



We’re going to take a deeper look at the oh so interesting field of small fiber neuropathy fibromyalgia (FM). A debate is raging over how big of a role SFN plays in FM. The central sensitization guys are saying probably “not much” while the immune oriented doctors/researchers believe the findings are telling us something new – and key – about fibromyalgia.
- Small fiber pathology—a culprit for many painful disorders? Nurcan Uceyler*2015 International Association for the Study of Pain n157 (2016) S60–S66.
- The Role and Importance of Small Fiber Neuropathy in Fibromyalgia Pain. Xavier J. Caro1 & Earl F. Winter. Curr Pain Headache Rep (2015) 19: 55
- What is the meaning of “small fiber neuropathy” in fibromyalgia? Daniel J. Clauw. International Association for the Study of Pain n157 (2016) November 2015·Volume 156·Number 11
They believe FM is not simply a central nervous system disorder. With studies showing damage to small nerve fibers in the skin in multiple places, they’re arguing that something systemic is causing nerve problems in many FM patients, and that something is probably the immune system.
First, let’s look at what nerve fibers are being affected and how they are being effected.
Those Small Nerve Fibers
Small nerve fibers are tiny, thinly myelinated or unmyelinated nerve fibers that convey sensory information such as touch, heat/cold and pain to the brain or regulate autonomic activities like blood pressure and sweating. These fibers generally stretch from an organ located just outside the spine called the dorsal root ganglia to the skin.
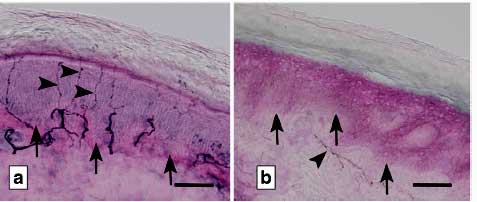
The first problem discovered in FM was fewer nerve fibers than usual in the skin. (The dark lines are the nerve fibers).
The problem that’s showing up is a reduced density of nerve fibers in the skin. Healthy people tend to have ten or more nerve fibers per ml of their skin. People with SFN have seven or less and some just less than three. Something is causing these small nerve fibers to disappear.
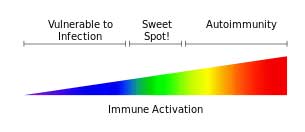
Since the density or number of pain sensing nerve fibers is reduced it’s not clear why many people with SFN experience increased pain instead of less pain. Several possibilities do exist, however.
Pain inhibiting nerve fibers could be selectively reduced leaving pain sensing nerve fibers more active, or the remaining nerve fibers could be more sensitive to inflammatory cytokines. It’s also possible that the sodium channels that transmit pain signals in the remaining nerve fibers could be hyperactive.
At least two types of small nerve fibers (A-delta and C-nerve fiber) with several subclasses (peptidergic, cholinergic, and adrenergic) are found. The work has not to my knowledge been done to determine if certain subclasses are effected in FM or if all of them are.
There is no doubt that central sensitization – the major finding in FM so far – plays a major role in FM. Central sensitization refers to a pathological magnification of pain signals by the central nervous system. The chicken and egg question facing the field now, however, is how to explain how nerve issues in the body cropped up in what has been assumed to be a central nervous system disorder.
A Central Sensitization Disorder?
“…this finding should be treated much like a herniated disc on magnetic resonance imaging, when accompanied by the appropriate findings on history and physical it may very well be responsible for pain, but it is also very often an incidental finding.” Daniel Clauw
Daniel Clauw is a major player in the fibromyalgia world. He deserves much thanks for his years of work to get FM accepted as a real illness. Clauw is an SFN skeptic and he’s not alone. Not long ago he provided an overview of FM which didn’t so much as mention SFN. Recently he provided a commentary on the role SFN plays in FM.
He pointed out that small fiber neuropathy has been found in most of the chronic pain conditions it’s been looked for in, and in conditions such as postural tachycardia syndrome (POTS) that are not associated with pain.
Clauw believes fibromyalgia is overwhelmingly as central nervous system disorder. He could be right.
