



(This is a lengthy blog. Now might be the time, if you haven’t used them yet, to use the print or PDF buttons at the bottom of the blog)
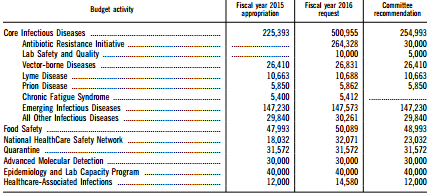
Recently a Senate Subcommittee zeroed out the entire budget of the CDC’s CFS program for next year in an Appropriations bill. It’s not clear why they did so, but initial reports suggest that chronic fatigue syndrome’s lack of representation on the Hill may have lead the subcommittee to believe it would be an easy mark. (Note that the Infectious Disease section of which chronic fatigue syndrome is a part received about a ten percent increase in funding.)
Losing the CDC program would cut in half the research dollars the federal government devotes to ME/CFS. Upon learning of the possible funding cuts Jennie Spotila’s question – “Why not just let the CDC program go?” – sparked an at times furious debate. That debate sparked me to do something I’d promised to do for a long time – a complete overview of the CDC’s research program.
A Controversial Program
If anything is a hot-button topic in ME/CFS the Centers For Disease Control’s CFS program is. From the sometimes troubling portrayal given it in Osler’s Web, to the misappropriation of ME/CFS funds in the 1990’s, to a “Toolkit” with few tools in it, to the Empirical definition with its huge and never fully explained jump in prevalence, to Dr. Reeves intemperate (although ultimately correct) remark that XMRV would not work out, the CDC has had a talent for getting itself in hot water with the ME/CFS community.
Dislike of the program can be intense. Recently participants in a heated discussion stated things like the CDC has never studied pathogens, and that the CDC has never done a single good thing for the ME/CFS community. Another person in another email exchange stated that the CDC had spent millions on CBT studies.
None of the above are true. The CDC has done more pathogen studies than any other group, it has never done a CBT study, and it has produced numerous studies that have contributed to our understanding of ME/CFS.
This is not to say that the CDC team has not made mistakes – some of them major — or done things which have contributed to unhelpful impressions of this disease – but some misunderstandings about the program clearly exist.
In an effort to assess the CDC’s impact on the research field – good and bad – this blog reviews virtually every research study that Reeves and other major figures in the CDC team have published since around 1995.
The CDC’s Research Program: A Review
Bill Reeves
It all begins with the bald one. Next to Simon Wessely, Bill Reeves has probably been the most polarizing figure in ME/CFS history.
Reeves cut a striking figure – but temperamentally may not have been best choice to lead the CFS program
Reeves, an epidemiologist, brought a strong viral background to his work at the CDC’s CFS team. From 1977 to 1989, he worked in virology and epidemiology at the Gorgas Memorial Laboratory in Panama. While there, Reeves produced the first large population study to find a link between sexually transmitted viruses and cervical cancer. From 1982 through 2005 Reeves published almost 60 studies on uterine cervical cancer. His work was later described as being fundamental in establishing the link between human papillomavirus and uterine cervical cancer.
Reeves with his bald pate, fierce glare and military manner may not have been the best choice temperamentally, to run a program for the ME/CFS community. A fairly gruff individual, Reeves was not inclined to communicate much. Despite being on the federal committee for ME/CFS (CFSAC) for years the committee gave him a no-confidence vote during his ten year review.
The first part of the blog is focused on papers on which Reeves was listed as co-author. Later sections of the blog feature other studies the CDC funded while he lead it. Finally the blog looks at Dr. Unger’s work.
Epidemiological Studies
Reeves was trained as an epidemiologist and did many large epidemiological studies. His first epidemiological study used physician referrals in four cities to collect epidemiological data on CFS patients. It found that the mean age of onset was 30 years old, 85% were women, 97% were white and average duration was almost 7 years.
Reeves second large epidemiological study screened 8,000 households in San Francisco for chronic, idiopathic (unexplained) fatigue. The study rarely found ME/CFS-like conditions in people under 18, but the study suggested it was surprisingly common in adults (2%). Reeves noted that symptom patterns in people who meet the criteria for CFS were similar to those who experienced fatigue but did not. This question – where to split off CFS cases from CFS-like cases – would come up again and again in Reeves studies.
Another 2003 population-based study underscored the need for symptom relief in the disease, with CFS patients being more likely to use pain relievers, hormones, antidepressants, benzodiazepines, gastro-intestinal, and central nervous system medications.
2004 was a hallmark year in Reeves epidemiological work with several important papers coming out. A nationwide 2004 study suggesting that 2.2 million Americans had ME/CFS (Fukuda definition) indicated ME/CFS was a common disorder affecting many. The authors noted, though, that after a more thorough examination some would not meet the criteria.
Another 2004 paper highlighting the high economic costs of the disease estimated that lost productivity due to ME/CFS accounted for $9.4 billion in economic losses a year. With only 16% of the patients the CDC identified as having ME/CFS being diagnosed, a 2004 paper indicated the urgent need for better educated doctors. This number would be used again and again to call for better physician education.
- VERDICT – Significant positive impact. Reeves epidemiological studies are still used to demonstrate that ME/CFS is a major disorder with significant unmet needs.
Pathophysiology
Pathogens
Early studies (pre-Reeves) in 1992 and 1993 failed to find evidence that HTLV or other retroviruses were present in ME/CFS. Reeves first paper on CFS reflected an initial interest in the role viruses play in the disorder. Despite testing for a “large number of infectious agents” or antibodies to a “wide range of agents including herpesviruses”, however Reeves 1995 seroepidemiological paper found no evidence of infection. That would begin a dispiriting pattern at the CDC.
Over the next four years Reeves would look for herpesviruses, bacterial agents, mycoplasma and endogenous retroviruses in ME/CFS. Neither PCR nor DNA tests found evidence of HHV6 or HHV7 in 26 CFS patients vs 52 controls. A search for an endogenous retrovirus turned up empty as well. A cell-free DNA study found no evidence of bacterial infection in 35 CFS vs 55 controls. The results of a mycoplasma study lead by Suzanne Vernon were similar.
In 2005 a small study failed to find evidence of GBC-virus in ME/CFS patients. That was it for Reeves and pathogens until th. Failure after failure would cause Reeves to swear off the pathogen search until XMRV came along – and thee CDC’s 2010 study found no evidence of it in ME/CFS patients and healthy controls.
Reeves appears to have become convinced that pathogens did play a role -but as a triggering factor – not a perpetuating one. In the mid-2000’s Reeves helped fund at least four of the seminal Dubbo studies which examined the role pathogens play in triggering ME/CFS. One of those studies indicated, probably at no surprise to Reeves by then, suggested that increased viral load was not responsible for the prolonged illness the ME/CFS patients were experiencing.
Immune System
The CDC has produced quite a few immune system studies but Reeves imprint only appeared on a few. As with the pathogen studies getting a positive outcome was not easy.
An early paper on the immune response found no or only marginal differences in a wide variety of immune factors in Reeves 1997 study. When Reeves subgrouped the patients according to onset some subtle differences emerged and Reeves proposed that disease onset should be assessed in ME/CFS studies.
