choice_Plus.html
And these are the ear clips:
http://www.bodyclock.co.uk/acatalog/auricular_clips.html
This site has US, German and French sites as well (see flags in the top right of the site’s page).
I attach one electrode to the tragus and one to the ear lobe.
Settings are: Pulse Rate = 30, Pulse Width = 200. I turn it up until I feel a pleasant tingling sensation.
This worked out quite cheap as it was an initial outlay of £50 with no follow up costs (except replacing the battery).
Cort did a blog about VNS via the ear which put me onto it in the first place:
http://www.cortjohnson.org/blog/2014/08/29/system-reset-reduce-fight-flight-response/
Here are the pictures that go with the blog that show where the tragus is:
https://drive.google.com/folderview?id=0B_5idc3rcKskODI0VWlzQ1VZMG8&usp=sharing
Thanks very much. I think I might try it; I have huge autonomic dysfunction. Are there any side effects? I’m a little concerned about getting dizzy from inadvertent transcranial stimulation.
I haven’t noticed any side effects.
I guess it’s always a good a idea to try anything new slowly, so start with 5 minutes at a time and see how you go.
Just to add. The current should never be going across your head, only between the lower parts of your ear.
OK, I think I see . . . but the photos show the electrode at the tragus only, not at the lobe. Does the lobe electrode prevent the current from crossing your head?
That confused me as well. In their study, they somehow managed to attach the red electrode to the otherside (inside) of the tragus.
I couldn’t find clips that would do that, so I attach the red electrode to my ear lobe instead, I have one clip per electrode. The black one goes on my tragus.
In this way, the current passes between the two electrodes and never across your head.
OK, thanks for clarifying.
This is a fascinating thread on a massively useful site. Thanks to all.
I have a practical question. I have just bought a TENS machine and some of the same earclips as you, tandrsc, but like you I’m unsure exactly how to attach both terminals of the machine’s leads to a single earclip.
In the photos and video from Leeds University that you link to, it looks as though they’re plugging the black terminal into the jack on the earclip and then the red into an electrode they’ve perhaps cut out from an adhesive pad. They’re then using some electrical tape to attach that to the live side of the clip that goes on the inside of the tragus.
I don’t understand enough about the process to improvise with any confidence. Do you believe your method of separate clips on tragus and lobe is achieving the same thing?
Perhaps Duane could chip in if he sees this – I wasn’t sure whether to reply here or at the bottom of the whole thread.
Anyway, thanks in advance for any advice. In the meantime, this new device is sitting on my desk looking at me.
Darn! Maybe a lower dose???
In the University of Leeds study where they stimulated the Tragus and showed increased Heart Rate Variability (signifying increased Vagus Nerve activity) I noted that they didn’t say which ear was stimulated. So I wrote one of the researchers and he replied:
“Dear Duane, we did one ear or both and found no difference, so routinely did both (not particularly logical I know, but it worked). ”
The patients that have used these clips in our clinic will either attach to both sides, or to one side and the opposite ear lobe. The ear lobe is innervated by the nerves that come out of the top of your neck. The upper part of your ear (the largest part) is innervated by the Trigeminal nerve.
Stimulation of the Trigeminal nerve may also increase vagal activity (called the Trigeminocardiac reflex). Trigeminal stimulation is being studied for the benefit of migraines and other headaches, both treatment and prevention. I do not have any experience with that, but note it here for your curiosity. It is quite possible that stimulating the tragus on one side and either the trigeminal nerve or ear lobe on the opposite side may have other effects in the long run and may be more beneficial for different conditions, such as headaches or fibromyalgia. So far, in all the studies, and in long-term studies of implantable vagus nerve stimulation, it has been incredibly safe (minus the surgical complications).
A patient literally just stopped by (pain patient) and noted that he doesn’t know if it is helping his pain, but he states he is sleeping much better since starting to use it. It is interesting that I just noted an article today that shows the effect of pain on a part of the brain called the Locus Coeruleus may be why pain patients have difficulty sleeping. Vagal Nerve stimulation directly affects this part of the brain. I still have a lot of reading to do, and a lot of research needs to be done. But it is a fascinating area of study.
I hope this helps.
Duane
Duane,
By stimulating the tragus on both sides, or on one side and the opposite ear lobe, aren’t you then stimulating the brain in unknown ways by creating a circuit through it?
Sorry, I meant to say attach one electrode to the tragus on one ear and the second electrode to either the tragus on the opposite ear lobe. You could technically just attach one to the tragus (with the electrode inside the ear canal on the back of the tragus) and the second to the earlobe on the same ear. Remember to put a little saline on the electrode. (A pinch of salt in a little water will do).
Duane
Thanks, that’s useful and interesting stuff.
One ear or both, though, the Leeds study still attached both terminals from any one lead onto a single earclip. That’s what I’m struggling to replicate and that’s what’s worrying me that I might be doing it ineffectively.
Perhaps I’m being obtuse (in which case apologies) and the information that it doesn’t matter whether it’s both ears or one also means that it doesn’t matter whether each earclip gets a single jack attached to it or two.
I’ve just been experimenting with plugging red and black jacks into separate earclips and attaching them to the same tragus, both with electrode side innermost. It’s a bit cramped but manageable. Would that do it?
Sorry to bang on about this. The desperation to glean some improvement and the anxiety that you might not be doing it right is a powerful combination.
Gary
If the goal is to just stimulate the Vagus nerve and you are nervous about it being on the opposite ear, then put one electrode inside the ear, on the tragus, and the other on the same ear lobe.
