

(Darden has looked high and low to find ways to understand and treat her ME/CFS/FM, and, if she’s not healthy now, she’s still been able to improve her health substantially. Recently a diagnosis of a Ehler’s Danlos Syndrome – a lesser known disease that often overlaps with chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) – helped her fill in some more blanks. Thanks to Darden for allowing Health Rising to republish her blog on getting a diagnosis of Ehlers-Danlos Syndrome and what it’s meant for her search for health. (Images and headings added…CJ )
Ehler-Danlos Syndrome (EDS)
“Ehlers-Danlos Syndrome isn’t rare – it’s just rarely diagnosed” Jan Groh
It took me forty-three and a half years to get a diagnosis of EDS hypermobility type.
Ehlers-Danlos Syndrome (EDS) is a genetic connective tissue disorder caused by structural deficiencies in collagen, the most abundant protein in the human body. All the tissues of the body including ligaments, bones, tendons, muscles, skin, blood vessels, gums, eyes and large organs rely on collagen for their strength and flexibility.
In EDS collagen is altered by a genetic defect or mutation that allows tissue to be pulled beyond normal limits resulting in systemic weakness and instability. The most common form of EDS is called EDS hypermobility type.
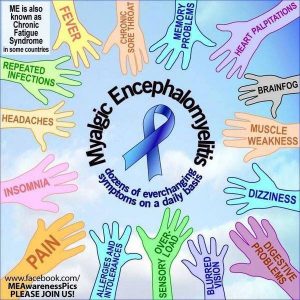
The problems resulting from a body built with defective collagen are widespread and variable. Persons with EDS Hypermobility often exhibit symptoms of dysautonomia, a dysfunction of the autonomic nervous system, which regulates unconscious organ function including heart rate, blood pressure, temperature, respiration and digestion. Chronic pain, sleep disorders and fatigue are common in persons with EDS Hypermobility.
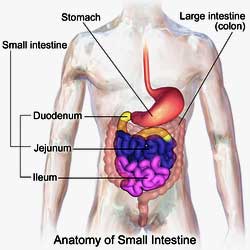
Structural abnormalities of the gastrointestinal track are also common, resulting in a variety of conditions including Irritable Bowel Syndrome. Chronic recurrent headaches and eyestrain are also common, as a result of abnormal intracranial pressure and enlargement of the dura, a membrane of fluid surrounding the brain and spinal column. Patients frequently suffer from allergies and sensitivities.
Chronic Fatigue Syndrome (ME/CFS)
Officially my health condition, which has affected multiple systems over the decades, was undiagnosed. However, my symptoms had a lot in common with what is now called Chronic Fatigue Syndrome. At the beginning of my illness I had severe headaches, eyestrain and fatigue and significant gum recession.
Fibromyalgia
Twenty-eight years into my illness I developed chronic muscle pain after any type of physical exertion that sometimes escalated to full body pain, which I suspected was fibromyalgia. About five years ago I listened to a lecture on the Internet given by Dr. Byron Hyde, a Canadian physician and researcher for CFS and ME at Nightingale Research Foundation, who said that there was a subset of patients with fibromyalgia who had Ehlers-Danlos Syndrome and one way to ascertain this was if the patient could touch their nose with their tongue.
Since I can do this I was curious about this possibility. However, my primary physician immediately dismissed this as did a cardiologist and a rheumatologist because I do not have any overt symptoms of joint hyper mobility or hyper elastic skin. My elongated tongue had caused some of my chronic fatigue symptoms which were relieved by doing Oral Systemic Balance, a system that employs oral appliances to address restrictions of the air passage due to the anatomy of the tongue and mouth.
Imbalances between the sides of my heart and the size and position of the atrium and ventricle were observed by my OSB dentist Dr. Farrand Robson on heart ultra sound equipment. Robson uses heart ultrasound to get feedback on the adjustments of his patients’ oral appliances. I suspected that the irregularities Robson observed as well as my low blood pressure and pulse were due to the hyper elasticity of the connective tissue in my heart.
Small Intestine Bacterial Overgrowth (SIBO)
Two years ago I was diagnosed with Small Intestine Bacterial Overgrowth (SIBO) and started treatment under the supervision of Dr. Melanie Keller, a naturopathic physician who specializes in this disorder. Dr. Keller told me that she had several patients with similar presentations of SIBO who had been diagnosed with EDS. The gastrointestinal tract is primarily made up of connective tissue and persons with EDS often have problems with gut motility that can lead to IBS and SIBO.
