

The Post Infectious Syndromes Pt I
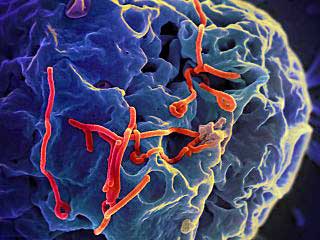
They came down with infection and never got over it. They’re experiencing fatigue, dizziness, abdominal pain, muscle and joint aches, headaches, sleep problems, weight loss and vision problems. They’re not ME/CFS or fibromyalgia patients – they’re Ebolavirus survivors – but the resemblance is uncanny.
The Ebolavirus outbreaks are prompting examinations of the virus after- effects in survivors. Given the high incidence of infectious onset in both chronic fatigue syndrome (ME/CFS) and fibromyalgia any examination of a post-infectious illness is interesting.
This blog the first of two – focuses on three of these: post-infection Ebolavirus syndrome, post-infectious mononucleosis and Giardia syndrome. It asks if the symptoms, course and possible causes of these post-infectious disorders are similar or different?
Does one central post-infectious illness exist or are there many separate ones?
Post Ebolavirus Disease Syndrome (PEDS)
A recent study published in Lancet found that two years after a 2007 outbreak survivors commonly experienced blurred vision, headaches, neurological symptoms, fatigue, sleep problems, joint pain, low mood and memory loss.
The most common persisting symptoms appear to be fatigue, joint, muscle and chest pain, and headache. Approximately 50% of Ebolavirus survivors, most of whom are or were engaged in occupations requiring manual labor, experienced severe fatigue – and difficulty working. At least four studies over time have examined Ebolavirus survivors and they have all had similar results.
The Ebolavirus survivors all look like they have one form of ME/CFS/FM – a form that is characterized, in particular, by high rates of joint pain. Some symptoms – not found in all survivors – such as hearing loss – are not commonly found in ME/CFS or FM. Problems with concentration and attention span – found in about a quarter of survivors – may also be less common than in ME/CFS and FM. Anorexia may be another symptom that is more commonly in post-EBV syndrome.
Still the general symptomology with a focus on fatigue, joint and muscle pain and headache is similar. Early studies of myalgic encepthalomyelitis found that symptoms might begin differently but they tended to devolve over time into the same symptoms: mainly fatigue, exertion problems, muscle and joint pain, etc.
What’s causing all this illness? The first disease the Ebolavirus study cites as an example of post-viral syndrome, encouragingly, is chronic fatigue syndrome. As in ME/CFS, the severity of the initial immune response may play a role in who comes down with PEBV; one study found that the Ebolavirus survivors with higher antibody titers were more likely to experience joint pain.
The author proposed several ways Ebolavirus could be causing long term problems, most of which have to do with persisting infection in the central nervous system or other areas.
- Fatigue – persisting infection produces encephalomyelitis (inflammation of the brain/spinal cord)
- Joint pain – Ebola virus replication in the joints or the deposition of immune complexes or intravascular coagulation.
- Eye problems – persisting infection
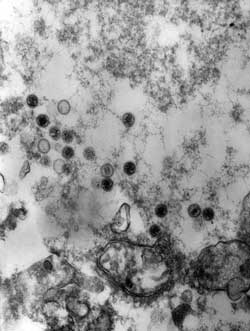
Infectious Mononucleosis (Epstein-Barr Virus)
Infectious mononucleosis (IM) is usually associated with later onset Epstein-Barr virus (EBV) infection.
IM typically presents itself in one of two ways; a sudden onset of sore throat and swollen neck due to lymph node enlargement or the slow development of malaise, muscle pain and fatigue; i.e. there is such a thing as gradual onset IM. Many of the symptoms of IM and ME/CFS are identical.
Considerable research indicates IM is a risk factor for ME/CFS. After two years approximately 5% of people with IM experience an ME/CFS-like illness.