Cranial Electrotherapy Stimulation (CES) has been done safely for 40 years across the head for anxiety/depression/sleep (attached to the ear lobes -which is why they make the elecrode clips). I think tVNS will be more successful. We have fMRI studies to show how it is effecting different parts of the brain, so it is not a complete unknown.
If you are worried about the unknown risks, then don’t do it. So far all the studies have shown incredible benefit and minimal side effects, or risks, but there are always unknown risks over a long time with a large population that you might not see in smaller studies over just 1-2 years. It just depends on what you want to try. Use at your own risk. Which is the same thing I would say about any exercise I recommend, or any medication that someone might try.
Duane
Duane, I think Garyl is asking about how to hook up the leads to the machine – he is not worried about putting the electrodes on opposite ears.
I’m replying to my own post because ‘Reply’ seems to have disappeared from below PamJ’s last post. Perhaps this exchange was getting too long and narrow.
Pam you’re right, I was just trying to find out how best to hook both wires up to one earclip. In the end I contacted Jim Deuchars of the Leeds University study and he kindly sent me a pdf showing how they did it.
He’s happy for me to share it with anyone who wants it. I don’t know if it’s possible or allowed to post attachments here, but if you’d like it let me know.
It’s basically a case of cannibalising TENS adhesive patches and taping the exposed filaments to the inside of the earclip.
If there’s some way to post or attach the document, I’d like to see how they did it, too.
@GaryI,
Do you think it is necessary to have the wires in one clip? Will it work better or differently than having one clip on the ear lobe?
If there is a reason to do it this way. I would like the pdf.
Lynn
Ellen
I lack the understanding to answer your question. Here’s what Jim Deuchars said when I asked him:
Q: What’s the particular benefit of making the electrodes this way?
A: We just thought we would be applying the stimulus across the tragus.
Q: would a pair of clips, one wired to red, one to black, on the same tragus achieve the same thing – and would the flat, electrode side be on the inside in both cases?
A: Possibly, if there is space for them on one tragus!
As far as posting the pdf goes, if Cort could let me know how to do it, if it can be done, then I’ll happily post it.
Otherwise, I could email it to people individually. What’s the forum protocol for making contact?
You are right, this thread is getting too thin.
Easier way than cannibalizing the ear clip is to just cut a teardrop shape out of a tens electrode (follow along the wire). Then use a small piece of double-sided tape on the non-electrode side of the clip, put the back of the now smaller electrode pad on this, and tape the bottom of electrode pad and wire to the clip to hold it in place. Voila, both wires can now be hooked to one clip.
With a 2-channel TENS, you could now stimulate both sides like this.
The nice thing about this is the slight stickness of the electrode holds onto the tragus better.
I recommend trying it without using saline on the clip electrode. I found that it still conducts and stays on the tragus better.
By doing the electrode this way, you will also be stimulating the Trigeminal nerve, and may be getting some of the effect through this nerve. The trigeminal nerve is responsible for the “Dive reflex” and the “Trigeminocardiac” reflex, both of which are stimulated via secondary activation of the Vagus nerve. Just an interesting tidbit. Both vagal nerve stimulation and trigeminal nerve stimulation are being studied for treatment of chronic headaches.
Just to point out, many people, including me, have allergic reactions to the self-stick electrodes.
Garyl, can you attach the pdf, if possible? I’m having brain fog trying to figure out what this looks like. Thanks.
No cannibalising of the earclip, Duane, just the electrode patch – and going one step further than your method by exposing the wire.
Your way might be easier though – the Leeds method is quite fiddly. But useful for people like Ellen who react to the sticky patches.
You can find a description of how to do this here: http://www.cortjohnson.org/forums/resources/preparing-tens-leads-to-use-in-vagus-nerve-stimulation-of-ear.178/
Glad to hear it! ME/CFS patients must lead the pack in innovation….When you have no other choice you get innovative! 🙂
Hi Cort,
Can you let garyl know how to attach a pdf. We would like to know how to attach the both wires to the tragus.
Lynn
Hmmmmm….I don’t see one…If he sends tme the pdg though I’ll attach it to the blog.
Cort
I’m going to email you the pdf. The Leeds team are happy for it to be shared so long as it’s made clear that it comes from them.
Could you please email me the pdf too, along with any other information about the experiment? I really am confused about how to hook the earclips and what settings to use on my tens machine. Also, my tens machine doesn’t have a “continuous” setting. It has massage, beat, and knead. Will it still work to stimulate the nerve? I use “beat” at the highest speed because the other two settings are too painful. This is the machine I have: http://www.amazon.com/truMedic-TENS-Electronic-Pulse-Massager/dp/B00DCEBLP4
And these are the earclips: http://i00.i.aliimg.com/wsphoto/v0/2046486680_1/100pcs-lot-DC2-5MM-Ear-clip-electrode-wire-cable-connecting-wire-for-digital-therapy-machine-tens.jpg
Laura
Hi. I emailed the pdf to Cort last week so with a bit of luck he’ll attach it to the blog soon. In the meantime, I’m happy to send it individually to anyone who wants it. You’d have to give me your email address – or perhaps it would be easier if I posted mine here (if that’s allowed) and that way anyone who wanted the pdf could contact me. Assuming it’s ok, I’ll spell mine out: gimlach at yahoo dot com.
Thanks GaryI.
I would like the pdf as well. My email is lynn at cultureshift dot com.
Lynn
You should have the pdf now. Let me know if it doesn’t show up.
Pam, Ellen and anyone else who wants it, please email me at gimlach at yahoo dot com.