I knew that my colon was elongated because when I had a colonoscopy the exam could not be completed due to the unusual fact that the examiners ran out of scope.
Furthermore I discovered that I had low amounts of serotonin and DAO – two things that are produced in the gastrointestinal tract. I suspect that this is due to the altered environment of the connective tissue in the colon. Supplementing for these things by taking 5HTP and HIST DAO (diamine oxidase enzyme) has improved my health. Low levels of DAO contribute to a condition called Histamine Intolerance (DAO is the enzyme that breaks down histamine in foods).
Mast Cell Activation Syndrome (MCAS)
The nutritionist I consulted about this condition suspected that I had some kind of mast cell disorder. This was positively diagnosed by blood tests that showed elevated levels of tryptase. When researching Mast Cell Activation Syndrome (MCAS) I discovered from Jan Groh, chapter coordinator of the Pacific Northwest Mast Cell Support group that EDS and MCAS are overlapping conditions.
Groh is the author of a blog which has a lot of information about EDS hypermobility type and its comorbidities Mast Cell Activation and POTS. She is convinced that most people with EDS are getting diagnosed with fibromyalgia. She says “Ehlers-Danlos Syndrome isn’t rare – it’s just rarely diagnosed.”
Ehlers Danlos Syndrome
In March of 2016 I went to see Dr. Osvaldo Schirripa at the Central Oregon Clinical Genetics Center in Bend, Oregon. Dr. Schirripa is a geneticist with a background in pathology and is one of the few experts in EDS in my region of the country. My appointment with Schirripa lasted four hours and consisted of physical evaluation, a detailed family history and review of symptoms.
Dr. Schirripa was the first and only physician of the countless number that I have consulted over the past four decades who was not mystified by my diverse symptoms and health history. He diagnosed me with EDS hypermobility type. Based on his evaluation he gave me a 7 seven out of 9 nine points on the Beighton scale. I think that he was pretty lenient on this scale as some of things I could only do slightly with the exception of being able to bend forward with straight legs and place my palms flat on the floor.
Physical evaluation was also made on the smooth texture of my skin, pronounced gum recession and low blood pressure. Dr. Schirripa said that I was “highly functioning” for someone with my health condition, which I attribute to the effective ways I have found to manage and in some cases reverse my symptoms.
He mentioned a couple of things that were of significance to me. He said that people with EDS are often intolerant of drugs, having adverse reactions or reactions opposite to what the drug is intended for. This is definitely true for me. He said this is due to an extremely rapid phase one liver detoxification. This was found in several past liver detoxification laboratory tests I did that measure caffeine clearance.
“ there was most likely nothing wrong with my muscles (I know this from extensive testing with a neurologist). Rather, my muscles are working extra hard to protect hypermobile joints.” Darden
Another interesting thing that Schirripa discussed was the fact that there was most likely nothing wrong with my muscles (I know this from extensive testing with a neurologist). Rather, my muscles are working extra hard to protect hypermobile joints. I had suspected that my muscle condition (fibromyalgia?) was some kind of stress induced protective response so this made sense to me.
Schirripa reported that for many of his patients this muscle condition began suddenly and some patients reported that it began with a vibration. This was the case for me. Dr. Schirripa looked at my sleep study, showing fragmented sleep with interruptions accompanied by spikes in my pulse. He said this was a typical sleep pattern of persons with dysautonomia. (The several sleep specialists I consulted about my study did not identify this pattern as such, and basically had no explanation for my disturbed sleep.)
Although Dr. Schirripa is primarily a diagnostician I asked him if there were any particular supplements or treatments that he recommended. He said that everyone is different however some of his patients have been helped by large doses of COQ10 (2,000 mg.) a day. Schirripa thinks that the emphasis on hypermobility in the diagnosis and understanding of EDS hypermobility type is not comprehensive enough. His preference would be to call it a “multisystem spectrum disorder”.
The Driscoll Hypothesis
Last January I read an interview on Yasimina Yklenstam’s blog with Diana Driscoll called “Vagus Nerve Stimulation and POTS/Mast Cell Activation”. Driscoll is an optometrist who has EDS, POTS and MCAS and has proposed a theory on how these are related to intracranial pressure and abnormal vagus nerve functioning.
As an optometrist she learned how to identify in eye examinations abnormal patterns in the optic nerve and blood vessels of POTS patients. From her experiments in treating her own health problems she suspected that patients with these disorders have low levels of acetylcholine. Supplementing for this made a huge improvement in her health and the health of her children who also suffer from similar disorders.