The IM review paper missed the idea that IM is a risk factor for ME/CFS completely, but it did indicate that it is a “strong” risk factor for multiple sclerosis and non-Hodgkins lymphoma. Either individuals with IM are believed to have a predisposition to all three illnesses or their demonstrated lack of early control of the virus – manifested in their IM – result in poor later control of the virus – and the later appearance of EBV triggered MS or lymphoma.
Cause
But what causes IM associated post-infectious illnesses?
Determining how IM is causing ME/CFS, has not been easy. Katz and Jason found no evidence that many of the usual suspects (peak work capacity, activity level, orthostatic intolerance, salivary cortisol, natural killer cell number and function) believed to play a role in ME/CS, did so. They did find, however, differences in autonomic nervous system functioning, exercise efficiency (oxygen consumption, peak oxygen pulse), gender, psychological factors and cytokine networks, between those who recovered and those who did not.
The Dubbo studies found no link between viral load or cytokine levels and a post-infectious illness. Alterations in immune genes suggest an immune factor is present.
Unlike Ebola but like Giardia below, EBV infections often cause few symptoms except in individuals who are severely affected. That suggests that a genetic predisposition to coming down with IM – and perhaps lymphoma and MS – is present as well. A huge Danish study indicated that IM does indeed tend to run in families. A Simmaron Research Foundation study is beginning to examine hereditary factors in EBV infection in ME/CFS.
Genetic factors, plus alterations in autonomic nervous system functioning, plus possibly exercise problems, etc. may contribute to post infectious ME/CFS but how EBV is causing those problems is unclear.
Several hypotheses exist:
- Low level EBV reactivation is present – Lerner
- Partial EBV reactivation produces proteins that produce an immune response and possibly NK cell dysfunction – Williams (major study underway)
- EBV reactivation in localized nervous system tissues triggers an immune response via the vagus nerve- Van Elzakker (preliminary study underway)
- An initial infection alters central nervous system functioning in some way – Lloyd (neuroinflammation study underway, I believe, in 2016)
Preventing ME/CFS (and MS and Lymphoma?)
There is no approved treatment for infectious mononucleosis (IM). Why? Possibly because a recent review described it as a three week illness that rarely has severe immediate complications. It is clear, however, that IM is a risk factor for MS and lymphoma.
Two studies in 2007 and 2010 studies found that valacyclovir, described as a very safe drug, reduced EBV loads and symptoms in people with IM. Because symptom severity was strongly associated with an increased risk of coming down with ME/CFS after an infection, in the Dubbo studies, that’s a potentially very important finding. If researchers can identify individuals at risk of coming down with ME/CFS after IM, giving them a short treatment of a safe antiviral could possibly prevent decades of illness. Leonard Jason has begun a large study attempting to identify those individuals.
EBV’s association with autoimmune diseases and cancers has made it an object of considerable study. A recent review article listed three priorities for EBV research:
- The development of a vaccine in order to prevent or modify the severity of infectious mononucleosis, multiple sclerosis, EBV-positive Hodgkin lymphoma, endemic Burkitt lymphoma and nasopharyngeal carcinoma and other diseases. That work is underway.
- Define the factors that enable EBV to trigger cancer or autoimmune disease and infectious mononucleosis.
- Develop specific anti-EBV drugs to treat infectious mononucleosis.
Giardia
Halliez MCM, Buret AG. Extra-intestinal and long term consequences
of Giardia duodenalis infections. World J Gastroenterol 2013; 19(47): 8974-8985
Like infectious mononucleosis, an initial giardia infection is often asymptomatic but can in some individuals cause diarrhrea, bloating, etc. The fact that Giardia often causes no problems at all confused the medical profession for well, about three hundred years. It took three hundred years (from 1681-1981) for the medical profession to recognize that giardia can cause illness.