You can find a description of how to do this here: http://www.cortjohnson.org/forums/resources/preparing-tens-leads-to-use-in-vagus-nerve-stimulation-of-ear.178/
Laura
Hi. I emailed the pdf to Cort last week so with a bit of luck he’ll attach it to the blog soon. In the meantime, I’m happy to send it individually to anyone who wants it. You’d have to give me your email address – or perhaps it would be easier if I posted mine here (if that’s allowed) and that way anyone who wanted the pdf could contact me.
*I just tried spelling out my email and the site wouldn’t let me post it. If Cort, or anyone who’s more used to forum-posting than me, can suggest the best way for me to get this pdf to all the people who want it then I’ll happily try it.
Ah, I see my original post got through despite the error message. The pdf is on my computer which I won’t have access to until tomorrow. I’ll send it out to everyone then.
I would like to see POTS/ME patients getting VNS stimulator. It could be ‘a prove of concept’ if it could cure the ANS problem. I Always thought that the PNS is defect. This puts the SNS in overdrive. But i am still not sure if this reaction is for compensation, lack of energy, bloodflow problems. The chicken or the egg. But for me the ANS is the keydriver for ME/POTS not the immunesystem.
I ordered this from crowd funding site for $200., to be sent out in June, has 60 day trial, can’t beat that, now can buy for a bit more from their web site. I will try it for FM, will post back after I get it. They presold thousands, to people with lots of sad pain stories, like us LOL, and they’ll get them all back if they don’t work!
What did you order and what is the website?
Jeez, sorry, I didn’t think brain fog was one of my SX..
http://www.neurometrix.com
The Quelle device pictured there. It seems too good to be true but free trial…
That looks interesting, but it doesn’t seem to be addressing the ANS.
Well, that is an interesting question. It is being marketing as a device to stimulate endorphin production but a medical device technician friend said “oh, that gadget is just another TENS.”
So…
Looking forward to hearing how it goes Steve. Good luck!
Really promising result. Certainly more research is needed
I know for me the key to key to curing most of my FM pain was finding out my IBS triggers. For me those are gluten, soy, most spices and probably many other things too. My goal is no longer to find the foods that I read to, but rather to only allow foods that I am sure are 100% safe for me. Even being this conservative it’s still a big challenge
Anyways when my IBS symptoms are gone I have pretty minor FM pain. Minor enough that while sleeping is a bit of a pain, I don’t need meds to manage it anymore
OTOH when I accidentally ingest something that brings my IBS symptoms back I have a relapse of excruciating pain
Thanks for relaying that Ian – diet can be huge for some people.
Should we expect to see NIH increase funding for such devices? If a patient decides against such a device, will a psychiatrist have the authority to override the patient’s decision? As with CBT/GET, will state disability insurers deny assistance to those who choose not to have such a device – for example, if (side)effects are not tolerable?
National Institute of Mental Health director Thomas Insel:
“… Neuromodulatory treatments, such as brain stimulation, have seen the most innovation but will need considerably more rigor in terms of establishing mechanisms of action and required dose… In the current climate, with funding tight and clinical needs urgent, we will be shifting to trials that focus on targets as a way of defining the next generation of treatments. The goal is better outcomes, measured as improved real-world functioning as well as reduced symptoms.”
National Center for Complementary and Integrative Health:
“Topics of Interest to NCCIH: …The standardization and characterization of active components of mind-body medicine interventions… Brain and behavioral neuroscience… Pain management… The accurate assessment of adherence and/or fidelity to the use of practices and interventions… Advancing pain research, from the micro perspective of molecular sciences to the macro perspective of behavioral and social sciences, including technologies associated with the neural pathways of pain… The etiology, diagnosis, and pathophysiology of chronic fatigue syndrome/myalgic encephalomyelitis…
Pathways to Prevention (as reported at / adapted from OccupyCFS):
Speakers from the psychosocial school of ME/CFS were chosen for the following P2P workshop topic, “Given the unique challenges of ME/CFS, how can we foster innovative research to enhance the development of treatments for patients?”: co-authors Buchwald, Clauw and Afari.
*Pre-P2P* Buchard wrote: [CBT/GET] “Treatment-resistant patients should be referred to a mental health professional.
Pre-P2P, panel chairman Green presented at an NIH Overlapping Pain workshop, co-chaired by Clauw and Unger. Clauw also spoke about “fibromyalgianess (the tendency to respond to illness and psychosocial stress with fatigue, widespread pain, general increase in symptoms, and similar factors)” at the P2P Opioids workshop.
http://www.nimh.nih.gov/about/director/2014/a-new-approach-to-clinical-trials.shtml
https://nccih.nih.gov/grants/types/sbir-sttr
http://www.occupycfs.com/2014/10/31/p2p-agenda-what-the-huh/
https://prevention.nih.gov/docs/programs/p2p/ODPPainPanelStatementFinal_10-02-14.pdf
http://web.archive.org/web/20150104175404/http://www.ninds.nih.gov/news_and_events/events/meeting-summary-chronic-pain.htm
???
No one ever requires someone to do a treatment.
Given how the P2P report turned out I’m not sure how Buchwald’s comments are relevant ???
