There’s something about migraines and fibromyalgia and chronic fatigue syndrome (ME/CFS). Migraines aren’t usually talked about as major comorbid disorders with these diseases but recent studies suggest, however, that migraine may be one of the most, if not the most, common comorbid disorder for both of these illnesses. These studies – most of them fairly small – have suggested that from 20-30% of people with FM and as many of 80% of people with chronic fatigue syndrome may experience migraines.
One study suggested that most people with ME/CFS, FM and/or GWI who experience tension headaches (dull head pain, pressure around the forehead, tenderness around the forehead and scalp) also experience migraines. Frequent tension headaches alone can induce an overall hypersensitivity to pain.
Perhaps because it was picked up by the medical community before “central sensitization disorders” like FM, IBS, interstitial cystitis and ME/CFS became known, migraine is not often included in that pack. Migraine, though, appears to share similar central nervous system findings as other central sensitization disorders and it’s hard to think of a disorder in which hypersensitivity to outside stimuli plays a bigger factor – at least for a time – than migraine.
Migraine shares some other features with ME/CFS and FM; it largely strikes women, it most often appears during times of hormonal fluctuations, pregnancy often reduces symptoms, it can be triggered in many ways including stress and there’s a genetic and sometimes a relapsing/remitting component. People with ME/CFS and/or migraines typically retreat to the same environment – dark rooms – in order to recover.
It turns out that migraine sufferers don’t spontaneously recover from them. In the days or week following a migraine many people with migraine can look very much like ME/CFS/FM patients.
One description of a typical “failed” migraine patient is instructive
“..a middle-aged woman with chronic migraine and medication overuse, as well as fibromyalgia. In addition, there is anxiety and depression, fatigue and insomnia, and the familiar exhaustive list of psychotropics and antiepileptic drugs tried and failed”
Now a very large study tells us definitively not only how common migraine is in fibromyalgia but what kind of burden it adds to the illness. It turns out that the burden is large indeed.
Frequency of Migraine Headaches in Patients With Fibromyalgia. Brinder Vij, MD, FACP; Mary O. Whipple, BSN, RN, CCRP; Stewart J. Tepper, MD; Arya B. Mohabbat, MD; Mark Stillman, MD; Ann Vincent, MD. Headache 2015; doi: 10.1111/head.12590
This study demonstrates how potent a tool patient registries can be. In this REDCAP study, emails sent out to 4421 FM patients in a Mayo Clinic Patient Registry asked for demographic and medical information and included a validated “ID-migraine screener”.
The migraine screener simply asked if the participants headaches were associated with sensitivity to light, nausea and what kind of effect their headaches had on activity. A yes answer to two of the three questions indicated they met the criteria for migraine.
The diseases asked about included: hypertension, coronary artery disease, myocardial infarction, mitral valve prolapse, epilepsy, stroke, asthma, irritable bowel syndrome, gastrointestinal disorder, glaucoma, Raynaud’s phenomenon, chronic fatigue syndrome, depression, anxiety disorder, bipolar disorder, and post-traumatic stress disorder.
(Studies suggest that having fibromyalgia is associated with an increased risk of having many other disorders including irritable bowel syndrome, chronic fatigue syndrome, rheumatoid arthritis, systemic lupus erythematosus, osteoarthritis, sleep disorders, hypertension, type 2 diabetes, depression, and anxiety.)
Results
1730 people returned the questionnaire. The demographics were familiar. Ninety-two percent of the participants were female, 97% were white, and the mean age was 56.
Some general findings stood out as well. Very high rates of depression, anxiety, chronic fatigue syndrome, irritable bowel syndrome and high rates of hypertension (something that’s probably at odds with ME/CFS), asthma and gastrointestinal disorders were found.
Migraines Very Common in Fibromyalgia
Fifty-six percent met the criteria for migraines. (A higher percentage of FM patients met the criteria for migraines than had been diagnosed with ME/CFS.)

The “penalty” for having migraines and fibromyalgia was a greatly increased chance of having other co-morbid disorders as well.
The “penalty” for having both fibromyalgia and migraine was a steep one. Women with FM and migraines had significantly higher chances of also having been diagnosed with hypertension (p<.004), asthma (p<.01), irritable bowel syndrome (p<.02), depression (p<.0002), anxiety ( p<.001), PTSD (p<.005) and finally (and most of all) chronic fatigue syndrome (p<.0001).
