

With an enormous potential therapeutic gain and a high safety profile, further development and application of VNS is encouraging. Yuan et. Al
Vagus nerve stimulation is one of the most promising chronic pain interventions under development today. An earlier blog on Health Rising featured an astonishing story of a woman whose very severe fibromyalgia was largely ameliorated by a vagus nerve stimulator implant.
She was part of a small 2011 study which suggested that VNS may be very effective in fibromyalgia. The study was small but the success rate was high. Dr. Natelson, a neurologist who’s been treating and researching FM and ME/CFS for decades said:
“The results blew me away. I have never seen an effect as powerful as this.”
Many of the participants in that study no longer met the criteria for FM after it: that’s a criteria for success that few FM studies are willing to even contemplate using.
The study also required the surgical implantation of a vagus nerve stimulator. That’s an option – running somewhere around 30-40K – that’s available to few. Thankfully non-invasive vagus nerve stimulators worn on the ear have and are being developed.
When a recent three part review did an overview of our understanding of what the vagus nerve does, how vagus nerve stimulation works and how it effective it is, I jumped on it. This blog took the following papers as a foundation.
- Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part I. Yuan H, Silberstein SD. Headache. 2015 Sep 14. doi: 10.1111/head.12647. [Epub ahead of print] Review.
- Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part II. Yuan H, Silberstein SD. Headache. 2015 Sep 18. doi: 10.1111/head.12650. [Epub ahead of print] Review.
- Vagus Nerve and Vagus Nerve Stimulation, a Comprehensive Review: Part III. Yuan H, Silberstein SD. Headache. 2015 Sep 14. doi: 10.1111/head.12649. [Epub ahead of print] Review.
Besides the fibromyalgia study, the vagus nerve is of particular interest in both fibromyalgia and chronic fatigue syndrome (ME/CFS) because of the role it plays in
- regulating the autonomic nervous and immune systems
- providing sensory and other information to the brain and
- Michael Van Elzakker’s Vagus Nerve Hypothesis – Van Elzakker suspects small infections in or around the vagus nerve could be triggering it to tell the brain to produce flu-like symptoms in people with chronic fatigue syndrome (ME/CFS). A pilot study to assess that possibility is underway now.
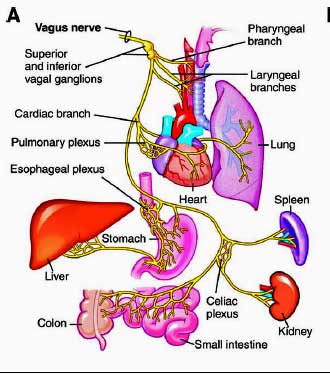
The Wanderer
Called the wanderer, the vagus nerve is the longest “cranial nerve” (a nerve that emanates from the head) in the body. Attaching at the medulla at the bottom of the brainstem, the many fingers of the vagus nerve reach down our torso to infiltrate most of our organs. The extensive network it forms – it’s the largest neural network in the body – provides a pathway through which information is sent to the brain regarding the status of our organs.
Vagus nerves densely innervate every ‘sensing area’ of the body with a particular focus on the walls of the blood vessels throughout the body and the digestive system. The vagus nerve regulates our heart and breathing rates, blood pressure and blood flow via receptors in the blood vessels that monitor O2, CO2, and pH levels in the blood and blood pressure.
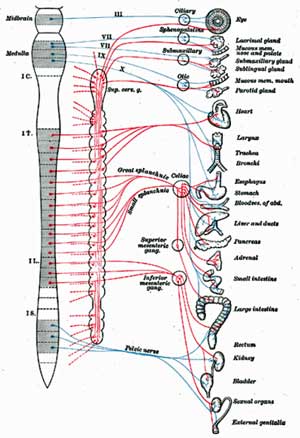
If a pathogen is present the vagus nerve will let your brain know that. If you’ve cut your finger, are feeling hot or cold, or have just eaten something – the vagus nerve will let your brain know that.
Ultimately information on touch, heat/cold, pain and chemical, metabolic, and hormonal operations of the organs is all transmitted via the vagus nerve to the brain. It effects the functioning of every system – from the immune to endocrine to the hormonal system – in our body.
Immune Regulator
The last ten or twenty years have revealed that the vagus nerve (VN) is a significant immune system regulator. The cholinergic anti-inflammatory immune response it regulates mostly takes place in the spleen.
Think of the spleen as an enormous lymph node which dictates much of the innate or early immune response. Besides filtering blood the spleen synthesizes antibodies, removes bacteria and plays host to half the monocytes found in the body. These monocytes – which turn into dendritic cells and macrophages play a key role in the innate or early immune response, which plays a key role in producing many inflammatory states.
The cholinergic anti-inflammatory response has been shown to reduce the levels of a wide variety of inflammatory cytokines. Studies are underway to assess the ability of VNS to reduce inflammation in diseases such as rheumatoid arthritis and inflammatory bowel disease.
Autonomic Nervous System Regulator
The vagus nerve’s effects on autonomic nervous system functioning could easily account for the benefits thus far seen in fibromyalgia and other pain disorders. The vagus nerve boosts the activity of the parasympathetic nervous system (rest and digest) and reduces sympathetic nervous system (fight or flight) system.
Reduced heart rate variability findings suggest that reduced parasympthetic nervous system functioning is present in both ME/CFS and FM. Reduced HRV has been associated with increased sympathetic nervous system activity, pain and sleep and cognitive problems in ME/CFS and/or FM.
Because VNS increases heart rate variability it’s possible that besides reducing pain it could also improve sleep and cognition.
Vagus Nerve Stimulation
Vagus nerve stimulators use electrical pulses to increase vagus nerve functioning. The vagus nerve runs up and down the neck. The stimulators contact the vagus nerve either by being surgically implanted in the neck or by non-invasive devices worn on the ear or neck.
The first vagus nerve stimulators attempted to interrupt epileptic seizures in the late 1890’s. Those attempts largely failed, and it was not until the 1990’s that the researchers felt confident enough to attempt it again in humans. In 1997 the FDA approved a surgically implanted device in the neck for people with treatment resistant epilepsy. In 2005 treatment resistant depression joined the list. Since then more than 70,000 people have received surgically implanted vagus nerve stimulators.
VNS stimulation is currently being assessed in a wide variety of diseases and conditions including heart disease, inflammation. Crohn’s disease, depression, stroke, tinnitus, diabetes, migraine, irritable bowel syndrome and others.
Pain Reducer
The first hints that VNS might helpful in reducing pain came when epilepsy patients reported experiencing reduced pain.
VNS may be effective with chronic pain because it’s able to effect a wide variety of factors that contribute to it including inflammation, oxidative stress, autonomic nervous system activity, the opioid response, central sensitization, and pain perception.