Cort, I think IOM and P2P are not the friends of ME/CFS patients. They wrote a definition of ME/CFS that does not include any reference to immune dysregulation/abnormality which is a proven component of ME/CFS. They also did not exclude psychiatric illness, which means we are back to the old problem of proving we are sick, not crazy……
I think you’re getting some bad information Katherine Remember who wrote the IOM report: Dr. Bateman, Dr. Klimas, Ron Davis, Dr Rowe, Lily Chu – ME/CFS patient, Dr. Lerner, Dr. Natelson, Dr. Keller – exercise physiologist- none of these people think ME/FS is a psychiatric disorder. Most have spent their careers treating ME/CFS – these are the pioneers in the field
This just came out from CBS News
http://www.cbsnews.com/news/doctors-urged-to-take-chronic-fatigue-syndrome-more-seriously/
Christine Lisio suffers from exhaustion and body aches from chronic fatigue syndrome, but getting the right diagnosis wasn’t easy. Doctors would often say, “She’s just tired, you know,” Lisio told CBS News. “She’s got two kids. All the labs look good so you must be fine.”
“Patients like Lisio hope the IOM report, which states that chronic fatigue syndrome is a legitimate and serious disease, will get doctors to pay closer attention to their concerns.
“It says the disease is real,” Dr. Gary Kaplan of the Kaplan Center for Integrative Medicine explained. “That is the most critical piece. Secondly, it gives some clear guidelines for physicians to make the diagnoses.”
The P2P report called for urgent increases in immune and other research. It was very clear about that. It downplayed the importance of CBT.
Psychiatric disorders like depression and anxiety have never been excluded from research only certain kinds of psychiatric disorders. They simply didn’t want to exclude the sizeable number of patients who have mood disorders from research studies.
There’s some “advocates” out there that are committed a negative slant on virtually everything…They don’t give the whole picture in my book.
Thanks for bringing up your concern 🙂
“No one ever requires someone to do a treatment.”
Sadly, at least one EU country rejects ME-associated disability insurance/assistance if an individual has not done CBT/GET or completed CBT/GET to the state insurer’s satisfaction.
Even with statements from multiple specialists which say otherwise, state lawyers “win” with the claim that an individual with severe ME can be immediately back to work following six weeks of CBT/GET.
And of course, an EU psychiatrist sectioned ME-patient Karina Hansen and has held her over two years now. And EU children with ME have been taken from their parents and subjected to “therapy”.
Regarding Buchwald… Buchwald advocates further mental health services for pwME who do not recover using CBT/GET. I would like to understand how patient autonomy (and/or parents’/guardians’ rights) holds up against the biopsychosocial label and its suggested “treatment.” And why is NIH placing biopsychosocial advocates (w/ extreme views) in positions that influence policy?
What does this have to do with this article, “Reversing Fibromyalgia With Vagus Nerve Stimulation” ???
@PamJ
“This” was an answer to Cort’s questions concerning my first post.
“What does this have to do with the article..???”
VNS is a therapy/treatment. Patient autonomy is an individual’s right to refuse a particular therapy/treatment.
However, and depending on country, doctors and governments can legally violate patient autonomy. Additionally and through coercion, both public and private insurance violates patient autonomy, and this coercion is also supported by courts.
Proponents of the biopsychosocial school of thought often group Fibro with ME/CFS and Gulf War Illness, etc., as biopsychosocial, chronic pain conditions to be managed with CBT/GET.
And though patients overwhelmingly describe CBT/GET as a cruel failure, government fraud and corruption continue to force it upon people.
My thoughts then — regarding diseases categorized by some as biopsychosocial, chronic pain conditions — were to ask if NIH is moving to replace CBT/GET with VNS or other neuro- devices. Or if NIH is moving to recommend VNS or other neuro- devices, in addition to CBT/GET or once CBT/GET has failed.
Will individuals labeled with biopsychosocial, chronic pain have more patient autonomy with VNS or other neuro- devices than such patients have had with CBT/GET? Or will doctors, insurance, and government force this therapy/treatment upon patients, no matter the harms for any given individual?
Thanks, anonymous. I see your point.
However, this was just a small trial of I think 11 people w fibromyalgia, so I think it is too early to determine if this will be a worry.
I started this program July 2014 and within 4 days had energy and have not stopped since..Ive lost all my fibromyalgia weight and have reduced my meds by 60%. I have my life back for the 1st time in 10yrs. and it didn’t involve any surgery!! Ive helped many others get their energy and lives back!! I still cant believe how good I feel most days! You can find me on facebook or my website http://www.connieeagles.isagenix.com !! Loving life again and you can too!!
Congratulations Connie 🙂
Excellent news. Can you elaborate on the trial you took please. I have been searching for 17 years to find something other than drugs can alleviate the pain of Fibromyalgia.
I was diagnosed with drug-induced FM after taking a 16 week course of Roccutain for adult acne in 2005. I was prescribed 20mg Nortriptyline and gave taken it ever since.
I have tried stoping – but I can’t bare the pain. I will look into this treatment and ask to be referred, if possible. I am aware of the vagus nerve, as I use manipulation to the earlobe to control a hyper sensitive cough,that suddenly appeared 10 years ago. All the usual lung/ stomach tests came back negative.
I have a tens machine and will purchase the ear attachments- I’m really hoping this will help.
VNS has been done for a long time, in over 100,000 patients for epilepsy and depression. As discussed above, VNS at the ear(tVNS) has been studied and so far is showing to be as effective as the implantable form. Note that while there are benefits for depression and seizures at 1 month, in all the long term studies response improved at 3, 6, and 12 months. This was also seen in this small study on fms. Consistent patience is the key. Note that in studies of VNS and epilepsy, 75%of people who DID NOT respond (less seizures) reported improved mood.