Driscoll developed a supplement called “Parasym Plus”, which is supposed to address a low functioning parasympathetic nervous system. It contains alpha-glyceryl phosphoryl choline, acetyl L-carnitine, hyperzia and thiamin. I tried the supplement and had a bad reaction. The problem with multi-ingredient supplement formulas, which I generally avoid, is that if you have a bad reaction you don’t know what ingredient you are reacting to.
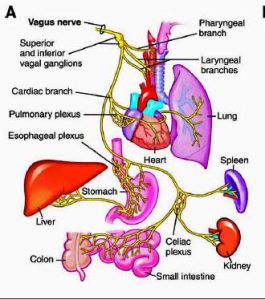
Driscoll also developed a supplement called Soothing Digestive Aid for Vagus Nerve Support, which contains apple cider vinegar and ginger root (two things that are easy to buy separately and I take as part of my treatment for Small Intestine Bacterial Overgrowth), and a supplement that contains digestive enzymes. Although I do not entirely agree with Driscoll’s theory, (I think that activation of the vagus nerve is secondary) her discovery of the benefits of treating low levels of acetylcholine in patients with CFS/FMS/EDS/POTS is important. For more information on Driscoll’s theory and treatment go here.
The symptoms of EDS hypermoblity are virtually indistinguishable from those of Chronic Fatigue and Fibromylagia Syndromes especially when one takes into account that its presentation is variable from person to person. I recall several years ago when I saw Dr. Andrew Holman, a rheumatologist and leading researcher in fibromyalgia, that he mentioned to me that many of his fibromyalgia patients were very flexible.
Dr. Sharon Megalathery, a physician with MCAS, POST, CFS and POTS has a theory of how these and other overlapping syndromes may be connected to a set of gene mutations. She and her colleague Dr. Karen Herbst have set up a non-profit corporation to fund research on this here .
The diagnosis of EDS hypermobility type has lead me to connect some more dots in my health condition. I do not think, however, that finding this out earlier would have significantly changed the course of my search for effective treatments. Until a definitive laboratory test is available to test for a genetic defect in collagen in EDS hypermobility type, the diagnosis is in my opinion still theoretical. Meanwhile, as a patient my most productive path is to find ways to manage my unique variation of this multifaceted disorder and to share my stories of successes and failures with others.
More on Ehlers Danlos Syndrome
Diagnosis is made by physical evaluation, family history and symptoms. Laboratory testing for EDS hypermobility type is unavailable as the genes involved have not been completely identified. The condition overlaps with Mast Cell Activation Syndrome (MCAS); Postural Orthostatic Tachycardia Syndrome (POTS) and neurally mediated hypotension (NMH); Chronic Fatigue and Fibromyalgia Syndromes.
Few physicians specialize in EDS, and diagnosis is most frequently made by a geneticist. The most common sign of EDS Hypermobility is an unusually large range of joint movement. This is diagnosed by receiving a score of five or more on the Beighton scale.
The points are as follows:
- one point if while standing forward bending you can place palms on the ground with legs straight
- one point for each elbow that bends backwards
- one point for each knee that bends backwards
- one point for each thumb that touches the forearm when bent backwards
- one point for each little finger that bends backwards beyond 90 degrees.
Another major criteria for EDS is soft or velvety skin with normal or slightly increased extensibility (stretchiness).
Minor diagnostic criteria include recurrent joint dislocations, chronic joint and muscle pain, easy bruising, irritable bowel syndrome (IBS), neurally mediated hypotension (NMH) or postural orthostatic tachycardia (POTS), high narrow palate with dental crowding, and gum recession.
Family history of similar features is also an important criteria in the diagnosis. EDS hypermobility is inherited in an autosomal dominant manner meaning that a mutated dominant non sex gene has been passed to the affected person by the parent and that there is a 50 percent chance of a parent passing on the dominant gene to his or her offspring.
An excellent article on EHS hypermobility type authored by Marco Castori can be found on PubMed Central
There is no medical treatment or cure for EDS hypermobility. The Ehlers-Danlos National Foundation website has some good information about the disorder and lists some management recommendations.
Strategies for improving muscular skeletal symptoms include minimizing joint impact, hyperextenision and resistance exercise; avoiding excess body weight; wearing shoes with arch and heel support; doing low resistance muscle toning exercises to help stabilize joints; myofascial release type therapies to reduce muscle pain; using supportive mattress and a pillow that keeps head in a neutral position while sleeping; and using fat-grip writing utensils.