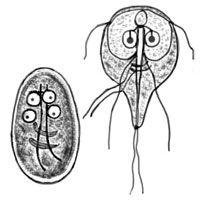
The most common parastic infection in children was not believed to cause disease for hundreds of years
Giardia is now considered to be the most common parasitic infection in children. It’s present in from 20-30% to even 100% of the population in some developing countries. (Contrast that with exposure rates in developed countries of 3-7%.) The WHO lists it as a neglected tropical disease. The infection tends to be self-limiting; i.e. the body takes care of the pathogen and moves on – but not always.
How giardia produces its most immediate effects – the diarrhea, bloating, etc. – are becoming known. The long term symptoms giardia can produce – particularly those not associated with the gut — are mostly a mystery.
Indeed, it’s only recently that these symptoms have been assessed at all. A recent study suggested, however, that Giardia infections will cause long term ‘extra-gastrointestinal symptoms” from a third to forty percent of those infected – a much higher rate than found in the Dubbo studies.
The long term results of a giardia infection can include eye problems, arthritis, allergies including milk allergies (possibly due to gut damage), muscle weakness, failure to thrive in children, malnutrition, irritable bowel syndrome, cognitive problems, extreme fatigue (ME/CFS), and long term gut problems.
Some may derive from a failure to fully eliminate the parasite but others clearly do not. The Norwegian Bergen studies, for instance, indicated that high rates of post-infectious illness can persist even after the parasite has been eliminated.
Several hypotheses have been advanced to explain the post–infectious symptoms giardia can produce
Possible Causes of Symptoms Associated with Post-infectious Giardia Syndrome
- Eye problems – toxic metabolites produced by the parasite
- Arthritis – bacterial antigens uploaded into the synovial fluid during times of increased gut permeability
- Allergies – dysfunctional intestinal barrier; i.e. increased gut permeability
- Failure to thrive – reduced nutrient absorption, malabsorption
- Chronic fatigue syndrome – altered natural killer-cell levels, lower ratio CD4:CD8
- Post-infectious irritable bowel syndrome – microscopic inflammation, gut flora alterations
An IBS Aside
Meta analyses indicate that the risk of developing IBS rises six-fold following a gastrointestinal infection and stays elevated for several years. From 7-31% of individuals with a gastrointestinal infection may develop IBS afterwards. Salmonella sp., Shigella sp., Campylobacter jejuni and Giardia duodenalis have all been shown,that can trigger irritable bowel syndrome (IBS) – even in those patients with apparently resolved infections.
As with ME/CFS more severe and longer lasting infections and being female appears to increase the risk of coming down with IBS.
Numerous mechanisms have been proposed to be at work in IBS including problems with gut motility, permeability, altered gut flora, inflammation, molecular mimicry and smooth muscle hyperactivity. All of these could be initiated by an infection.
Conclusions
The Dubbo studies indicated that a post-infectious fatigue state lasting a year or more can be expected to occur in about 10 percent of people coming down with a serious infection. That finding suggests that a considerable number of people around the world are affected by post-viral illnesses.
Post-infectious illnesses are therefore probably common but under-recognized and poorly treated. This short survey suggests that we are nowhere near close to answering whether they present common end states or distinct illnesses, or have components of both. Only the Dubbo studies, so far as I can tell, have attempted to compare post-infectious illness states caused by different infections.
Most hypotheses regarding these states revolve around the idea that either the pathogen still persists in difficult to find locations or that a continuing immune response is present. The Dubbo studies also suggested some sort of central nervous system reset occurred early in the illness.
Because Ebolavirus and EBV can affect many parts of the body, the post–infectious issues with either, could reflect localized difficult to detect infections or the remnants of the original infection in the form of antigens, or immune complexes persisting in the body.
Because giardia does not travel outside of the gut the many symptoms attributed to post-giardia infection must come about another way. Given the strong gut-brain connection, gut alterations caused by Giardia could affect central nervous system functioning.
(Williams, interestingly, is examining EBV’s possible effects on gut cells and Mady Hornig is uncovering evidence of gut induced central nervous system problems in ME/CFS.)