In 2005 a Vernon/Reeves search for autoantibodies and antibodies to neurons failed to find significant differences between ME/CFS patients and healthy controls. Reeves and Suzanne Vernon co-authored a Dubbo study that failed to find evidence of cytokine upregulation in post-viral ME//CFS patients. (Another, however, found some evidence of altered gene expression. )
A rather uninspiring 2009 peripheral inflammation study found that inflammation was increased in CFS and CFS-like patients relative to healthy controls and was associated with reduced physical functioning in CFS, CFS-like and healthy controls.
HPA Axis
Reeves first foray into genetics in 2007 revealed multiple polymorphisms in the NR3C1 gene regulating the HPA axis. The study suggested CFS patients could be genetically prone to HPA axis instability. A 2008 study finding reduced morning salivary cortisol levels in women but not men helped to solidify the understanding that salivary cortisol is low in ME/CFS but only in the morning.
Stress
Later in his time at the CDC Reeves focused more on impacts to the stress response system. Some CDC researchers conceived the idea broad breakdowns in the bodies homeostatic mechanisms (allostatic stress) were responsible for the altered cortisol and aldosterone level found. A 2009 allostatic load paper appeared to represent a turn towards fashioning CFS as a ‘stress-disorder.
A 2010 paper – which Suzanne Vernon told me was hotly debated in the CDC CFS group – asserted that metabolic syndrome was common in ME/CFS. In 2011 Reeves found that “cumulative life stresses” were increased in ME/CFS and proposed that “stress may be an important factor in the pathophysiology of CFS”. Several studies in the Pharmacogenomics studies would find evidence of increased allostatic stress.
- VERDICT – Some positive impact. The allostatic stress studies went nowhere and gave the impression that while Reeves was fiddling around the edges of ME/CFS – looking for some grand, if somewhat vague explanation of it – other researchers were digging deeper. Reeves did some work on the immune system – and the neuronal antibodies study was years ahead of it’s time – but he doesn’t appear to have been particularly interested in it and it showed. Reeves tried hard on pathogens – you can’t begrudge him the effort – but was unsuccessful. If unusual pathogen activity does turn out to be a key factor in ME/CFS, he will, of course, have missed the boat on that one – but he will join many others in doing that.
Empirical Definition
Reeves early recognized that the Fukuda definition was problematic and initially prepared for a new definition in an organized and collaborative manner. Over several years Reeves brought together an international group ME/CFS experts to assess the issues with the Fukuda Definition and provide solutions.
ME/CFS, it appeared, was about to enter a new era of study using an improved and widely accepted new definition. Reeves then sabotaged his efforts by developing a new definition in house at the CDC. The definition used scores from patient assessment tests such as the SF-36, MFI and CDC symptom inventory to produce an “empirical” assessment of CFS-ness.

Reeves failure to produce a definition the research community would embrace left the Fukuda definition in play for another ten years.
With even Peter White publicly stating some doubts, however, the “empirical definition (ED)” was controversial from the start. A startling 6-10 time increase in prevalence sent shock waves through the ME/CFS community. That study suggested that 2.4% of the American population had “CFS” … and validated some researchers doubts about it.
Leonard Jason would subsequently several studies highlighting problems with the definition including the possibility that the definition could misdiagnose about a third of people with depression. Jason’s data mining study, however, found similarly unimpressive findings for both the ED and the Canadian Consensus Criteria. When asked to identify a new patient the ED did so correctly 68% of the time and the Canadian Consensus Criteria did so 73% of the time. The ED correctly identified 79% of already established cases correctly, while the CCC identified 87%.
Whether it wasn’t trusted or too complicated or whatever the ED flopped. Outside of the CDC it doesn’t appear to have been used by another research group. More importantly, a major opportunity to reform and strengthen the ME/CFS research field had failed. The Fukuda definition would continue to be the definition of choice for ME/CFS researchers for at least the next ten years. Not until the IOM panel convened would a group with significant clout attempt to produce a new definition.
By around 2007, Reeves studies now had two question marks against them. The fact that a significant portion of the CFS patients selected by population sampling no longer met the criteria for CFS several years later suggested he was studying a “CFS-lite” group. The advent of the ED raised further questions about what kinds of patients were showing up in CDC studies.
- VERDICT – Negative Impact. A major missed opportunity for CDC program and for the ME/CFS field itself.
Symptom Assessment
Reeves introduced two improvements to symptom assessment in ME/CFS.
A 2005 paper demonstrated Reeves attempt to broaden the symptom assessment beyond the symptoms than found in the 8-symptom Fukuda criteria. The CDC Symptom Inventory assessed the presence, frequency and intensity of 19 symptoms including diarrhea, fever, chills, sleeping problems, nausea, stomach or abdominal pain, sinus or nasal problems, shortness of breath, sensitivity to light, and depression.
Reeves continued to broaden the instruments used to assess ME/CFS with a 2009 study validating the use of the Multiple Fatigue Inventory (MFI) in the disease.
- VERDICT – Positive Impact in an important area that needed and still apparently needs help.
Symptoms and Conditions
Reeve’s studies assessing the prevalence and cause of several important symptoms/conditions met with mixed results.
In 2004 a factor analysis study found three symptom clusters – musculoskeletal, infection and cognition-mood-sleep in the disease. The clusters overlapped, however, between people who meet the criteria for ME/CFS and those who had ME/CFS-like symptoms but did not meet the criteria. That suggested that other than symptom severity there was little dividing line between the two – at least with regard to symptoms.
Sleep
A large Unger-lead study suggested that most people with ME/CFS had a least one sleep abnormality but noted that sleep studies were needed to confirm the findings. A 2006 sleep study indeed, found that 18% of the people thought to have CFS had a primary sleep disorder instead and that and rates of sleep apnea were also increased.
Similar sleep architectures between the CFS patients and the healthy controls, however, provided no clues to the sleep problems CFS patients reported. A 2007 sleep study employing population based subjects and the empirical definition also found no differences in sleep pathology or architecture in CFS patients vs control.
A 2007 population-based sleep study, however, hit pay dirt. Boneva, in a finding that would be validated by another lab, found increased heart rates and reduced heart rate variability during sleep in a population-based set of patients. Those findings along with higher norepinephrine levels and lower plasma aldosterone suggested “a state of sympathetic predominance was present” in ME/CFS.
Reeves continued to examine sleep. In 2009 he found widespread albeit modest differences in brain-wave patterns (significantly lower theta, sigma, and beta spectral power during stage 2, Slow Wave Sleep, and REM) during sleep. Among others these findings also suggested problems with the sympathetic nervous system might be important.
Other Conditions
Reeves population-based 2006 cognition study indicated that people with ME/CFS were mentally fatigued and that the mental fatigue was associated with poorer performance on cognitive tests.
A 2005 orthostatic intolerance study, however, fared poorly. It found that none of the “CFS” patients in the study exhibited orthostatic intolerance in the standing test. Thirty percent of the ME/CFS patients had postural orthostatic tachycardia syndrome on the tilt test but 50% of health controls demonstrated “orthostatic instability” as well (much of it due to neurally mediated hypotension.) Reeves concluded that some form of orthostatic intolerance was common in the population and was not a major factor in CFS.
- VERDICT – Some positive impact. Reeves seems to have pinned down a significant cause of sleep problems but his work on validating symptoms/conditions in ME/CFS in general was uninspiring and not particularly to say the least.
Behavioral Studies – the Heim-Nater Collaborations
Reeves first behavioral study did not occur until later in his stay at the CDC. Reeves would never fully abandon his efforts to understand ME/CFS on a pathophysiological level; over time, though, behavioral studies would fill out more of the CDC’s study portfolio. Reeves association with Christine Heim and Urs Nater produced a number of controversial studies that would solidify his reputation in the ME/CFS community as the prime bogeyman.