Because damage to the periphery; i.e. the body often does not correlate with the amount of pain a person is in Clauw largely discounts the idea that SFN is the cause of, or is contributing to FM. The pain in FM, he believes, is largely a function of central nervous system dysfunction.
He rightly asks how damage to the nerves in the skin could account for the deeper feelings of pain or for the fatigue, sleep, cognitive and mood symptoms FM patients typically experience. These appear to be central nervous system type symptoms.
But Clauw also suggests the central nervous and peripheral nervous system problems could be linked; both could reflect hyperactive nervous systems, he believes.
At the end of his commentary, however, Clauw asserts that for now, at least, the SFN findings in FM are most likely to be “incidental”.
A Small Fiber Neuropathy / Immune Disorder?
Many of the considerations put forth within this article imply that we are entering an exciting era of shifting paradigms in this enigmatic disorder. Caro and Winter
Caro and Winter, two doctors who have treated FM patients for decades, provide another viewpoint. They point out that many of the therapies used in FM (pregabalin, gabapentin, and the tricyclic antidepressants) may actually be treating the SFN problems found in the disease.
Caro and Winter believe the immune system may be causing both the SFN and the central nervous system problems in FM
They note that there’s nothing incidental about a consistent loss of nerve fibers in the skin and now the corneas of FM patients. While Clauw questions whether the pain in FM is similar to that in people with SFN, Caro and Winter point out that the language FM patients often use to describe their pain (hot, burning, pins and needles, knife-like, unbearable, miserable) is very much the language of people with small fiber neuropathy.
They propose that the peripheral nerve issues in FM may, in fact, be worse, than currently thought. Besides the reduction in density of small nerve fibers in FM, Caro and Winter point to studies using techniques like quantitative sensory testing, sudomotor axon reflex testing, and microneurographic recordings which have found other problems with the peripheral nerves in FM. Their own findings of abnormalities to vibration, sensation and muscle weakness, indicate a “mixed fiber neuropathy” (MFN) consisting of both small and large fiber neuropathies may be present in many patients.
In fact, Caro and Winter reported they expect to publish a paper soon indicating that large fiber neuropathy is often found in their fibromyalgia patients as well.
New Diagnostic Criteria For Fibromyalgia?
They propose that clinicians should routinely examine FM patients for signs of nerve injury using the Wartenburg pinwheel and a 128-Hz tuning fork in their lower extremities. They report that almost 90% of their patients exhibit a “stocking distribution” which increased nerve problems the further one goes out from the trunk (i.e. in the feet and hands).
Caro and Winter have gone so far as to use SFN findings to diagnose and subset their patients. They describe three subsets of FM patients they’ve found.
FM Patients with Normal Nerve Fiber Densities
They believe that FM patients with normal nerve densities often have another, hidden disease such as rheumatoid arthritis or osteoarthritis. They pointed to the case of a 21 year old college student with FM whose pain responded to Cymbalta but not to Neurontin or Lyrica. (The lack of response to Neurontin/Lyrica was apparently something of a clue that SFN may not have been present.)
The normal nerve fiber levels in her skin biopsy prompted them to look for a pain generator other than SFN. Tests indicated she had elevated C-reactive protein levels (but normal sedimentation rate, rheumatoid factor, CCP-IgG, and antinuclear antibodies). With her history of early morning stiffness and small joint pain they diagnosed her as having early “seronegative rheumatoid arthritis.”
She was successfully treated using a tapered regimen of steroids, hydroxychloroquine, and an immune modulating biologic drug called Orencia (abatacep).
FM Patients With Very Low Densities (< 3.0 fibers per ml) of Nerve Fibers
The belief is that FM patients with very low (< 3.0 fibers per ml) small nerve fiber densities in their skin have another condition known to produce SFN. These conditions include diabetes mellitus, untreated Vitamin B-12 deficiency, an autoimmune/connective tissue disorder (Sjogren’s, lupus, scleroderma, etc.), infection, metabolic disorder (hypothyroidism) toxins and others. The treatment protocol for these patients is to identify the undiagnosed disorder and treat it.