Since ME/CFS and FM can be triggered by many different pathogens, they could consist of distinct post-infectious states or they could, as the Dubbo studies suggested, devolve into the same general illness. The more research including comparative studies of different post-infectious illnesses is clearly needed.







Hi Cort
This is very interesting. I have a related query. Do you know of any link between Hepatitis A and ME/CFS? I had Hepatitis at age 7. I know I can trace ME symptoms back to my high school days but I can’t remember any specific symptoms from primary school days – though my general behaviour (and propensity to take time off school for what I suspect now was weariness) indicates I may have had it then. I have never had a really severe bout, and managed to keep working until I was 53. I don’t think my hepatitis was over-severe, either.
I would be interested to know if there is a link. My diagnosing doctor thought the two were related.
Diane
My bet is that an significant infection increases the risk for coming down with ME/CFS or at least experiencing increased fatigue, brain-fog, etc. A quick search found the below. It looks like we can add hepatitis A to the list – thanks for the idea 🙂
Note that liver function had returned to normal in each of the patients. This study suggests, in fact, that some viral illnesses may be more prone to cause ME/CFS than others. In the end I imagine that makes sense – which leaves the question why hepatitis would be more likely to do that…..If they could figure that out – we would have a real clue to ME/CFS.
http://www.ncbi.nlm.nih.gov/pubmed/7493307
Check this out from 1995
J Viral Hepat. 1995;2(3):133-8. Post-hepatitis syndrome revisited.
Berelowitz GJ1, Burgess AP, Thanabalasingham T, Murray-Lyon IM, Wright DJ.
To examine the role of acute hepatitis A and B infection in the aetiology of chronic fatigue syndrome and psychiatric morbidity we studied 40 patients with acute viral hepatitis A or B consecutively admitted to an infectious diseases unit and studied at least 6 months after recovery. Liver function tests (LFT) had returned to normal in each case.
Forty-seven patients with other infectious diseases, of which 12 were presumed viral, admitted immediately after each hepatitis patient during the same period acted as controls. The main outcome measures were scores on a fatigue and muscle pain questionnaire, general health questionnaire (GHQ-12) and supplementary questions.
The hepatitis cases scored significantly higher fatigue scores, GHQ-12 scores and muscle pain scores. Length of time since recovery from illness, age and sex were not confounding factors. Hepatitis cases were also less energetic, had greater weight change, had altered alcohol tolerance, had less exercise tolerance and felt less fit than the control group and compared with their premorbid state.
Hence fatigue is more common after recovery in patients hospitalized for hepatitis A and B up to 30 months post-infection compared with matched controls hospitalized for other infectious diseases. Hepatitis A and B infection is a risk factor for post-infection fatigue, intermittent fatigue, as well as for psychiatric morbidity.
PMID: 7493307 [PubMed – indexed for MEDLINE]
Thank you so much for this Cort!
I am now 64 – having been diagnosed with ME/CFS 25 years ago – and my mother and sister are just beginning to get interested in the illness and read articles and watch TV programmes. That’s encouraging. I think I will have a good talk with my mother to see what she remembers of my hepatitis. I can only remember peripheral things, nothing about the illness itself.
Hi Diane.
I too developed ME very soon after appearing to recover from Hepatitis A at the age of 20. I have been ill for 26 years now. My GP and I have always thought that the hepatitis was a trigger for my illness.
Thank you for the information Cort.
Sam
Thanks Sam. It’s good to know I’m not alone.
This is an ingenious article, Cort. If this couldn’t get the attention of the NIH, I surely don’t know what could. You bring up many considerations for a sound study hypothesis and identify a group of people who could be poster people for awareness. Think about how you can get it into the right hands. Bravo!