Two disorders, in particular, stood out. The greatly increased risk people with FM have of being diagnosed with ME/CFS and/or depression, if they also experience migraines. ( Many doctors tendency to first misdiagnose FM and ME/CFS patients with a mood disorder could exaggerate the incidence of mood disorders).
That suggests, of course, a common pathophysiology is present.
Common Pathophysiology?
The high concomitance of fibromyalgia and migraine suggests that these pain disorders may share some degree of common pathophysiology. Authors
The author proposed it’s past time to take a deeper look at the commonalities in FM and migraine, and suggested a raft of possible factors that might fit: alterations in neuroendocrine functioning, vascular (blood vessel) changes, immune activation, neuronal plasticity, nerve issues, hormonal influences (gender imbalance) and neurochemical alterations.
They’re not the first. Baraniuk, an ME/CFS, GWI and FM researcher finds similar kinds of altered brain structure and “brain energetics” in all these diseases.
“Similar patterns of gray and white matter abnormalities and altered brain energetics in GWI, CFS, FM, and migraine suggest that common central mechanisms may contribute to the type of headaches and cognitive impairments perceived as ‘brain fog’.
In fact, Baraniuk proposes that the hypoxic and anaerobic conditions that migraines and other disorders which feature cortical spreading depression (CSD) leave in their wake has become chronic in ME/CFS. In other words, whether you experience migraines or not, Baraniuk believes your brain looks like you just had one.
Migraine Treatments
Migraine is not easy to treat but Baraniuk believes that migraine treatments can be helpful in both ME/CFS patients experiencing and not experiencing migraines and highlighted Imitrex (sumatriptan). Other (triptan) drugs include rizatriptan (Maxalt), naratriptan (Amerge, Naramig), zolmitriptan (Zomig), eletriptan (Relpax), almotriptan (Axert, Almogran), frovatriptan (Frova, Migard, Frovamig), and avitriptan (BMS-180,048).
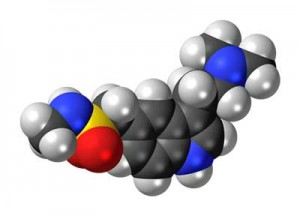
Sumatriptan is a well-known anti-migraine drug that reduces inflammation in arteries and veins in the brain by enhancing 5-HT (serotonin) production. Increased 5-HT production causes over-dilated veins to constrict. Sumatriptan also deceases the activity of nerves called the trigeminal nerves that are associated with cluster headaches.
Dr. Katherine Downing-Orr features nimodipine, a calcium channel blocker used for migraine relief, in her treatment protocol for ME/CFS. Dr. Jay Goldstein also recommended nimodipine. Find out more about Nimodipine and ME/CFS/FM here.
Dr. Teitelbaum uses natural remedies including magnesium to get patients out of a migraine. Dr. Hyman also recommends magnesium and other factors (including CoQ10) depending on how the migraine is triggered. (See Health Rising’s video section for more.)
Check out more possibilities for treating migraine including natural alternatives – Migraines, Chronic Fatigue Syndrome and Fibromyalgia: Treatment Options
- If you’ve tried Imitrex please tell us how that went here.
- If you’ve tried Nimodipine please tell us how that went here.
Poor Funding
One last commonality between ME/CFS, FM, migraine and other central sensitization disorders exists: poor funding. Despite the fact that approximately 20 million Americans suffer from migraine and that migraines cost the American economy about 30 billion dollars a year, migraines receive just 21 million a year in funding. Per patient spending, per year on migraine is about the same as it is for fibromyalgia – about a dollar a year.
Diagnosis
Migraines are under-diagnosed but migraines can be self-diagnosed using a simple three question test. Do you experience migraines? Find out and let us know here:
Chronic migraines are even less well diagnosed that migraines. A new self-scoring questionnaire has been produce that diagnoses chronic migraines. Check out that questionnaire in the Resources section of the Health Rising Forums.
Migraine Video’s : Check out our extensive media section on migraines including more in depth discussions on pathophysiology and treatment.







i have a friend with fibro BUT headaches are very rare for her and VERY SEVERE for me with M.E. so severe i can’t even talk and let anyone know how ill i am. i just lie and can’t do a thing because nothing helps with this pain and pressure. they are not as powerful as they were almost 2 decades later. what gives?
