

Lactate (L-lactate) is an organic compound produced during anaerobic energy metabolism. It’s constantly being formed – even when we are at rest – but is formed in higher quantities when ATP levels are low and anaerobic energy metabolism is high. Several forms of lactate are also produced by anaerobic bacteria in the gut.
Lactate in small amounts is not bad – it actually reduces muscle fatigue – but the presence of high levels of lactate (lactic acid) signal that the anaerobic energy production process – which produces toxic metabolites that cause pain and fatigue – is in full bore.
Lactic acidosis is a state of low pH accompanied by high lactate levels. It most commonly occurs in its temporary form after excessive exercise but is found in a more permanent form in people with illnesses which produce low oxygen levels (hypoxia/hypoperfusion) including heart or lung disease, sepsis, severe physical trauma, shock, Vit B deficiency, or interestingly enough, decreased blood volume. Symptoms include a burning feeling in the muscles, muscle weakness, rapid breathing, nausea and vomiting.
The question this blog asks is whether the processes that produce lactate/lactic acid levels could be causing pain, fatigue, cognitive and other symptoms in fibromyalgia and/or chronic fatigue syndrome.
First a look at the gut.
The Gut
D-lactic acidosis is a different form of lactic acidosis caused by the production of D-lactate by bacteria in the gut. Two forms of lactate are produced in the gut. L-lactate in the gut is considered benign but the D-lactate hypothesis posits that D-lactate contributes to leaky gut problems. It proposes that once D-lactate gets into the blood it can push its way through the blood-brain barrier into the brain where it can cause neurological symptoms including feelings of panic, hyperventilation, delirium, ataxia and slurred speech.
Reducing the levels of streptococcus bacteria in some ME/CFS patients resulted in improved sleep and vigor.
This study reported on the effects of using an antibiotic to reduce Streptococcus bacteria levels in 21 ME/CFS patients. Prior tests indicated that these patients – out of about 75 – had increased Streptococcus and/or Enterococcus bacteria. Streptococcus spp. tend to produce lactic acid, including the D-lactic form which has been associated with increased gut permeability.
After the 21 ME/CFS patients were given an antibiotic, erythromycin, to reduce the levels of lactic-acid producing bacteria in the gut, their sleep patterns were measured using an actigraph. Fecal samples were taken after the antibiotic.
Of the 21 ME/CFS with increased bacterial levels, tests indicated significant declines in Streptococcus spp. in a third of patients. The patients with reduced Streptococcus spp. levels slept about 45 minutes longer each day and reported improved vigor. It was expected, given the results of other studies, that mood measures, in particular anxiety, might improve, but that did not happen.
Antibiotic treatment alone was not sufficient to significantly alter the Streptococcus levels in the other ME/CFS patients, and increased sleep times or vigor were not seen in these patients.
Erythromycin – a broad spectrum antibiotic – also reduced Lactobacillus and Bifidobacterium levels in some patients – possibly putting their flora further out of balance.
The authors believed that the central finding of the study – that antibiotic treatments can reduce Streptococcus bacterial levels and improve sleep and vigor in some ME/CFS patients – supported the D-lactate hypothesis. (They did not directly measure lactate levels in the blood or urine). Antibiotic treatment was not effective in lowering Streptococcus levels in most patients, however, and it may disrupt the flora of other bacterial species, including, presumably, some beneficial ones.
Several factors prevented the study from being definitive. It was small and because it was an open-label study, it was impossible to disentangle placebo effects from the effects of the antibiotic. Actigraphy is also unable to measure restorative vs non-restorative sleep.
(Antibiotics are not the only way to reduce levels of D-lactate producing bacteria in the gut. Galland reports a case of a man with short bowel syndrome and D-lactic acidosis for whom antibiotics and dietary restrictions failed. The use of two probiotics, Bifidobacterium breve Yakult and Lactobacillus casei Shirota and the prebiotic galacto-oligosaccharide worked by limiting the growth of D-lactate producing bacteria. )
The Brain
In fact several studies do suggest lactate may be causing problems in chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM). Sheedy’s 2009 study found that two species (E. faecalis and S. sanguinis) found in ME/CFS patients guts were high D-lactic acid producers.
Shungu believes the increased lactate levels he has twice found in the brains of ME/CFS patients may result from reduced oxygen levels. He believes increased oxidative stress may release substances called isoprostanes which restrict the blood vessels in the brain. Those constricted blood vessels result in low oxygen levels (hypoxia), anaerobic energy production and the release of lactate.