VNS inhibits inflammation, and is being studied in rheumatoid arthritis, Crohns disease and other inflammatory conditions. It is being studied for many conditions, including tinnitus, headaches, chronic pain, heart arrhythmias, heart failure, improving memory, PTSD, and insomnia. Does it start to sound too good to be true?
Even more impressive is the fMRI studies showing tVNS affects the same areas as VNS, but without the surgical side effects. Overall safety of tVNS has been impressive.
Then there is the issue of cost and availability. If you read the studies, many are just using TENS units with modified electrode. As mentioned in other posts, the settings are 20-30hz (frequency or rate) and 200-500microsecond pulse width. Even cheap TENS units can be adjusted to these settings. If you buy the clip electrodes, put a drop of saline (a pinch of salt in some water) on the rubber electrode and attach the electrode to the tragus (right in front of ear canal) with the electrode part inside the ear canal. The vagus nerve innervates the ear canal, especially the front part. However, you do not need a clip electrode. You can take a regular reusable TENS electrode and cut it smaller, to the size of the tip of your pinky finger. Then place it just inside the front of the ear canal. Then use a common foam ear plug to hold it in. (One person glued his to his ear plug to make it more convenient). Unlike a TENS unit, the intensity is just to where you feel it, or if that is annoying, just below the point of feeling it. This was done in some studies, and still showed effects. Too much stimulation will not fry your brain (these units are not that strong), but will be less beneficial. a couple of people I know cranked it up to a strong current, and too much stimulation caused headaches (I did warn them, but they still thought more would better. Now they only do it to light intensity).
The idea about only doing it on the left ear was based on the implanted stimulators, because the right vagus nerve has more influence on the heart. However tVNS, because it stimulates the brain first, will affect both vagus nerves, but is not directly electrically stimulating them like the implanted units in the neck. In the recent study showing tVNS increased heart rate variability (which is a very good thing), they initially found the same effect if the stimulated the right or left ear or both, so for the purpose of the study they did both.(email communication with the author).
From what I can find 20 to 30hz is based on the frequencies used for implanted VNS stimulators. This is because below 20 or above 30hz affected the vocal cords. tVNS does not affect the vocal cords, but the same frequency has been used. So we don’t know what is best. tVNS has also only been done on constant stimulation 15 to 60 minutes once or twice a day. This has shown to be effective, by we don’t know if a “pulsed” mode would be more or less effective, or if longer times or more frequent usage would be better. The good news is that so far, over many years of animal and human studies, it is amazingly safe so far. So for many it will be worth the trial. But again, stick with it and be consistent because the benefits increase over time.
Breathing at a rate of 6 breaths per minute or less will also stimulate the vagus nerve. 8 will not, 10 or 12 breaths per minute will not. This has even been shown in unconscious patients on a respirator. Not until they put the rate down to 6 breaths per minute did the heart rate variability increase. So anytime using tVNS you should practice slow deep breathing to maximize the effect. When you aren’t doing tVNS you should consciously practice slow deep breathing to prolong the benefits. Over time research shows that your overall breathing rate will slow, and the benefits of vagal tone will be more consistent. There are phone apps that you can use that can show you your improving heart rate variability with slow deep breathing. This is a type of biofeedback similar to that used in many clinics.
There is a lot more on this topic, but that is enough for now
Thanks Duane!
Thanks, Duane, is there a website you know of where I can read more about what you’ve written?
Sorry. I am not aware of any one source for all the information. I have been studying this topic for the last couple months because it relates to my work in an integrative pain management clinic. I have read hundreds of abstracts and papers on this topic. If you search for “vagus nerve stimulation” on PUBMED you will find most of this research. A good overview of vagus nerve stimulation is “Vagus Nerve Stimulation” by RH Howland in Curr Behav Neurosci Rep. 2014. Jun;1(2):64-73. I have a background in biochemistry, physiology and anatomy so I am fascinated with the research being done in this area, but the research can be a little technical for the lay public. I am in the process of writing a paper on vagus nerve stimulation, but there is so much research to correlate that it will be a while until I finish it. If someone has a specific question on something I said in my last post, I could possibly point them to a specific reference so they could see the research.
Thanks for sharing your considerable knowlege. When you finish and publish your paper, perhaps you could send the link to Cort Johnson
Afterthought: “Cyberonics CYBX, +1.01% shares fell 8.1% to $53.10 on moderate volume after an appeals board supported a 2007 decision by the Centers for Medicare and Medicaid that the company’s pacemaker-like device for treating depression did not necessitate national coverage for the device. The company said it is evaluating options for challenging the decision handed down by the Department of Health and Human Service’s Departmental Appeals Board…”
http://www.marketwatch.com/story/gm-ford-hollyfrontier-shares-in-focus-monday-2015-01-04
Also, and just as a curiosity: “The year 2013 marked the 25th year of clinical vagus nerve stimulation (VNS)… Bailey and Bremer [2] (Bailey & Bremer, 1938) demonstrated the direct effect of vagus stimulation on the central nervous system.” http://cdn.intechopen.com/pdfs-wm/47055.pdf
And: “Charles Beard (1839-83), who popularized the disorder known as neurasthenia or nervous exhaustion, also promoted the use of electricity to treat it. Beard suggested that applying electricity to the spine or key areas of the body would reinvigorate the cells and restore the patient to health… Physicians using electricity claimed they could cure intractable neuroses such as neurasthenia or hysteria. The practice was popular from the late 1800s until after WWI when it was identified by Morris Fishbein and the American Medical Association as a form for quackery and quickly abandoned…” (from “Mental Healthcare Issues in America”)
I bought a TENS machine and the ear clips.