I don’t know. ME/CFS has not had the big studies examining migraine prevalence like this recent study but migraine is clearly found in both. She’s probably in the 50% or so FM patients who, thankfully, don’t get migraines.
Teitelbaum says intravenous magnesium IV’s can be very helpful during an attack – if you can get them..
My doctor diagnosed me (in 2013) as having both ME/CFS and Fibromyalgia, and said that they were caused by a chronic long-term disease.
He gave me close to 30 blood tests, and diagnosed the “cause” as chronic Lyme disease, plus co-infections including babesiosis, bartonellosis, plus the Herpes Family.
The spirochetes of Lyme disease (Borrellia burgdorferi) can cause migraines, as the corkscrew bacteria inflames the brain.
In high school, circa 45 years ago, I had terrible migraines. Bright light would often trigger them. I suspect that stress did, as well. They came out of my back at the base of my neck (a-ha! a fibro trigger point), crept across my scalp and overwhelmed me with pain. They made me nauseous and I had to lie down in a dark room.
I learned that I could ward them off by taking 4 aspirin (at one time) if I felt that pain start in my neck. If I needed to take four more, I would.
If I took codeine for those headaches, it would not touch them.
These days, I take 4 Aleve every afternoon for pain throughout my entire body. Some days, although hard on the liver, I might take two doses of four. After suffering from chest pain in 1997, my doctor had me start the 4 Aleve dose. (A-ha! Another fibro trigger point that I was not told was a trigger point.)
I also take LDN and Ketamine at bedtime (for pain).
After studying ME sites such as this, along with chronic Lyme, co-infections, and more, I am convinced we’re all suffering from the same malady and that it is a dysfunction/suppression of the immune system. Acquired Immune Deficiency. Probably infectious.
i have fibromyalgia and chronic migrane, ibs, cfs, along with alot of other medical issues. these are the most urgent ones. getting migrane between 7-10 times a week is not so fun. all i can do is go to a dark, quiet room and lay as still as i can be. i miss out on alot, but this has been my life since i was 13. i am now 42 and mother of one. i think he gets migrane and fibro too. i would not put this on anyone. have spent many nights-weeks in hospital because of all this. thank god i have a wonderful and compassionate dr whom understands, and tries to help me as much as he can. i don’t know what i’d do without him. i also have a wonderful husband and son who support me. their support is my life line.
Good luck to you Shannon!
I have migraines with FM and CF, Adrenal Insufficiency, Crohn’s just to name a few. In April 2018 mine were so bad for nearly a month and I could hardly get out of bed. After trying a few different meds in addition to Topamax, my Neurologist put me on Propranolol and it has been great except for the fact that it lowers my blood pressure even more and I also have POTS. I have to take Midodrine too now but at least my migraines are few and far between. I also had the daith piercing and I’m not sure if it helped the headaches but it immediately got rid of the stopped up feeling in that ear.
There’s a great effervescent (mix powder and water) magnesium supplement called Calm for anyone who doesn’t like shots or big pills.
Hi All,
I started on Cymbalta years ago to round out my cocktail of pain medications. It took awhile before I realized my migraine headaches had stopped. I had no idea that was even part of this medicine’s responses. My long history had been 5 – 7 debilitating migraines weekly.
I am no longer on Cymbalta. Sudden Withdrawal from it was horrendous. I thought I was dying. Unbelievable experience.
Once again the constant tension in my head, neck and jaw (as well as highly increased pain levels) is causing me to wonder if I should add Cymbalta back into my regime of care. ????? How poor a decision would that be? Any thoughts or experiences on this you can share with me would be greatly appreciated.
Carol
Hello, Carol-
I couldn’t take Cymbalta at all. It didn’t help me at all but made me feel quite insane. I was so relieved that the terrifying symptoms disappeared almost as soon as I stopped taking it! However, I was then prescribed Cipralex (not the generic, which, no matter how much they insist is identical is NOT) which worked extremely well. After suffering at least one 3-day migraine (or would have, if not for Imitrex) every month for many, many years, I began to notice that both the frequency and severity of the headaches had diminished and that whenever I stopped taking Cipralex, I would get a migraine.
