

(Dr. Mady Hornig recently reported that preliminary results from the Chronic Fatigue Initiative’s microbiome study suggested a subset of people had low gut serotonin levels. She noted that serotonin is an important immune modulator, and proposed that serotonin’s precursor, tryptophan, could be being metabolized into kynurenine metabolites instead of serotonin. Kynurenine pathway activation occurs in many neuropsychological and neurodegenerative diseases. In a later discussion with a patient she suggested low serotonin levels could contribute to the “low resilience” some people with ME/CFS have towards stress.
Thanks to Darden for adding to this picture by allowing Health Rising to present this adaptation of her original blog on serotonin and fibromyalgia. Darden has fibromyalgia. Find out more about her here.)
Serotonin – An Important Part of the Fibromyalgia Picture?
Serotonin, also known as 5-hydroxytryptamine (5-HT) is an important chemical neurotransmitter found in the human body. Serotonin is manufactured in the brain and the intestines. The majority of the body’s serotonin (90%) is found in the gastrointestinal tract where it regulates intestinal movements that stimulate gut motility. The remainder is found in the central nervous system and blood platelets where it plays a role in the formation of blood clots through vasoconstriction. It is synthesized along with its metabolite 5-hydroxtryptophan (5-HTP) from the amino acid L-tryptophan.
Serotonin is popularly thought to contribute to feelings of well-being and happiness. There is no scientific evidence, however, that low levels of serotonin contribute to depression. Antidepressant medications such as selective reuptake inhibitors (SSRIs) are thought to inhibit the re-absorption or serotonin and norepinephrine neurotransmitters. This increases the levels of serotonin in the synapse of the nerves in the brain resulting in an elevation of mood. Recreational drugs such as MDMA and cocaine are also thought to inhibit the re-absorption of serotonin to create their highs. Scientists, however, are still not sure precisely how these drugs work.
Early research connected serotonin with mood disorders but more recent research has revealed that serotonin affects many parts of the body. It has been associated with pain, sleep, pain, bone density platelet aggregation, gut functioning, the immune system and others.
A recent review focusing on serotonin’s immune modulating effects suggested serotonin may be affecting immune functioning in many inflammatory diseases. Serotonin is necessary for the proper Many immune cells are littered with serotonin receptors and require it in order to respond to infections. Serotonin affects the migration, activation and cytokine production of many immune cells.
In fact, the authors asserted studies indicated that the serotonergic system is altering immune cell functioning in fibromyalgia, depression, arthritis, allergies, asthma and Alzheimer’s disease. Studies suggest low serotonin levels are present in the serum and cerebrospinal fluid of FM patients. A recent study suggested low serotonin levels may be making ME/CFS worse in some patients.
Tryptophan
It is possible to raise serotonin levels in the body by taking tryptophan and its metabolite 5-HTP. Tryptophan was taken off the market in 1984 when thousands of people developed a severe blood disorder called Eosinophilia – Myalgia Syndrome (EMS). The cause was later traced to a contaminant found in batches of tryptophan manufactured by a Japanese company.
The FDA rescinded its restriction of sales of tryptophan in 2001. Both tryptophan and 5-HTP, which is made from the seeds of an African plant Griffonia simplicifolia are readily available in stores that sell nutritional supplements and online.
5-HTP is also a precursor to melatonin, a hormone that regulates sleep-wake cycles. As a supplement it’s used to help individuals with insomnia, and is advertised to improve mood and reduce food cravings. Natural ways to increase serotonin include increasing exposure to sunlight and exercise.
An 1992 open-label and a 1992 double-blinded study suggested that tryptophan could be beneficial in fibromyalgia. Dr. Murphree is strong proponent of using 5-HTP. He reports that
” I’ve consistently found that many of the most troubling symptoms associated with fibromyalgia, poor sleep, fatigue, chronic pain, IBS, mood disorders, and “brain fog,” are diminished (sometimes dramatically) when serotonin levels are boosted and normal circadian rhythms restored.”
Because serotonin levels are already low Murphree does not believe SNRI’s will help many people with FM. Find out more on Dr. Murphree’s thoughts on 5-HTP and serotonin in fibromyalgia and his 5-HTP sleep protocol in Health Rising’s Resource section.
My Experience
In the fall of 2014 I consulted a naturopathic physician who ordered a laboratory test for neurotransmitters from Pharmasan Labs. The test measured levels of serotonin, GABA, glycine, glutamate, histamine, PEA, dopamine, DOPAC, norepinephrine, epinephrine, cortisol and melatonin. My test results showed that all these substances were within normal levels with the exception for serotonin, which was quite low.
At that same time I was being treated for Small Intestine Bacterial Overgrowth (SIBO), a condition that causes IBS and fibromyalgia. For more about that read my post on SIBO. The treatment of SIBO includes taking a prokinetic agent that stimulates gut motility to prevent bacteria from staying in the small intestine.One of those prokinetic agents is the drug Resolor that binds to serotonin receptors in the gut. Resolor does not, in fact, raise serotonin levels; after three months of taking the drug I retested my serotonin levels and they were slightly lower than before.