In a small study Baraniuk subsequently tied increased brain lactate levels in Gulf War Syndrome to reduced cognition. A subset of GWS patients with increased brain lactate levels prior to exercise demonstrated significantly reduced cognition after exercise. Baraniuk attributed the cognitive decline to the brains inability to utilize the lactate produced by the muscles during exercise. The inability to use the energy resource that lactate presented resulted in the brain using anaerobic metabolism to try and meet its needs.
The Muscles
Fibromyalgia
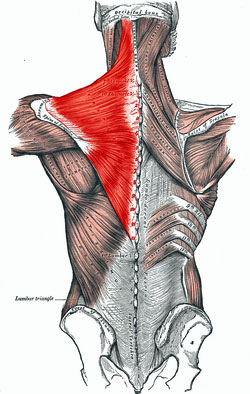
Significantly higher elevations of lactate have been found in the trapezius muscle of fibromyalgia patients and in women with chronic widespread pain – a condition similar to FM.
While many lactate studies in FM have not been done some studies suggest that the conditions for increased lactate production such as low muscle oxygen levels (hypoxia) may be present.
Reduced oxygen intake during exercise was recently associated with increased pain in FM. Hypoxic conditions in the skin above tender points are present. Reduced capillary density, altered microcirculation and decreased muscle blood flows could help explain that finding.
Because muscle ischemia/hypoxia (low oxygen conditions) are associated with increased pain, it’s been suggested that they could be driving the central sensitization found in FM. (Staud points out that a more acidic mileu in the muscles – possibly produced by low oxygen conditions in FM – primes the pain receptors in the muscles to act up.)
EEG studies suggest the muscles in FM have trouble relaxing, causing them to stay in a more contracted state – a state that can be associated with hypoxia and causes increased pain sensitivity. Another study suggested that deficient activation of the muscle units could be causing fatigue and leading to pain.
Mitochondrial problems are another possible cause of the increased lactate found in the muscles. Enlarged mitochondria, structural muscle abnormalities and reduced numbers of mitochondria all suggested “increased muscle stress” was present. Biopsies of the trapezius muscle in FM have shown signs of mitochondrial disturbances.
Chronic Fatigue Syndrome (ME/CFS)
A computer model of exercise intolerance caused by mitochondrial dysfunction in ME/CFS predicts increased lactate production in the muscles will occur.
Lane found increased muscle lactate production in ME/CFS three times. The third time he linked it to the presence of enteroviral RNA in the muscles.
Newton has shown that people with ME/CFS produce up to 20 times more acid and have more difficulty removing acids from their muscles during exercise. In a rather remarkable study Newton linked muscle pH issues in ME/CFS with hyperventilation and reduced oxygenation of the brain. Nijs’s finding that recovery of muscle function after exercise was associated with improved cognition suggested that muscle problems and brain functioning may be linked.
Numerous other studies, of course, have found problems with energy metabolism during exercise in chronic fatigue syndrome.
The Lactate Question
The lactate question ends up not being a question about lactate per se, but about whether widespread problems with anaerobic energy production are found in the brains, muscles and/or guts of FM and ME/CFS patients. Multiple studies in both diseases suggest that they may. High lactate or similar problems have been found in multiple areas in patients with ME/CFS and in the muscles of FM patients.

Numerous studies on the other hand suggest that widespread low oxygen conditions could be causing a variety of problems including reduced energy production, muscle issues, increased pain and fatigue and cognitive problems in ME/CFS and FM.






Supplemental oxygen is likely to help this. Also helpful in practice based on my own experience and the experience of many people I know.
Can you say more about supplemental oxygen? Are you talking about a CPAP
Machine, hyperbaric oxygen, or literally oxygen with a cannula? I’m about to do a sleep study with the hopes they will
Let me try a CPAP machine for this very purpose (severe fibro). Oxygen supplementation makes a lot of sense to me. There are no locations for hyperbaric oxygen treatment near me. Thanks!
Increased oxygen intake would help when the red blood cells are blocked in the capilliaries, for the few oxygen carriers that can get through, but the real question is – why are the RBCs deformed and unable to deliver the oxgen that is already available?
A breakthrough in ME research would be incredible, my vote would go to Alaedini’s research suggesting that the ME/CFS patients response to gluten was different than seen in coeliac disease. In 1977 after a duodenal biopsy I was told, ‘You are a coeliac and you are not a coeliac’. Are Alaedini’s findings the key to help clarify this? My response to gluten is extreme and it includes oxygen deprivation to all vital organs as well as muscle.
Quote from the article; “Celiac disease is clearly characterized by antibodies to an enzyme called transglutaminase 2 enzyme. One study reported that these antibodies are so prevalent in celiac disease that they exhibit “extraordinar(ily) high …. specificity and sensitivity” for a disease.