🙂 Thanks Celeste….A nice way to start my day 🙂
So happy to see post-infection studies being done. Can’t believe there haven’t been more as it is so prevalent. ME/CFS started for me after coming down with IM/EBV. If it indeed helps, I hope people in the future will have access to antivirals when they first get sick so that they might not develop ME/CFS going forward. How wonderful to think that the many young adults in their teens & 20s who come down with IM/EBV might have hope for a future free from disability. Fingers crossed
Another great trail to follow! I’m curious about the overlap with polio too. During all of my years of illness, my most empathic friend has a sister who came down with polio in the 1940s as a child, spent many weeks in an isolation unit in the hospital in an iron lung. She recovered her health in time and enjoyed good health for some decades–but still developed post-polio syndrome. She tells me that for years and decades doctors did not believe that such a post-polio syndrome existed, and told patients that their symptoms were all in their heads. Of course in time the science and medical practice changed, and thankfully she is treated with both compassion and actual medical treatments to manage her condition. Like so many of us, it’s the concomitant conditions like interstitial cystitis and others that are the most painful. There is no cure for polio or post-polio syndrome, but she doesn’t have to fight for the help she needs, and it’s covered by insurance. Amazing that EBV, giardia, polio, Ebola induce a post-viral syndrome that is so very similar.
thanks Cort, for another excellent & intriguing article.
two of my big relapses/downhills were EBV age 21, and suspected barmah forest virus age 33. i’m fascinated by other post-viral infections, viral reactivations, occult infections – post-polio syndrome, shingles, etc – and Van Elzaaker’s vagus nerve infection hypothesis.
i wish we could fast-forward to the answers !
Me too! I recently asked Van Elzakker if he got the vagus nerve study (or pre-study or whatever you want to call it) up and running and he has – he’s been working on it this summer.
I believe you have definitely hit on something extremely important. Hopefully, the post infection reaction can be studied and people can get treated.
Thank you!
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4051361/
Thank you, again, Cort. This is a link to a very interesting article on the possible long-term consequences of Varicella zoster, or chicken pox. Wow. Even a few years ago could we have imagined that chicken pox could produce inflammation in the cerebellum, cranial nerves, vascular system, and more. There is no history of the typical zoster rash and the CSF is normal in one third of patients. There is an average of 4.2 months delay from zoster infection to neurological symptoms and signs. The DNA of this virus is often not present in the CSF.
Don Gilden, Professor of Neurology and Microbiology, at University of Colorado, is lead author. He is an expert on viruses and the central nervous system. His special interests are:
Clinical neurology, Multiple scerlosis, acute and chronic virus infections of the nervous system, and virus latency in the nervous system.
He seems an obvious person to help sort out this situation.
Yes, we had one person in support group who had ‘typical ‘ chicken pox in her 30s, and developed classic FM/CFS/ME – never got better. Plus, my son had a lab documented Epstein-Barr infection in 1986 ( age 5 !!), but no mononucleosis. He would get better ( after months) and then relapse if he caught a cold or flu. This went on for years. The relapses were characterized initially by onset of severe and sudden urinary frequency. Has anyone else had similar experience ??
I just do not understand ( still !) why the CDC/NIH, etc. did not ‘jump’ on this whole viral causation issue back in the 1980s. As I mentioned before, there was research in the 1970s at the latest for weaponizing EBV, and for using this virus to transfer genes to the cell nucleus. Hmmm. Just don’t know.
I was really intrigued by the gradual onset possibility of IM…I had sore throat, muscle pain and fatigue and somewhat gradual – over a couple of months. I now wonder if it was EBV for me after all..
And I see that EBV (and Parvo 19 and CMV) can cause cerebral vasculitis, too. Thus, blood vessel ‘problems’ could be due to structural issues or viral infection.
Thanks for the link – another post-infectious illness!
Note: Why the price of Ampligen suddenly doubled…. being considered as (post) Ebola med.
Also, Dr. Suzanne Vernon recently met with Senator Hatch’s assistants and hopefully we will be leaving the Office of Women’s Affairs and into our own niche in the NIH where we more so belong and where money is available: NINDS. To which I say YAYYYYY. I think we are finally making some headway. Hopefully. marcie myers
I sincerely hope so! Thanks Marcie for passing that along. 🙂
Hi Cort,
http://www.biomedcentral.com/1471-2377/11/37
Thanks very much for the good work that you do on this site.