A 2006 study found more “escape avoiding behavior”; i.e. “maladaptive coping” in CFS and CFS-like patients. Reeves 2006 childhood trauma study suggested that childhood trauma was a “major risk factor” for ME/CFS. A 2009 study with similar findings suggested that low cortisol levels were associated with a tendency for childhood trauma. Because childhood trauma is associated an increased prevalence of autoimmune, inflammatory and mood disorders, the studies did in an odd way legitimize CFS as a disease, but they were done at the wrong time at the wrong place. For an ME/CFS community looking for pathophysiolgical answers they were a considerable step backwards.
A 2009 population study suggested that almost 60% of people with CFS had at least one current psychiatric diagnosis and almost 90% had been diagnosed with one in their lifetime. (When ME/CFS is so often misdiagnosed as depression one wonders what relevance a study like this has.) A 2010 study found that most people with ME/CFS (71%) did not have evidence of a personality disorder but that ME/CFS was associated with “an increased prevalence of maladaptive personality features and personality disorders”.
- VERDICT – Negative Impact: – the psychological studies did nothing to further our understanding of ME/CFS pathophysiology. While the personality study did find evidence of a personality disorder in 29% of patients – that still left over 70% of patients without one. Nor did the childhood trauma studies, except perhaps by obliquely relating ME/CFS to other inflammatory disorders with similar findings, provide any clues as to pathophysiology. The second childhood trauma study did highlight cortisol, but it’s hard to imagine that the mildly low cortisol findings found in ME/CFS are anywhere near ground zero for this disease. Except for the childhood trauma studies much of this work had already been done anyway. It was another of the CDC playing mop up.
A Complex Figure
Reeves then was a complex figure. Coming out of the human papillomavirus field, Reeves initially believed that pathogens caused ME/CFS. When that didn’t work he suspected that homeostatic mechanisms in the body had broken down. He appeared to be leaning at the end to the idea that behavioral responses to the illness were contributing to those homeostatic breakdowns.
We shall see, though, that Reeves’ funding of the open ended and exploratory Pharmacogenomics studies indicated that he was not a closed book on ME/CFS. His funding of Dubbo studies turned out to be prescient as well. Despite his turn towards the psychological at the end when Reeves was replaced he was still funding large pathophysiological studies. It’s hard to know exactly what he thought about ME/CFS.
It’s hard not to escape the conclusion that Reeves, himself, was not a particularly creative thinker or researcher. Many of his research efforts are not particularly inspiring and he devoted considerable efforts to validating (some might say invalidating) findings from other groups – as if the CDC program presented some sort of seal of approval. His tenacity with the sleep research, however, was admirable.
Reeves did do much to put ME/CFS on the map. His whistleblower testimony brought millions of dollars of funds back into the ME/CFS program and initiated the first media campaign the CDC had ever done. His epidemiological studies indicated ME/CFS was a common and costly disorder that was poorly diagnosed. He never stopped arguing the ME/CFS was a serious disorder.
He also used expensive population studies to find patients who fit a questionable definition. It could be argued that Reeves sampling strategy was backwards – he would have been more successful if he had developed a more stringent definition based on the patients in clinics first – and then applied it to the population at large. Instead his application of a vague definition to the population at large appeared to cause him to end up with a “CFS-lite” group in his studies.
Reeve’s development of the Empirical Definition could almost be described as tragic. Seemingly just steps away from developing a definition that would be embraced by the ME/CFS community -and take over for the much maligned Fukuda definition – Reeves turned inward and developed a definition that was never embraced. An major opportunity to move the entire ME/CFS field forward was lost.
That’s not the end of the Reeves story, though. Reeves also funded significant numbers of pathophysiological studies and allowed another member of his team focused on pathophysiology, Suzanne Vernon, to do much work
Back to Biology – Vernon and Unger Studies
An examination of Reeves legacy is not complete until we examine the work of Suzanne Vernon, a researcher Reeves brought onto the team from his human papillomavirus work. With her intense interest in complex statistical analyses, gene expression and the immune system, Vernon brought a different slant to the CDC’s work, and Reeves does not appear as a co-author on many of her studies.
As was noted earlier Vernon was the lead author (and Reeves was a co-author) of studies looking for mycoplasma, bacterial DNA, neuronal antibodies, glucocorticoid polymorphisms and molecular profiling.

Part of Reeves legacy involves Suzanne Vernon a creative research focused on the pathophysiology of ME/CFS.
A pre-Reeves study (senior author Jones) had found evidence of complement activation in the blood during exercise in 2003. Vernon’s first “solo” (non-Reeves) effort in 2005 examined the effects of exercise as well. It found greatly increased activity of ion transport and ion channel genes after exercise – two subjects that are of great interest today in pain and fatiguing diseases. A 2009 exercise study found enzymatic abnormalities that could account for the complement upregulation in ME/CFS during exercise.
In 2007 Vernon built a model which showed how the HPA axis might flip into an alternate suboptimum stat similar to that found in ME/CFS. In 2008 she and Broderick introduced neuroimmune network modeling to ME/CFS. In 2009 she and Broderick produced a model demonstrating how a period of short-term cortisol depletion could help reset the HPA axis. The Nova Southeastern team under Broderick would greatly expand on these types of models.
A 2008 CDC study suggested that polymorphisms concentrated on one serotonin receptor gene could play a role in ME/CFS. In 2008 Vernon also co-authored a study combining gene expression and gene polymorphism data in ME/CFS.
A 2009 study using the empirical definition was the first to identify B-cell abnormalities in ME/CFS. It suggested a B-cell dysfunction might be producing persistent inflammation and altering NK and T cell activity. Another 2009 study suggested that polymorphisms in complement genes could be contributing to the complement activation seen during exercise in an earlier study.
Vernon’s first attempt at integrating large amounts of disparate data (gene expression, clinical and epidemiological data) suggested that fundamental metabolic perturbations might be present in ME/CFS.
Besides her ME/CFS work Vernon did substantial work while at the CDC improving methodological procedures associated with gene expression and mass spectrometry. They included work on micoarrays, improving mass spectrometry data, optimizing assays, improving mass spectrometry (again), assessing gene expression kits, assessing gene expression effectiveness (7 studies).
The Pharmacogenomics studies would be her chief legacy, however.
The Pharmacogenomics Studies
The almost $13 million swiped from the CDC’s CFS program was returned to it over several years in the early to mid-2,000’s. A significant amount of that money appears to have gone to a novel Vernon lead effort that came to be called the Pharmacogenomic’s studies.
These studies represented a creative effort to redefine and understand ME/CFS. They were amongst the first studies in any disease to use advanced statistical techniques to simultaneously assess huge data sets of epidemiologic, clinical and laboratory data. They included ME/CFS researchers outside the CDC such as Nancy Klimas, Vollmer-Conna, White and Broderick and brought in other researchers from statistical fields.
In 2006 the studies filled an entire issue of the Pharmacogenomics Journal and prompted the head of the CDC to publicly assert in a National Press Club meeting that CFS was a real disorder.

