



Migraine effects 12% of the population (!) or about 40 million people. Two studies suggest as many as 75% of people with chronic fatigue syndrome experience migraines and that most migraines in ME/CFS are undiagnosed. A recent large fibromyalgia study suggested that 55% of FM patients may meet the criteria for migraines. WebMD, which has very little to say otherwise about chronic fatigue syndrome, states ME/CFS is one of five disorders with high migraine rates.
If those studies are accurate, ME/CFS and FM may have more in common with migraine than with each other. That’s an astonishing possibility given that migraines were hardly talked about with respect to either disease five or ten years ago.
That makes a recent migraine study highlighting hypoxia (low blood oxygen levels) and increased lactate – two intriguing possibilities in ME/CFS and FM – all the more interesting.
A recent blog suggested that increased lactate levels in the brains of ME/CFS patients could set the stage for increased fatigue. Several studies, in fact, suggest that increased lactate levels exist in the brain, muscles and perhaps guts of both chronic fatigue syndrome and fibromyalgia patients.
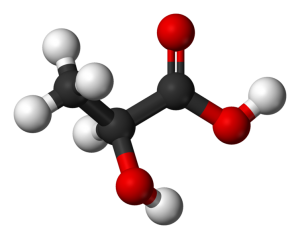
What is causing these lactate accumulations is unclear but one of the possibilities is hypoxia or low oxygen levels. When oxygen levels are low cells turn to glucose to produce energy via a process called glycolysis. This process produces pyruvate which, in turn is converted into lactate and released into the bloodstream. As that happens hydrogen ions also build up causing acidosis.
The Migraine, Hypoxia, Lactate Connection
A recent study exposed people who experience migraines to hypoxic conditions to see if they would trigger a migraine. They found that low oxygen conditions did, in fact, trigger a migraine in about half the women with a history of migraines but not in the healthy controls.
Migraine induced by hypoxia: an MRI spectroscopy and angiography study. BRAIN 2016: 139; 723–737 | 723. Nanna Arngrim,1 Henrik Winther Schytz,1 Josefine Britze,1 Faisal Mohammad Amin,1 ark Bitsch Vestergaard,2 Anders Hougaard,1 Frauke Wolfram,2 Patrick J. H. de Koning,3 Karsten S. Olsen,4
The ability of low oxygen conditions to trigger migraines in such a high percentage of women was astonishing. Why? Because, historically, it’s been very difficult to intentionally trigger a migraine in the lab. The oxygen levels the researchers subjected their subjects to was quite low but it did suggest that hypoxia may play a role in triggering migraines.
How was it doing that? It’s long been known that small dilations of the blood vessels in the brain occur during a migraine. These researchers showed that hypoxia did indeed cause those arteries to dilate – but in both the healthy controls and the migraineurs. Since the amount of dilation was no larger in the migraineurs than in the healthy controls it wasn’t clear that enlarged blood vessels were behind the migraines.
Nor were levels of glutamate, an excitatory neurochemical long been believed to play a role in migraine, increased.
Instead, lactate levels significantly increased in the migraine patients brains and blood. Why the migraineurs responded to low oxygen levels by producing higher levels of lactate than the healthy controls was unclear, but it was clear the lactate increases were associated with a migraine and/or the occurrence of unusual visual disturbances.
Some of those visual disturbances may be familiar to people with ME/CFS or FM; they included black spots, “worms” (floaters?), difficulty focusing and blurred vision. (Those visual disturbances technically fulfilled two criteria for migraine. Three of the four people with visual disturbances also experienced a migraine-like headache.)
The high levels of lactate were also sustained for several hours after the hypoxic challenge ended. That suggested that mitochondrial problems may come into play. A 1998 study, in fact, found increased plasma lactate levels after exercise in migraine, and numerous other studies have shown decreased ATP production in the visual cortex of migraineurs as well.
Conclusions
What do we know? We know that migraine is common in ME/CFS and FM and vice versa, and that hypoxia and lactate accumulations and mitochondrial problems may be involved in each of these diseases.
We also know that as with ME/CFS and FM, women are primarily effected by migraines, and migraines and ME/CFS symptoms are often substantially reduced during pregnancy. People with severe ME/CFS, in particular, often have significant problems with stimuli – as do migraineurs – and migraineurs and ME/CFS/FM patients also often seek out low stimuli environments during attacks or crashes.
We know exercise during a migraine is usually impossible. People with migraines often experience ME/CFS-like symptoms of fatigue and cognitive issues for several days following their migraine attack.
In fact, in a 2015 paper Rayhan and Baraniuk proposed ME/CFS/FM patients may exist in a kind of chronic migraine-like state. Given the considerable symptom overlap migraine has with ME/CFS (visual disturbances, sensitivity to light/sound, weakness, pins and needles, speech problems, nausea, vomiting, increased urination, etc) they could very well be right.
It’s not exactly clear how migraines, ME/CFS and FM are related but the connections are growing.