Gastrointestinal symptoms can improve by treating IBS. Frequent brushing with soft bristles and flossing can help with periodontal disease. Dental appliances can help with TMJ pain. Maintaining adequate hydration and salt intake is important. A dental exam and cleaning twice a year and an echocardiograph exam to check for heart abnormalities are recommended.
EDS is considered a rare disorder but this is most likely because it is under-diagnosed. Physicians are most familiar with the classical type of EDS, which manifests itself in hyper flexible joints and hyper elastic skin. The diagnosis of EDS hypermobility type is much more difficult because the outward manifestations are more subtle.
The Beighton Score uses a small number of joints and is meant to be a general guide. Some patients may not score high on the prescribed joints but be hyper-mobile in other places such as the spinal cord, hips or shoulders. Also some patients may be flexible as children but become less flexible over time due to injuries. A physician has to be very familiar with the disorder and look at the whole picture of the patient to make the diagnosis.
- Check out more of Darden’s blogs on Health Rising here
- Check out her website here
- Check out video’s on EDS here.
- Health Rising’s EDS Resource Section








I saw Dr. Sharon Meglathery mentioned here and she has quite the intricate theory about how these diseases go hand in hand. Would it be possible to see an article devoted to her work? Cort?
Yes, one is coming up – thanks for the reminder 🙂
They go hand in hand simply because they can have similar symptoms. This does not mean they are related to each other or are all part of any one specific disease or syndrome. One person may have been misdiagnosed with FM and later discover it was Ehlers Danlos another person will not.
These symptoms can be given different diagnosis depending on certain criteria. Ehlers Danlos hypermobility type is simply one version of Ehlers Danlos that they have not yet found a gene for so a lot of things can get lumped in there and people categorized with it if they are not careful in their diagnosis.
People with it can have similar symptoms to FM but have a history of hyperflexible joints and often have pectus excavatum (like those with Marfan). So, it can be readily apparent that there may be a genetic cause and not an infectious one. This helps distinguish the symptoms from getting another diagnosis, like FM.
However, even vitamin D deficiency can cause pectus excavatum, POTS, bone pain, and some of the other symptoms also experienced by people with FM, CFS, and Ehlers Danlos. These days, D deficiency is a new problem often caused by trying to protect ourselves from skin cancer.
So, chicken and egg problem. Do people with CF have low D as a side effect or is low D part of the problem causing FM.
The diagnosis of Ehlers Danlos type III is made by exclusion (done by symptoms and the exclusion of anything else being the cause) because there is no genetic test. They (FM, CFS, Ehlers Danlos-hypermobility type III) are diagnosed by a collection of symptoms. Syndromes are a collection of symptoms and conditions given a label by how frequently they occur together.
Syndromes may have genetic causes or the cause my not yet be identified. Some of these syndromes may be categorized as diseases in the future depending on if they find a certain cause. POTS is one symptom of many of these syndromes. The other types of Ehlers Danlos have had genes identified. It is likely just a matter of time.
Dear Meg,
Vit D deficiency (as measured by amount of calcidiol (the inactive form) in blood is not sufficient; the active form (calcitriol can be very high) as in sarcoidosis , FM and probably other chronical illnesses.
For more information and a lot off discussion on the subject see ;
“supplmenting with vitamin D?not so fast by Meg Mangin.
Did anyone check this with Ehler Danlos?
Or could low Vit D be a compensatory response of the body? I recently found out I have calcification in soft tissue. I have low Vit D levels. Research says it can be caused by either not using Vit K along with Vit D to keep calcium in the bones or it can be the bodies way of lowering Vit D as a response for too high calcium for whatever cause. Having MCAS (mast cell activation syndrome), I use GastroCrom, one of my best meds for both my MCAS and POTS). It is a very mild calcium channel blocker along with being a mast cell stablizer. Having been trying to up my Vit D with 10,000 a day of Vit D and it barely budging, makes one wonder if my body doesn’t need extra Vit D after all. It could be trying to keep my calcium in check by staying low. I have recently lowered my Vit D and added Vit K a few times a week. Being summer I get in the sun more now. We will see how it goes.