Studies indicate that VNS may be able to reduce the process of “temporal summation” that plays a crucial role in the production of many chronic pain states. Temporal summation refers to the windup mechanism that causes the nervous system to become more and more sensitive to pain.
During wind-up the nervous system learns to respond more and more quickly to the slightest hint of pain signals. VNS appears to help the CNS to unlearn this process in a manner that allows VNS, unlike other therapies, to become more effective over time.
The poor response to opioid pain drugs found in a significant portion of people with fibromyalgia could have its roots in vagus nerve problems. It turns out that good responses to opioids only take place in people with healthy vagal nerve activity.
Non Invasive Ways of Stimulating the Vagus Nerve
Two non-invasive means of stimulating the vagus nerve at the ear and the neck have been produced.
Ear Devices
The NEMOS stimulator that attaches to the ear was approved for epilepsy and depression in 2010, and pain in 2012 in Europe. Imaging studies indicate the ear device has similar effects on the brain as the invasive device.
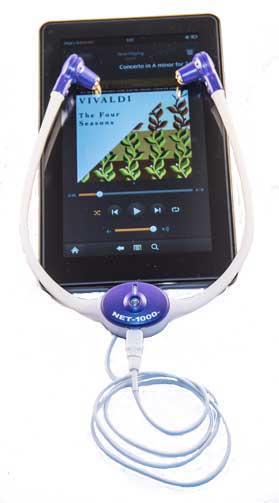
A similar device in the U.S. called the NET 1000 is being currently marketed as a microcurrent/music therapy device by a private company named Aura Stim Medical. The company markets the device, which costs $650.00, as a music therapy device for migraines and other disorders. It has been assessed in three studies.
The company believes that the electrical frequencies and audio signals the device delivers can induce the secretion of pain reducing substances such as beta-endorphins and neurotransmitters such as serotonin and dopamine. The device, which can be hooked up to a smartphone, is marketed to people with migraine and other types of headaches, premenstrual syndrome and/or depression, anxiety, and stress related to chronic pain.
Neck Devices
The gammaCore device produced by a New Jersey company ElecroCore LLC has been cleared in Canada and parts of Europe to treat severe headache (migraine, cluster), reactive airway diseases (asthma, COPD, exercise induced bronchospasm), epilepsy, IBS, gastric mobility disorders and panic disorder, PTSD and other mood disorders. It appears to be able to inhibit glutamate expression in the trigeminal nerve in the head in migraine.
The Gamma Core Device
Three gammaCore headache studies were published in 2013 and 2014 and the company states three more are underway.
Another device that can be placed on the skin overlying the vagus nerve on the neck and then activated several times a day has been cleared to be clinically tested in an ME/CFS-like disorder.
Complex System
The vagus nerve encompasses a complex system. It carries autonomic, sensory, metabolic and other information to the brain via afferent nerve fibers. It also regulates autonomic and other activity (heart rate, blood pressure, blood vessel functioning, gut activity, secretions, immune functioning, etc.) via efferent brain fibers leading to the organs.
Given the vagus nerve’s widespread effects, altering its activity has the potential to affect many processes and diseases. The expensive and invasive nature of surgically implanted vagus nerve stimulators has undoubtedly, however, interfered with its more widespread adoption. (Even in the two diseases VNS has been approved for, it’s approved only for treatment resistant versions of them.)
As noted above non-invasive means of VNS stimulation have been and are being developed, but studies are few. The few studies that have been done suggest the invasive and non-invasive devices producing similar effects on the autonomic nervous system and brain.
Evolving Technology
Vagus nerve technology is continuing to evolve. Miniaturized devices are being tested in rheumatoid arthritis. A heart failure device able to unidirectionally activate vagus nerve fibers is being tested as well. It’s the only device, thus far, able to activate only the nerve fibers going from the brain to the body. It specifically activates the B-fibers leaving the brain that stimulate parasympathetic nerve activity.
Researchers are becoming able to identify which frequencies work best in which diseases, as well. The anti-inflammatory response of the vagus nerve, for instance, is best triggered at specific electrical frequencies (5Hz, 15-20 Hz.).
It’s clear that intensity matters as well. High voltage VNS stimulation can cause low blood pressure, low heart rates and bronchoconstriction, while low voltage stimulation can reduce bronchoconstriction without effecting the heart rate at all.
Natelson’s experience in this field may be instructive. His and Gudrun Lange’s ability to produce a small trial of surgically implanted stimulators in FM was remarkable given the expense and newness of the technology to FM.
It stopped there, however. It’s remarkable to me, given the excellent results of the study, that five years later no followup has occurred. It hasn’t been for the lack of trying.
The NIH turned down Natelson’s request for a followup study because the study would not reveal more about the mechanisms at work. (The NIH apparently does not fund clinical trials to determine treatment efficacy!)
No FM VNS studies are in progress that I know of either. Efficacy, as we’ve seen in ME/CFS, does not always translate into more studies.
A non-invasive VNS study, that will, however, begin soon in an ME/CFS-like disease could provide a bridge to further ME/CFS and FM studies, and gammaCore may be available in the U.S. soon.
More on the Vagus Nerve
For more on the use of vagal nerve stimulation including past blogs, and how to possibly use a TENS unit to stimulate the vagus nerve visit Health Rising’s Vagus Nerve Resource page.
Other Means of Increasing Vagus Nerve Activity
Breathing slowly in and out through the nose, some yoga practices, gentle resistance breathing and other practices may be able to stimulate the vagus nerve as well.







Interesting! Thank you, Cort.
Any implications for the treatment of orthostatic intolerance? Any clinical trials of VNS for OI?
Nothing I saw for POTS but since it’s affecting the ANS I imagine it could have significant effects on orthostatic intolerance.
Of course, the field of orthostatic intolerance and POTS is relatively new as well and isn’t very well studies.
Studies have increased quite a bit recently but I’m kind of miffed that more study is not occurring. I think the fact that non-invasive devices may work has not really gotten out there.
Or, it simply isn’t as profitable for pharmaceutical companies selling so many people so many drugs to manage pain and other symptoms……so big pharma is using influence to block more research funding
on this.
Dr Diana Driscoll has just created a supplement for Vagus Nerve Support called ParaSym. She also has POTS, MCAS, EDS. The website is vagus nerve support.com
She has been doing research on the Vagus Nerve. I have not tried the supplement but I just ordered it. Being very sensitive to supplements, I don’t have any expectations.
I will report my response.