They’re not present in ME/CFS, though. Something else is happening. In fact, Alaedini believes the response to gluten he’s seen in ME/CFS may be unique to the disorder. (ME/CFS just HAD to be different (lol)). That perhaps doesn’t surprise patients who have found their disease fall through the cracks again and again but it does set the stage for a possibly exciting (and newsworthy) finding. Given the interest in celiac disease and gluten intolerance a novel finding in ME/CFS would be sure to spark considerable interest”.
Yes, yes, yes. It does spark considerable interest, it is the most exciting finding I have heard in the past 40 years of gluten free ME/CFS.
Please, please, expand on it.
except that i don’t do gluten and still have either chronic fatigue or fibo-
While you testing for Coeliac disease and reaction to gluten why don’t you test for Candida Antibodies. Candida loves oxygen and deprives alls cells red or muscle of oxygen. It destroys oxygen as it did to me during my illness. It wasn’t until I destroyed or did a Candida Kill off that I my cells could get any O2. See the link to my site further down. coconutcreamcare.com
Are You Fermenting?
Consider testing for MTHFR, DNA mutation.
How do I get my doctor to prescribe supplemental oxygen and what form is most beneficial of it? Will insurance cover it?
follow
Both acute and chronic muscle spasms generate tissue anoxia, lactate production, reactive substances like Substance P, and peripheral neural pain transducer stimulation. Fibromyalgia sufferers harbor widespread chronically spastic soft tissues that hurt during locomotion and when directly pressed. What more needs to be understood about Fibromyalgia pain generation than why these soft tissues are spastic? This question has been answered by this Commentor at his various blog sites at G+ and Quora.
Thanks Laurence. Didn’t know that substance P could be involved. Feel free to drop a link to your blog sites if you wish.
Would then the protocol using 35% food grade perhaps be helpful for fibromyalgia sufferers as its main claim is oxygenating the body. I am trying it at the moment as I have found nothing that has helped my symptoms. Has anyone else tried the 1 minute cure protocol or similar? I would be very interested as it is quite a challenging protocol.
I think it probably depends on what the cause of the hypoxia, if present, is. Dr. De Meirleir has said that oxygen supplementation can be helpful but only temporarily as it does not address the cause – which could be vasoconstricted blood vessels, acid dumping into the bloodstream aka Newton’s hypothesis, if I got it right, Pall’s hypothesis of run away oxidative stress or I’m sure any number of other possibilities.
This latest research, through the links and further references, Cort, is very confirming and I believe it is heading in the right direction.
Muscles are being deprived of oxygen by the tension, knots and adhesions. Lactate is everywhere, which would be consistent with muscles operating anaerobically far more of the time than would be normal. But what comes first, the cart or the horse? FM sufferers are in a vicious circle, these problems must all affect and worsen each other – but what started the process off in the first place?
Stress, failure to breathe normally when pre-occupied during the day, inappropriate posture and muscle loads, infections, toxins – all potential causes. Maybe it is combinations of too many such factors, that is the initial problem. Different researchers and practitioners tend to be focused on one aspect. My naturopath says it is infections and toxins. Now a “body mechanics” therapist I am going to, says it always was inappropriate posture and muscle loads. Others have always said stress. I say all of these things were issues with me, maybe the absence of any one of them would have preserved me from FM?
Yes, it’s multi-factored. 99% of practitioners are clueless. The key to recovery is a diverse, multi-factored, concurrent approach.
Thank you Cort, this is very interesting. Oxygen is definitely a part of the equation for me. If I need to be mentally sharp and reduce brain fog, I do deep breathing exercises (you might even call it hyperventilating!) Also, I feel better when I’m outside. Conversely, when I’m crashing, my breathing is extremely shallow, and I experience “air hunger”.
Such a bizarre illness. All these findings and still no one can solve the puzzle…
http://dailymedicalresearch.com/fibromyalgia-mystery-finally-solved-2/
http://dailymedicalresearch.com/little-known-high-tech-treatment-could-be-answer-to-fibromyalgia-mystery-researchers-say/
This makes SOOOO much sence! Has anyone seen these two links? If you get a chance to read then, you will see so many similarities in what we are talking about here!!
Fellow FM sufferers, I think we are on the cusp so something GREAT!!!! PRAISE JESUS!! HALLELULAJ!!!!!
‘and still no one can solve the puzzle’
I’m not sure how much research you do on solutions, but many people have many answers. People recover all the time, literally all the time.