I used it for the first time yesterday. I followed tandrsc’s advice and attach one electrode to the tragus and one to the ear lobe. The settings were as advised : Pulse Rate = 30, Pulse Width = 200. I turned the intensity up to 2 and felt a tingling. It wasn’t pleasant but it wasn’t painful either. I used the unit for 15 minutes.
Results:
While using the unit, I could really feel myself breathing with my diaphram. I have problems doing that naturally and am currently seeing a physical therapist to help me with that. I thought the breathing was a good sign. Unfortunately, I had a headache afterward all afternoon but began to feel better after dinner. I think I had the intensity too high and perhaps I did it for too long for the first try.
Unexpected Results:
My husband and I often play a game of cards at night. Last night we played and I was able to deal out the cards very crisply and rapidly. This is something I have not been able to do in years. In fact I would say that I usually fumble the cards out rather than deal them crisply.
This gave me so much hope. Nothing else had changed that day except the usage of the TENS machine. So I used it again before bed. Only for 10 minutes and hardly any intensity at all. I couldn’t feel the buzz on my ear but I could feel my breathing improve.
I woke up this morning in good spirits with an involuntary smile on my face. I also lay in bed and could feel the easy breathing that normally is so hard for me to do.
I have great hope for this treatment. We’ll see what comes of it.
Lynn
Lynn,
Do you have breathing problems from fibro or some other problem? I’ve found that pain from fibro makes me breathe shallowly and I have to consciously try to breathe deeply. I’m glad the TENS helps and keep us posted.
I’m awaiting the delivery of my apparently-TENS unit, Quelle, as mentioned above.
Hi Steve,
I have the same shallow breathing associated with ME/CFS and Fibro. I am diagnosed with both but have more energy problems than pain.
I was able to get on some good insurance this year and am seeing a Physical Therapist to help me build my exercise capacity. I did some biofeedback sessions and they determined that I needed help with breathing using the diaphram before I could even begin to exercise. I tend to hold my breath a lot. So I was already working on that and the TENS machine looks like it might help me with that goal.
Good luck when you get your Quell.
Lynn
Good luck Lynn!
I have another blog on vagus nerve stimulation coming out. It can really produce results in the right person.
Please let us know how it goes.
Hi Lynn,
Was wondering if you had more benefits after using the tens for a while now ?
Less fatigue or better sleep maybe ?
( brainfog ?) and what type of machine did you buy?
Best John
Hi John and Lynn,
My question to Lynn is whether you have significant pain reduction. I have many varieties of severe FM pain, my primary sx. I have the electrodes on order but if pain is not your major problem or if no one here finds a significant pain reduction with this technique, it will be difficult to get myself to do it. John, am trying Thync a few more times today, doctor friend will try once tomorrow. Will let you know results.
Sorry to hear from your pain Steve. Good luck with trying thync again, it sounded so promising !
Best John
John apple and Steve,
I bought the ear clips and a TENS 7000 from discountmedicalsupplies.com. They cost about $40.
Unfortunately I discontinued the protocol due to irritation in my sinuses and especially my ears. I continue to have ear aches even after six weeks of non use. I did use the machine on the lowest possible level. Barely even turned on.
Interestingly my increase in dexterity has stayed with me even though I discontinued the process.
Pain is not a major symptom for me. I cannot speak to whether it will help with that. I did not notice any decrease in fatigue or better sleep but I only used it about six times.
I hope that helps.
Lynn
Thanks, Lynn,
This is informative and unsettling. I’m terribly sorry you have been experiencing these problems. Your experience will certainly help me reevaluate this procedure. Your attempting it shows the degree of desperation those of us with these disorders experience. Since I have chronic severe sinus infections and have barely avoided surgery several times, I’m particularly nervous about a procedure that could cause that side effect. I may just consider the thirty bucks sent off for those GB ear electrodes as dumb money.
I just ran into an acquaintance my age, 67, who told me he is retiring and will be teaching skiing FT up north this winter. WTF. I was standing there with my cane thinking how I can’t even do simple exercises I’ve done for 25 years anymore without awful neuro pain several hours later. It would be tempting to feel sorry for myself except a nearby college acquaintance died suddenly in his sleep and another family friend is dying of ALS. I guess chronic pain is a step above those. GLTA.
Hi Lynn,
Thanks for your answer. Its a pitty it didnt bring you more positive results
Best John
Could someone email me the pdf from Leeds please? Thank you 🙂
Cort has posted the pdf on the forum:
http://www.cortjohnson.org/forums/resources/preparing-tens-leads-to-use-in-vagus-nerve-stimulation-of-ear.178/
Click the big green “Download Now” button.
I’ve only just noticed the thread on my original comment. I’m so pleased people have given this a go.
I should have said to turn the intensity down if the tingling is painful or unpleasant so that you barely feel it (or don’t feel it at all), but Duane and Lynn have covered that point nicely in their comments.
I use the “continuous” mode on my device. I’ve tried the “beat” and “Modulation” modes but like “continuous” best.
Thanks to Garyl for contacting Leeds to find out how they attached black and red electrodes to the same clip. I’m kind of glad that they had to muck about with scissors and tape as my two clips solution is better for me.
This picture shows that some of the vagus nerve endings are in the ear lobe, so I am comforted to think that the current is passing across more of the endings with two clips.
http://www.biomedcentral.com/1472-6882/12/255/figure/F2
I’ve posted some pictures of how I attach the clips in one of Cort’s forum posts:
http://www.cortjohnson.org/forums/threads/reborn-ii-vagus-nerve-stimulation-and-inflammation.2645/#post-5197
It always takes me days to reply as I have to follow every link on every page!