Our 2 sons became chronically ill after what looked like a viral illness. We experienced the usual challenges in finding a diagnosis. They shared similar symptoms but experienced them differently in terms of severity and frequency. Our youngest son ended up seeing Dr. Adrian Miranda, a neurogastroenterologist at the Autonomic Disorders Center of the Children’s Hospital of Wisconsin for daily abdominal pain and nausea. He tested borderline normal with the autonomic testing but was still diagnosed with POTs based on his clinical picture. To make a long story short, through Dr. Miranda, we were referred to Dr. Christopher Brown, who administered a vagal nerve stimulator for our son. He wore the device on his ear continuously for 5 days and it cycled on and off during that time. He noticed changes within a week. We were told that at first, the symptoms may get worse, and they did. But Dr. Brown encouraged us to stay the course. We repeated the 5 day cycle four more times. Each time he felt his pain decrease. His pain went from a 7-8/10 to a 3/10 and he elected not to continue treatment to see if he could eliminate it completely. However, about a month after his last cycle, he was pain and nausea free. His symptoms improved slowly on their own until they were gone. After being out of school for 2 years because of his illness, he is now back in school. We have just weaned him off Florinef and he seems to be tolerating that. His tachycardia has improved overall, however, strangely, for him, that wasn’t a daily problem. That said, we also had him tanked on Gatorade and taking salt tabs. So although we monitored his nausea and pain, we didn’t necessarily keep a close record of his heart rate so we don’t know at what point that got better. If he gets behind on fluids, his heart rate trends up again, but not to 110-120 (at rest) like he used to. He continues to suffer from fatigue but even that has improved and he is managing that much better now. Did the pain and nausea contribute or worsen the fatigue? Perhaps with the more severe symptoms eliminated, he could tolerate the others better? It’s hard to know for sure. I think the “problem” with the nerve stimulator, and perhaps the reason it hasn’t become more mainstream is that the vagus has so many connections – to the body and the brain, that to some degree, you just don’t know what is going to happen. Even so, that in itself is not a reason to withhold this treatment. One could say that about almost every FDA approved medication- there may be side effects and we simply won’t be able to predict to a person what is going to happen. Like all treatments, it should be decided upon after open discussion between providers and patients. What I do know is that we feel blessed that we found the right doctors and the right treatment. The nerve stimulator has been a gamechanger for our son.
That’s great new Cris. Sounds like you have a great doctor there – thanks for sharing. It would be great to get your son’s recovery/recovering story in Health Rising Recovery/Recovering stories section by the way. http://www.cortjohnson.org/forums/recovery-stories/
That’s great news Cris. Sounds like you have a great doctor there – thanks for sharing. It would be great to get your son’s recovery/recovering story in Health Rising Recovery/Recovering stories section by the way. http://www.cortjohnson.org/forums/recovery-stories/
Cort,
I’m trying to ask Cris a question (in this thread) but there’s no ‘reply’ button next her comment. I’m trying to find out if this Dr. Christopher Brown is with Duke or somewhere else. There are several Dr. Christopher Browns is why I’m asking. Also, what type of equipment did he use and is it commercially available. Thanks a lot!
Dr. Brown is in private practice in Indiana. Here is his contact info: Christopher Brown, DDS MPS, 823 S. Adams St. PO Box 685, Versailles, IN 47042. Tele (812) 689-5151. The following is a link to one of his articles. Good luck. He has changed our lives. I would also recommend the Autonomic specialists at the Medical College of Wisconsin and/or Vanderbilt.
http://article.sapub.org/10.5923.j.cmd.20150504.03.html
Cris, could you tell me which device did Dr. Brown use for your sons?
As a neurologist, I’ve been involved in using and programming VNS devices for patients with epilepsy for years (not much in my present position, though). I think that it is quite likely that the mechanism of action of VNS in treating FMS is via its effect on GI motility. FMS is highly correlated with having SIBO (small intestinal bacterial overgrowth). SIBO is both caused by impaired intestinal motility (absent or sluggish migrating motor complex – ‘MMC’), and is a common cause of increased GI permeability (‘leaky gut’), which is the primary driver of inflammation and autoimmunity in the body. Stimulating the vagus nerve activates or strengthens the MMC, and therefore may help to treat SIBO, which helps heal leaky gut, and therefore reduces body-wide endotoxemia and inflammation.
I had read of the study of non-invasive VNS for treating FMS in the UK, and actually wrote the the principal investigator, asking him to try a different stimulation protocol, as his was derived from the usual pattern in which the device is used for treating epilepsy. This usually begins with stimulating the vagus nerve for about 30 seconds every 5 minutes. The frequency, pulse-width of each mini-shock, and other parameters are also programmed and adjusted as the treatment is introduced. I speculated that if it does work by stimulating intestinal motility, it may work better to stimulate the nerve more like the physiologic pattern of the natural MMC, which occurs about every 90 minutes, but is aborted by any food entering the stomach. I suggested that they try stimulating the nerve for about 5 minutes out of every 90 to 120 minutes, as a starting point, but unfortunately, I got no reply.
I may speak with some of my epileptology colleagues to see if I could review records for their population of VNS patients, so as to identify those among them who also have FMS listed in their medical history, and then do some follow-up interviewing of them to see how their FMS has done since starting VNS therapy for their seizures.
Has VNS ever been tried or considered for people with MS? Wouldn’t stimulating the VN help with bladder, bowel, cognitive, headaches, swelling, balance, heat intolerance?
There may be some data on VNS trials for some MS symptoms, but I’m not aware of any. It is being used for both migraine and cluster headache, as mentioned above. I don’t know if it would be helpful for balance, cognitive issues, swelling or heat intolerance, as those would primarily be caused by CNS damage in the brain and spinal cord, but since I don’t think that even the mechanism of action for epilepsy has been clearly demonstrated, who knows? There are likely quite a few people around using VNS for seizures who also have MS by coincidence, since both of these disorders are fairly common, so there may be some case reports out there, if they did not some MS symptom improvement after starting VNS.
Dear David, I am wondering if you know the wave length/hz recommendation for this treatment. I have a TENS/microcurrent unit and the original study I read was just using a TENS unit and getting good results for Fibromyalgia. But they never told the information I am lacking. I have been trying different settings, not having the money to buy the much more expensive units that do the same thing but have built-in settings. Can you help at all with this information? It would help a lot of people. I doubt that few of us don’t have money issues, especially those who have had it long term like myself. Thanks for your post. warmly, joya skye
I’m afraid that I’m not familiar with TENS settings. With the Cyberonics VNS generators that I used to program for epilepsy, I think that the initial settings were something like a 1mA current output, 30Hz frequency, 500uSec pulse width, on for 30 sec, then off for 5 minutes. That probably wouldn’t have much to do with TENS settings, since the leads were surgically implanted and wrapped directly around the vagus nerve in the neck, and so didn’t have to penetrate the skin and sub-Q tissues.
