



Opioid Painkillers Under Attack
Opioid based pain drugs have dominated the pain relief marketplace for years but their dominance has more reflected a lack of other options than anything else. They’re quite effective at reducing acute pain but not so good at with chronic pain or with neuropathic pain.
Plus, their pain relieving capabilities can come at a high cost. The respiratory depression they can cause can result in death. They can produce a paradoxical hypersensitivity to pain and more mundane but still troublesome problems with constipation and itch. Plus there’s the euphoria that abuse causes which can lead to addiction and a host of other problems.

Opioid pain relievers dominate the pain relief marketplace but are under attack for the side effects they can cause
Plus, patients responses to the drugs vary so widely that pain medicine has been called more of an art than a science. Some people react well to one drug but poorly to a similar drug. They may react well to one dose but poorly to another.
Citing some pretty alarming stats the CDC recently came down hard on opioid pain killer use; nearly two million Americans are either dependent on or are abusing prescription opioid pain relievers. About forty people die every day from prescription drug “abuse” and over 400,000 people visit emergency rooms because of prescription opioid drug overdoses.
CDC director Thomas Frieden stated that “We know of no other medication routinely used for a nonfatal condition that kills patients so frequently. We hope to see fewer deaths from opiates. That’s the bottom line. These are really dangerous medications that carry the risk of addiction and death.”
With so much negative news one might wonder if opioid pain killers are on their way out?
They could be, but if Dr. Gavril Pasternak has his way they might actually be on their way in. In a recent Pain Research Forum webinar “Safer Opioid Analgesics: It’s All in the Telling of the Tail” Dr. Pasternak talked about the new class of opioid drugs being developed that are able to effectively reduce pain without causing any side-effects. At some point people in pain may be able to have their cake and eat it too.
New Pathways to Pain Relief
“The future for safer, potentially less abusable opioid analgesics looks bright” Dr. Pasternak
The breakthrough Dr. Pasternak believes is occurring began with the ability to “clone” and understand the genetic structure of the opioid receptors that dot our cells. The receptors on our cells are the keys that unlock our cells potential. Opioid drugs that lock onto opioid receptors in cells on our spinal cord and brain cause those cells to produce substances that reduce our pain.
Deep analyses of the genetic structure of the mu opioid receptor that traditional pain drugs interact with produced insights that may spark the production of a new kind of opioid pain reliever.
Most opioid pain relievers activate pathways that reduce pain and cause side effects. Newer drugs will activate different pathways (From Dr. Pasternak’s PRF presentation)
It turns out that opioid receptor gene produces twenty different receptor types or “splice variants”. These splice variants allow a single gene to code for multiple proteins depending on which portion of the gene is activated. Further research indicated that these 20 different receptor types fall into three classes of opioid receptors.
These classes are based on the “signal transduction pathways” these receptors activate in a cell. Once a molecule locks onto a receptor on a cell it activates a signal transduction pathway which prompts the cell to act.
It turns out that most opioid drugs lock onto one type of receptor (7TM) which activates pathways which reduce pain but which also cause most of the side effects we associate with our current regimen of opiate pain killers.
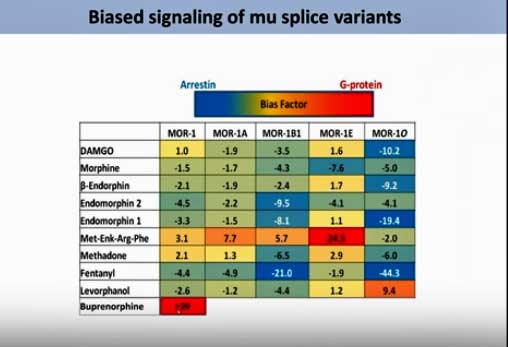
The figure to the right indicates that most of the opioid drugs used activate the wrong pathways. The pathway with more side effects is in blue, the one with less side effects is in red. Notice that only two drug-receptor combinations are in red. The rest are in some version of blue.