FM Patients With Low Densities of Nerve Fibers (< 7.0 per ml) Who Do Not Have Another Condition
Absent the identification of another disease, Caro and Winter propose that the immune system is largely driving the small and large fiber neuropathy seen in FM. Since the immune system is often implicated in tissue injuries it makes sense, they assert, to assume that it probably plays a role in the small nerve problems found as well. They report that a substantial number of their FM patients respond to immune therapies such as IVIG.
Caro and Winter end their review by asking if in some people FM presages inflammatory disorders such as rheumatoid arthritis or if it exists in a kind of limbo between better defined disorders. They suggest that the gastrointestinal microbiome would be the most likely place to look for the source of the inflammatory activities they believe may be causing FM.
- For more on SFN and Fibromyalgia see – the Small Fiber Neuropathy (SFN) Resource Page for Fibromyalgia







About the time I was in early stages of FM in the 1980s, I developed another problem that the doctor described as my having too many nerve endings. This was long before any studies were done, or interest was put, on FM. I was diagnosed later, in addition, with seronegative rheumatoid arthritis. Unfortunately I was never tested properly in the last few years as the high cost of my drugs has interrupted any FM testing. With so much time gone by, and new methods of testing available, I would love to be able to see a specialist in ME/CFS or FM to get some current information.
I find all of the new studies very interesting, yet I refuse to take Lyrica or Cymbalta (and my doctors agree) because I don’t want the chemicals in my body. I do have to take 2400 mg of Neurontin daily, but that was given to me in the 1990s for restless leg syndrome. It was not yet used for FM and other painful diseases and syndromes. I have no idea, therefore, if Neurontin does anything for me other than help with RLS — and it does help me very much. Interesting stuff!
I so look forward to this newsletter and getting a better understanding of what we are all going through. Keep researching.
Thanks!
Oh, my…another “maybe, maybe not” scenario. I guess time will tell, with further research, if SFN does play a significant role in FM. I’m of firm belief that for sure the CNS (sensitization), immune system and gastrointestinal microbiome definitely do. My IBS/gastrointestinal issues directly cause vasovagal activation, and they’re worsening with age: increased rapid heartbeat, orthostatic hypotension symptoms, sweating, vertigo, increased pain. However, my pain can increase w/o any gastrointestinal activation by simply doing physical activity, like house chores. This is off subject, but I bought one packet of PEA Pure capsules from The Netherlands. This was discussed in another Health Rising article awhile back. I only took one in the a.m. with my Cymbalta. I didn’t want to spend $160.00 for the multi-pack unless I thought it would help, so that’s why I only took one/day. $160 is still too much money for my tight budget, but I went ahead and ordered them. With the increase to two pills/day over a longer period of time, I’ll be able to more objectively evaluate whether or not they do help. If there’s not a significant difference after some months, I won’t buy them anymore. It’s possible the dose may need to be even higher than that. I have to find that article again and check what dosage people said they took in the comments section. Cheers! Judith
Good luck with the PEA Judith!
Have you looked into Ehlers-Danlos syndrome? I have been dx with that after years of various dx of RSD, Fibromyalgia (both now in remission) and Dystonia. My variants of chronic pain conditions may all spring from a “parent organization” of EDS in addition to an epigenetic trigger from trauma in my youth. I believe there is a genetic cause but also severe trauma makes me more susceptible to illness.
Wow, a Wartenburg pinwheel! I haven’t seen one of those used for sensory testing since medical school in the mid-80’s. In this age of HIV and multiple types of transmissible viral hepatitis, they were all throw away in favor of good, old-fashioned, disposable, safety pins!