5 HTP
I then decided to take 5-HTP. I started with a small dose gradually increasing until I was taking 100 mg. three times a day for 6 weeks. When I retested my serotonin levels they were slightly above normal levels so I decreased my dose slightly. My gastrointestinal symptoms and fibromyalgia have subsided over the past year with SIBO treatments and the addition of 5-HTP seems to have helped with this recovery.
Taking 5-HTP did not improve my sleep which remains disturbed with multiple awakenings throughout the night. I suppose that is not surprising since I do not have low melatonin levels and I have never experienced improvement in my sleep by taking melatonin supplements.
People with fibromyalgia may be typically deficient in serotonin. Since serotonin regulates gut motility serotonin deficiency may be a contributing factor to developing gastrointestinal dysfunction, IBS, SIBO and fibromyalgia. Because serotonin can also affect mood, pain and immune functioning it could also play a role in problems there.
Getting tested for neurotransmitters and raising serotonin levels to normal levels by taking 5-HTP could be an important part of the treatment of fibromyalgia.
Have you tried 5-HTP? Let us know how that went here:
Health Rising’s 5-HTP Resources
- Dr. Murphree on 5-HTP and serotonin in fibromyalgia
- Dr. Murphree’s 5-HTP sleep protocol
- Check out more 5-HTP video’s


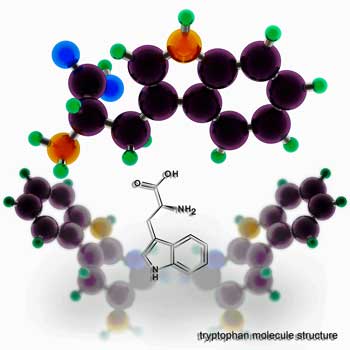




I’m looking at an image of the tryptophan pathway, but I’m confused about the relationship between tryptophan and 5-HTP. Am I right in thinking that supplying 5-HTP could shunt tryptophan away from the kyurenine pathway, in the direction of converting into serotonin and melatonin?
The way Dr. Murphree explains it it sounds like it might…
Darden says 5-HTP helped her fibromyalgia symptoms but it’s not really clear which ones…pain, fatigue,…?
I actually do not have fibromyalgia symptoms any more. My specific fibro symptoms were muscle pain and injury after physical exertion. These symptoms went away gradually over a period of a year and a half when I started treating SIBO. Taking 5HTP to raise my serotonin levels (serotonin stimulates gut motility) was part of that treatment. Before treating SIBO I was unable to lead an active lifestyle. Now I can exercise and practice the piano (I’m a musician) on a daily basis. This was not true before.
That’s great to hear 🙂
Darden, how did you treat SIBO? I’m on it with Rifaximin and Neomycin. I’m seeing improvment, but small ones, and when I reduced the dose those improvments went away.
There may be a subset of ME/CFS sufferers that have low serotonin, but I would tend to think the opposite is true (excess serotonin), especially in women. Symptoms of excess serotonin are very similar to many of the symptoms of ME/CFS.
Nausea
Diarrhea
Tachycardia
Cognitive problems
Headache
Changes in Blood pressure and/or temperature
Agitation
Etc.
I agree with you Rachael. The sx of low serotonin are quite different from high serotonin although some do overlap.
Good observation!
My GI function went from critically poor to “very good” on Wellbutrin. I understand that this drug indirectly boosts serotonin, dopamine, and norepinephrine. The serotonin only drugs ( ie Prozac and several others) caused even more constipation. Same with Cymbalta. But, Wellbutrin quit working after 5 or 6 years.
Dr. Murphree believes the antidepressants can only work to some extent because the supply of serotonin is limited. He believes you have to get more serotonin into the system via 5-HTP
Hello Cort,
Personally I believe their is something to this information Cort.This really makes alot of sence.I to believe low serotonin plays on alot of our symptoms.Please let us know how people are responding to increased serotonin.I want to again thank you for your hard work and dedication and devotion to the needs of the CFS ME and Fibromyalgia community.Really like the new web version.
God bless
Sincerely Dave Downer
Gee, maybe the 5 HTP works in a better way than the various prescription meds?? Anyone else have 3 shoeboxes filled with old supplements/ meds that didn’t work???? Going to dig to see if there is some 5 HTP in there.
Darden, thank you for sharing, even though you are well. This is important info for those of us still struggling.
I have at LEAST 3 boxes in the basement of supplements that didn’t work or didn’t agree with me. And then there is a big box of meds that gave me side effects!
Are there alternative ways of treating SIBO? I don’t know of a doctor who would treat it.
Will silver work?
Yes there are herbal alternatives to taking Rifaximin and Neomycin. Silver is not one of them. Because of my sensitivities I cannot tolerate herbs but I do fine with the drugs. Check out http://www.siboinfo.com/herbal-antibiotics.html for information on herbal antibiobics.