The puzzle starts with the degradation of the mitochondria, which occurs in ME/CFS. The mitochondria are the cells responsible for converting food into usable energy for the brain and whole body. There is also recent research that shows the brains of ME/CFS patients are higher I. Temperature than healthy brains, which also leads to a myriad of system imbalances. You might want to lookup this article:Mitochondrial Dysfunction and Chronic Disease: Treatment With Natural Supplements
Garth L. Nicolson, PhD
Does anyone else here feel as if their regular / non-specialist doctor just doesn’t listen anymore when the word “Fibromyalgia” comes out of your mouth? Doctors seem to know that whatever is going on in Fibromyalgia is so complicated, that they just … they don’t care. My doctor just told me to take massive doses of pain medicine as a preventative measure to pain. I can’t help wondering if I am doing damage to my liver, stomach, or whatever else is affected by massive doses of pain medicines. I know that there is still so much unknown about Fibromyalgia, so some doctors feel kind of helpless when they hear that word, but I feel discouraged that when I talked with my doctor about this last year, she really did not suggest trying any other measures to figure out what is going on.
Amanda, I totally agree. My doctor is just like, “here it goes again.” I have the most minimal amnt of pain medicine (he doesn’t like prescribing it for chronic-pain sufferers) and has told me many times that a person isn’t meant to be pain free. I understand that, I can deal with a certain amount, but because it’s fibromyalgia, I get the eye roll.
So frustrating!
In the early 70’s I lived near an oil refinery and farm lands, noxious gases from the refinery and aerial agricultural spray resulted in repeated gastric attacks which were treated with antibiotics. Result – Candida albicans overgrowth and subsequent leaky gut caused by penetration of the gut wall. Result – lots of macro molecule food particles that caused severe food intolerance reactions and a hyperactive immune system.
Result – many blood changes, especially in the mobility of red blood cells, enlarged and clumping together – the delivery of oxygen to all areas, through fine capilliaries, was severely impeded. Result – lactate formation due to imperfect breakdown of glucose in the reduced oxygen supply.
On WebMD site it states “When you exercise, your body uses oxygen to break down glucose for energy. During intense exercise, there may not be enough oxygen available to complete the process, so a substance called lactate is made. Your body can convert this lactate to energy without using oxygen. But this lactate or lactic acid can build up in your bloodstream faster than you can burn it off. The point when lactic acid starts to build up is called the “lactate threshold.”
About 30 years ago a researcher using an electron microscope found the above blood changes in marathon runners and also in ME patients, the difference was the runners took 4 hours to return to normal and the ME patients 5 days.
The effect of enlarged and clumped red blood cells is widespread affecting all organs of the body including skin, lungs, heart, short of breath, headaches, gut and liver changes, acidosis, fatigue etc. etc.But ME sufferers don’t need to run a marathon for this to happen, do they?
I asked, “Why is this not recognised?”
A doctor’s answer, “Because we don’t know how to treat it, so it has been swept under the carpet”.
Very good response Audrey. Candida Yeast overgrowth is the cause of forcing your body to create lactate acid since the Yeast hates oxygen and destroys oxygen before your body can use it. The more sugar you eat the stronger the Yeast gets for it feeds off sugar and creates sugar addiction in a demand for more. I too suffered from Candida Yeast overgrowth and became so weak I could barely walk. I had air hunger and had to hyperventilate to get any O2. I spent 8 days in the hospital they didn’t know what to do until I demanded an colonoscopy and that is when they found yeast in my throat.
Read my story and my article http://coconutcreamcare.com/2016/01/10/are-you-fermenting/
Thank You
Joan
Thank You
That’s an amazing story Joan. Thanks for sharing that. From what I gather anti-fungal medications and diet played a major role in your return to health. Anything else?
Nothing replaces personal experience Joan even when termed empirical. Read your article, excellent, thank you, Orion Truss ‘The Hidden Diagnosis’ was the first to bring Candida Albicans to my notice.
I was on a very low carb diet of 16 ingredients, 4 a day and repeat for 7 years, plus continuous anti-fungals, both Nystatin and Ketaconazole.
I found I had to cook my food in oil to slow down the absorption of carbohydrates.
Two steps was exhausting especially up stairs then rest, felt as though wearing deep sea divers boots. Diagnosed as Coeliac then ME & Immune dysfunction. Food & chemical sensitivity made life almost impossible; but slowly improved until 10 years later was given a cardiac stress test, told to ‘keep going, keep going’ even when only my arms were holding me upright, the air hunger was extreme with whooping (as in cough)in breaths, this only engendered the criticism & disdain of the consultant, he seemed to think I was acting! Then an angiogram – 3 arteries almost closed, but was it a reaction to the Xray contrast? Triple bypass and post op convusions due to injected heparin, plastic tubing, ECG leads, Xray chemicals, (2 punctured lungs) cleaning fluids etc.