The fact that the same drug can attach to different receptor types helps to explain why such variable responses to pain drugs are present. If your cells happen to be littered with the MOR-1A receptor, for instance, you probably won’t have too many problems with methadone but if the MOR-1BA receptor dominates you can expect to experience lots of side effects.
A New Class of Opiate Pain Drugs
With its broad analgesic activity in thermal, inflammatory, and neuropathic pain models (5), as well as its lack of respiratory depression, physical dependence, and reward, IBNtxA may represent a new class of analgesic distinct from those associated with traditional opiates Pasternak et. Al.

A new class of opioid pain relievers may at some point provide pain relief without dangerous side effects
The solution to the opiate drug problem that’s staring pain drug makers in the face right now is to produce a molecule or drug that targets the opioid receptors that activate the good opioid pathways. If they can manage to do that the news is very good indeed. Animal studies suggest that not only do these other pathways produce many fewer side effects but that they also appear to be better at reducing pain, particularly the hard to treat neuropathic pain.
At least three compounds have been produced, two of which are in clinical trials. The one Dr. Pasternak has developed called IBNtxA (3-iodobenzoyl-6β-naltrexamide) accomplishes a pain trifecta; it appears to be more effective against all three types of pain (inflammatory, neuropathic, thermal) than traditional opioid drugs….plus it’s side effects, with one possible important exception – are nil.
The one side effect that still appears to be present is tolerance. Tolerance occurs when more and more of a drug is needed to produce the same level of pain relief. Dr. Pasternak said, however, that recent studies suggest that tolerance may have a ceiling; at some point if enough of the drug is provided no more will be needed to reduce pain.
Many groups, Dr. Pasternak said, are working hard to produce opioid drugs that activate these other pathways. IBNtxA – perhaps the most promising on the new slate of opioid drugs – is still being tested in laboratory animals. Two other drugs are in clinical trials.
In September 2016, PZM21 was shown in animal studies to deliver similar effects as opioids but without the side effects associated with them. This molecule was custom engineered to fit the opioid receptors in the brain, a feat made possible by the ability to image the atomic structure of those opioid receptors.
Opioid drugs are getting a lot of heat right now but a different class of opiate drugs that are under development or in clinical trials now could end up spelling relief for many.






Where can one find info on the human trials on the new opioids?
thanks
when will this medication be available in australia
It will be awhile. The IDN one has to go through clinical trials first and it hasn’t started. I don’t know the status of the other two drugs.
The two drugs were mentioned in a question following Dr. Pasternak’s presentation. I can’t remember what they are but if you go to the link and go to the question section they should be in there.
This new opioid drug sounds promising hopefully it will come to market in the very near future. I stopped opioids so I could take LDN and I’m glad I did it has been a true pain reliever.
What is LDN that you take?
I think it’s the Low Dose Naltrexone .
Sorry MK Smith for not responding to your question. Debby is correct it is “low dose naltrexone”. Cort has written some articles on this drug – search LDN on Health Rising.
Isn’t this what was promised when OxyContin was introduced?
(….I believe Purdue promoted this as a safe opioid for patients in pain.)
Pls understand that I am NOT oppose to managing pain with opioids if there is no other form of relief. I am however cautious every time I hear a new miracle pain medication is being introduced. We definitely deserve relief from this debilitating illness…
I have learned however (after many years of horrific side effects & complications from both opioid & non opioid medications), everything is not always as promised.
Let’s hope this time they are accurate!
Indeed. They are using a different pathway than Oxycontin but as you say – you don’t know until you know.
This sounds very promising in also getting people who are physically Dependant, such as myself, a way to get off of the addicting meds without having to go through withdrawal. I cannot wait!
