

Fibromyalgia/ME/CFS sure feels like it’s in the muscles. After exercise, at least for me, they’ll often feel constricted and painful and muscle stiffness is common. The central “sensitizationists: (look -a new word :)) say those pain sensations are the result of the central nervous system misinterpreting signals coming from the body. There’s nothing wrong with the muscles – the problem is in our heads (so to speak). It’s in the upregulated pain sensing and downregulated pain inhibiting pathways in our central nervous system.

Plus, given the underwhelming performance of central nervous system acting drugs in fibromyalgia, and the difficulty accessing the brain, we might hope that something is happening in the body.
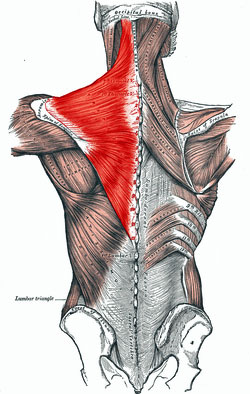
If it is happening, one place it might be happening in, is the trapezius muscles. The trapezius muscles that run from the shoulder down to the middle of the back and up to the neck might just be ground zero for the upper body pain in FM. If you have upper body pain – and upper body pain appears to be rife in FM and ME/CFS – the trapezius muscles are probably involved.
This recent study on the proteins present in those muscles sought to understand why they’re so often so painful.
The Study
The researchers took biopsies of the trapezius muscle in 18 people with chronic widespread pain/fibromyalgia and 19 healthy controls and examined the proteins found. (The authors referred to the patients as chronic widespread pain/FM patients.)
Results
The study found that the proteins found in the trapezius muscles of the two groups were different. Twelve proteins were highly correlated with increased pain intensity in FM, and 11 proteins were associated with reduced pain thresholds in FM.
The proteins identified suggested that the muscles of these CWP/FM patients were inflamed and under stress. That problems with energy production (i.e. the mitochondria) may exist, and that muscle damage had occurred.
Proteins Associated With Increased Pain Sensitivity
Several proteins stood out. One (ankyrin repeat domain-containing protein 2) that was highly correlated with increased pain sensitivity defends muscle cells against injury and regulates inflammation. Low levels of this protein suggested that the FM muscle cells having trouble, protect themselves against damage and/or dampen down inflammation.
Because the inflammatory pathway (NF-kB) this protein regulates has been found upregulated in FM, low levels of this protein could induce inflammation and reduce the muscle cells’ ability to cope with it.
Reduced levels of two proteins (carbonic anhydrase 363–65 and heat shock protein) that play protective roles against oxidative stress suggested the muscle cells might be getting whacked. Another that (Triosephosphate isomerase) plays a role in glycolysis suggested energy production had taken a hit.
All in all the results suggested that low energy muscle cells were immersed in an inflammatory environment they have trouble protecting themselves against. (No wonder they’re sending out pain signals.)
Muscle Proteins Associated With Increased Pain Intensity
When they looked at proteins associated with increased pain intensity the ankyrin repeat domain-containing protein showed up again – cementing it, at least in this study, as potentially a key player in the muscle problems in FM. Increased levels of glutathione transferase suggested the muscle cells were busy trying to protect themselves from high levels of oxidative stress. Decreased levels of an enzyme (a creatine kinase) involved in the ATP production process suggested that energy production was low. Increased levels of other proteins (myosin light chain 6B, troponin) involved in muscle atrophy and chronic muscle disease rounded a protein study which suggested significant problems with the muscles may be present in FM.
Other Findings
Considerable evidence also suggests that something is going on in the trapezius muscles of people with FM, and a related disorder called trapezius myalgia and/or chronic widespread pain.
A 2014 study found increased concentrations of lactate and glutamate in the trapezius muscles of people with chronic widespread pain. Electromyography readings indicated that trapezius muscle activation during mental stress tests, breath holding, and even during eating may be contributing to the upper body pain. The study suggested mild stressors contribute to upper body pain in people with FM.
In fact, people with trapezius myalgia (TM), display the same autonomic nervous system signature (low heart rate variability) found in fibromyalgia and chronic fatigue syndrome. Their low HRV readings during sleep suggest they may experience the same type of ‘micro-arousals’ speculated to occur in ME/CFS and fibromyalgia at that time.