Reeves ended much of his support for pharmacogenomics type work but it lives on in Nancy Klima’s Institute
Among others the project produced classes of ME/CFS patients using gene expression data, identified gene polymorphisms associated with those classes and associated the expression of certain genes with specifc fatigue measures. One study combining symptom and fatigue measures with gene expression data suggested that oxidative stress, immune system dysfunction and potassium imbalance were associated with impaired sympatho-vagal balance (low HRV) in ME/CFS. Another study using a complex set of variables identified 24 genes governing immune response, apoptosis, ion channel activity, cell growth and neuronal activity in ME/CFS. Several other studies focused on allostatic load denoted by increased waist:hip ratio, low cortisol and aldosterone levels.
One intriguing study found that polymorphisms in just five genes (neuronal tryptophan hydroxylase (TPH2), catechol-O-methyltransferase (COMT) and nuclear receptor subfamily 3, group C, member 1 glucocorticoid receptor (NR3C1)) allowed investigators to accurate predict who had or did not have ME/CFS.
It was a promising start, but Reeves axed most of the further pharmacogenomics studies. The effort would live on in two places, though: Broderick would use similar methods to form the core of Dr. Klimas’s research program and Unger would retain some investigators from this period.
- VERDICT – Significant positive impact. Vernon picked on the exercise findings in ME/CFS and expanded them and she was successful in doing that. She was the first person to find B-cell abnormalities in ME/CFS. and the first to use sophisticated statistical techniques to analyze large amounts of data. The Pharmacogenomics project laid the basis for one of the more successful endeavors in ME/CFS research – Klimas/Broderick work at NSU in ME/CFS and GWS. This line of research is one of the few that the federal government appears to have consistently funded.
Dr. Elizabeth Unger Takes Over
After Reeves unexpected sacking (he had recently survived a ten-year overview of the program) Dr. Unger took over as CFS program director in 2011. Her concentration in ME/CFS prior to taking over was almost wholly biological. She, like Vernon, also tended to work on technical methodological studies focused on gene expression technology. She was rarely listed, however, as the lead or senior author on her ME/CFS studies.
She had, however, co-authored hundreds of papers on the human papillomavirus and was not uncommonly the senior author listed. (Note that the major players of the CDC CFS research team – Reeves, Vernon and Unger – came out of the papillomavirus field.)
Unger has now been directing the CDC’s CFS program for four years. The CDC’s pace of publication has slowed since Unger took over, possibly because she’s been devoting so much time to the large and data–rich multi-site studies. Since taking over as head of the program she has co-authored ten papers, three of which probably began during Reeves term.
Unger’s Studies
An early menopause and other gynecologic risk factors study using the empirical definition found, as did an earlier CDC study using the Fukuda definition, very high levels of gynecological disorders either preceding or following ME/CFS.
A basal ganglia study (Decreased basal ganglia activation in subjects with chronic fatigue syndrome“) piggybacked on Andrew Miller’s intriguing findings that hepatitis patients given interferon – a powerful immune agent – came down with similar symptoms as people with ME/CFS. The study found evidence of basal ganglia dysfunction and reduced dopamine activity. Miller suggested those factors could result in central nervous system hypersensitivity to inflammation. Miller’s finding suggested hat inflammation plays a strong role in ME/CFS.
Unger was the senior author of the first ME/CFS paper to comprehensively assess single nucleotide polymorphisms (genetic variants) in immune and inflammatory genes. Remarkably, the study singled out polymorphisms in the complement system – the same part of the immune system that two earlier CDC exercise studies had highlighted. This is the first time I am aware of that one immune factor has been highlighted in gene expression, the blood and genetic ME/CFS studies.
A complex study attempting to get at the cause of the natural killer cell dysfunction in ME/CFS examined the effects of acute stress on the epigenetic expression of a gene associated with perforin. Perforin plays a key role in natural killer cells ability to kill infected cells. The study had somewhat mixed results but did suggest that increased methylation could be altering perforin gene expression and thus contribute to the NK cell problems found in ME/CFS.
In 2011 Unger co-authored a study integrating single nucleotide polymorphism and gene expression results in ME/CFS. The study found two genes, a glutamate regulating gene and a neuronal gene, which displayed both altered gene expression and unusual gene variants. Unger also produced a 2011 paper suggesting that a serotonin receptor polymorphism plays a role in altered methylation processes and ultimately serotonin receptor activity in ME/CFS.
Under Dr. Unger, the CDC is the first group, as well, to finally provide an objective assessment of Dr. Chia’s findings. They are current analyzing samples from Dr. Chia’s enteroviruses.
Unger also co-authored two review papers: one on current and emerging biomarkers and one on the minimum data elements needed for research studies in ME/CFS and two methodology papers (Multiscale analysis of heart rate variability in non-stationary environments, Identification of Phosphoglycerate Kinase 1 (PGK1) as a reference gene for quantitative gene expression as well as a study producing a pilot registry.
VERDICT – Positive Impact – Unger at this point may have the highest success rate of any of the major CDC researchers. The gynecological studies produced startling evidence that high rates of gynecological disorders are present in ME/CFS – something Broderick’s models suggest might happen. The basal ganglia study, in fascinating fashion, pointed a finger straight at the immune system and the brain. While Unger’s attempt at explaining the NK cell problems in ME/CFS did not appear to me (a laymen in this complex topic) to be particularly successful it was a worthy effort. Her immune/inflammation polymorphism study, in what may turn out to be a major finding, highlighted the complemennt system again. Time will tell whether glutamate plays a role in this disease or not.
The most significant dig on Unger’s directorship is probably that it has not been particularly prolific. Nor has it been particularly speedy. She presented preliminary results of the first multi-site study about two years ago yet no papers have been published. Unger also continues using the ED but it’s time is surely coming as Jason’s studies bring us closer and closer to the best criteria for ME/CFS.
Conclusion
Unger charted a different path from Reeves. She stopped the stress and psychological papers and began a focus on immune factors and using the genetics and gene expression techniques the CDC team had helped to create. The gene focus continued with the CDC’c presentation at the IACFS/ME conference indicating telomerase lengths were reduced in ME/CFS and aging may be increased.
The results of Unger’s main work since she took over, though – the multi-site ME/CFS experts study – with its exercise, cognition, lactate, gene expression and salivary cortisol components – have yet to be published. The study will likely contribute to our understanding of diagnostics, comorbidity, family history, disease course and treatment effectiveness. Phase II of the study is examining large numbers of severely ill patients and pediatric patients.
Achievements of the CDC’s CFS Research Team
Contrary to popular opinion the CDC’s research team has contributed to our understanding of ME/CFS. Below are some of the ways it has done that:
Epidemiology
- Determined that ME/CFS causes severe direct yearly economic losses in the U.S.
- Determined that the vast majority of people with CFS are undiagnosed
- Produced studies indicating that ME/CFS is a relatively common disorder in the U.S.
- Produced the first pediatric prevalence study in the U.S.
- Identified that the highest rates and chances for remission occur in the first two years of the disease
Symptom Assessment
- The CDC’s Symptom Inventory increased the number of symptoms assessed in CFS evaluations and added frequency and severity measures
- the CDC’s Multi-Fatigue Inventory presented an improved symptom assessment instrument
Pathogens and Immune System
- Found no evidence of pathogen persistence in ten studies over two plus decades
- Provided funding for the seminal Dubbo studies that identified infections are common triggers of ME/CFS and that symptom severity and cytokine upregulation early in the infection are key factors. (Reeves, Vernon were co–authors on several papers)
- Produced four studies suggesting that complement activation may play a factor in the ME/CFS – particularly during exercise in ME/CFS
- Produced the first gene expression study to find B-cell abnormalities in the blood
- Several Pharmacogenomics studies pointed to possible immune system abnormalities
Symptoms and Conditions
- Identified, in two studies, abnormally high rates of gynecological disorders in women with ME/CFS
- Identified that as many as 25% of people meeting the criteria for ME/CFS may instead have a primary, untreated sleep disorder that would show up in a sleep study.