Hi David, thanks for responding. You are on a ME/CFS, fibromyalgia site, so I am assuming you have some familiarity with those illnesses. We have a lot of the same symptoms as you have described, although, I don’t have epilepsy (Thank God for that one anyway). I have not used it on TENS, but on microcurrent, and with ear clips which does put it in contact with the vagus nerve. Does that help? I don’t know if Cort ever heard the settings in the FM study that used TENS. And I don’t know if he reads all of these. Kinda doubt it as he has it too, so energy is at a premium. Thanks for responding. warmly, js
Joya,
Unfortunately, my familiarity with CSF/FMS is as a patient, not as a practitioner, as my area of practice mostly deals with stroke. I’ve never used TENS, and unfortunately don’t have an answer for you about the settings. Good luck!
I just wanted to tell everyone considering the Vagus Nerve Option. Number 1) There were trials starting Summer 2015 with ear acupuncture and temporary TENS with Military, to be extended to Civilian Pain Specialist, this is free or maybe they even pay, who knows. But they were going to rework the acupuncture needles, because I showed them my brass ones stayed in better for up to two weeks. It’s worth a look into to see if it even works. Also, if you have insurance that covers epidurals and can find a doctor, my Military Pain Specialist also has Neurological background, who does naval block.
Today is my 7th day post Complete block both left
and right side. My physical spinal complications make this dicey at best for even temporary success for pain. For 3 years, I have experienced daily migraines, lesser to greater magnitude, some requiring me to be sedated and ice packs to my head. My whole spine is now involved in disc degeneration because their are quite a few, lower, mid, cervical, even though I had to have one surgically removed, oops there’s another. I am probably as diagnosed over 17 years ago living out, years of being a punching bag as a child, mostly directed daily at the head and neck. My head sits two inches to far forward on my spine, and leans right, as my vertebrae are worn. This was first noted by my grandmother’s doctor when I accompanied her one day on at the age of 8. Said all that to say, today after driving yesterday, which I have just started doing since October since my first block and 1 month of Cannabis Oil without THC. Haven’t drove any where because of pain in 8 years. Today my Pain is tolerable after a 80 mile commute round trip, lunch out, full day, 5 hour excursion, no nappies, up with hubby till 11, joking, good night sleep and all with harrowing visit about PTSD no Fight/Flight stress yesterday or today. No muscle jerks, no headaches. Had some nerve pain in my hands last night probably from gripping steering wheel from crazy drivers,iced my hands, it went away. So I am taking baby steps. In 25 years of having Fibromyalgia, which now has developed into “we don’t know what the eff you have” Syndrome. I have been guinea pig to enough Quackery. But this has given results so far, if just for the migraines, the panic attacks, being in fight mode always on guard, this worth it, but it seems to dull the pain, too.
My gosh Deborah – good luck! You deserve it!
No, Cort, from the inmost of my being, I know it was a blessing that sent me originally, to this site. Without it I would never have heard about Vagus Nerve Treatment. Or Vagus Nerves. I have learned so much valuable information about studies, causes, and began to hope again, when I was just lying in my bed suffering, day in, day out. I was no longer depressed about as I am a believer and had my eyes opened to the beauty of suffering. Funny, when you accept your fate, it changes. If this is temporary, there is always another block, or maybe something more permanent, but this is something. Something is working on me! I wish the researchers could know, I could be a Rosetta Stone for “we don’t know what the eff you have”, but if you listen to me, maybe it started with human parvovirus B19 Spring 1990. Maybe it started with Cervical Cancer 1991. Or my DNA,maybe MTHFR, with all of the above. But it’s working today only my lower spine hurts which is the very worst of it, and I am barely registering, thank you Cort, for sharing your thoughts, knowledge and encouragement
Many Blessings to Everyone,
Deborah Shaffer Turner
Dallas Georgia
Interesting–you’re the first person I know of that had the brass acupuncture ‘barbs.’ I had a dozen or so inserted into both earlobes December 2014 because the accupuncturist had tried everything else. I didn’t know at the time, but when X-rays were taken of my painful hip, the radiologist neglected to get the report to my doctor until the following April. Grrrrr. It was then diagnosed as end-stage hip arthritis and a total hip replacement was performed in May. So maybe that technique only works for neurological pain? (which I also had, but the joint pain was so overwhelming that the barbs couldn’t work..?) Btw, I kept them; l they’re about 1/16″ long–amazing. Rheumatologist finally got me off Oxycontin because it’s getting so much bad press these days, now I’m using Nucynta ER and IR for break thru–I’m not impressed. (I paid $1,335 for a months’ worth yesterday because I haven’t met my deductible yet–don’t know how I’ll finance that one.) Haven’t told the doc yet, but I’m still supplementing the Nucynta IR with 15 mg oxycodone just so I can get my dog out to do her business. 😉 What kind of life is this?
Sally, Don’t know if they were actually brass materials, but nubby little brass looking thingies, being their super technological name, I am certain. My Pain Management Doctor Woodbury, at Atlanta Veterans, puts them in my ears, after my usual visits. They have some major staying power, whatever they are made out of. The record holder was just a couple days shy of 3 weeks but he was up high under a flap part of my ear. The Vagus Nerve Research Design guys saw their high tech acupuncture delivery needles didn’t have the stick in there the nubbies did.
I have been dx with PTSD,ANXIETY, ADD,CF, IBS, Fibromyalgia, RA, GASTROPARIESIS/DTP, chronic constipation and now Systemic Lupus so of course chronic pain. I have been seen and discussed the gastric pacemaker for vagus nerve because of GP/DTP stimulation at MUSC. This sounds like it could also be helpful for Lupus?? Sounds like I’d be perfect for a study on this noninvasive approach at VNS! I want my life back. I’m in the Charleston area and MUSC does the gastric pacemaker which I was told there’s a 50/50 chance of it working. Just don’t understand why they wouldn’t fund this less expensive, noninvasive approach that could possibly help those of struggling day by day. The swelling/ inflammation from Lupus is so debilitating I can literally feel my organs being squeezed! I’m on so many medications and I hate that. This seems to help a multitude of chronic diseases and there’s no cure for any of them and very little they can do for any of these. So many people are suffering and dying even little children. Praying for funding this. Thank you for advocating for those of us struggling to do the simplest of tasks. God bless!
That is fascinating. I have had FM and spinal stenosis for 20 years, and just got IBS/possible SIBO diagnosis. I can work 50 hr weeks, but excercise wreaks havoc with my muscles. I wish you luck on your investigation. Please keep us posted. Do you think a VNS supplement is viable? as referenced in a previous entry?