Issie
Nice write up and description of what us EDS, POTS and MCAS people have. EDS was a biggie for me. How about crossing your legs, in a standing position, and putting your hands flat on the floor – yes I can – and I have long legs I’m 6′. I was first DXd with FMS. But I wonder whether FMS and EDS3 are one and the same. I appreciate that you are helping in getting more awareness out there. Good job! I do think there may be a close connection with MCAS and EDS3.
Issie
Issie:
Was just rereading this thread and saw above that you are taking Vitamin K? Please be very careful. Vit K is what helps our blood clot. I have a clotting disorder; I clot too easily and have had 4 Pulmonary Embolisms. I’m on blood thinners and I’m to stay away from all foods High in Vit K. It’s a big deal, most people get more than enough if you eat a healthy diet as Vit K is found mainly in leafy green veggies and fruit like blueberries, etc. I had to give up being a vegetarian when I was diagnosed. Please be careful. I’d hate you to have a blood clot from taking Vit K. Please ask your doctor.
Thanks, I don’t take it daily. Just a few days a week. With the high doses of Vit D I was using it was something I needed. Have lowered D down. Will see how the ranges go with my next test. So many of the herbals I am on would counter it. But need to keep calcium in my bones, not soft tissue.
Thanks for the heads up, I’ll be cautious. Sorry you have had those issues.
Issie
I’m on blood thinners also for factor ll, factor VL and protein S defincency. Which ones do you have?
I have been urged to be tested for EDS for years. I just have never concentrated on it because of all of my other issues. I had a hip replacement when I was 42 because I had grown tumors in that synovial joint. My awesome orthopedic surgeon was concerned about my extreme flexibility. He would tell me that I was flexible to a fault. I score 4 out of 5 on the scale when I’m healthy and practicing yoga. I score 3 of the 5 when I’m not practicing yoga. Yoga was effortless when it came to stretching poses. Yoga is an amazing workout and would never claim that it wasn’t a difficult practice…the ease came only with the stretching poses. As always I have most of the co-morbidities, which are the same the come with Fibromyalgia. I love the information given here. Finally some testing I can have done.
What are the genetic markers to look for?
Unlike the other forms of EDS, it appears that genetic markers for EDS type 3 are yet unknown. However, there is the hypothesis that this subtype is, in fact, just a symptom of MCAS. In this case, the following genetic markers relevant for MCAS may also apply here:
http://link.springer.com/article/10.1007%2Fs00251-010-0474-8
Strangely, I have two friends who have EDS. One had no problem being diagnosed since it was passed down through the generations and she had a very severe case. Her skin breaks open with the slightest bump and her legs were covered in scars from repeated injuries by the time she was 20.
EDS is divided into 6 major types and all but one, the Hypermobility type, the most common, can be confirmed with genetic testing. There are also some lab tests that can be used to diagnose some of the other types.
http://ehlers-danlos.com/eds-types/
I suspect that EDS is more common than thought since so many doctors are not aware of it or think it is extremely rare.
Have you thought of doing 23andme testing? It must be able to pick up something to indicate a possible diagnosis of EDS, would it not?
Dear Claire:
I have often considered taking the 23 and me testing, but I am really unclear on what you receive. Are the genetic markers analyzed and explained to you? Also the last time I was seriously considering it they were shut down. Now that they are back up and running I should look into it again. I wasn’t until I had some testing done that I discovered I had Epstein Barr and Mono and I didn’t even know I had either. I need to get in touch with them and get some clarity on what it is you receive back from them. Thanks for the suggestion!
EDS hypermobility type cannot be diagnosed with genetic testing. Dr. Schirripa insisted that there is a lot of scientific evidence that the disorder is genetic even though the specific gene mutations have yet to be identified. The other 5 types of EDS can be diagnosed with genetic testing but not with 23 and me. At Dr. Shcirripa’s recommendation I am having my whole xome sequencing done by a lab called Gene DX.
Yeah, I tried calling them today but they had a “heavy call volume” and asked me to call back later?! So I went on youtube and found some reviews and basically they don’t give out very much health information anymore. Now it’s $199 and you get a lot of ancenstory information. I think they’re trying to find their place, but I’m not going to do it.
I have my 23&me testing. It does show me with genetic markers. But, the only type you really want to be completely aware of is the Vascular type. With it there can be anuresiums. I even flag high on a chance of anuresiums with 23&me. But having talked to a geneticist at Mayo about it and not ever having a rupture, other than my appendix, she didn’t feel I needed to have the expensive testing. Just knowing I have some form of EDS is enough for me. There isn’t anything that can be done for it other than “putting a bandaid on it”, anyway. You just have to be aware and do what you can to support yourself. Not having kids, I won’t pass it on. My sis has had her kids and they have it. So, we just do what we can to have quality of life with what we got handed.