You might find the above link interesting also.
Ha! SARS – and by Moldovsky – an FM guy – THANKS!
My brother had infectious mononucleosis when we were in our early 20’s. He was 2 years older than me. I remember he had to stay in the hospital for quite a while and no one could drink after him, etc. I was pregnant at the time and had to have a very memorable shot to protect me and baby. It hurt the whole day. I was diagnosed back in 1998. I am now 63 going on 64 this month. Maybe it does run in families like you stated.
Wow, I’ve had Epstein Barr virus, mono, giardiasis, roseola (HHV6), pneumonia x 3 and chickenpox in my early 30ies and quite probably never fully recovered from any of them. My viral blood work shows active HHV6 and pneumonia but not the others.
Cort, why would the other viruses I have had not show up? When blood work is done for viral loads would all active or dormant viruses not show up? Or are only certain viruses checked?
First, only viruses checked on would show up on your lab results. Also, there are viral loads which indicate how active the virus currently is but there is also something called “titers” which would show in theory how recently you had the virus. It would be very high if recent and as time goes by and your body “forgets” to recognize it so immediately, the titers go down, down, down unless confronted with the same virus again in which case it shoots up again. A titer is a dilution and you’d have to read about it if you’re further interested. Hope this helps. marcie
Yes, thanks so much. I am (was) an RN so I do know what you’re talking about. My epstein barr virus titre indicated I was infected but a long time ago. The viral loads indicate more active HHV6 and c-pneumonia. Did I get that right? I’ll need to discuss what other viruses have been or should be checked. If indeed that’s what is causing the ME/CFS. It does make a lot of sense to me that a virus of some sort leads to ME as other viruses have been shown to cause other diseases.
Speaking of titers, my doctor checked some viral titers in November of last year. I was befuddled that my rubella IgG titer was 431 IU/mL! “Immune level” is >10. Looking at the literature, rubella titers appear to decline steadily after immunization, and I was last given MMR (measles mumps rubella vaccine) 40 years ago! I certainly don’t recall getting a rubella infection, either. Weird. Unfortunately, my EBV IgG and IgM’s were reported as merely “Positive” or “Negative” (Positive IgG, negative IgM) so I have no info on those titers.
I’ve got an appointment at OMI in November 🙂 Perhaps they will do more useful viral testing.
Hi Katie–Dr. Chia believes that the viruses are opportunistic; as my body gets on top of one pathogen, others have the opportunity to proliferate, ad infinitum. The changing scene of pathogenic dominance is responsible for how changeable our symptoms can be. Chia measured in my blood elevated levels of EBV, HHV-6, enterovirus Coxsackie B5, and echovirus, and Chlamydophila pneumonia when I got sick in 2003. I have since developed chronic HHV-3/varicella zoster/shingles which is the most problematic of all of them. He says that we often don’t find pathogens in blood because they are in the nerves; once they get to the brain they can go anywhere along nerve paths. So we can truly suffer from something that won’t show up in blood work. Drug treatments will also have a difficult time reaching nerves and the brain. In his focus on enterovirus, he has found that the pathogen can hide out in plain sight inside within cells, too. If I have this right, in one study he found that enterovirus can hide in the T-cells. How is that for opportunistic?! The very cells we need to fight these latent viruses! For me, low levels of T-cells are a big part of why I have chronic zoster, but has my body decreased T-cells in an effort to fight the enterovirus? A conundrum indeed.