I’ve tried 5HTP several times in the past. My mood improved. But after a short while I would get chest pain each time I tried it. I looked around online and discovered that 5HTP raises serotonin level in the blood as well as in the brain. Too much serotonin in the blood causes vasoconstriction of the coronary arteries. That was scary. I stopped taking 5HTP. Tryptophan didn’t seem to have the same effect at first, but after a while that gave me chest pain, too. Several other drugs and supplements have given me chest pain every time I’ve tried them – tyrosine, Cytomel, Armour thyroid.
Interestingly I had the organic acids urine test recently – it suggested that I might be low on serotonin. Maybe I’ll try tryptophan again.
I’d to share more information on 5HTP, sleep, and fibromyalgia. There is a link to an older block article taken from an article I had published in The Townsend Letter for Doctors and Patients.
http://thefibrodoctor.com/true-cause-fibro/
While there is no one size fits all, I’ve had considerable luck in using 5HTP in the overwhelming majority of my patients. It can,but infrequently does, cause short term nausea, headaches and rarely hyper anxiety with serotonin syndrome (seen this happen in less than a couple dozen patients in 20 years). Unfortunately my CFS/ME are the ones will have trouble with 5HTP. If you have funny reactions to meds, especially antidepressants then you may have reverse effect of 5HTP. If so take during the day with food instead at bedtime. Hope this help and is appropriate.
Thanks for passing that on Dr. Murphree
I was hospitalized with Serotonin Syndrome in 2012,I never want to experience that again. At the same time,I am almost willing to try anything,if there is a possibility of having even some quality of life back while living with fibro and CFS. In your opinion, would I still be a candidate for 5HTP?
I’m one of the ones who has a funny reaction to 5HTP. For me it was chest pain. I’ve tried 5HTP a number of times and got the same side effect. I did find other people with this side effect when I searched the internet. The theory is that high levels of serotonin in the blood can cause coronary vasoconstriction.
Tryptophan didn’t give me the same side effect. What would you think about me trying that amino acid again? Does it have to be taken on an empty stomach?
Thanks in advance for any responses.
As far as I know tryptophan can raise serotonin levels as well as 5HTP so this might be worth trying.
I’ve had the opposite experience. SSRIs make my pain worse, as does melatonin, 5HTP. But medications like Flexeril, which antagonizes serotonin, help me. Many benefit from Trazodone, another serotonin antagonist. This Pub Med article suggests some fibromyalgia patients have antibodies to serotonin. I wonder if there is a connection?
http://www.ncbi.nlm.nih.gov/pubmed/1287679
🙂 No one ever said these diseases were simple!
Thx, very interesting.
Reminds you to remember to think of meds in classes, rather than just individual possibilities.
I have fibromyalgia. I am currently on Venlafaxine 150mg and Bruproprion 150mg. Not giving me a lot of relief of pain. Can I take 5-HTP while taking these SSRI?
I don’t know. The easiest thing might be to simply check with your pharmacist.
I’ve found that the pharmacists at CVS don’t know that much about supplements. And they are so super busy that they don’t care much . What they have is a database where they can look up interactions. I think you need a special database that has info about herbs and nutritional supplements. You can find some online, but maybe the pros have better info.
Sometimes true at CVS.
Tramadol, in addition to hitting mu receptor pain sites, supposedly raises serotonin levels, possibly doing that for me, subjectively. Anyone tried Nucynta (tapapentadol), kind of improvement supposedly, more pain control, fewer side effects, ? serotonin effects.
In the early l970’s researchers at MIT discovered how brain serotonin in made : when carbohydrates ( except fructose) is consumed with little or no protein, tryptophan gets into the brain and is immediately converted to serotonin. Brain serotonin and gut serotonin have different roles in the body; brain serotonin is involved in regulation of mood, food intake, symptoms of PMS, and possibly pain . If you eat the carbohydrate along with protein as in a turkey sandwich no serotonin will be made. All protein prevents tryptophan from getting into the brain. High protein diets mean low brain serotonin. Eating carbohydrates is nature’s way of having the brain make serotonin; buy supplements is not.
Very helpful, Judith, thx, believe you wrote a book I read a while back.
FWIW, folks, Nucynta is an opiate and classified as such, not just I got a sideways Tramadol improvement. I got small scrip but it is a heavy duty venture, PCP will prescribe sparingly and insurer apparently flags you as opiate user, need periodic urine test, etc. will save for level 10 pain I guess, level we just suck up, right? This country is rewarding substance abusers and encouraging irresponsible behavior IMO while punishing chronic pain sufferers. Heads to all, my PCP told me it is going to get worse and he will be told to cut in half the number of pain meds he can prescribe to current patients yearly. He is telling his patients to get refills while they can and hoard meds. Welcome to American medicine, most expensive in the world but far from the best. My PCP can’t deal with it, is retiring.