Issie
you have the info. Download onto http://www.geneticgenie.org and get your results. Lots of info.
Hi I hope it’s ok if I just pop into this great discussion. I only want to mention a caution that having certain kinds of testing done can be problematic in terms of insurance. This has affected me and my husband for mortgage insurance. We were originally both covered so each had the mortgage paid if the other died. But when my health issues began and I was being tested for many different things including neurological disorders, we were also renegotiating our mortgage at a different bank and had to resubmit our health investigation info. They declined to cover me even on appeal and even though, as docs kept saying, MS is not so much a lifespan-shortening disease anyway! And that was even before I had an MS diagnosis. And that’s been set aside anyway many years on with the diagnosis of FMS (plus other autoimmune stuff). So beware. Just having had some MRIs was an excuse to decline my coverage. So if it’s not something you definitely need to pursue, you might want to save yourself the aggravation and worry.
Note: we’re nearly finished paying out the mortgage so I’m relieved that if I were hit by a bus, my husband wouldn’t be stuck paying our mortgage on just one income.
What a horrible thing. You have to pick between getting the testing you need or getting mortgage insurance. This sort of insanity makes me really hate insurance companies. They’ll take your money as long as there is no risk…what!? They are in the risk business!
Amazing the co-morbidities that can go with FM. You mean some people get FM because of a condition of hyper-mobility in connective tissue? And they don’t lose that hyper-mobility?
I am wondering now whether a lot of the symptoms I have, that I thought were all FM, are actually FM plus other co-morbities – completely different ones to the people with EDS plus FM, say.
With me, FM has always been associated with muscle tension and reduced range of movement – and I certainly never had extended range of movement, far from it, even in my fit, pre-FM days.
But is my FM, and my myofascial tightness and pain, and my muscle trigger points, and my POTS-type symptoms, all different problems – “FM plus co-morbidities”, not “just FM”? If so, I wonder what came first – is my “FM” actually a response to another morbidity that came FIRST – just as EDS “comes first” and triggers FM in the examples on this thread?
Philip,
It’s my belief that Fibromyalgia is a disorder of the nervous system. It often happens when one experiences trauma so great that the nervous system doesn’t recover properly. For me the trauma happened in 2009. I just never recovered, but instead I started having a ton of aches and flu like symptoms. My skin could barely tolerate the sheets laying on me in bed. I was an early to rise girl, and completely stopped waking up until noon and couldn’t go to bed until 3:00 am. I already had IBS, so I don’t know if we already have the co-morbidities and they worsen with Fibromyalgia. I don’t know if the many many tendon problems I have are related, are part of another disorder or are just another part of my bad genes. I have 3 autoimmune diseases, countless tendon disorders. Also I have bones that ache so badly. One of the worst aches ended up being a rare tendon disorder in my foot. Cast for 6 months and I wear a steal rod brace on that leg now. I can’t separate it out. Don’t know what’s fibro and what I would have had anyway. It’s all just bad.
I used to believe that it was entirely a chronic stressful (and unjust) situation in my life that gave me FM (it was not a sudden shock, it was a prolonged and chronic situation). But I have come to think that there were one or more other factors as well. Some hereditary, or dysfunctions from birth that have never been diagnosed; possibly an infection or an exposure to a toxic substance at the same time as the stress. The body may be able to cope with one thing on its own, but all 3 at once tipped me over the edge into FM. With me the toxic substance was cadmium. I did not know about it till years later (hair mineral analysis testing revealed it). Possibly my body became dehydrated trying to excrete the cadmium, and the dehydration combined with the stress resulted in the permanently tense fascia and muscles, and the formation of knots and trigger points.
Another hypothesis that has occurred to me, is whether a pre-condition some of us had all along (from birth?), was some dysfunction of autonomous muscle control. Like a mild version of cerebral palsy. I am being told off now by a therapist who tells me I have “lazy abs” with the muscles permanently relaxed – when they shouldn’t be – and a thrust-out rib cage due to THOSE muscles being “tensed” when they shouldn’t be. This is so like cerebral palsy, that I wonder why mainstream medical research is not positing hypotheses that a similar mechanism is causing milder issues in some people.
FM as far as I was concerned, is about permanently tensed muscles (all of them all over the body!) when they shouldn’t be, so it is an epiphany to me if I have always suffered from SOME muscle groups being “switched off” when THEY shouldn’t be!