Micro-circulation tests indicated that an hour of computer work resulted in reduced blood flows and oxygenation saturation and higher lactate and pyruvate levels. Another study that found high rates of ‘hypertrophied muscle fibers and low rates of capillarization sounded like a recipe for low blood flows.)
The upshot is that there’s good evidence something is going on in the trapezius muscles of people with TM and/or FM.
Conclusions
This was, by the author’s accounts, a small exploratory study that needs to be validated. It provided enough potential clues to FM that hopefully it will be repeated and expanded upon and will encourage more research into the muscles in FM. With recent FM studies finding evidence of reduced microcirculation in the lungs – possibly due to nerve damage – and more small nerve fiber problems in the skin and the eyes – the body is becoming an ever more interesting place.
- Is Nerve Damage Affecting the Lungs in Fibromyalgia?
- Eye-Opening Finding: Small Fiber Neuropathy Found in Fibromyalgia Patients Eyes
The cause of those problems, however, is a mystery.






Thank you, Cort, for continuing to bring us the research news. I have had muscle aching for forty years. My life is organized to minimize it, but still it plays one of the theme songs of my day. I will be glad when the fictions applied to FM and ME/CFS are thrown out and scientific fact replaces them. But to get there we need not just money but intelligently designed research projects. My suggestion for this is to draw on the knowledge of the best clinicians or else an in-depth knowledge of the history of this field. For newcomers, wanting to make a quick name for themselves in a neglected field, to simply apply the latest “gadgets”–the currently fashionable methods and areas of study–the result is likely to be more wasted dollars and years. There is no substitute for either a thorough knowledge of the field or at the least, that of drawing on the knowledge of the clinicians who know our systems the best.
Well said Cecelia!
Isn’t it true that all along, massage therapists and those who work with the muscle tissue of FM sufferers, have been able to feel the problems with those muscles – the taught bands and the trigger points and so on? The “it’s all in the mind” hypothesis has always been the nonsense one. The problems with the muscles may stem from dysfunctions in the brain, which is the case with Cerebral Palsy and other conditions too, but to allege that there are no problem with the muscles is just cruel and arrogant. Nothing like the arrogance of some experts who don’t want to admit when something is too complex for them. This is taking far too long to change, even many of the alternative health practitioners I see who are not specialised in FM-related knowledge, seem to have read some outdated encyclopedia entry and proceed to mouth off the same old bullshit to me about “attitude” and so on. In fact it would not surprise me if there is some source of information for alternative health practitioners, that all of them are reading, which is completely wrong and cruel about FM.
It’s amazing how certain ideas – often associated with a paper or two or an experts pronouncement – can get cemented in the medical communities mind. You might very well be right.
I agree with your comment on the arrogance of “experts” who think they already know everything!
I do want to point out, however, that trigger points and taut bands are symptoms of myofascial pain syndrome, not fibromyalgia. Of course, most fibromyalgia patients have myofascial pain as well, I believe because pain leads to increased muscle tension (protective reflex). Massage is very helpful at treating myofascial pain, reducing a significant source of pain in fibromyalgia.
I sometimes wonder whether Fibromyalgia is merely a set of symptoms like “dizziness” or “excessive urination”. Diagnosing “fibromyalgia” merely lets the medical profession off from getting to what the actual cause is, of the painful spots. As if a diagnosis of “dizziness” would be acceptable.
I believe in my case, and possibly typically, the myofascial pain syndrome PRECEDED the “fibromyalgia”. Some other people with “fibromyalgia” have Ehlers-Danlos syndrome, muscle tissue hypermobility, the absolute opposite of “tightness”. Others have a thyroid malfunction. Others have something else. In all cases, the actual diagnosis required, is something more than “fibromyalgia”, which merely means “a few sore points at a recognised pattern of locations”. People have suffered for years with the CAUSE of those sore points undiagnosed, because the diagnosis has been one of a condition “with no known cause or cure as yet”.
My own experience, hypothesizing and self-treatment applies to “fibromyalgia by way of myofascial pain syndrome”. This, incidentally, is the one common form that has “no known cause or cure” – the people who get something else diagnosed eventually are luckier. I believe that research needs to concentrate, for the majority of us, on “why the myofascial ground substance goes sticky”.