Sarah, you can always try ” Suboxone “, which is a medication that helps you to get off of all opiates. I was on 100mcg of fentanyl patch and 30mg of oxycodone for 6 yrs due to serious surgery I had,along with chronic pancreatitis, something so painful, I have suffered with this my entire life. I got to the point where I was so sick and tired of being sick and tired,I decided that I had had enough. I wanted off all of this crappie but was terrified of the withdrawals
I found a doctor who specializes in drug dependence and he put me on this medicine called, Suboxone. It literally changed my life, for the better. It has been a miracle for me,no withdrawals at all. It’s been 6months now and I have my life back. My story is very long and I don’t want to bore you with it. So if you really want to free yourself of your dependence, look up Suboxone on Google, read all about it. It gave me my life back and I would recommend it to anyone who wants to beat a dependence or addition. It’s all pretty scary, making that choice, and sticking to it but, believe in yourself. Be strong, be free and be happy
Thanks Marie for sharing that and congratulations!
The medical community should have an effective replacement ready and available before they try to take away what we do have. It seems inhumane to me to not provide people with chronic pain effective relief in this day and age. I think some of these desperate people will self medicate with alcohol and other things that may be bad for you.
Very very good point .
I agree with Cynthia. Some are on their soapbox trying to take medication away from even those who use it responsibly. It’s asenine. Anyone can abuse any drug or any substance – even water. It is up to the individual. We watched a show where a woman couldn’t stop eating the foam in her mattress. Should we now outlaw foam mattresses because some people are abusing them? I was in church and a woman asked for prayer for a relative because he was being denied pain relief for cancer! On the opposite end of the spectrum, in CA a doctor was sued for not providing adequate pain relief to a cancer patient and the family of the patient won.
Lawyers are advertising. asking if you’ve developed a drug problem from a doctor’s prescription, and now you can sue him and get money (of course that’s going to tempt less than ethical individuals in need of cash). These folks are going to ruin it for those who 1) are in dire need of the HOPE of finding relief from pain, if even for a short time 2) those who take medication responsibly.
Good and caring doctors are going to be afraid of prescribing due to the new hype. There is no balanced view of it.
Couldn’t agree more.
Sadly I cannot even get a pain medication as I am so hypersensitive to many they have tried. Ironically the one that works, although it causes nausea, dizziness and a some disorientation helps me sleep a few hours yet isn’t in the formulary. My doctors are leery of doing anything but prescribing Motrin 800 which is eating at liver and kidneys. What is the recourse?
I have a wonderful Nurse Practitioner (whose supervising Dr is a GP) I have been her patient for 10 years. She listens, she discusses, she looks things up, we try new things, she coordinates my care, and she makes me laugh so I always look forward to seeing her. I have had FMS for 26 years. I have tried everything -and try whatever comes out that is promising- but nothing relieves my pain but opioids. My NP prescribes NORCO for me. I never abuse it and she trusts me.
I just got a letter from her office (she had called me to warn me it would be coming as she knew I would be upset) saying they could no longer prescribe opioids because of the new CDC rules and that they had already been contacted and warned by the DEA.
So, as Rose said, Good and caring doctors will -and are- afraid of prescribing the meds their chronic pain patients need.
Now I am scrambling to find help. I went to one of those so-called pain clinics and it was a horrible place. The Dr. was rude, condescending, snarky and dismissive. I hated him. Oh, he will give me the drugs alright, but I hope I can find another source. The irony-he knows NOTHING about me and its OK according to the CDC for him to prescribe but my GP for the last 10 years has been scared off.
Someone really needs to be advocating for Chronic Pain patients.
Dr Richard “Red” Lawhern HAS been advocating for us for years. Check him out. He has so much information, is intelligent and well spoken. He will restore your hope.
I have severe Rheumatoid Arthritis & FMS. I have been told by my Rheumatologist that I, likely have Juvenile Idiopathic Rheumatoid Arthritis,& have had this my whole life. (I wasn’t diagnosed until I was 37. I broke my hip in the 5th grade. My elbows & shoulders used to dislocate regularly as a child. My ankles have popped loudly all my life, everytime I roll them.)