Fascinating discussion. Carollynn, your blood test results remind me of my own, and my own a-ha! moment about 8-10 years ago. The first time a doctor tested for pathogens in blood (after decades of telling doctors I didn’t feel well and was tired all the time), it came back positive for Epstein-Barr Virus, cytomegalovirus, and 4 or 5 others. That was the moment I said to myself, this isn’t about any particular infection, this is about my *immune system*! And since I started going to Dr Nancy Klimas’s clinic down in the Miami area, they have been treating me to specifically support my immune system. I’m happy to say that my immune markers have gradually gotten better over time, which, even if I don’t feel well yet, they say should help lower my chances of other associated illnesses. Oh, yeah, I’ve had shingles too (HHV-3/varicella zoster), in my 30’s I think it was. Nasty experience, and it ran right along the nerves on the left side of my body. So I’m inclined to think Dr Chia is on the right track.
Thanks Carollynn for that information. It’s a mind-boggling disease. It makes a lot of sense to me that these viruses do a lot of damage to our systems, especially the nervous sys.. I constantly feel as if I’m getting over or coming down with a virus, very similar symptoms, that never goes away. Some days slightly better, some days much worse.
Cort, thanks for another interesting article. I had to laugh at the description of Infectious Mononucleosis (IM) as a “three-week illness”. I came down with it my first week at college. I was so ill my parents had to come and un-enroll me from school and take me home. I was treated by our family doctor with a stiff shot (in the behind) of gamma globulin to help my immune system, and told to otherwise go home and rest while I recovered. I slept 20 hours a day for the first month or two. Boy, was that ever weird, days passing so quickly. It took two years for me to recover enough to go back to college full-time, and even then I was sleeping every chance I got between classes. It took another two years before I felt I had fully recovered and was healthy again. Three weeks… not even close, in my case.
I would like to add Coxsackie B infection to this infectious disease causation of ME/CFS. I became seriously ill at age 27 while nursing children. Coxsackie B enterovirus was identified at the time as the agent. 37 years later and still counting.
My three sons all contracted EBV at once as teenagers and one went on to develop ME/CFS as well
Thanks Cort.
Great article, Cort! You pulled many strings together, and you make a compelling case that there are connections here that modern medicine has yet to really even consider.
Consider the theory that ME/CFS has everything to do with an immune system in overdrive, so as patients we feel like we have a chronic disabling flu there simply does not go away. Now think of all the ways that a person’s immune system might kick into high gear, causing them to have the ME/CFS symptoms of a complete “shut down”. Gulf War Syndrome — soldiers who are hyper-vigilant for months or even years who then return home only to have to resume a civilian lifestyle. Maybe their immune system just shuts the body down until it can “re-calibrate” into a normal rhythm. The same can be said for patients who experience trauma, like a car accident, who experience severe fatigue even after their injuries have healed and yet they struggle physically to get back into an active lifestyle. I am also reminded of a dear friend who had surgery, radiation and chemotherapy to treat breast cancer and while recovering she came down with an ME/CFS type of illness — the cancer was in remission and there was nothing for a doctor to treat, but she could not get out of bed. Could it be that we are seeing a patient’s immune system shut the body down for a variety of reasons, but we are only beginning to understand the mechanics of that physical “shut down”?
Dear Liz,
Well put. It’s long been my personal theory based on my readings about my own disease and progression that this is an Autonomic Nervous System that is for any variety of reason sent into overdrive that ultimately results in a meltdown/shutdown. High cortisol and then not enough. Same with several other hormones. Same with the immune response. High viral titers and other hypervigilant immuno responses followed by subnormal immuno response. From the broadest systems down to the micro operations of cellular energy in our mitochondria.
So while the concept of virus is important, I think it’s the cascade of central nervous system’s “the tiger’s chasing you” battle gone awry that is what research will ultimately be studying for medication treatments by way of immuno-modulation.
Viral meds will hold a place but in a more secondary way when old viruses break loose again via the base of the ganglion at our spinal cord and pose additional problems. I don’t believe that an antiviral medication is going to set right all in our neuro-endocrine-immune systems that have been thrown totally out of whack. Those and other hormones will be used as supportive, secondary treatment while the need for modulation of our CNS will become the primary goal.