Hi David,
My brother Sean suffers from severe CFS/ME. He possibly contracted a virus while working a gap year in South Korea (he is also coeliac) and has been bad for over four years. He is bed ridden for most of the day, terrible crashes and brain fog, finds it difficult to speak for more than a few minutes and lately isn’t even fit to see anyone. Its like the life is being sucked out of him more each day. We do not know where to turn. Doctors in Northern Ireland are unfortunately clueless and there are no specialists. Sean doesn’t want to go into hospital as he says his brain just isn’t fit and from my research they probably wouldn’t know how to treat him. His own doctors have ran some blood tests but all has came back clear.
I only just tonight came across the ‘Vagus Nerve’ for the first time and it makes so much sense. Could you recommend anything for Sean? If i contacted the doctor maybe you could recommend a particular test to ask for?
Thanks in advance, any help would be greatly appreciated.
Natasha
Natasha, is it possible to ask the doctors for a dose or two of immunoglobulins for your brother?
Also, my husband has ME/CFS after contracting a virus (after also fighting a huge wildfire) and he’s now getting some benefit from betainterferon (brand name Betaseron)
Both of those treatments are expensive. My husband’s doc is one of the best for ME/CFS (Dr Chia in Southern California) and those are the treatments he’s given my husband.
Also for the vagus nerve stimulation (which I only learned about last night) I have him doing what he can at home. My research shows humming stimulates the vagus nerve. Also breathing in slow for a count of five and breathing out slow for a count of five to eight seconds. You can research other ways to stimulate the vagus nerve at home. (Chanting Om among others)
I am super interested in your understanding of using the device to help with gut motility and SIBO. Do you have an email we could correspond with?
Could this treat an overactive Th2 immune as seen in CFS?
I believe that it makes sense that it could. If my memory is correct the kind of ANS problems seen in ME/CFS and FM lend themselves to Th2 dominance. So do the HPA axis problems I believe.
There’s a new device, not being marketed as medical equipment, but I wonder if it would be helpful. It’s called Nervana and it stimulates the Vagus Nerve while you listen to music. http://experiencenervana.com/achieve-nervana-music/
Thanks Gail!
Hey Cort, I picked up on this approach in the article you published about a year ago about Tens stimulation. My problem is that I can’t find the frequencies they use for this. I have a tens/microcurrent unit, but don’t know where to set the impulse. I have tried a bunch but not with any success. I can’t seem to get to that info anywhere in the site. Can you please advise, or point me at where I can find this info. Thanks for all you do for all of us. js
I’m certainly not an expert, nor have I had experience with TENS. My sister is a nurse and she tells me TENS units are just one source of irritation to substitute/distract you from whatever is currently irritating you at any given time. Anyone else heard this opinion? 🙂
Sally, this is just my experience, also. I got my first TENS when they first came out like a few decades ago for back and neck pain, agreed, only worked while using the unit.
I was a test subject using a TENS stimulating the Vagus Nerve via acupuncture (4) type needles in my ear area spring 2015 for 4 weeks relieved my Fibromyalgia pain and general nerve pain, but did nearly nothing for my back pain which has now developed into Degenerative Disc Disease. Again relief lasted as long as TENS unit was on which was intermittent 24/7 for 4 weeks and close enough in timing I got relief.
So, if you have generalized nerve pain or Flu like discomfort, this TENS implant just maybe the real deal because I was just given a new high techie techie TENS, supposedly way better results than original. I tried it a few times, way longer than recommended 30 minutes, and pain was back in 5. So regular TENS unit for some reason don’t work for me.
Hi Sally, I sure wish my CFS/Fibro was just because I was irritated with someone. I have a microcurrent (that also does TENS) but it is to stimulate the Vagus Nerve to assist in many symptoms, up to and including passing out. The Vagus Nerve is connected to every organ in our bodies. Thanks, but a nurse is no better trained than I was and I know from experience that stimulating the Vagus Nerve is important to getting well.
I am also really interested in the vagus nerve – and have long thought it might play a role in my ME/CFS. I have pretty severe Orthostatic hypotension (OH) at this point (considered orthostatic failure). I would be interested in any info regarding relationship between vagus n. and OH.
Joyce, the article talked about impacts to blood pressure, heart rate and other autonomous nervous system functions controlled by the vagus nerve. It also shifts you to the parasympathetic nervous system and gets you out of fight or flight which can’t hurt. Seems like it might be worth sharing the article with your doc. Might prescribe it for pain at least. Then you can see if it helps OI. It sure doesn’t sounded like it would cause harm. I’m intrigued, anyway.
Cort, do they believe it will address the root cause, or simply manage symptoms for better quality of life?
I think it’s more of a symptom manager…
Interesting, seeing Silberstein I figured there had to be a headache angle. Going to have to research the NET 1000, my migraine meds are pretty expensive!
gammaCore believes its device will be licensed for use in the U.S. in 2016. You might want to wait for them. Based on the appearance of the different websites I would have more faith with them.
Thanks for this great summary, Cort. Re: your passing comment about yoga, I do a gentle practice most days of the week, and find that chest-opening poses can stimulate the vagus nerve and improve gut motility.
Although I’m fascinated by the idea of external VNS devices, yoga has been around a lot longer, and is a lot cheaper!
Cort, do we know what frequency is needed for the immune and autonomous effects to be achieved? Versus pain only? And is a model with those frequencies obtainable in the US or elsewhere?
Yes, Kate, this is what I have been asking and want to know. The units themselves are not the deciding factor, it is the pulse wave length and the pulse rate I am looking for. The more expensive units do not necessarily do anything the less expensive units do, they just have the right settings and so far, no one has answered this question. And, dear Cort, I’m pretty sure that enough vagal stimulation can do more than symptom control, although that would be better than nothing at this point!
TENS Settings in this study:
http://www.brainstimjrnl.com/article/S1935-861X(14)00260-5/fulltext
The effects of tVNS parameters on autonomic function in 48 healthy participants were investigated using heart rate variability (HRV) and microneurography. tVNS was performed using a transcutaneous electrical nerve stimulation (TENS) machine and modified surface electrodes. Participants visited the laboratory once and received either active (200 μs, 30 Hz; n = 34) or sham (n = 14) stimulation.
Here’s the layman’s review of the study: http://www.eurekalert.org/pub_releases/2014-08/uol-ye081914.php
Here are two other studies that use 25hz and 25v (same measurement?) respectively:
http://www.cerbomed.com/upload/Poster_fMRI_evidence_Komisaruk.pdf
http://www.brainstimjrnl.com/article/S1935-861X(14)00260-5/fulltext
In the summer of 2015, my Pain Management Doctor at VA Atlanta recommended to be a candidate for a TENS unit that used acupuncture sites on the ears to stimulate the Vagus nerve. I wore the TENS during the four week trial with very favorable results. I experienced no TMJ, no migraines, I was more relaxed as I am in constant fight mode, my PTSD episodes were down and I experienced better sleep. But as soon as the TENS were removed, the symptoms creeped back.