- Identified sleep apnea as a common and undiagnosed cause of fatigue in ME/CFS patients
- Produced the first study to indicate that reduced heart rate variability (i.e. sympathetic nervous system dysfunction) played a key role in the poor sleep seen in ME/CFS. That finding was later validated.
- Found that ME/CFS patients were mentally fatigued and that mental fatigue was linked to reduced cognition
HPA Axis
- Identified and validated what turned out to be the core HPA axis finding in ME/CFS – low morning salivary cortisol levels
Genetics, Gene expression, Data Mining and Modeling
- Produced the first neuroimmune network modeling study in ME/CFS. (The study suggested inflammation and thyroid dysfunction are present in ME/CFS.) Network modeling has played a major role in Dr. Klimas’s later work.
- Produced the first model of HPA axis instability suggesting how HPA axis problems occurred in ME/CFS and how the axis might be reset.
- Produced the first study combining genetic and gene expression data in ME/CFS
- In 2006 CDC studies filled an entire issue of the Pharmacogenomics Journal. Upon publication of the journal the head of the CDC announced in a National Press Club event that CFS was a real disorder.
- Pharmacogenomic studies identified immune, ion channel, oxidative stress factors that remain pertinent in today’s research
- Produced a dual gene polymorphism/gene expression study suggesting abnormal glutamergic neurotransmission may be occurring in ME/CFS.
- Demonstrated that abnormal methylation of perforin genes may be occurring in ME/CFS
- Found that reduced telomerase lengths in ME/CFS suggest more rapid aging
Brain
- Produced a study demonstrating that people with ME/CFS have similar basal ganglia dysfunction and symptoms as hepatitis patients given a strong pro-inflammatory drug. This finding strongly suggested that inflammation plays a major role in ME/CFS.
Others
- Reeves introduced Suzanne Vernon to the ME/CFS field. Vernon went on to successfully revamp the Solve ME/CFS Initiative’s research effort, build the Biobank and introduce many new researchers to the field. Reeves also introduced Elizabeth Unger who has refocused the CDC’s CFS program on pathophysiology to the field. The Pharmacogenomics efforts also appear to have introduced Gordon Broderick to the field.
An Assessment
The CDC did produce numerous accomplishments over the course of its 15 or so years of work. Did it produce enough? I would suggest that the program has underperformed.
Reeves may have been an excellent epidemiologist but except for his work with Suzanne Vernon he does not appear to have been a creative thinker. The CDC did lead in some areas. The expensive population studies, for instance, suggested there was little qualitative difference between CFS and CFS-like patients. No group, however, has shown interest in furthering that line of research.
Reeves singular contribution – the attempt to quantify CFS patients more accurately using SF-36, MFI and symptom scores in the Empirical Definition – failed to attract interest. Reeve’s development of the ED ultimately isolated the CDC and put it on a confusing course. Reeves attempt to validate others findings also often ended with sometimes disastrous (orthostatic intolerance) mixed (sleep) or muted results (cognition).
Contrary to popular belief, however, Reeves CDC program did focus heavily on biological issues. Only six of the sixty plus studies Reeves funded focused on psychological or behavioral studies. The psych studies may have gotten the lion’s share of attention but the vast majority of funding at the CDC went to other types of projects – and at times significant progress was made.
Reeves most positive influences may have occurred in three areas – two of which he had little to do with. His epidemiological work helped to validate the high economic costs due to and the low diagnostic rates present in ME/CFS. The Pharmacogenomics projects birthed the work that Dr. Klimas is doing at NSU, and the Dubbo studies validated and expanded our knowledge of the pathogenic triggers present in ME/CFS.
If the CDC’s research program has not lived up to its promise there’s no doubt, however, that it has moved our understanding of ME/CFS forward in multiple ways. If that’s so why is the CDC not just disliked by hated by a portion of the ME/CFS community. Why are it’s accomplishments almost completely unacknowledged?
A Pattern High Profile Failures / Low Profile Successes
I suggest that a pattern of high profile failures and low profile successes have been partly to blame

The successes the CDC has had have not been significant enough to erase the high profile mistakes it’s made.
The CDC has been notable in it’s ability to produce high-profile failures that have stuck in the ME/CFS communities mind. It’s successes, on the hand, have mostly been incremental, tend to involve complex studies that are difficult to understand and explain, and are mostly low profile. It has not produced the kind of breakthrough success that would give the public cause to reassess its opinion.
Studies indicate that negative rather than positive impressions tend to stick in our mind and the CDC has a long history of high profile negative events which have stuck.
- The negative stories about the CDC that came out Hilary Johnson’s Osler’s Web stuck. The positive aspects of the CDC’s response to ME/CFS – that fact that it did a 180 degree turn when it appeared the De Freitas findings might turn out – did not stick.
- The misappropriation of $13 million from the CDC’s CFS research program in the late 1990’s stuck. Less well-remembered is the CDC’s response: the return of the money plus the first multi-year media campaign ever done by the CDC.
- The finding that the Empirical Definition increased prevalence rates by 6-10’s and may select depressed patients stuck. Jason’s finding that the ED was not that much less accurate than the CCC in defining new patients correctly did not stick. Nor has the pattern of positive results in pathophysiological studies using the ED been noticed much.
- The few psychological studies (psychiatric diagnoses, childhood trauma, etc.) Reeves funded really stuck. The many more pathophysiological study Reeves and now Unger have funded haven’t stuck.
- The problems with the CDC Toolkit stuck. Dr. Unger’s removal of the Toolkit from the site and her efforts using CFSAC members to improve the website have not stuck. The CDC’s extensive use of ME/CFS experts to produce training materials for physicians appears not to have stuck much in the minds of the general ME/CFS community, either.
The Sin of Failure
The CDC has also committed the sin of failure; i.e., the failure to get positive results in areas the ME/CFS community dearly wanted positive results. The chief example is the CDC’s pathogen studies. Between 1992 and 2010 ten CDC studies failed to find any evidence of pathogens in ME/CFS. Reeves was surely correct to say that the CDC had funded more pathogen studies in ME/CFS than any other group. They also, however, failed to find pathogens more times than any other group.
The CDC, of course, has not been alone in difficulties in finding pathogens. The failure of the huge recent Lipkin/Hornig pathogen and the Blood Safety Research Institute studies demonstrate the difficulty in finding pathogens in this disease. The search is not over; it may be that ME/CFS patients have an atypical form of infection. Should the CDC have looked for those types of infections? Perhaps, but those kinds of infection are controversial and the decision to stop looking for pathogens was not an unreasonable one.
A Tough Act To Follow
Dr. Unger took over a program with enormous baggage. Reeves is associated with most of the factors the ME/CFS community finds disturbing about the program. Unger, whose work was mostly focused on pathophysiology, was not.
Unger is still using the ED, however; she has not acknowledged that PEM is the core symptom in ME/CFS (but is doing exercise studies), and the CDC’s website — which relies mostly on evidence based studies – still a source of concern to some.

Conclusion: with more upside to the CDC’s CFS program than ever before, it would be a shame to lose it now.