Ok it is a long complicated story but I still think it started with the overuse of antibiotics and interference with the gut flora causing colonisation with Candida Albicans.
A modern problem – babies pick up Candida & other friendly bacteria during a vaginal birth, which is good and necessary, but NOT during a Caesarean Section, this is now belatedly showing some distressing results.
Yes Acid, gas and alcohol ruined quite a bit of my life within the whole ME/CFSyndrome, in Japan they called it ‘Drunken man’s disease’
Thanks again for your excellent article, like you still mainly controlling it with diet.
Yes Audrey diet but also many many herbal, oil and essential oils I have a neck and back of head itch drives me crazy at times but I am breathing free my sinus are almost clear my nose use to cold all the time its getting to be normal. I have been cold for years nice to take a deep breath and have a clear head. I was diagnosed with COPD. So much for that and Diagnosis. I couldn’t blow up his stilly machine because I was full of oxygen hating Candida.
Joan,
Thanks for the hopeful story!
What herbs and essential oils do you use to treat candida?
Do you use any as a nasal wash?
Sorry Terry I just saw your question. I am new to essential oils and I am exploring just getting started my real purpose is my kitty cat who has some issues the vet has dismissed and given up on her since I won’t pay for the exploratory stuff she wants to do. Anyway because Candida releases over 84 toxins when it dies I have gone threw a long list of things. For the nose I’m using good ol’ sea salt mixed maybe some tree oil and hot water. I also use a lot of silver. I also have gone thru a long list of oils coconut, sesame, Castor, Mustard apple cider vinegar etc. etc. I have chased the yeast out of my organs and now its in the sinus and for some reason the back of the neck. I guess the best thing to say is you name it and I have tried it.
My symptom flares include reactive muscle pain and reduced cognitive function. These two symptoms never seem to increase or decrease independently of one another. My muscles are unusually reactive in general to ordinary activities and I also experienced long term/permanent complications following a treadmill stress test. I believe there is no question of a connection and it is only a matter of testing, however when I consulted one of the supposed CFS/ME experts involved in the recent NIH talks, he blew me off, totally ignoring these and other symptoms and their association, which prevented my being included in important studies for which the illness will be defined. What good does it do when “experts” are unwilling to include exemplary examples of long term consequences of the disease?
Yes Cort
Plant based foods to start, then bitter food, I did not have any anti-fungal medications it was all food. It is four years later I’m not Yeast free it is still hanging out in my sinuses but I’m strong and feel like I have found the fountain of youth. Using Herbs and different oils. I am breathing better than I have for years.
Joan
I have been telling my doctors for years that my muscles feel like they are not getting the nutrients and oxygen they need, and that muscle overuse always leads to worsening of all FMS symptoms, which are identical to Overtraining Syndrome.
As an ex-competitive cyclist, I know and tolerated the muscle burn from going anaerobic. Fibromyalgia is that same burn, only all the time, without doing any exercise. And because that burn is all the time, you get a permanent state of Overtraining Syndrome (Fibromyalgia).
The stress that started my fibromyalgia came from daily training while my Testosterone and Growth Hormone levels were very low due to a pituitary gland problem called Empty Sella Syndrome.
Before my fibromyalgia became permanent on one specific day, I had been battling for 6 years, a lower level of Overtraining Syndrome that would come and go.
My ability to workout was greatly diminished, but not as bad as after that one day when I knew something went horribly wrong inside. When a 20 minute walk took 3 weeks to recover from, and left me in a severely Zoned – Out Daze for weeks.
I was a Zombie, lights are on but nobody’s home, shell of a person. If someone had broken into my house, I would not have been able to react, and the stress would most likely have done me in, as I could no longer tolerate stress as before.
I was disabled in every sense of the word, and not one doctor gave a damn.
I researched my symptoms and mentioned to my first doctor it felt like CSF. He made a note of that but no diagnosis. 25 doctors later I finally got the right diagnosis and treatment. But by then everything was permanent, and I lost my ability to function normally.
I certainly recognize ‘the burn’ David. Hopefully, this will not turn out to be permanent though. Good luck with everything.
“When a 20 minute walk took 3 weeks to recover from, and left me in a severely Zoned – Out Daze for weeks.
I was a Zombie, lights are on but nobody’s home, shell of a person. If someone had broken into my house, I would not have been able to react, and the stress would most likely have done me in, as I could no longer tolerate stress as before.”
I could not have described it better myself. I’ve often referred to myself as a rag doll, not just physically but mentally… cognitively.