Then Dr Woodbury and I discussed the next step, getting a vagal block. That’s basically where they thread a catheters up through your neck and into your lower brain where the nerve resides and I don’t know what kind of medication they injected but it was a slow and quite painful process. And this is from the woman who can take epidurals like it’s nothing and walk around with a fracture and not do anything about till my foot turned black and was misshapen. To my chagrin they can do only one side, left or right at a time.
My left was done in October 2015,and my right just last Friday. I also am the Cannabis Oil Queen, legal CBD. I am really doing quite well. The CBD has all but alleviated my fiery red ant all over nerve pain. My hands and feet don’t ache and burn. I am sleeping better. My IBS is better,and so is my IC. I have had one migraine. My muscle spasms continue to be a problem,so tense my back muscles pushed out acupuncture needles. My spinal pain due to degenerative disc is still prevalent. Thanks to blog friends here, I have gotten in touch with others like me who had experience with Medical Marijuana. They have told me,they pain and spasms go away with THC which CBD oil doesn’t have. They assure me you don’t sit around stoned out of your gourd, but when I smoked pot I didn’t do that either. Kept a 3.4, held down a job and won Awards,very functional. ROFL.
But back to Vagal block, I will know just how good it works in a few days.
Also,investigating MTHFR GENE, since we have midline defects and cancer, looking at the B12 and Folate Vitamins they recommend for anyone diagnosed with immunological disorders and Fibromyalgia.
Thanks for putting me on this path originally.
Hi Deborah, thanks for sharing. Could you please advise if you know of a good specialist dealing with MTHFR issues (which I have) ?
Karin,
I have been getting the majority of my information from MTHFR.net. He has listings of MTHFR Specialist. Be forwarned pricey, pricey. He just suggested cheap self DNA Test, unless you already have done. And the ones in my area,Atlanta, don’t take insurance.
The NIH and CDC are poo pooping it, but Dr Ben has nailed my medical and family history, from our and my cancers to our minor midline defects. I have been prescribed B12 shots for years and it’s supposed to metabolize out of your system in 3-4 days, but a few years ago when tested it showed I had bookoo in my body. The Fibromyalgia Network said go ahead and take the B12 Methylcobalamin and Folate Sublingual it can’t harm you. Dr Ben warns to slowly start vitamins. I am going with his products, they aren’t that expensive and get excellent reviews, and see if my energy builds and immune system gets stronger. I found out about Chelatin Calcium Magnesium, for us folks that don’t digest well in the gut to better help with muscle spasms. I have decided to forego the DNA test, me,
my children, and ancestors are too quirky and fit right in the moderate medical snapshot.
I am not sure what state you are in but I have seen several naturopathic physicians (licensed in my state, OR) and they are very familiar with this.
Congratulations on your success and thanks for passing that along. Good luck with the block.
Hi Cort, so were you ever apprised of the settings on the TENS unit? And if it helped, why haven’t you continued with it? I realize it was a trial, but any info you can provide would so help the rest of us. I bought a Tens/microcurrent unit after reading that article, but the settings were not in the article and I have been fumbling around with it ever since. I know the units that claim to cure insomnia, depression, anxiety, etc. are very expensive and they are basically the same as their much cheaper counterparts not making such claims. The key seems to be knowing the settings. Can you help with this? Thanks, Cort, you are such a help to us all. I am sorry I have not been able to contribute, but I am broke beyond all reason after being housebound since ’06. When I have it, you will get some! warmly, joya skye
Hey Cort,
It’s Wednesday after my Vagal block and I am doing pretty good. Actually, really good because this morning had an interview with a new psychologist, which means going over a the “highlights” of my life and why I have PTSD,always a day at the beach. Well,it was alrighty because I was able to leave the experience there at her office and go to lunch with my BFF and some how ended up talking about whose the sexiest movie Cowboy, it’s definitely Sam Sheppard. We were laughing so hard, in our debate, we had guys doing cowboy imitations at the next table. So, that’s one symptom, down. I don’t know if I feel less fight, but I haven’t felt aggressive today and driving in Atlanta traffic, can make you want to commit heinous acts and give the one finger salute. But I slow landed and figured pass me please. I am driving myself again, even long hour away Doctor appointments. In Metro Atlanta, if you’re from a small town like my family is, you have to commute an hour to get anywhere and think nothing of it, unless like me prior to Cannabis Oil, I was so disabled I couldn’t drive myself, and just riding was too painful. I drove!!! I was out for 5 hours!And though I am laxing,I am not sleepy and I am cheerful. So thanks again for the helpful information many months ago on the Vagus Nerve. I will be able to tell tomorrow if it was helpful with the Degenerative Disc Pain. I have so many now, this is my big hope. Or transfer to a Medical Marijuana State. Cause last night hubby said one of our illustrious Georgia Legislators was discussing the illegality of CBD OIL in our Great State, but when questioned if he would have people arrested. We have a store now in Atlanta, hello! He said he would hate to hurt folks who was benefiting from it that had seizures and such. He would just hate having his happy@$$ not getting reelected and such!
I envy your access to cannabis oil–the rheumatologist that treats my OA, FMS/CFS/ME, Hashimoto’s, scoliosis, neuropathy due to a failed back lumbar fusion (that has led to spondylolithesis), a hip replacement (in two words: Chronic Pain), said he’d give cannabis to me in a skinny minute if it was legal in PA. As it is, he’s taking me off opioids since I have to move to down south soon and he thinks I’ll have a tougher time finding pain relief down there. I’ve been on everything he’s licensed to prescribe. I’m at my rope’s end, to the point I’m, well, you know, when you feel there’s no options left. I enjoy this blog, but at 61 it’s frustrating to hear about new developments I know I’ll never be able to try.
Sally,
CBD oil is legal in all 50 states. That’s what I take. My “Fibromyalgia” presents like MS without brain lesions, so have had great success. You can contact the Realm of Caring, they have counselors, and you can even enroll so that you can sometimes get your oil discounted. CBD doesn’t have the THC, which is why I went with the Vagal Block, do to my chronic spine pain, I need the THC, but in Georgia they are afraid of people like us becoming Medical Marijuana Junkies and leading down the path of ruination. It would be much safer and less addictive for me to pop 3 Percocet 10MG a day, but gosh darn, I have drug sensitivities and that would knock off my @$$ 12 ways to Sunday, plus the itch and unsightly rash factor, maybe a swollen throat, and possibly stop breathing, hate when that happens!