I live in Georgia. I have to go to a Pain Management Dr. To be able to get narcotic pain meds. My Rheumatologist & GP cannot prescribe the amount I get every month. (I don’t take the amount I’m given.) I have been going to the same pain clinic, but different Dr’s within that clinic, for 7 years. They still make you do random drug tests & pill counts.) The things we law abiding non drug abusers have to go through to get our meds bc of the abusers, is getting harder & harder to deal with. But I put up with it,BC I have NO CHOICE!!! If I want my pain meds at all, these are the hoops I must jump through.
I just hope & pray they get these NEW DRUGS to market SOON!!! I’d love a drug w/less side effects. Gosh, how I hate this itching from the narcotics!!
Hang in there Theresa. I was just told that the NIH want 15 new drugs approved for pain/opioid relief in the next five years. They’re putting out hundreds of millions of dollars to do that. Cross your fingers and hang in there! 🙂
Are you kidding, wait 5 years. That’s what people with severe pain want to hear. I’m sorry but we have been promised this before. The drug companies make all this money on people in pain and I’m sure the next new medication will be just as or more expensive than oxycotin was and still is. Wasn’t that long ago that the oxycotin manufacturer got their patent extended so no one else could sell a generic. Why did they do that. To make as much money as they could on people that were in so much pain they had no choice. I can’t believe they weren’t aware of how addicted it was to people would didn’t need it for pain. Only now when Congress is throwing a wrench in their profit making did they come up with another medication. I’m so tired of the people who need and responsible take these medication are lumped in with people who have addiction promblems. Why do we all have to suffer. What’s the point in following all the rules when you will be punished anyway.
No I’m not kidding and no you haven’t been promised this before – not like this. You can make this into “I’ve heard it all before” if you want but this is different – the federal government has never ploughed this much money into painkiller drug development before – not even close.
Dear Cort Johnson,
Well it’s January 2020 now and I was just curious about the status and the progress of this new wonder pain medication? I will be first in line! Will you please keep an update here if possible? Thanks
absolutely agree with you Gin… like you I have been on the same narcotic since Jan 1999 and only once has my dose increased in 2012… Not bad for time…
I have never abused the medication and I have followed the rules religiously (I am a registered nurse by trade) so yes I would be physically addicted to the meds as I would have been if I was on an antidepressant… but i also have a doctor here that can detox me off the medication If i need to and this is not problem for me (I did detox off the medication 6 months after (1999) I commenced on it as I didn’t want to be on a narcotic… I came off it with no problems but 7 days later I realised how much the medication helped me (my symptoms all returned severely and the pain and fatigue was off the scale) so I was commenced back on it on a higher dose as I was told I was not on the correct dose to start with. They were right. The higher dose although not making a massive difference did give me a much better quality of life. Getting the pain management better was the thing that then enabled me to get up off the bed more and I could actually start a walking program. I also then had a decrease in the fatigue level so I could organise a meal a couple of times a week. I could then get a bath once or twice a week without sending myself to bed for weeks after.
Now with all the scare mongering around narcotics… I fear for my life … I have been told that I could have the medication taken from me and pain doctors here now are so anti narcotics they treat me like some drug seeking addict… I can assure you that has never been part of my profile.
I cannot understand why we are not given the individual treatment we deserve and that if these doctors are as good as they think they are they should be able to treat us individually and those of us that are controlled on narcotics should be monitored as usual and be given our dignity back to live the life that we can manage…
I am tired of the way I am spoken to and treated … its rude and I do not deserve it when all I have ever done is stick to their rules in the first place.
I also take LDN. I’d have offed myself years ago if I didn’t have it!
Dear Cort, I along with Sandra am waiting for this new drug, if there are any clinical trials in my area I am ready!
Although my ability to get out my front door has decreased severely.
Thank- you for your work!