Chlorine Dioxide takes care of FM and CFS.
Wipes out all the bad bugs and adds oxygen to the cells.
I have this issue my left leg fills up with lactate so bad just walking a short distance and I’m out of breath. If I push myself my muscles fill up so bad I become paralyzed and I can’t lift them. I just wish I knew why.
So overuse of the muscles, holding breath (hypoxic state while training) is a good way to get this, as this how i got this.
Still trialing everything possible.
Vegan with fish (limited fruit)
Keto
A number or variations to exercises and diet.
Concluded
Ewot and endurance exercise seems beneficial in theory (need to do longer)
Keto or Pescatarian
I tried lots of supplements and herbs over the years trying to find a special synergy effect but nothing, will keep you posted.
David can you let me know the condition and treatment.
I have burning muscles when lifting arms like holding phone up, brushing teeth etc.
thanks,
Chris
What was the treatment
Hi David. I assume the correct diagnosis was the empty sella syndrome which caused hypopituitarism and the treatment was replacing all the hormones you were lacking as a result of the dysfunction INR pituitary: ie thyroid hormones, growth hormone, cortisol, testosterone and possibly others. Am I correct? A lack of any of these hormones will cause crushing fatigue & CFS type symptoms.
David Morris, I found your post quite interesting. I to went to 25+ doctors and was finally diagnosed at UCSF with Partial Empty Sella Syndrome. I’m on growth hormone now, but it hasn’t reversed my symptoms.
I know it has to do with oxidative stress, lactate build up and low oxygen levels. I found a doctor that combined hyperbaric oxygen with high doses of IV antioxidant vitamins, minerals and glutathione. It was miraculous. I immediately started feeling better and after 10 treatments I felt like my old self. The treatments were very expensive ($1,000 a pop). I felt better for about a month, then the symptoms started coming back. The doctor wanted to do more treatments, but I couldn’t afford it.
I used to be a gym rat and enjoyed lifting weights and body building. Before my diagnosis, because my body stopped producing growth hormone,it wasn’t repairing after workouts. I started to decline. I didn’t know what was happening!!
How are you doing these days?
“Fibromyalgia is that same burn, only all the time, without doing any exercise. ”
Exactly the pain i have been trying to explain to doctors for 35 years now- “Burning Muscle Pain with very little activity”, and constant, but some days are better than others- but still the burning pain is present- and i have been trying to explain to docs that it is like my muscles are not gettign the nutrients they need to function for any length of time during exercise- The burning pain stops me- it has ruined my life- and it takes at least 5 days to recover when i have overdone some light work- which i understand is called ‘post exertion malaise’ which goes along with Chronic Fatigue, but i guess also Fibro? I’ve gotten nowhere with the docs- other than them prescribing the usual antidepressants in low amounts-
They do say Low Dose Naltrexone is supposed to be very helpful to SOME patients- but it is off label use- and docs won’t prescribe it unless you find a specialist who is willing to do so- But they say it can’t be taken with opioids, which is a bummer because the opioids are what help the most with the inevitable sore muscles that come with light exercise-
I used to overtrain quite a bit; about all my brain can shout out right now. barely keeping head up today, may need to leave work – feel like hit by train. Fighting ME/CFS 5-6 years, can’t work out anymore, only light swimming on occasion when i can make it across to gym. tried jogging a few minutes on beach saturday – bad idea, functionality next to nothing this week since then.
The VOX exercize test did show my body switches to anaerobic after just very light pedaling on stationary bike after just a few minutes…
Compared to the way i used to run a spin bike; its barely walking across the house…
Ouch! You gotta think that with a response like that that at some point researchers are going to come up with a finding that blows everyone’s mind…
June Beaumont April22nd.
I cannot peddle for more than 20seconds some days. The lactate in my legs and arms is ridiculous, it hurts so much.
I was an athlete and sports person that could go all day but not for the last 15 years. My life is none existent were sport or exercise is concerned.
Where can one buy Bifidobacterium breve Yakult
Listening to returned astronaut Scott Kelly made me wonder if lactic acid, autonomic disturbance,and changes in blood volume might play a role in how he feels. His symptoms are similar to Fibro. He is experiencing muscle pain, fatigue, and skin hypersensitivity (“almost burning”).
He also, apparently, measured substantially taller than usual, but then quickly compressed back to normal height after returning to earth. Must have been a shock to the muscular system.
Meanwhile, I have been getting relief from months of debilitating leg and hip pain with a gravity-inversion table. Initially I thought it was an injury, even though I have FM and know the muscle-burning well. But physical therapists concluded the problem was, in fact, FM, magnified into a specific area by over-pronation syndrome.