Still, Unger ditched the stress and psychological studies. She began a huge multi-site ME/CFS experts study which could have major ramifications for understanding of how to diagnose ME/CFS, what subsets are present in it and our understanding of disease course, comorbidity and how to treat it. Besides furthering our understanding of the severely ill, the protrayal of the severely ill that will result from the second phase of the study will surely heighten the consciousness about the potential severity of this disease.
Unger’s study slate is entirely pathophysiological. She’s funded gene expression, immune, natural killer cell, gynecological, blood lactate, cognition and telomere studies. She’s incorporated acute stressors such as exercise into her studies. She’s communicated with ME/CFS support organizations. She’s worked with CFSAC members to improve the website. For some in the ME/CFS community, however, it’s still the same CDC: for them few of Unger’s efforts have “stuck”.
This review has covered only the research portion of the CDC. It suggests that while the CDC is not god’s gift to the ME/CFS community neither is it necessarily the bogey man many have made it out to be.
It also suggests that Unger has dramatically changed the CDC’s direction. It suggests Unger’s program is moving in the right direction. Unger’s outreach to the ME/CFS community, her now strong collaborations with ME/CFS experts, and her pathophysiological focus suggest that the best of the CDC’s CFS research program is ahead of us. This is not a program we want to lose.











This will take me a while for me to read, and I mean a while. But it is evident to me more than ever, you know what is going on in the research community and you are very good at writing about it in a very organized manner.
I also like the fact you are a positive blogger. As a community we need bloggers and advocates to remain positive no matter what happens. And when there is something bad, writing about that without bringing us further down is a gift. If there is no good to be found you can point that out but reading something written in a non positive manner is not helpful. Giving us a path or an action to follow is positive which you did immediately with the writing campaign.
And I personally feel after skimming your article especially the end that there is a lot to be positive about.
Thanks Sue 🙂
Wow, yes an impressive piece of work! I second “Sue’s” comments. MC
Thanks Maggie 🙂
‘undiagnosed’ Ehlers Danlos Syndrome type(s) that has already been proven ME/CFS will no longer be used ‘get used to that fact’ EDS with it numerous Spine Brain issues involving all organs
a Genetic Born mutation of ‘Collagen’ skin bones also involved in fact some also have ‘partial incomplete’ Marfans Syndrome or some do not have EDS they have ‘full’ Marfans
Syndrome…ME/CFS died it will no longer be used we will also see Lyme b.s. fade away like XMRV…
EDS also comes with MCAD Mast Cell Activation Disorder plus small percentage will have CVID or Primary Immune Deficiency…There are numerous types of EDS the Hypermobility type has no
blood test the Vascular type is the more serious one all are Chronic…
Thanks for putting this together Cort.
I think what is most disappointing to me is the failure of all of this work to translate into anything helpful for us as patients. It has not helped change friends, family, or the general public’s perception of the disease, it hasn’t helped the medical profession’s understanding or ability to recognize the disease, and it hasn’t helped the government realize the seriousness and huge need for funding for research. I realize that the CDC has in the past and is still presently making efforts to address the former two, but again the results just aren’t there yet and it’s devastating.
I think the program has helped in each of those areas but obviously not enough. I think, for instance, that physicians do know more ME/CFS in general. I know we get better and more media coverage. Of course we still have a long way to go and we’ve actually backwards on funding – witness the subcommittee shenanigans.
Then again, as research programs go – and the CDC program is also tasked with physician education and epidemiology – it does not have a big budget – and I don’t think it’s been particularly successful in any case as whole. I imagine that if the program is struggling to survive – it has little chance at this point of having a significantly increased budget. The only way to do that may be to produce a startling finding – which doesn’t happen all that often.
I agree that the CDC program has not realized one of it’s primary missions which is to galvanize the field with findings that bring it more recognition and move it forward as a research topic. The Pharmacogenomics project did that temporarily but that faded – as everything has faded.
I do wonder what impact the multi-site studies will have. Will they bring more recognition to the field and funding? Time will tell.
Hopefully the CDC won’t go back to using the (so-called) empirical definition (Reeves et al., 2005) for new studies (though it is still publishing papers on old data collected using the “empirical” definition).
Note a petition was created on the issue in 2009 which has over 2600 signatures. People can still sign if so inclined at:
http://www.ipetitions.com/petition/empirical_defn_and_cfs_research
My guess is that the CDC – for reasons they’ve really never explained – will continue using the ED until a new definition is agreed upon. It may be that for all it’s issues they feel it’s better than Fukuda. I would love to find out why the prevalence figures didn’t scare them enough to retweak the ED. I may try and find out.
Thanks for this overview, Cort, which must have taken a lot of work.
You won’t be surprised that I’m not convinced the data mining study’s findings (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3228898/) regarding the empirical criteria and Canadian criteria are quite as interesting as you make out
Extract 1:
Leonard Jason would subsequently several studies highlighting problems with the definition including the possibility that the definition could misdiagnose about a third of people with depression. Jason’s data mining study, however, found similarly unimpressive findings for both the ED and the Canadian Consensus Criteria. When asked to identify a new patient the ED did so correctly 68% of the time and the Canadian Consensus Criteria did so 73% of the time. The ED correctly identified 79% of already established cases correctly, while the CCC identified 87%.
—
Extract 2:
The finding that the Empirical Definition increased prevalence rates by 6-10’s and may select depressed patients stuck. Jason’s finding that the ED was not that much less accurate than the CCC in defining new patients correctly did not stick. Nor has the pattern of positive results in pathophysiological studies using the ED been noticed much.
—
Here’s the discussion section from the paper itself:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3228898/
Discussion
The study’s overall findings were that the Reeves et al. (2005) criteria were not as capable of identifying cases from non-cases as the Canadian criteria (Carruthers et al., 2003). As mentioned in the introduction, the Reeves criteria have been criticized as being more general and broader than the Fukuda et al. (1994) criteria, and the results of this study suggest that these criteria are only able to discriminate 79% of cases from others, whereas the Canadian criteria were able to 87% of cases. Also, the Canadian criteria appears to generalize better to new cases. In addition, when examining the items selected in both analyses, it is apparent that the Canadian criteria appear to select cardinal and central features of the illness.
ME/CFS is often thought to include post-exertional malaise and neurocognitive disorders, and both did emerge as predictive factors in the Canadian criteria, but not within the Reeves et al. (2005) empiric case criteria. In addition, sleeping disorders and pain symptoms, other key symptoms of ME/CFS did emerge from the Canadian criteria. Even within the other category of the Canadian criteria, two symptoms emerged in the immune areas (i.e., sore throat and multiple chemical sensitivities), and this supports evidence for the Canadian criteria. In contrast, the empiric criteria tended to identify more general areas, including less activity, social and role functioning problems, and some pain issues. However, critical symptoms such as post-exertional malaise, neurocognitive symptoms and sleep disorders were not identified as discriminating symptoms.
Data mining may be a useful tool in aiding in the diagnosis of ME/CFS. There are many challenges in diagnosing ME/CFS because it is a very heterogenous disease, some symptoms associated with it are common of other illnesses, and, as we have outlined, there are competing definitions that investigators may use. More work with data mining in ME/CFS research could aid in further identification of cardinal symptoms, leading to better diagnostic ability. This would also combine an objective, computer driven decision with a physician’s medically influenced decision to come up with a better and more reliable way to diagnose and treat ME/CFS. This technique has been used in other medical diagnoses, like breast cancer. Kuo et al. (2001) found that using data mining with decision trees in diagnosing malignant breast tumors increased diagnostic accuracy to 95% from just 87% with a physician alone.