Check out
- Migraines, Chronic Fatigue Syndrome and Fibromyalgia: Treatment Options
- The ME/CFS and FM Migraine Test: Do You Suffer From Migraines?
- Fibromyalgia Bad – Fibromyalgia with Migraines Really Bad








Very interesting article, Cort – thank you!
I get migraines but found that reducing tyramine in my diet helped reduce the frequency and severity of them tremendously.
I don’t know how that would relate to oxygen and lactate.
Are there any treatment implications for migraine of this research?
Thanks. I don’t know about the treatment implications but Baraniuk suggested, if I remember correctly, that triptan drugs might help stop crashes in ME/CFS
http://www.cortjohnson.org/treating-chronic-fatigue-syndrome-mecfs/migraine-treatments-and-chronic-fatigue-syndrome-and-fibromyalgia/
Sumatriptan reduces inflammation in the arteries and veins in the brain by enhancing 5-HT (serotonin) production which causes the over-dilated veins to constrict. Sumatriptan also deceases the activity of nerves called the trigeminal nerves that are associated with cluster headaches. Interestingly, some research suggests triptans may be affecting the periphery (the body) more than the brain. Triptans’ difficulty passing the blood-brain barrier has stimulated research into its effects elsewhere. Studies suggest triptans ability to reduce pain-producing peptides such as substance P in the periphery may block pain signals to the brain.
Dr. Teitelbaum emphasized petadolex, Vit B-2, magnesium IV’s, COQ10, excedrin for migraine (as effective as Imitrex) and others in his video.
Supplemental oxygen is pretty useful for CFS/ME. It does nothing for my migraines, though. (For me MSM has been the most effective migraine preventive and I treat them with celecoxib.) One symptom oxygen has particularly helped for me is vision disturbances. I don’t mean migraine-type stuff but chronic low-grade CFS/ME vision problems that are well documented. I have had migraine auras and they are completely different. Before oxygen I couldn’t even pass a normal vision test at opticians, because my vision was “too weird”. Now? No problem.
There is a Finnish doctor with the idea that CFS/ME is a type of chronic migraine, though his ideas are quite controversial, especially since he likes to prescribe a big stack of mostly psychotropic medication (stimulants, tricyclics and Lyrica, I think) with triptans.
Some people with CFS/ME do get major improvement from triptans. But not too many. One person on my forum has even reported that in ten years. My own doctor doesn’t recommend triptans at all.
Hello Maija , can you explain what supplemental oxygen is in terms of form and how it is given ?
Tim, did you get a reply from Maija about supplemental oxygen? I assumed she meant oxygen with a cannula and an oxygen concentrator.
I was born with Fibromyalgia 74 years ago. I say that because my mother had it all of her life too. The pain really kicked in for me at age eight with preambles of discomfort before that, referred to as “growing pains”. I did not hear the word Fibromyalgia until I was 38 years old. I had very bad migraines from the time my period started at age eleven until menopause…if that has anything to do with the process.
This almost word for word my story. Change the numbers from 74 to 64.
I had Migraine symptoms since getting M.E. and the Auras were getting to me so I went to the eye dr. only to find out I have Mac. Degeneration as I was suddenly blinded from strange zig zag worms a few days ago that I called my eye spec. and he said it sounds like MIGRAINES. I’ve had Auras for a long time with and without headaches but the headaches I got after suddenly getting M.E. are so powerful that I can’t even speak. what does one take for Migraines since my tummy dr. told me NOT to take even Tylenol because of the damage to the stomach from those powerful drugs.
Hi I also have migraines and me cfs for 55 years. I spend my time supine in an effort to avoid migraines. Recently have been diagnosed with macular degeneration . Seems AMD common complaint with cfs
i find that curcumin and enzymes help my migraines. also terry naturally brand has a good formula called curamin for headaches.
i forgot— (darn brain fog!) i’ve mentioned this before-hemp canabidiol,cbd works better than anything else i’ve ever tried.
Chewing coca leaves (with an appropriate activator) as is done in the Andes for (among other things) problems with high altitude can help. Is there less oxygen at higher altitude? It is an alkaloid – can this improve acidosis? It is also a vaso-constrictor.
where do you get coca leaves if you don’t live in the Andes? I know they help with energy levels for high altitudes.
There is a lower concentration of oxygen at higher altitudes. I grew up at 7,000 ft and never thought about it. Now I live at 3,500 ft and my oxygen levels are around 93. When I drive an hour away to a level of 200 feet my oxygen levels are 97..
Cort.. So would oxygen therapy help do you think? Even for the headaches? The trip tans are not working or the topi max ?
You may make some good points here but I didn’t read beyond the first sentence. Please learn the difference between ‘effects’ and ‘affects’ or correct the typo, if that is what it was.
Robert, you apparently have much less weighty issues than 99% of us following this forum do if the mixing of effects/affects throw you off balance. Count yourself extremely lucky and go look for some interested party to volunteer grammar lessons to.