Exercise was not helping. But deep-tissue massage was. That could be because the massage was, in effect, releasing pockets of lactic acid.
Hanging upside down seems to be doing something similar. Each day the tight, compressed burning areas are able to release a little more. Also, I find I can delay lying down when I start feeling badly achy and heavy. I can buy about a half hour of lightness and relief by inverting for about ten minutes.
Now that I think about it, my earliest symptoms — ten or 15 years before being diagnosed with FM — were restless legs and IBS. Now when my RLS is bad it’s almost indistinguishable from the burning of FM.
PAW
I too found massage was the only thing that would help the pain, I unfortunately did not have the ability or equipment or knowledge to hang upside down but that does the same thing massage does plus it helps drain the lymph system. I came up from other article a skin brushing routine which really helped me plus massage
I wrote an article on it
Skin Brushing
http://coconutcreamcare.com/2014/07/06/you-brush-your-hair-and-teeth-what-not-your-skin/
I have written an essay, “Fibromyalgia and Lactate” posted at Quora.com, @badgleylaurence, and at Laurence Badgley G+. Lactate seems to be one of the missing links.
‘Very interesting article! I do have low oxygen levels as I measure them myself with an oximeter that I got at the local drugstore. I use supplemental oxygen (oxygen concentrator) for an hour or two a day….not sure if that helps. Is that what others meant when they referred to supplemental oxygen?
I have also purchased a Bemer mat to increase cellular oxygen and microcirculation.
For candida (and I am just guessing I have it) I have used Candex and probiotics.
Does anyone have a suggestion for an accurate test for candida?
Are there specific strains of probiotics for candida?
This is from the website found in the link
Saliva Test for Candida Infection
Also called CANDIDA SPIT TEST and/or The Thrush Saliva Test
http://lifeslim.net/spit-test-for-candida/
http://phytomedica.co.uk/fibromyalgia-treatment-promyalgan-candida-test.htm
If you have Candida overgrowth, there are blood, fecies, and urine test all require the prescription from a doctor. But there is an easier less expensive way. It is called The Thrush Saliva Test. It was created by Robert Harrison who has used it to make thousands of tests for Candida Overgrowth in the body. If you have candida overgrowth, it will show up in the saliva, a friendly environment for candida.
It is interesting that the tennis star, Maria Sharapova, has been using Meldonium which increases blood flow and oxygen levels. According to Wikipedia it is is a precursor in the biosynthesis of carnitine.
It sounds like somthing like this would be helpful or at least worth a try. It is not approved in the USA.
Thx Prashanti. That info on meldonium is very interesting for treating long haulers / long covid people.
I have tested my blood l lactate levels and every time they are elevated. The worse i feel the higher my lactate levels.
Why dont researchers just test blood l lactate levels in people with cfs/me?
Anyone else have this finding?
Anyone tried to supply patients with EPO? Reading this, I believe it would be interesting to investigate the reactions, and it may open up some further clues on the physiology of all this.
Some doctors have used it with success I believe.
EPO. Side-Effects of Erythropoietin
There are major side-effects of using erythropoietin which have proven to be fatal in previous cases:
•Increased viscosity (thickness) of the blood (which increases the risk of heart attack and stroke)
•Fever
•Seizures (fits)
•Nausea
•Headache
•Anxiety
•Lethargy
Most people with ME/CFS would need EPO side effects as much as a hole in the head.
Following a number of courses of antibiotics I fought severe ME & Systemic Candidiasis for 7 years with strict diet, minimum Carbohydrates, Nystatin & Ketaconazole, plus strict avoidance of all chemicals and food additives. It was the start of a slow but steady improvement. Recovered? No, not entirely but LIVING within the reality of ME/CFS, still cannot walk uphill, up 10 stairs or more than 100m level but for pratical purposes it is enough. The awful rapid spasmodic flicks in my head have never gone.
Is there a difference between Food & Chemical Sensitivity,Immune Dysfunction, and ME? – I do not think so. Will an overall cause be found? I doubt it.
We are all individual physiologies with different reactive stress levels to the chemicals which have steadily been introduced into our lives. Humans have always been adaptive beings but not to the overwhelming & increasing toxic chemical onslaught of the last 60 years.
The original caption, “Allergic to the 20th Century” was not far wrong, but do chemical, oil, pharmaceutical industries and governments have a vested interest in avoiding that conclusion? Think about it, insecticide, antibiotic, antifungal all mean killing something living, if it affects the nervous system of insects it affects human nervous systems too. It does me, pollution, streets & supermarkets are a complex of chemical hazards, medical drugs have unacceptable side effects, food & water needs to be without additives.