There were several limitations in the study. The sample size was relatively small, and there clearly is need to replicate this study with larger samples. In addition, the Fukuda et al. (1994) criteria were used to select cases, and this might have biased the study toward having the empiric case definition do better, as it is based upon the Fukuda et al. criteria. However, this was not the case as the Canadian criteria was better able to classify cases and non-cases. There were more items in the Canadian criteria than the empiric case definition, but if we were to compare the two sets of criteria, we needed to use what is specified in both criteria, and to select fewer items for the Canadian criteria would have not been a fair test of these criteria. Note further that despite the disparity in the number of features, both definitions produced the same number of significant items.
In conclusion, the present study examined items that could discriminate two criteria for identifying cases versus non-cases. The Canadian criteria appeared to have a better risk statistic, and this indicates that it was better able to separate cases from non-cases than the empiric case definition. In addition, when examining items selected, the Canadian criteria appeared to have more items that are central to a ME/CFS case definition, and this provides some construct validity to this criteria.
The central fact for me is that neither test did particularly well and while the CCC did better than the ED it didn’t do that much better. I may not be understanding this correctly but the fact that the CCC tended to select out more symptoms associated with ME/CFS than the ED is secondary to the fact that when the two were asked to select of a group of new patients which ones had ME/CFS the ED selected out the new patients only 5% less accurately than the CCC.
I am not arguing for the ED as the definition for ME/CFS. I am suggesting though that it has not turned out to be the bogeyman many people thought it would be or feel that it is. One of the reasons I feel that way is that the results of the pathophysiological studies the CDC has done using it have generally fallen in line with what we know about ME/CFS.
Great work Cort – thanks! I didn’t realize pathogens have been looked into so extensively. I wonder why Stanford is still focusing on them?
I was surprised as well that the CDC had done so many pathogen studies. I think our ability to find them has increased significantly since when Reeves started looking for them, though. That said, neither Lipkin nor BSRI found them. That said, they may not have done the kinds of tests needed to look for the atypical herpesvirus infections some believe characterize ME/CFS. all in all it’s a complicated field – as we know.
In regards to the pathogen research, were there good efforts put forth in looking for enteroviruses? Dr. Chia had a study a few years back that found a high percentage of PWC to have enteroviruses using gut biopsies and I’m wondering if anyone has tried to replicate his findings?
Your organizing of the long meandering history of CFS research is impressive, Cort. All the more so in consideration of the burden of having CFS. Thanks for your work.
I can’t say about a good faith efforts because I quite frankly don’t know that entails in pathogen studies. Thanks for bringing this up because I had forgotten to note in the blog that the CDC is the first group to independently assess Chia’s enterovirus findings. This year they started examining his samples for enteroviruses.
This, of course, is another indication of Dr. Unger’s openness to a variety of possibilities in ME/CFS.
Dr. Chia’s samples are being analyzed by the CDC’s Picornavirus lab, Dr. Unger made a point to specify that it was not the CFS lab dealing with this. She may not have even been aware of it had the question not been asked on the recent PCOCA call.
Probably because they haven’t been looked into as extensively as this would make you believe. Also there are numerous studies that have found associations with pathogens and it sounds like Stanford has another one in the works. Pathogens as a cause are not ruled out at this point.
I agree that they’re not ruled out.
But here’s the thing with the CDC and pathogens – it appears that they made a reasonable effort and came to conclusions that were understandable. They may not have been correct – time will tell us about that – but they were understandable. They did not ignore the possibility that pathogens could be causing ME/CFS.
Did they not dig deep enough? Possibly – time will hopefully tell us that. As we know pathogen research is very complicated.
I would think it’s not coincidental that so many folks had an infection of some sort just previous to being chronically ill.
It’s just interesting that people like Dr. Montoya, Dr. Peterson, Dr. Lerner, Dr. De Meirlier, and Dr. Chia all have no trouble finding significant levels of various pathogens in their patients. Why has the CDC found nothing? The only reason I can think of is cohort. These expert clinicians know the disease when they see it. Who are these people that the CDC is testing? Do they really even have the disease?
Actually Chia had trouble finding evidence of enteroviruses in the blood; he was able to do it but it was not easy and he switched to stomach samples. The cohort the CDC has used is a possibility. Most the studies done were done earlier in the program when Reeves was using samples from clinicians, though. Still you never know. Of course, Lipkin and BSRI had cohorts straight from the ME/CFS experts including Montoya and Peterson and didn’t find evidence. I believe he is relooking though. It certainly is very confusing – I agree with that…
It’ll be interesting to see what Dr. Montoya comes up with.
Yes Chia had trouble using PCR but elevated antibodies are readily detectable. The British also had no trouble findings these (IgM antibodies even) as well as enteroviral VP1 in the blood and RNA in the muscle. Lipkin was only looking at plasma so much could have been missed. As Dr. Chia has shown, the viruses are in the tissue not the blood, so this renders the CDC and all other blood based research findings moot. Poor methodology has plagued the viral research in this disease for years.
Given that Montoya is bringing a gastroenterologist onto his team to collect GI biopsies I’m going to guess they’re looking for enteric pathogens.
Wow! What a comprehensive overview of the CDC’s work, Cort. Kudos on your hard work and for sharing it with us and the world.
I, for one, would love it if you can find the time to
“find out why the prevalence figures didn’t scare them (CDC) enough to retweak the ED.”
Thanks again for your amazing work on our behalf.
I will try…One of Unger’s failures actually in my opinion has been that she’s hasn’t at least so far as I am aware – is that she hasn’t explained why the CDC continues with the ED and why we shouldn’t all be freaked out by the prevalence figures.
Excellent & comprehensive analysis of “the state of the CDC”! Your assessment of the failures that “stuck” & the successes that did not “stick” rings true.
It’s a lot to take in. Two of the questions that popped for me:
(1) what is the backstory on why Reeves stopped collaborating with ME researchers & created his own definition instead?
(2) Why do the CDC studies say that 25% of patients have sleep apnea INSTEAD of CFS — what do you think about those with BOTH?
(Also, The 2006 abstract says those CFS patients found to have sleep apnea were excluded, but that they did not have significantly higher apnea events than the controls.)
I have no idea why Reeves stopped collaborating with the “International CFS Group”. I would love to find out. If he had he surely would have produced a definition that would have found consensus and been picked up..
I remember Lenny Jason saying that he was astounded when Reeves came up with the definition on his own…
Interesting about the CFS patients and sleep apnea. Did they find sleep apnea in the CFS-like group and then automatically exclude them from the CFS group?
Re: the sleep apnea exclusion from CDC study — Was it you who recently wrote about Dr. Jason’s comment that it is an unappreciated complex undertaking to decide which conditions are comorbid & which are exclusionary?
Yes, he wrote that in a study somewhere.
Hi, Cort, it is awesome. Much more appreciated! This is my first time to learn that pathogens have been investigated so broadly!
Wow, the research that has gone into this blog – I’m impressed! Thank you, Cort.
Great article Cort! One quibble… could you stop using the “perfectly made-up white woman looking tired” photos? I know you don’t usually use them, I was sort of surprised to see them here.
