Jarred Younger was lured away from Stanford by a University that wanted to get a lead in an emerging field. By definition emerging fields are not quite there yet…they’re emerging. Picking a winner in the medical field sweepstakes may be a bit like backing a startup in Silicon – you never know what is going to catch on.
If the first year is any evidence, the University of Alabama at Birmingham made a good bet. Jarred Younger’s focus on fibromyalgia and chronic fatigue syndrome is paying off and graduate students are flocking to his lab. So many, in fact, that Younger had trouble with the latest count (he believed he was at 18 ) and he’s had to turn people away.
That might not be too surprising. Suzanne Vernon recently noted that in her experience that talking to someone about fibromyalgia and chronic fatigue syndrome will almost inevitably elicit the response “I know somebody with that – and it’s horrible”.
If both diseases still get poor support from the NIH and from doctors in general, if Younger’s and Staci Steven’s and Dr. Klimas’s experience at their respective Universities bears out, the next generation is going to view these diseases not as something to avoid but as their opportunity to really make a difference….
They’re certainly believers at the UAB at Birmingham. The University has given him money, expanded his lab and featured his work prominently in their publications. In his recent YouTube event Younger said his Neuroinflammation, Pain and Fatigue Lab was engaged in no less than 12 studies. The students interest is allowing him to do multiple studies at the same time; that’s really good news for a community that often has to wait years for a study to get done.
The lab now has a clinical trial unit, a brain scan unit, and an immune modulation unit and if Younger has his way – and let’s hope he does – that’s just the beginning.
Treatment
LDN ME/CFS Study
Younger began with an emphasis on fibromyalgia and in recent years has branched out to chronic fatigue syndrome and Gulf War Syndrome. He’s young, he wants to move the bar for patients as quickly as possible and he’s pretty daring. Early on he took on a compounded drug patients were raving about, but researchers pretty much weren’t touching. Two studies later low dose naltrexone (LDN) was a hot item in fibromyalgia circles. If you’re getting benefit from LDN you can probably thank Younger for that.
Younger’s expanded his LDN studies into chronic fatigue syndrome (ME/CFS). He believes both FM and ME/CFS are caused by neuroinflammation in the brain that LDN is turning down. How closely related the two diseases are will be partly answered by how the ME/CFS patients do on LDN. If they do as well as the FM patients did that will suggest they’re pretty closely related.
Botanical GWS Study
In a earlier talk Younger posted a long list of potential microglial inhibitors which included quite a few herbs. A Department of Defense grant is allowing him to study the effectiveness of nine botanicals in Gulf War Syndrome (GWS). If some of those herbs end up being effective, the next stop is his FM and ME/CFS patients.
- See a list of potential microglia inhibitors
LDN Plus Dextromethorphan Study
If LDN is putting the brakes on the microglia in the brain why not combine it with another possible microglia inhibitor? Younger is doing that in his LDN/Dextromethorphan study.
Mostly used as the active ingredient in cough-suppressant formulations, dextromorphan in animal models is able to protect neurons from glutamate excitotoxicity, hypoxia and ischemia, and inhibit microglial activation. All these processes are high on the list of possibilities in ME/CFS/FM given the problems with blood flows found and high rates of oxidative stress in the brain.
As with LDN, low doses of dextromethorphan were more effective in reducing neuroinflammation in one study (using a mouse model) than higher doses. Five to ten studies, thus far, have examined dextromethorphan’s effects on central nervous system activation.
Jarred Younger’s YouTube Event
Research
Younger will know even more about neuroinflammation as he cranks up his new toy – an MRI scanner that’s been modified to assess small changes in temperature of the brain. Younger believes inflammation is slightly raising the brains temperature. (As in global warming small temperature changes can have large effects.)
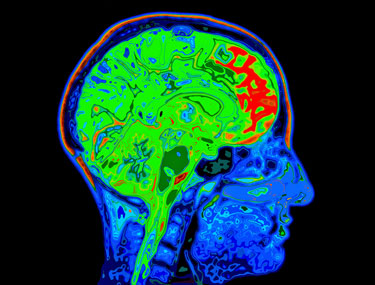
Because low blood flows could also be increasing brain temperatures, Younger will be analyzing blood flows to the brain as he measures brain temperatures.
He’ll be measuring brain temperatures not just in ME/CFS and FM but in rheumatoid arthritis, multiple sclerosis and traumatic brain injury as well. Including other disease control groups has, as the AHRQ report pointed out, only too rarely been done in ME/CFS. After Younger is done, though, we should know how the brains of FM and ME/CFS patients compare to those of people with some major neurological disorders. If the recent Simmaron spinal fluid study result comparing ME/CFS and MS patients is any indication, they may compare quite well.
Younger got a major NIH grant to expand his Good Day/Bad Day study. Kudos to the last batch of patients who, even after a fire shutdown the front of the hospital, successfully completed three weeks plus of daily blood draws. One wonders how many patient groups would show that kind of commitment.
When asked whether an MS drug like Copaxone could have a similar effect to Rituximab (Rituxian) Younger felt that was very possible. The difference between MS and ME/CFS and FM may be the neural damage in MS. All three diseases feature, he believes central nervous system inflammation but only in MS are the neurons damaged.
When asked about Rituximab he answered that any drug that depletes B-cell populations and keeps them from breaking through the blood brain barrier and assaulting the nervous system could be helpful in these diseases.
A validated biomarker could catalyze the field tremendously and quickly lead to a new drug. The problem with new drugs is not developing them; Younger stated some groups can turn research findings into drugs with a year. The slowdown comes in the drug approval phase; a new drug would take probably five years to get approved.
Drug repurposing is the best answer in the short term. With his LDN, dextromethorphan and botanical studies Younger is putting a lot of work into finding options for FM and ME/CFS patients now.
The biggest difference he may make in this area probably lies in the future, though, when he builds his fast track clinical center.
Fast Track Clinical Center

In a very (very) different election cycle George Bush talked about 1000 points of light. Jarred Younger and his booming Neuroinflammation Pain and Fatigue Lab at the University of Alabama at Birmingham is a point of light in the fibromyalgia and ME/CFS universe. He’s demonstrating that researchers can build their careers around these two neglected fields. Hopefully other young researchers and other academic centers will take note and following Younger’s and UAB’s footsteps.
- Sign up for the lab’s newsletter here
- Like their Facebook site here








A slightly tangential point of interest. Your linking Rituximab to b-cells and brain inflammation here. There could be another angle/layer explaining Rituximab’s effects as a study out a week or two ago showed that it reduced Ebv re-activation amongst immuno-compromised patients.
Is Low Dose Naltrexone likely to help severe M.E. patients? Do you plan any studies for LDN and severe M.E.? Any suspected downsides? My son is 22, has severe M.E., was straight A student, now bedridden, cannot talk, chew, listen or tolerate light
I really wish someone was doing research in Irelandon FM. I’d love to be a part of it as it has changed my life radically.