The human canaries are increasing in number but will anything change?
We are just collateral damage. Welcome to our collective future.
I also feel there could be a relationship with ME Fibro and chemical sensitivity. I am trying the DNRS program (Dynamic Neural Reprogramming System) with DVD’s at home. My friend feels it cured her chemical sensitivities. She had to give up her beautiful home and live in car not being able to even tolerate other homes….wi fi etc.
So far (2months in) I would say it has made some difference..wouldn’t say a cure. However, at times I can shift my energy to a higher level for awhile if needed. They say to stay with it for 6 months to see results.
My symptoms don’t seem to be as severe as yours. I wish you well.
Can someone please tell me!
What Break throughs for 2018
Has anyone found the Magic Wand !
So We know what to do and help People with this Horrible Painfull excistance!
People just have no idea ! We don’t complain and tell the world as it is pointless!
Suffer in Silence to try and live a Normal life!
I make the most of everyday !
Happy to be Alive !
but Omg so bloody hard when your Future ! your Dreams! your Capacity to earn a living has gone completely!
How to maintain our property
I could go on and on
how difficult it is to Throw everything over ones shoulder
always saying Dont’Worry be Happy with a Smile on my face !!!
How do I do it !
One thing I have learnt is PACE YOURSELF !!
ONE DAY AT A TIME!
PS I Thankyou all for Trying to find the Answer ?
Cheers
Sandy
Heres my youtube channel
https://www.youtube.com/channel/UCD-Ee-vZqolnnNoaVA6TRxA/videos?view_as=subscriber
If any has the same symptoms as me please connect as we can figure out a way to cure this problem.
High lactate can also result from low magnesium. Magnesium oil is a good way to test and increase your magnesium. CFS has also been linked with low magnesium in Red blood cells:
https://www.ncbi.nlm.nih.gov/pubmed/1672392
How to improve/fix your CFS:
Increase Magnesium with magnesium oil on your skin.
Increase your magnesium in your red blood cells via
Zinc + B complex (especially B6, B2, B5).
https://www.ncbi.nlm.nih.gov/pubmed/7271227
Reduce Caffeine, refined sugar and control your Calcium intake.
Take some D-Ribose to restore your ATP. (“From fatigued to fantastic” – Teitelbaum).
Increase Vitamine D, E through COD liver oil.
Find the stressor, when your CFS started (virus, stress…)
Cort, excellent article and fascinating comments.
Thank you!
Thanks!
Thanks for your advice ,,,I dound ghe stresser ..it was a virus ..so is impossible to reverse what a virus had caused
I stumbled across a youtube by an FM sufferer saying Alka Seltzer Gold helps her symptoms. Turns out intravenous sodium bicarbonate is the gold standard for treating Lactic acidosis. I started taking Alka Seltzer once a day three days ago. I immediately feel a rush of euphoria followed by reduced fibro brain fog. After two days I woke up feeling almost normal. A little muscle soreness at the level I wouldn’t have noticed pre-FM diagnosis. Cheap and easy, worth a try to see if it helps you.
Hi 👋 how is it going for you with Alka Seltzer? Still taking it? I’m trying baking soda… going to try Alca Seltzer! thank you!
Ive been taking low dose naltrexone. I didnt knw it would help stop the crash cycle and improve energy but it did so im back exercising for first time since i gor cfs at 21 with no crash cycle. But im still, now and then getting this lactate thing. Does anything help with it? After exercise say i roll over and i can feel my leg burning so every movement is like here comes that feelin in my legs (legs is mostly where my exercise happens i guess) its a pain. I also want to recop; or do i jst rest if have it till it stops? Im not used to asking myself these questions as of course in the past id rest and also have never been able to do this amiunt of exercise in first place. Ive heard its temporary in thenpopulation but mine can go on for half a day or more.
try massaging the legs- maybe get a massager to help with it- also perhaps baking soda can help alleviate the acid a bit- they make pills over-the-counter you can buy- it’s just such a horrible condition- especially in hot humid weather which we are having right now- with no end in sight- uggh-
Hi, fibromyalgia patient. The only way to get a relief from muscle pain and all sorts of aches for me is to take 1/2tsp to 1tsp of baking soda with a glass of water – oh my goodness in a couple of hours I feel such a relief and so much energy ! The painful burning sensation in my body is gone, I am reborn! But I am not sure one can take baking soda daily… any thoughts? Did all candida/parasite cleanses, loads of vitamins minerals etc and the best result is with baking soda.
Update: taking extra beta alanine on a daily basis (and baking soda for emergency cases) has changed my life!! Alcar for brain fog episodes. Good luck!