Really interesting Phil, I wouldn’t be surprised if this highly tensed, highly relaxed pattern is not true for most of us.
Philip,
I wanted to respond to this because I was diagnosed as having Cerebral Palsy at about five years of age and had surgery that never did much to correct the problem, but did make my muscle and joint instability worse. Upon taking my daughter to a geneticist regarding her extreme flexibility, sleep issues, and soft skin (all of which she has had since birth) I was informed by the geneticist that I had EDS too. The rigor in my legs that was diagnosed as CP was simply related to underdeveloped tendons due to my being born 2.5 months prematurely.
…was also diagnosed with mitral valve prolapse at birth, mitral valve prolaps, supraventricular tachycardia at age 12, and POTS at age 19.
Does anyone understand why the autonomic nervous system would be down regulated, or at least involved, with this connective tissue disorder? I have ME/CFS with low autonomic nervous system functioning such that one of my “sub-diagnoses” is called either Pure Autonomic Failure or Pandysautonomia. As far as connective tissue is concerned, mine is hard, contracted along with muscles, and it also seems to be shrinking with age. What in the world is the connection between the muscle and connective tissue symptoms and the autonomic nervous system, I wonder again?
With EDS we are always in a contracted state trying to hold ourselves together. Our muscles get fatigued from always contracting. We have pain not only because we are so easy to sublax something, but because we are in a spasm from constant contraction.
As for things being out of place – that is a common occurrence with us EDSers. We get good at twisting or pressing and putting ourselves back in place. We learn tricks of certain ways to sit or lay as to not throw something out. Many use bracing if they are really stretchy. Yet, for me to sleep and get out of enough pain of “tight” muscles – I take a very mild muscle relaxer at night along with another med to calm the overactive autonomic nervous system of HyperPOTS. Then I have to put pillows in certain ways to sleep as straight as possible, and support things when I’m trying not to contract and sleep. Hey, whatever works.
It’s not unusual for EDS3 to be in families. Mine goes back 4 generations now. Along with POTS and MCAS. I have theories and hypothesis – but no way to prove them. Some docs are looking into it though. So maybe, we will know more in the near future.
As for PANDAS in dysautonomia – that type is closely connected to a strep infection that brings on the dysautonomia. There is extensive treatment for the underlying infections. Also, I know of several who have also found Lyme as part of their DX With Pandas. There are some mothers on the DINET site who were a few years ago talking about their kids and their endeavor to help them. You may can do a search and pull some of it up. That type of dysautonomia is different from PAF (pure autonomic failure). It brings on many brain functioning issues.
Issie
Issie:
I find what you say here to be very interesting. If I have EDS, I have the hyper-mobility type. What you said about our bodies always trying to keep ourselves together; one day I was in an elevator and my back felt tight. I was alone, so I quickly did a front bend, hands flat on the floor and when I came back to a standing position, I knew something didn’t “fit back in right”. It was the was my “hips” landed in my pelvis. I say “hips” because hips aren’t a body part, but a joint created by the femurs fitting into the pelvis. That was years ago and I never felt it go back in place. It creates a special sort of pain when I sit and try and twist or scoot in the sitting position. It’s not a subtle pain, but one that makes you gasp and stop. I find myself holding my body in a way that prevents me from getting the pain, but also isn’t very natural. I’ve also been diagnosed with a tendon disorder in my foot and my hip flexor is really messed up. Again, I don’t know if I have EDS, but I do know my tendons cause me a lot of pain. In terms of genetics expressed, I always say you could pick my sisters and mother with bags over our heads but our knees exposed. Our knee joints all hyper extend.
I have been diagnosed many years ago with EB virus, CFS, and FM. Now I have constant loud ringing in my ears….any connection?
I don’t know. Tinnitus is a fairly common condition; I have it but it would be interesting to see if its increased in ME/CFS. It could be…
A lot of us have tinnitus, but that can also be caused by MCAS as well as ME/CFS, other autoimmune processes, plus a bunch of other disorders (including “depression”).
I had a severe virus,similar to the EB Virus. It was about the time of outbreak in Incline Village. I was flat on my back, out of work & I can say my life changed at that point. Since I have been tested for everything and diagnosed with FM/ME. What caught my attention in these comments was tinninitus was my first symptom. I returned to work weak, but I began to get a ringing in my ears. Often so loud I couldn’t hear. I eventually got control by cutting out certain foods that I had suddenly become intolerant of. That was just the beginning of a long list of changes that have occurred.