Keep up the good work, Cort. I’m glad that you don’t seem to ever let the negative piss ants of the world detour your efforts.
Thank you, Cort. Really interesting. I have had migraine since age 18. The cfs/me came a few years ago. My Dr talks about glycolysis & mitochondrial dysfunction all the time, as well as the lactate build up. Who knew in the brain? For me big ?n is how do we get our bodies to clear out the lactate? Would a high ph diet make a difference? Is it to do with our poor methylation?
I wish we had more answered.
Neurontin at night, a beta blocker twice a day and increased vitamin D and magnesium twice a day have really helped me.
I usually don’t comment, but wanted to add what has worked for me. I have had chronic, intractable migraine headache since a multiple rollover car accident in 1997. (ME/CFS and FM since that time as well.) I have been on nearly everything there is for migraine. I am currently fairly stable on topiramate (Topamax), butterbur, CoQ10, and MyoCalm (which contains calcium, magnesium, valerian and passion flower). I still have about 15 to 20 headache days per month, but they are tolerable, ie: I can still function. I have about 2 days per month of intolerable migraine where I have to just go to bed and sleep.
Because I have had migraine for such a long time and had daily migraines, I went through all the “triptans” long ago. I used to be able to use dihydroergotamine when I had a bad migraine, but I was told that after age 40, ergotamines are too dangerous to use. (Triptans should not be used either.) The University of Iowa Clinic of Neurology told me that there was no treatment for migraine attacks for those over age 40 because of the danger of heart damage. They said not to use Tylenol, Excedrin, Advil, etc. either because those just cause rebound migraine. I’m not saying I agree with them. I am just imparting to you what I was told by so called experts.
I think migraine is very individual. It takes a very dedicated neurologist or a person willing to try medications, herbs, and supplements until you find the right combination for you.
For me Tryptans did nothing, as did many other drugs. What has been a savior for me is Topamax(topiramine).
Yes, indeed, this is a great article. This is a theory that makes a lot of sense to me. I’m excited to see interest in excessive lactate build-up, decreased Vo2 levels and mitochondrial problems of transferring energy to the cells.
Who knows what causes these issues, did it all start with a virus, any one in particular or do many different viruses potentially
lead to ME/CFS, FM, migraine etc. I can see how many different diseases may be driven by the same driving force.
Hey guys, on my quest to get better and off medications especially since I have third stage kidney failure and my Blood Pressure is now at either stroke level or corpse level, so almost any medication can flip a switch and of course there is NO reason according to any of the tests that any of this is happening. I have Fibromyalgia with high inflammation, even though that’s an oxymoron that acts like MS, Lupus, and this year’s flavor Mono. So when I got diagnosed with Interstitial Cystitis, they said they don’t know the cause, but people do better avoiding acidic foods.
SO…I have been reading about acidic bodies, Ph levels and they talk about oxygen in the body. That a body that is too acidic can’t get good oxygen. I have been doing body work for 2 weeks. No sugar, no gluten, no yeast. I really miss my Wiessen Bier, total beer snob. Just fresh or frozen veggies, a couple of anti-Candida soups. No more Decaf Tea, even with Stevia. I still have my one cup of Coffee, that would be a death sentence to anyone within 100 mile radius. But quarts and quarts of lemon water, probiotic yogurt, oily fish, chicken and avocados. So I am doing Gut work and PH work, because I believe the oxygen theory holds merit.
Anytime I have been rushed to the ER. Driving 33,000 a year for 18 years, I was in 8 car accidents, only 1 my fault for fooling with GPS. At every ER, they put me on oxygen, telling me to take deep breaths because my levels were low, so there is fact that my oxygen levels were at those times habitually low, could have been stress, pain all the above but low.
Yet again, an article that points loud and clear to Les Simpson’s hemorheology studies…when any stimulus results in shape changes in the red blood cell population, into the irregular ‘non- deformable’ ones that can’t get through the microcirculation, then tissues which rely on the red blood cells to perform their function…delivery of oxygen and removal of lactates…become oxygen starved, and full of lactates.
This simple, straightforward explanation is consistently ignored.
Different things help different people…it is worth trying 6 g per day of fish oil, or 4g per day of genuine EPO. Vitamin B12 injected as hydroxocobalamin, and pentoxyfilline are suggestions that Les makes.
http://www.positivehealth.com/article/cfs-me/the-importance-of-blood-flow-and-evening-primrose-oil-in-me
Thank you for your excellent and extremely educating response. I learned a lot from you.
interesting, my daughter has had migraines forover 20 years and was also diagnose with fibro around 10 years ago. I developed migraines in my 40s but recently had a daith (stud in my ear at the bottom of the curve of skin above the earhole) this is to help stop migraine and headache like a permanet acupuncture and I find it works well I twiddle it when I feel a headache or migraine coming on and it goes away