I’m really interested in Georgia’s policies on medical marijuana,as my husband and i will be moving to the Norcross area (if and when we sell this farmhouse; they’re not in demand right now). He was transferred, and since we’re 61 & 62, we’ll go anywhere as long as they’ll keep him employed (I haven’t been able to work since 2005). I didn’t know about cbd oil. My rheumy says he uses something called ‘hemp lotion’ for his arthritis–can’t remember what it’s called. as for narcotics, I’m back on the oxy’s now, and they barely take the edge off. I’ll have to look into this oil. You would think that docs here, educated in Philadelphia, would know about stuff like what you’ve mentioned. My doc, who I love dearly and does what he can, looked at me like a confused pup when I mentioned Low Dose Naltrexone! Said he’s not licensed to try Suboxone, so that’s out, too. And all the publicity regarding heroin and kids overdosing makes it tougher on those of us who are really suffering.
I’m always reading Cort’s informational articles and know I’ll never get to benefit from future findings, so all I can do is stockpile my oxy’s and muscle relaxants, and klonopin and know when I can’t take any more of the pain and isolation, I’ll have an ‘out.’ I just wish I didn’t have to deal with the chores of moving out of state and setting up in a hose that I’ll never leave. Not sure how it’s going to go–I have trouble driving 1/2 hour to the doctors–I guess my husband will just pick out a ranch house and move me into it! 😉
Has anyone tried the net 1000
where can you buy a Gammacore? Not finding and sales points on google ….
The reported that they hope to have FDA approval in the U.S. in 2016. They are approved for sale in Canada and some parts of Europe.
Hi everyone. I would love to be part of the continued development for the VNS unit. The amount of pain, the limits put on my life, the changes I’ve had to make are all so discouraging and overwhelming. I’m widowed with a special needs young adult child. It is so hard to take care of us, sometimes..well, most times. The meds have the worst side effects and the last one did me in. I would do almost anything to be a subject for the VNS unit.
My best to you all.
Canadian medical writer Norman Doidge wrote about VNS in his recent book, The Brain That Changes Itself.
http://www.theguardian.com/science/2015/feb/08/norman-doidge-brain-healing-neuroplasticity-interview
It’s a good general read looking at Neuroplasticity and the subjects of pain & fatigue . ME/CFS or Fibroare not mentioned specifically but you other neurological disorders are examined.
Thanks – it’s an amazing book…
Thanks so much Sean for this information!
I am still wondering why the ANS doesn’t work well. It could be due to bloodflow/vasculair problems this could be the cause of every symptom in ME/POTS patiënts. If the ANS react as a compensator it is very dangerous to use PNS stimulation.
That’s true. It depends on how it all got started. It also depends how it is used to some extent; it can have opposite effects depending on the intensity in some cases.
The company that sells gammaCore reported this:
Currently, the gammaCore is not FDA approved and not available for sale in the United States. While we anticipate FDA approval in 2016, please note that there is not a standard timeframe for when we can expect approval of the device in the US.
Currently, the gammaCore is available in Canada and parts of Europe including the UK, Germany, and Italy as well as Australia. The gammaCore device is intended for non-invasive stimulation of the vagus nerve in the neck.
GammaCore is indicated for the acute and/or prophylactic treatment of Migraine, Cluster headache, and Medication Overuse Headache (MOH) in adults. Although the device is CE marked in the EU for other indications including gastroparesis, anxiety, depression, epilepsy, and bronchoconstriction, our clinical work to date has been the areas of cluster headache and migraine.
If you would like to receive updates regarding product availability, please visit the contact us page on http://www.gammacore.com to sign up for our newsletter.
I have been diagnosed with CFS almost 28 years ago. I just came across Mind Alive Inc. Mindalive.com. I wonder if these products would stimulate vagus nerve.
Do you think that the electrode pads of a TENS unit would be able to be placed on the body in such a way to stimulate the Vagus Nerve?
If so, the units are cheap enough that it could be worth experimenting with.
Also, how would you know (and this question applies for all the various types of units out there) that the Vagus nerve was being stimulated?
Yes, I’m curious about that also. I have a TENS unit but the pads are too large (3.5 x 2 “) to go on my ear lobe.
Hmm, I’ll do some digging on the net.
I don’t think the TENS will work….
“Making the world’s first noninvasive nerve stimulator was quite an engineering challenge. Consider the signaling problem: The vagus nerve is made up of many individual nerve fibers of several different types, some transmitting signals up into the brain and some signaling down to the organs. Some do helpful things such as calming over excitation in the brain or signaling the spleen to reduce inflammation, but others do things that could be dangerous such as slowing your heart rate. The signal must be able to activate the “good” fibers while leaving the “bad” ones unchanged.”
http://spectrum.ieee.org/biomedical/devices/the-vagus-nerve-a-back-door-for-brain-hacking
What about the Alpha Stimson mi rocurrent electric stimulator, using earprobes?
I first used it almost 20 years ago and it did help me with chronic pain of FM. Cannabis oil with CBD and THC has also helped. I do have SIBO, intestinal motility problems which nothing helps.
Also, mast cell activation disorder. Currently I have a relapse of the flu and I am very ill because of it. Everything is more difficult because of these underlying diseases. No one understands, recognizes the severity of these illnesses. I am hoping this flu will resolve soon, it is making life unbearable.
I have a regular TENS/microcurrent unit that cost around $70. I got ear clips with it (most units will work with them) and all we need is the settings. I have noticed other models showing up on the market that are costing $650 and more for basically the same thing, and they are just capitalizing on the demand in this new field. What we need though is the settings for HZ and wave length. Got any ideas how to find that out?
I guess you get to be the guinea pig, lol. Please let us know if you find anything. Also, if you have any success trying different frequencies on your own.
That’s funny because TENS the Military was using in their trial with stimulating the Vagus Nerve, using acupuncture on the ear as a pathway, was a disposable one that lasted one week. I had to go in every week for 4 weeks and get new acupuncture needles on the opposite ear and a new TENS. They were trying to see if was good at relieving chronic pain. But as soon as I didn’t have the TENS, I no longer experienced relief. But it was enough proof for approval for step 2, the Vagal Block. In a prior article, which started this journey for
me, a woman was cured with a Block, and didn’t need the one they surgically implant.
After reading so much of the Dutch, British and Israeli research I have come across. More and
more, I am positive my downfall was caused by the Human Parvovirus B19, which was like the house that Jack built in my system that stays inflamed. That illusive inflammation they can’t find that has wreaked havoc on my body in forms of immunity, migraines, cancer, sensitivities, gut issues, kidneys, endocrine, pain, spasms, fatigue, lethargy, confusion, depression, female issues, insomnia. But now my body is responding maybe the beasties are hidden in our brain.