Dear Darden,
I would like to point out that it’s hard to distinguish between primary and secondary disease, and after reading Dr. Afrin’s case reports on MCAS, I do believe that EDS3 is secondary, and MCAS is the primary disease. In other words, it may be that EDS is just the symptom, and chances are that herapy directed at mast cells (H2 antagonists, chromoyln, quercetin…) may significantly improve symptoms.
Review article on MCAS: http://www.wjgnet.com/2218-6204/full/v3/i1/1.htm
Of course, everything may be different from what we think it is, but I do recommend looking at MCAS more closely. 🙂
sounds familiar….
Great job Cort!! You are so amazing! With you at the helm, we should be out of bed in no time!!
Here’s to Cort!!! Thank you so much for keeping us so well informed
on what’s going on in so many different areas of ME/Fibromyalgia. Be it research, funding or the latest physiologic discovery, we get it straight from you. Given your diagnosis, it’s amazing you have the energy and the clearness of thought to deliver the information in a clear and precise manner. I never give you credit for all you do, well not often enough, so go Cort and you are doing an amazing service for us all.
This has been the best article i have read in a while. I was diagnosed with FM 6 years ago now. So many things have come up since then, mainly with my daughter developing problems in the last year and spending many doctors appointments trying to find out what is wrong with her for to be diagnosed with EDS type 3 and soem other problems that go with it. I too have suffered the same as my daughter with EDS symptoms, but i had never heard of this until last year. Now that i am 47 and she is 21 it is all making sense now. My aunt and grandfather on my mothers side also had EDS symptoms and i wonder if it could skip my mother but me and my daughter got it. Mind you she did have some of the symtoms but not all of the beighton scale signs like my daughter and i do. I know my grandfather died from a aneurysm in 1952, but how much did we know then. My aunt passed from vascular issues about 10 years ago, so again, not much to know now. But with this EDS diagnosis for my daughter and some of her problems it is all making more sense.
I think EDS is a contributor to the “perfect storm”, but not the only cause. I know a number of healthy, normal people with hypermobility syndrome/EDS, yet I like many others, plunged unexpectedly into severe illness and have diagnoses of ME/CFS/Fibro, EDS, MCAS, and SIBO. Dr. Afrin and others mention the connection between EDS and MCAS (Dr. Afrin even postulates that EDS type 3 could be MCAS, although that is his filter). I have low NKC function and reactivated herpes and tick borne illnesses, like many of us, and don’t see the EDS connection in this area of the illness.
I agree. I think it is a piece of the puzzle. I do think that MCAS and EDS are connected. And yes, us with a faulty immune system seem to have Lyme and other protozoa issues.
Here is a good interview of Dr Afrin on an EDS site.
http://www.chronicpainpartners.com/webinars/
Really pay attention to the slides and stop to read them. They tell so much more than he verbalizes.
Issie
Thanks for the link :).
Hmmm, very interesting. I have often considered EDS hypermobility, as my thumb joints and some fingers hyper-extend and my body cannot take any push, pull, or jarring (ie any type of exercise). When I travel, I use a neck pillow and another foam pillow on my lap to stabilize my arms so they don’t pull down at my shoulders and strain muscles, etc. However I, like another person posted, can’t touch the floor – or my nose with my tongue etc. Instead it seems like my muscles are tense and tired – but I do relate to some EDS symptoms, like burning eyes, IBS, SIBO, tendon issues, sprains, etc. When I get stressed in one part of my body, all my tendons and joints get “clunky” and clicky,( hard to explain but others with this will identify….lol) This also sounds similar to what Darden said ” Rather, my muscles are working extra hard to protect hypermobile joints.” Darden I guess I will have to try some of the supplements mentioned and see if they make any improvements. Always a pleasure, Cort, to see one more possible piece of the puzzle on Health Rising! Much Appreciation for all your work!
I got diagnosed with EDS at the age of 53 and POTS at 55. At last it was the right diagnosis and not ME/Fibro. I’ve since found out I have also got mast cell/histamine issues and a pituitary tumour.
I just found out that I have Ehlers-Danlos Hypermobility type at the age of 44 I was originally diagnosed with Fibromyalgia 20 years ago. So was my mother and my grandmother had problems with this and so does my daughter and other females in my family. Just thought I would share. I wish more doctors knew about this and could get it right the first time.
Are you also allergic to nickel?