This blog seems to fit me like a glove! I had infantile torticollis on the left side which was surgically released when I was around 18 months. This was followed by agonizing exercises for years – which my parents had been ‘trained’ to carry out. My first memory is of these exercises and my begging my parents to stop. My dad refused to carry on and I think this was the basis of my difficult relationship with my mother.
It seems entirely possible that the left branch of the vagus nerve was damaged at this time. How much did they even consider this in circa 1957?
Somebody – I think you Cort – mentioned using a tens machine to stimulate the nerve. I have frequently used mine in that area using a basic pulsing setting. It often lulls me to sleep. I don’t think this can be a coincidence! This is very exciting stuff!
I will research the normal location and the depth under the skin etc and have a go at using it daily for a while to see how it goes. Incidentally, I have recently been diagnosed with tachycardia following fainting episodes. Perhaps the most primitive autonomic system (according to Dr Porge) is making me play possum!
Wonderful as usual Cort.
Christine
This is my first time posting on this site and I’m not sure how long discussions remain current. I was so glad to find this article and discussion on vagus nerve stimulation. I have a history of CFS, fibromyalgia, and PTSD, and it’s long made sense to me that disruption of the autonomic nervous system from early trauma might be a key factor in my physical illness. I’ve had two severe flare-ups of the PTSD since January with a relapse in my health after the first. I’ve been experimenting with a rather old TENS unit and ear clips modified according to the resource section. I haven’t had any severe flashes of anxiety or terror since starting. It’s not clear to me whether this is just part of the PTSD cycle (closing down after a period of high arousal) or the benefit of the VNS. I’ve noticed that I my teeth hurt after the VNS and for some time afterward. I also have a slight headache that lasts. This is even at very low settings. I’m wondering if others have experienced these side effects. I would love to be able to hear from people who are experimenting with VNS in an ongoing way. Is that possible?
Low settings is a must. Just at the point of feeling it, or just below. It is not like using a TENS for pain where strong intensity is better. Too high tVNS stimulation diminishes the benefit. I have had patients try different ears and positions of electrodes. It seems each finds a position or combination that works best for them. So try different positions or each ear separately until you find what works best for you. Remember that the effects are additive. When you find what works best, be consistent because in most of the studies benefits were better at one month, even better at 3 months, and even more at 6 months and 1 year. But it should not be causing you pain or headaches. Either the intensity is too high or positioning is not optimal for you.
Thanks for the response, Duane. This is an old TENS unit and it seems to have different settings than others. I’ve set the frequency to 20 and the intensity to 1 or 2 out of 10 and still experienced the side effects. I’ll have to experiment with other factors. I do plan to try this for the long haul.
I hope people do keep this thread going as I will probably try VNS for my fibro. I’ve had to start Tramadol daily, not too effective and a bad long term semi-treatment. As I noted above, I am trying out Quell, a high tech TENS unit that sold 2000 crowdsourced devices. One month of solid treatment has not helped reduce my pain; there’s another free trial month I will plow through. About a dozen folks with various ailments have posted positive results on the Facebook page. Everyone has had this as long as I have, though, and nearly 2000 units will go flying back to Neurometrix for refund if they don’t work. I’ll let people know if it starts to reduce pain. I also have an old TENS unit with vague settings and don’t want to trade VNS side effects for fibro pain. I have a new Thync device on order, not marketed for pain but I wanted to see if it helps my pain while hacking my emotional framework. Last on my list will be direct crainial stimulation, also a bit spooky. I’m afraid that messing with my nervous system directly is even less comfortable for me than whacking it with Big Pharma.
I don’t have a big pain problem right now – but then I moved from Tramadol to a Fentanyl patch. I’m thinking of coming of it to see how bad my pain levels are now.
When you say ‘direct cranial stimulation’ do you mean Craniosacral Therapy? I’ve had sessions of that years ago and I think it was very powerful at the time – both physically and psychologically. I’d like to try it again if I can find a good practitioner.
I’ve got my ear clips from Amazon and at a low setting it will calm me down.
At a higher setting, it stimulates me a little too much and I can get irritable.
I can’t find a setting at the right level somehow. If I can, I hope that will help with the fatigue.
I’ve misplaced my oldest tens machine and have been using one I bought from the same chemist a couple of years later. It doesn’t have exactly the same settings. I can’t remember where I put my original one but will use that when I find it. I think the pulse setting is better on that one and I hope that it will be easier to find just the right strength setting to stimulate me just enough to help with the fatigue.
This is all very interesting! Keep it coming folks.
Hi,
I meant VNS, still a scary concept to me but within possibility as other treatments fail. I am going to send back the Quell device…it is just not helping my fibro pain. I am also d/cing my Tramadol, gave me one great pain reduced day after four days of use, then have had nothing but anticholinergic effects. No sense in getting dependent on a med that doesn’t work. The odd Thync device is now on its way, not marketed for pain but it is a type of neural hack so we’ll see. Will post results of that one. Looks like I will order some electrodes for VNS, try after a few med retrials, maybe LDN again. Not a good time here.