We are finally getting somewhere here. Research funding is being increased and Centers for Excellence are opening and award-winning famous researchers are taking more and more interest as is government agencies at long last.
What is lacking is the education of current practitioners and medical students but that was seriously addressed at the last CFSAC meeting and plans made to submit educational material to various professional science magazines and annual conventions and other venues. That will ultimately be a huge step move forward as well.
Continue to support our cause in whatever and however manner possible until we are a household word. Remember that the IACFS has a treatment primer for your physician or for you to pass on at this point and there are others. I’d call this a good beginning. Count your blessings every moment. MM
Hi Cort,
thank you for this site, it’s been a life line for me ever since discovering a few yrs ago. There are autoimmune illnesses on both sides of my family. My mother was diagnosed w CFS then later w Sjogrens. When my siblings & I were young we became a joke bc we got chicken pox multiple times, well, bc everyone knows you can only get them once! ? In elementary school I was checked for food allergies (negative) bc of coming home w low grade fever, swollen/tender glands/throat & going to sleep straight away. In my teens I developed the wired/tired & struggled to keep up w others my age. But will power & an adventurous spirit drove me on. UNTIL I was in Dominican Republic in my third year of volunteer missionary work at age 23 (hiking mountains, teaching the Bible in isolated areas & constructing houses of worship: as in mixing concrete by hand, no running water & many times no electricity). I contracted Dengue Fever. It took awhile for there to be any studies done on its long term effects bc it’s not a western illness but alas! Add this one to the list as well:
http://www.ncbi.nlm.nih.gov/pubmed/17137834
Hi Cort,
thank you for this site, it’s been a life line for me ever since discovering a few yrs ago. There are autoimmune illnesses on both sides of my family. My mother was diagnosed w CFS then later w Sjogrens. When my siblings & I were young we became a joke bc we got chicken pox multiple times, well, bc everyone knows you can only get them once! ? In elementary school I was checked for food allergies (negative) bc of coming home w low grade fever, swollen/tender glands/throat & going to sleep straight away. In my teens I developed the wired/tired & struggled to keep up w others my age. But will power & an adventurous spirit drove me on. UNTIL I was in Dominican Republic in my third year of volunteer missionary work at age 23 (hiking mountains, teaching the Bible in isolated areas & constructing houses of worship: as in mixing concrete by hand, no running water & many times no electricity). I contracted Dengue Fever. It took awhile for there to be any studies done on its long term effects bc it’s not a western illness but alas! Add this one to the list as well:
http://www.ncbi.nlm.nih.gov/pubmed/17137834
Anyway it slammed me & I’ve been in a downward spiral ever since 1997, vacillating between almost housebound & bedbound: ME/CFS/FM & according to one pathologist, Sjogrens.
Thanks again & keep the info flowing!
I had EBV 25 years ago, I have a meningioma in my head 5cm I use a Rife frequency machine. Searching for answers I discovered when I use the frequency for Giardia my head got a big hit.( Bug). This tells me, I am killing what ever is up there. Asking the question, is HHV#6 the same as Giardia, I got a yes, kind of. Giardia,I do not have symptoms in the gut. Please comment if I am on the right path, I believe you are , from your article.
Hi Suzie–
Giardia is a parasite; HHV-6 is a virus. While they are not the same, they could easily have an affinity for each other, or a symbiotic relationship. I have the enterovirus Coxsackie B5 and EBV, and Dr. Chia believes that they kind of “work” together; when I am able to diminish one of the them it fosters the other. I have other pathogens at reactivated levels, too. It may be that one pathogen alone doesn’t make us so sick, but a cocktail of pathogens that together will. There isn’t one treatment that addresses both simultaneously. So it could be that Giardia and HHV-6 do the same dance.
Sorry to mix metaphors of cocktails and dancing. I wish that the holidays were full of the literal cocktails and dancing for me rather than these metaphoric ones.
Wishing all of us a healthier new year–Carollynn