SFN is certainly helpful to understanding FM as a disorder affecting the body tissues themselves, not just “central nervous sensitization”. But more very helpful findings have been emerging regarding the knots / clumps / Trigger Points in muscle and myofascial tissue. Those adhering to the “central sensitization” hypothesis have still more answering to do. Hands-on therapists like massage therapists have long been familiar with the abnormalities in FM patients muscle tissue, in fact this is not really controversial at all even in mainstream medicine.
http://www.fmcmpd.org/physinfo.htm
I could extract a dozen paragraphs that make complete sense regarding “the way I feel”, but to keep it brief and focused:
“…As myofascia twists and sticks to other tissues, it can entrap nerves, blood and lymph vessels…”
“…Inside the TrP (Trigger Point) zone, there is a region of extreme hypoxia consistent with capillary compression, but tissue outside TrP zones are normal…”
“…local twitch response (LTR) releases irritating chemicals into the interstitial fluid around the TrP. An LTR from an active TrP sends forth a “sensitizing soup” of over 30 biochemicals, including significant amounts of bradykinins, calcitonin gene-related peptide, IL- α, serotonin, tumor necrosis factor and norepinephrine, and the pH of the area dropped to about 5. Substance P and CGRP dropped significantly after the LTR. (Shah JP, Phillips TM, Danoff JV et al. 2005) The pH drop and release of irritating biochemicals are sufficient to change the pain sensitivity in the TrP area. Taut bands and TrPs have been imaged at the Mayo Clinic and the National Institutes of Health…”…
I only have had to thank a lot to CortJohnson . I have FM since 2005 and this website have given me the most important news about this terrible disease FM.
I still have some hope that de FM cure will be discovery and Cort Johnson will bring us this fabulous news.
Thanks Juliana…I fervently hope your wish will come true. 🙂
Hmmm…more complexities. I must have the SFN subset symptoms, what I call neuro feet, they describe, of burning, freezing, crushing, pins-and-needles, unbearable is an appropriate word, in addition to “regular” deep muscle pain. 20 mg Cymbalta put a maybe 10% curtain between me and my neuro pain but I developed a weird side effect and d/ced it. 300 Neurontin did nothing for five days but then also gave me a different weird scary side effect so also d/ced. This week I started 50 mg of Lyrica at night. Knocked me out first night, woke up wtf dopey for a few hours but…almost no pain of any type until 2 PM. The first time I’ve felt almost normal in two years, couldn’t believe it, like a miracle. Second night of use…back to usual bad sleep, also dopey for a few hours…zero pain relief. Last night modest sleep help, dopey a few hours…pretty fair pain relief until about two when I tried another 50 mg. Bam…dopey, the seventh dwarf, sleep for an hour, some pain diminished ment, added Tramadol/ Tylenol. Will continue Lyrica now twice daily for a while. It looks like the med you will like to hate, may bring pain relief but no driving, thinking, maybe urinating, congestion…Hobson’s choice. Not cool. So is this SFN?
Did they test people with ME//CFS for SFN? I have had both for years. My impression was that of ME/CFS and FM, they had just tested people with FM. Then it seems they go galloping off with hypotheses before doing more research testing. This seems to happen pretty often. Research is expensive but hypothesizing is less so. It is kind of a boom and bust cycle for those on the sidelines, wanting hope of a breakthrough. It is important to keep in mind what has been suggested or demonstrated by research, depending on what kind and how many studies, and what is still just hypothesizing.
Right Cecelia. I think it’s pretty clear that SFN is present in a significant subset (but certainly not all) FM patients but what’s causing it – that’s all guess work right now.
Some people with ME/CFS are being tested and do have. We had a comment in the last blog from a person with ME/CS that that’s happening. I wouldn’t be surprised given my symptoms if I have some.
I believe it is possible, by the way, for these nerves to grow back.
No studies have been done on ME/CFS yet.
I’m Bob from the last post. There are two tests for SFN one simple and one not-so-simple. The simple one is a skin punch biospy. A small portion of skin biopsied near the ankle, takes a minute to perform and then just wait for the test results.
The second is a surrel nerve biopsy which involves surgery (cutting out a portion of a nerve that runs down to your foot.)
I’ve had both and both gave the same results. I would recommend the skin biopsy (cheap and effective) if at all possible.
The surrel nerve biopsy leaves part of your foot numb (no nerve.)
But as I told my doc; you can cut my foot off if it means restoring the rest of my body to full health.