Dear Deborah, your experience supports what I was saying: that they can do this fairly cheaply and effectively, but are keeping it mysterious, I think to keep it expensive. Whoever it was that thought I could be the guinea pig was missing the point. I am asking if anyone who has had the benefits of this knows the settings, so those of us without 30-40 thousand dollars, or even $650 for “their” unit can still gain the benefits of this simple technique. Thanks to anyone reading this and responding. Thanks Deborah. warmly, js
Has anyone tried the brand available in Europe, or the units in USA? Would be helpful to hear experience. Along with all the stuff with ME/CFS I was also diagnosed with trigeminal neuralgia. I cannot describe the pain. It literally makes you sick to your stomach. I’ve been getting attacks on the right side of my face and jaw. If anyone has one of these machines, would love to hear their experience.
Cort,
Dr. Diana Driscoll believes the vagus nerve is involved in a number of mystery diseases and is featured on http://lowhistaminechef.com/. There’s a podcast on the page as well as a transcript of the interview. Definitely worth a listen!
TENS Settings in this study: http://www.brainstimjrnl.com/article/S1935-861X(14)00260-5/fulltext
The effects of tVNS parameters on autonomic function in 48 healthy participants were investigated using heart rate variability (HRV) and microneurography. tVNS was performed using a transcutaneous electrical nerve stimulation (TENS) machine and modified surface electrodes. Participants visited the laboratory once and received either active (200 μs, 30 Hz; n = 34) or sham (n = 14) stimulation.
Here’s the layman’s review of the study: http://www.eurekalert.org/pub_releases/2014-08/uol-ye081914.php
Here are two other studies that use 25hz and 25v (same measurement?) respectively:
http://www.cerbomed.com/upload/Poster_fMRI_evidence_Komisaruk.pdf
http://www.brainstimjrnl.com/article/S1935-861X(14)00260-5/fulltext
Hi Cort/all
Here is a query which I think is very pertinent to this topic. Firstly, I also feel Vagus is a prime suspect for my CFS issues – which also seem to include ‘dumping syndrome’ & Crohns disease, and also Bradycardia.
So my out loud thought is what are people’s views about this PNS stimulation approach, and the plethora of Flight or Fight calming approaches (Lightening, DNRS, Gupta, CBT etc..). It very much seems to me to be two sides to a coin. Im not sure of it is the same coin. I have not seen these discussed, or considered as a tandem treatment. Anyone have any ideas or experiences which combines these approaches?
I am seriously thinking about embarking on some Limbic retraining (not sure which one – does anyone have a pointer on where to get a comparison?), and also some TENS stimulation, for which I have ordered the kit.
Thoughts anyone? I would really appreciate any views.
Thanks
I would go for it Luther. The autonomic nervous system is one system that can be trained to a certain extent. Meditative breathing and similar activities do stimulate the PNS. My sense with collecting recovery stories is that quite a few of them involve people using these types of activities in addition to whatever else they are doing. I think they’re an excellent adjunct, and, if nothing else they can improve your quality of life. That said, they’re often not easy! Good luck!
And just a second query here. I was enthusing yesterday to my Paramedic mate about VnST, who got very concerned, as we are both already Bradycardic (I am a 20 year sufferer, so I don’t know whether that has been a factor; I know Tachycardia is more common).
He told tales of the risks from Carotid Massage, and he has managed to make me think twice about plugging my ears in.
One possibility is that the run away SNS already has the PNS maxed out, which is failing to manage the out of control SNS, but in the process is causing a bradycardic effect on the heart.
Does anyone have any thoughts on this theory, and whether we believe that VST actually holds any risks for CFS sufferers with Bradycardia.
Appreciate your thoughts and responses!
I don’t know about bradycardia but I would look into this further and take it very slowly (no pun intended :)) if you try this. I don’t remember exactly what they were but I was surprised at some of the effects on the SNS that the stimulation can cause.
Luther, I’ve read of many studies done where only the left tragus is stimulated because the right tragus is linked to the heart.
Whoa! I never cease to be amazed at the number and depth of comments on these articles, Cort. So much information, and a lot of pain and frustration, along with courage and determination. I want to encourage those who may not have noticed the link at the very end of your article, “see more here,” to check it out. The brochure titled “Vagus Nerve” has quite good information there. I tried a few of the breathing techniques; they did calm me down. I checked yoga “asanas” on AARP and another site showing a set of almost the same poses for those who are older and/or limited in motion. My IBS has worsened so much over this last six months, so I’d be willing to give both approaches (breath work and yoga) a try. I’m on heavy duty probiotics, though no ingredients to help them flourish, like FOS, which I will get. Also using digestive enzymes. Definitely something wrong with my small intestine, probably related to what Dr. David Fantle described in his initial comment above. Tramadol just makes it worse by slowing the motility down. I try to counter with different types of fiber and foods, but nothing seems to make anything better. I now get a strong “vasovagal” response whenever I use the toilet, whether constipation or diarrhea: vertigo, pain, upsurge in fatigue, increased heart rate above my already fast heart rate, irritability, brain fog, etc. I checked out Dr. Diana Driscoll’s site like CDS recommended. The ParaSym works through increasing acetylcholine. I cannot take that since it revs me and my digestive tract way up and I get diarrhea and overstimulated. However, if your body lacks it or isn’t sensitive to it, maybe it can help. I may consider buying one or both of Driscoll’s other supplements: one a digestive aid (site doesn’t even say what’s in it) and the other digestive enzymes (again does not indicate specifically which enzymes). Only the ParaSym has the complete information. Also, I have no gallbladder, but it’s been out for many years. However, I’m also wondering if I even manage to produce enough bile as I’m aging. Like everyone else here, I’ll just keep reading and trying things. :-/ All good wishes to each of you as you continue your journey with these illnesses. Thank you for your dedication, Cort! Cheers! Judith
Has anyone with CFS tried any products from Mind Alive Inc. Mindalive.com
Has anyone tried any of the machines themselves? Realistically can’t afford any of them, but the back pain has always been the worst pain and seems to have become permanent now. At my wits end 7 years in with no painkillers helping at all and no more avenues my doctors can/are willing to try.
There’s the neuvana xen at 400 dollars, and the carbomed nemos at 2500 euros. Quite a bit of a difference, and 400 is a lot for me, but if there’s going to be a substantial difference in effectiveness it seems saving for the better one would be prudent. Sadly there’s no information on the difference between the two. Any help would be appreciated
Looking at this one for my son who has long covid and sooooo many symptoms
https://arcmicrotech.com/product/arc4health-complete-kit/
TRY NUCCA for all these ailments. Especially vagas nerve stimulation. Type NUCCA DR in your google search and find one near you. OR Upper cervicle works as well.