They are pretty much what is available to me actually. I buy my images online. What would you rather see?
There’s a site https://www.flickr.com/groups/meaction/pool/ that has a handful of representative photos taken by/of actual PWME . They really need more contributions, though. I’d love to see it take off.
Cort, thank you so much for expending the time and energy it must have taken you to produce this impressive background of information for us. You continue to be a treasure to the ME/CFS community and we are fortunate to have someone with your talent who is willing to keep us informed and encouraged despite your own struggles with this illness.
It was good to be reminded that the CDC has had some positive impact in altering the public perception and furthering the research into ME/CFS even though it has been a very bumpy ride along the way. When we only allow ourselves to focus on the negative aspects and don’t include the positive aspects, we become jaded with little hope for future progress. You have managed, yet again, to give us a more balanced picture so I, for one, can re-examine my “etched-in-stone” attitude about the CDC. As a participant in the multi-site CDC study, I’d much prefer feeling that something good will result from giving my time, energy, blood, etc., instead of feeling somewhat disappointed that it’s for the CDC!
🙂 Thanks Pat. It was fun project actually. It was good to recheck my sense of the CDC as well.
I was looking forward to a balance coverage of the good and the bad. I see the good. As for the bad, you gloss over it. The CDC stole CFS money. You say they paid it back. That doesn’t make it okay to steal. Not to mention that it took Congressional action to get them to pay it back.
You say they never did a CBT study. I agree. So then why did Unger defend the cherry-picked coverage on their website as simply being a reflection of their own research, when in fact most or all of their treatment recommendation do not stem from their research.
And as for the large educational program, I think quantity is not the only factor. I think quality should count for something too. I obtained their educational packet and it was worse then nothing. It was not much more than a reflection of their website, including treatment information based on fatigue-only studies. This is in the same doctor toolkit the CFSAC decided was so bad they recommended it be completely removed.
And I have other examples, but my point here is not to document CDC wrongdoings. My point it’s all well and good to list the positives they have done, but it helps nobody to spin the CDC’s harmful actions so they seem benign.
Where did I say it was OK to steal Andrew? I said the fact that the CDC paid the money paid and added a media campaign on top of it went mostly unnoticed.
As to your second sentence I can hardly understand what it says. I believe the CDC focused on CBT/GET in their toolkit because they only allowed evidence based studies to make it into their toolkit. The fact that Unger is now studying treatment outcomes in ME/CFS patients treated by ME/CFS experts might relieve your mind a bit about the CDC’s focus on CBT.
I take it you have not seen the video’s with Dr. Bateman, Dr. Lapp, Dr. Komaroff and others?
You are correct. You didn’t say it’s okay to steal. On the other hand, you were giving examples of “high profile failures and low profile successes.” And then you put the pay back into the low profile category. This leads the reader to assume it is one of the low-profile successes, rather than Congress forcing them to do the right thing.
I agree with Tom Kindlon’s take on Jason’s comments about studies using the 2005 empirical case definition. As the 2015 IOM reported, the “broad empirical definition… resulted in a biased sample with overrepresentation of individuals with depression and posttraumatic stress disorder.”
Given that overrepresentation, the lack of a requirement for hallmark criteria, and the resultant dramatic increase in prevalence, I believe the relevance of the findings of all these empirical studies – regardless of whether the findings are seen as positive or negative – need to be questioned.
As you noted, a number of the studies you discussed were Empirical studies. But what disease or diseases were actually assessed in these studies? What relevance does the empirical patient cohort have to patients with the neuroimmune disease described by CCC and ME-ICC and seen in the practices of disease experts in the U.S. or internationally. There is no way to know what diseases were studied because the empirical definition is so expansive. But I think it’s fair to say that an empirical cohort is not a good representation of the patients with this neuroimmune disease.
This is not just an academic concern or an historical problem. The findings from empirical studies muddle the research evidence base, creating confusion. These findings also negatively impact clinical care and harms today’s patients because these findings are posted on today’s CDC CFS website and in other medical education sources and articles – as is the finding that childhood abuse is a risk factor for CFS.
Regarding the Pharmacogenomics studies, it would be worth reading Jocelyn Kaiser’s May 2006 article in Science (“Genes and Chronic Fatigue: How Strong Is the Evidence?”) as not everyone was so upbeat.
Quoting the concerns of other researchers, Kaiser questioned the findings of this study because of the small sample size, and because of the “unusual” phone-survey approach used for patient selection to identify cases of CFS. She especially questioned the study’s focus on a narrow set of genes all related to stress, and CDC’s resultant finding that CFS was due to three specific genes within that narrow set of genes. As reported by Kaiser, Dr. Nancy Cox of the University of Chicago pointed out that other sets of genes might have had similar correlation – if the CDC had studied them instead.
Kaiser also reported the concerns of Dr. Jonathan Kerr (at the time at the Imperial College in London) with what he saw as a lack of robustness in the study because the technology used was not adequate to definitively state that a specific set of genes were involved. Amplifying on Kerr’s point, in testimony to CFSAC in 2009, Dr. Fred Friedberg, president of IACFS/ME quoted Kerr as stating that these studies chose to use a narrow set of genes instead of a microarray that “represented the entire human genome” and that the results were not confirmed by PCR, an approach that was necessary because microarrays are not specific. Kerr went on to state, “The findings of these papers do not lead anywhere and were not followed up by CDC. They do not provide insights into pathogenesis, nor do they indicate candidate treatment targets.”
Kaiser’s article – “Genes and Chronic Fatigue: How Strong Is the Evidence?” Science. May 2006; 312(5774): 669-671. http://dx.doi.org/10.1126/science.312.5774.669
Friedberg’s comments are here: https://wayback.archive-it.org/3919/20140324192910/http://www.hhs.gov/advcomcfs/meetings/presentations/fredfriedberg.pdf
CDC CFS Website – “Early Life Stress and Adult CFS” http://www.cdc.gov/cfs/news/features/childhood_adversity.html
I agree that this below is probably true….On the other hand I would not throw out the baby with the bathwater.
There is no way to know what diseases were studied because the empirical definition is so expansive. But I think it’s fair to say that an empirical cohort is not a good representation of the patients with this neuroimmune disease.
Kerr was asking far too much of that project – and to be honest his statements smacked of some bitterness and considerable overreach. The Pharmacogenomics projects did identify targets that are relevant today. The Pharmacogenomics project was an experimental approach; the first attempt in all of medicine apply gene expression, genetic and clinical data to a population. To expect it to use the entire genome was surely unrealistic given the enormous amounts of data that were already being assessed. To expect to go further and assess the outcomes was PCR was probably unrealistic as well. To expect the project to deliver definitive results was insane given Kerr’s own problems doing simple gene expression testing. The project was intended to show that this approach was viable and it showed that as has it’s progenitor – Dr. Klimas’s NSU program.
As for Dr. Kerr – he knows how difficult this field it. Kerr was able to break ME/CFS patients down into subsets using his gene expression data, later announced that gene expression results for the first time in ME/CFS ever had been validated – only to later find that they weren’t at all. With that he disappeared from the scene. If his rather intemperate remarks regarding the Pharmacogenomics project were any indication of how he interacted with his colleagues – maybe that was one reason he lost support.
Thank you Cort. That is an incredible piece of work. It should help focus research in a good direction for the future of chronic-fatigue-syndrome-research. After years of struggling with this disease, I’m very grateful for your help.
Thanks Kathhleen!