If you want to get rid of this you need to completely cut out sugar, wheat, & meat. You’re gut’s natural microbiom has been partly destroyed by the accumulation of bad bacteria which is caused by antibiotics. Sugar, yeast & wheat products increase the bad bacteria until the walls of your intestine have become permeable. Foods leak into your blood comromising your immune system. It causes all sorts of health problems from thrush to cancer.
You need to take a good probiotics every day on an empty stomach. Sauerkraut & kefir are also good to reintroduce good bacteria into the gut. Oregano oil, garlic & pau,darco herbal tea are great for killing off the bad bacteria. Its a long hard slog but its worth it to gain good health, especially if you suffer from chronic pain from nueropathy (or any chronic pain).
Follow GreenMedInfo.com & read its founder Sayer Jay”s articles for some well researched studies on this subject. Read ‘The China Study’ too for some extensive research on the link between what we eat & diseases.
I also go swimming. I think keeping active increases your metabolism & blood flow to the nerves. It all worked for me. I suffered from severe nueropathy in my feet which was so bad I became immobile. I can now walk for a good couple of hours without pain & am getting very near being back to fully recovered.
Good luck!
Thanks Eileen, I really think that everyone with these disorders should give dietary changes and fermented foods and probiotics a try. I’ve done well with home-made kefir and avoiding wheat is a must.
I know this sounds so morbid, but living near Emory University, here in Atlanta GA U.S. They have a medical school, and I know of quite a few people who have “willed” their bodies to Emory Medical School for study purposes. Has any researcher ever thought to study our bodies thoroughly that way. Our brains, the vagus nerve, the spinal cord, substance P, our every thing, that might be highly intrusive if we were living. It’s like we good child developmentalist study Piaget, and his theories on children, their behavior, best practices for learning and positive reinforcement, why Piaget actually studied children to learn about children not dogs and chimps. Maybe our inner body, our brains, nervous system and spine which is somewhat hidden actually might lead to break through. Because I feel like I am the proverbial elephant and my Doctors are the blind. I am told also by statistician in order to get a true sampling you need 1500 individuals to prove a hypothesis statement. Like when I tried to prove my new approach to delivery of Social Services, I only got to 700 plus Families with 88% positive, but it was not proof. Here we have researchers with a sampling as little as 28, I read once. Thus in studying the whole body that way maybe many Specialities could come together and learn as they did when they first learned.
Funny, I often think of willing my body to science and writing on my body with different Magic Markers, “look here, terrible gluteal pain for twenty years, what was it” and stuff like that.
I am an 81 1/2 year old woman who has been in pain for 20+ yrs.
I started with Peripheral Neuropathy, small fiber poly neuropathies, FM, and now Dystonia. My skin is covered in warts. and many other kinds of spots…embarrasing. The dermatologist like to say I was out in the sun too much in early life. I have tried so many meds that has not helped yet. Lyrica worked for a short time as I gained 15 lbs. in six weeks so I was taken off of it. I am to the point where I don’t feel bowel movements. My food is slow to digest. and I have no immune system left. Of all the problems, the Dystonia is the worse right now. I get no night sleep as my legs, feet and hands keep cramping like “charlie horses” all night. You try to stand up and walk the cramps off, but your toes are in different directions and can only stand on the side of your feet until the cramp stops. I hope they find a new med soon as I am too old for all of this pain.
Good luck Gerrie! I wonder if your slow digestion is due to autonomic nervous system problems that keep the food in your gut from moving along? Have you tried probiotics or dietary changes?
Yes, Cort, I take probiotics each day. I have yet to figure out why I have so many problems. My Dad had CI
DPN and after a year of it, he developed Multiple Myeloma
and passed away. Didn’t want his kind of neuropathy, but I sure don’t want mine either. I have had these problems for so long, that sometimes, because of the slow digestion, I feel nauseated, but just take a nausea pill.
I have a pharmacy to choose from for every problem. Some work, most don’t.
Has anyone had any experience with using 35% food grade hydrogen peroxide? I have heard some positive reports but would like to get a bit more feedback. Thanks