Hi Steve,
Was wondering if you already recieved the Thync device and tried it ?
reg
John
Hi John,
Yes, I was waiting to try it a few more times before posting but my preliminary trials have gotten me no effect from either the calm or energy ” vibe” strips, a big disappointment. You get several packets of strips, one use only unless you keep on the same electrode strip and keep redoing the Borg-like forehead device, controlled through an app. I was nervous trying it the first time so was on the phone with a rep while doing it. She told me the success rate is pretty variable. I had a doctor friend try the energy vibe yesterday, also no effect. She will try calm next week and I will retry both again maybe, got extra strips because I was a first adopter I think. Lots of prof. reviewers like it, one had no effect. Google the WSJ review, pretty amusing, a super high power neuro academic did not want to try it. I’m pretty sure you won’t do anything bad to yourself with it, more optimistic than the neuro guy LOL. The bottom line is, if you are on this thread and have $300. Plus postage for a “free” 30 day trial, you don’t have much to lose. We are all in pain here. The strips cost five bucks, I think, but I’d go into debt to keep in supply if they worked for me! I’m a lot more nervous about hacking my vagus nerve with a TENS, was joking with my doc friend I should do it outside my local ER.
Over 100,000 people have had vagus nerve stimulators implanted in their neck over the last 25 years. Side effects are mostly from the surgery, or effecting the nerve to the voice box due to the location of the electrodes in the neck. Functional MRI studies show stimulating the Vagus Nerve via the tragus of the ear affects the same parts of the brain that the implanted devices stimulate, and there is no surgical procedure and it is nowhere near the other nerves in the neck, nor is it directly stimulate the nerve towards the heart, so it is much safer. There have been no major side effects noted in all the studies where the Vagus nerve was stimulated at the ear. Light headedness in some patients is about the only reported side effect. Long term studies of VNS also show it is safe and even show benefits are actually additive over the long term.
If you are opposed to stimulating the vagus nerve electrically, then 20 minutes of slow deep breathing at no more than 6 breaths per minute will also incr the activity of the Vagus nerve. We show patients this with biofeedback. They can actually see that when they get to 6 breaths per minute the activity of their vagus nerve significantly increases. In a recent study 20 mintues slow deep breathing at 6 breaths per minute (versus another group breathing at 12 breaths per minute) has been shown to speed the ability to fall asleep in patients with insomnia and improve the depth and restfullness of the sleep. In animals vagus nerve stimulatin increases the production of Melatonin in the brain, which improves the more days that the stimulation is done. In fact, the patients I see and recommend VNS at the ear with a TENS unit, I always instruct them that they should be doing slow deep breathing at the same time to maximize the effect. By no ways is it a cure, but it won’t damage the liver, burn a hole in the stomach or cause kidney failure, so if it is beneficial, it would be worth the effort.
Duane,
Please don’t mistake my sense of humor as disparagement of your posts or VNS info;I am taking careful note of all of your and others’ helpful comments. I’m doing sequential trials of a few more probably useless things that have reportedly been helpful to some folks…magnesium supplementation, then colloidal Circumin. I’m also ordering some ear clips so I can dust off my rusty TENS and try VNS in a bit. I hope you and others continue to post info and experiences related to this technique.
Thanks Steve, for your answer. Maybe it will work after a couple of times more (hope so)
Ill probably give it a try also when the next devices ship,
Thanks again,
John
Dr. James Fugedy left this comment:
Transcutaneous vagus nerve stimulation (tVNS) produces similar effects to implantable VNS, but tVNS is safer, easier to do and much more affordable than VNS.
Transcranial direct current stimulation (tDCS), a painless, non-invasive neuromodulation technique, is even more effective than VNS for fibromyalgia (Efficacy of transcranial direct current stimulation and repetitive transcranial magnetic stimulation for treating fibromyalgia syndrome: a systematic review: http://www.ncbi.nlm.nih.gov/pubmed/?term=tdcs+fibromyalgia+marlow). The only drawback of tDCS is cost, but self-administration eliminates that restriction. tDCS is easy to do, without adverse or side effects and with appropriate training and supervision can be done at home.
Sounds like to me she had been suffering from a tick born disease. Because all her symptoms matched the ones I have. Which affects and infects the vagus nerve. Causing low energy, pain,weakness, swelling, arthritis, brain cognition, abdomen weakness or paralyze, heart, lungs affected and more. I was also bedridden for months and still not better. I can feel that nerve and it hurts bad. Fibromyalgia is a problem created from the disease. I’m not a Dr but I know how I feel.
Thanks for all the contributors to this forum for the information I have gleaned from then regarding tVNS; it has helped me with my usage – but which is not because I have ME or fibromyalgia.
Members may wish to know of the recent research that prompted me to look into this:
‘Tickle’ therapy could help slow aging, research suggests (https://www.sciencedaily.com/releases/2019/07/190730083706.htm)
From this I have looked at many pages, some from links mentioned in this forum:
http://www.onlinejacc.org/content/65/9/867
https://bmccomplementalternmed.biomedcentral.com/articles/10.1186/1472-6882-12-255
I bought my TENS machine, EM-6300A, on Amazon for £50/$US60:
https://www.amazon.co.uk/Professional-Rechargeable-Stimulator-Programmes-Adjustments/dp/B00KVOI74Q/ref=sr_1_22?keywords=med-fit+tens+machine&qid=1564489307&s=gateway&sr=8-22
And two ear-clip electrodes, also on Amazon, for £7/$US9:
https://www.amazon.co.uk/TENS-Ear-Clip-Electrodes-Machines/dp/B00OZMNWYA/ref=sr_1_fkmr2_1?keywords=2.5mm+ear-clip+for+TENS+machine&qid=1565096044&s=gateway&sr=8-1-fkmr2
I clip the red +ve on the vagus and theblack -ve on the ear-lobe; use program P1 for 20′ at 80Hz and 20microsecs pulse.