Have you tried Cipralex? Possibly my experience is- as so many medication effects are- unique to me, but it would be interesting to know if this drug has had a similar effect for others who suffer both ME and migraine.
The survey doesn’t include a category for ocular migraines which have many of the same symptoms as regular migraines but don’t always develop into full-blown painful migraine headaches. I have experienced ocular migraines regularly for many years. Given the information coming out of the recent ME Conference about the connection with the eyes in this illness, I find this to be particularly interesting.
Right, I was surprised to learn there are seven major types of migraines and some people break migraines up into many more types. It would be interesting, indeed, to learn if ocular migraines are over-represented in ME/CFS and FM patients.
A neurologist told me ( about 25 years ago) that he considered any headache that was bad enough that you couldn’t do anything a migraine.
I have hypermobility syndrome plus fibromyalgia and pstd due to being raped. I get terrible migraines which can last for 18 hours and then i get a rebound chronic headache which lasts days. Its a vicious circle and then they will suddenly stop, why? I dont know. The fatigue after these attacks is prolonged, lasts months. I also have IBS, TMJD, arthritus scoliosis and cervical spondilosis in my neck. Whiplash three times hasn’t helped. I would be interested to know more about nerve compression especially in my neck and joints when they are swollen with bursitis. I am 56 and menopausal which the dr uses as a reason for my conditions. I had a hysterectomy due to a bad prolapse in 2006.
You really fit in this group Stephanie. I’m sure the hypermobility just makes things worse with your head issues – and then there’s the whiplash – and all the other stuff.
hey cort, have you asked about NECK type injuries, NOT necessarily whiplash, just accidently twisting ones neck and it cracks then you notice things aren’t right anymore? it can even affect ones vision?
I’ve read somewhere that OUR headaches are WORSE then migraines.
I had neck & twists that a osteo. dr. was did on me when he twisted me wrong and for a week I couldn’t walk NORMAL till I went back and he twisted me RIGHT. look at football players brains & I mean i’m thinking simply injuring ones neck can really mess one whether right away or in the future and its something that doesn’t show in tests/x-rays? dr. from fibro/fatigue place told me I have a “WEIRD DEMENTIA” from M.E./CFIDS.
Check out this thread on the Health Rising Forums – http://www.cortjohnson.org/forums/threads/high-intracranial-pressure-symptoms-anyone.2797/#post-6302. There are some more as well. Merida has some information on this and we have a blog coming up from her on it. 🙂
I am not sure wheree you’re getting yor info, but great topic.
I needs to spend ome time learning moree or understanding more.
Thanks for magnificent info I was looking for this information for my
mission.
🙂
I have fibro myalgia, Interstitial Cystitis, MS, Chronic migraines. I am seeking a Doctor who works with IV Ketamine, nothing else works.
Superior CBD pain relief oil works! I am chronic pain sufferer, migraine and fibromyalgia patient. For the first time in 32yrs no side effects and pain are diminished enough to do everything I want and when pain bleeds through two drops under the tongue and 20 min later I am able to breathe again with significant pain reduction! No joke people!
Thanks Jackson, Health Rising just published a CBD success story and have another article coming out. Can you say which CBD product works best for you and include the level of THC in it if it has any as well?
https://www.healthrising.org/blog/2018/11/25/pinetrees-chronic-fatigue-syndrome-m-e-cbd-oil-success-story/
We’re creating a page of products that help people.
I have been diagnosed with CFS/ME and been in bed for 4 years, I have had healthy mind therapy and been following the guidance of a private nutritional therapist, as it seems that with the limited availability of knowledge and understanding of this unseen illness, a healthy diet is more likely to increase my energy levels. This is very important to me as I suffer with increased intestinal permeability (leaky gut) The constant battle between health and bad gut bacteria is a real struggle with my recovery. Just to add to my grief I have been suffering with an intense migraine which is now 12 days long and I am pretty suicidal, I am in bed in a pitch black room, attempting to relief the pain using a combination of sumatriptan tablets and zolmitriptan (nasal sprays). Is anyone out there in the same situation and can they share their advice, I am at the end of my tether.
My head pain is in the back half of my head. It burns and stings so badly. I had my neck twisted by a chiropractor twice 16 yrs ago. And had lidocaine injection on the left occipital nerve 18 mos ago. Now the pain is worse than ever. Lyrica does help some, except in cold weather. Does anyone have any advice for me?