After following research and theories on FM for 15 years, most of which I find useless, this article caught my attention. It definitely fits with my upper back pain that is constant. What we need to know is what can we DO for this?
That’s a good question.. When I feel around my shoulder blades the muscle attachment points are all painful. I would dearly like to know why the upper body is so effected for me. Everything about my sternum basically hurts – below my sternum its all lax.
Unfortunately no treatment outcomes come out of this study; it points an arrow at inflammation and the mitochondria and hopefully future studies will determine if they are a problem and produce some treatment options.
With me it was never just about the upper body, although it certainly has been tight and painful right from the head downwards; the neck, the shoulders, the pecs, the back, etc. But I have always had tight, painful big leg muscles that I said felt like “rocks on fire”, and never responded to massage treatment other than to get worse. Furthermore, the groin area had extremely tight fascia. All these symptoms have been slowly getting better under my approach of the last 3 years.
Yet it has recently been a revelation to me, to learn that I have had SOME lazy, under-utilized muscles that are highly important in musculo-skeletal function. The abs and the lats at least. This gets me thinking, why did these muscles not go tight and get riddled with trigger points? So FM obviously does not attack “muscles” indiscriminately. Therefore, I suggest that FM ends up affecting muscles that are in situations of tension and static load for longer periods. One practitioner suggested to me that FM people with leg muscle problems, often have had a job that involved a lot of standing. In my case I believe it would have been because I did a LOT of bicycle riding.
The upper body problems most of us have, possibly relate to having a sitting-down job with arms constantly “held” at a particular angle – a gentle static load but nonetheless significant. But the tendency to relaxed leg muscles most of the time, is the explanation for the absence of problems there.
My hypothesis now, is that there is a problem with muscle lubrication – I have said this before – but that the results are that muscles under constant tension or static load, are the ones that end up with “stuck” fibres and layers, and trigger points. Muscles that are NOT being used (or mis-used) in this way (such as lazy abs) escape the formation of the stuck and knotted fibres and layers.
There may well be inappropriate stress responses involved – muscles tensed for a long period when they should not be – but I believe that people without FM can suffer from this tension and not end up with the stuck and knotted fibres and layers. I believe research for the cause and cure for FM needs to be focused in the area of muscle lubrication and its loss. It may be “loss” of lubricant ingredients or it may be “build-up” of “glue” ingredients such as calcium and lactic acid. I believe that the many other symptoms, including the blood flow ones, are the consequence of blood vessels, major and minor, simply being trapped in tight muscle fibre and fascia – rather than the original cause of the loss of lubrication.
Boy Phil – it sure feels like the muscles need “lubrication”; it feels exactly like that. I like the insight into the lack of painful spots on the abdomen as well. It seems to me that some of my painful spots are where the muscle appears to attach to the bone…
You’re talking about ground substance here, Phil. This is the nitty- gritty of the bodily manifestations of FM, LOL! I like where you are going, though. Not so much lubrication as shock absorbing. For more about this I really recommend the book “Healing Through Trigger Point Therapy, A Guide to Fibromyalgia, Myofascial Pain and Dysfunction” by Devin J Starlanyl and John Sharkey. Devin is carrying on and expanding the work done by Travell and Simons and gives a good overview of trigger points and their relationship to FM (she is a central sensitisationist! but sees this as an exacerbation to the pain of trigger points and originates from one or several FM initiators). Take a look at her diagram of The Cycle of Misery – the trigger point formation hypothesis. I got my copy very cheaply on kindle. I also recommend Trigger Point Dry Needling, An Evidence and Clinical Based Approach by Jan Dommerholt which gives an in- depth look at the biochemical changes induced at the cellular level by trigger points. Unfortunately this one is not available as an E-book.
I was able to read it online however by googling “protons and trigger points” – 11th entry down when I did it.
Tricia, it is quite possible you are right. Even if the problems with lubrication are limited to the myofascial ground substance rather than in the tissue of muscles themselves, it would still be an explanatory hypothesis. Of course there is a lot more myofascia where muscle attaches to bone, which would explain worse pain at those locations. I have Devin Starlanyl’s book and endorse your recommendation of it.
Do you think this study could help those who are experiencing pain with arthritis or suffering from pain through conditions such as lupus and sjogren’s.
Im almost certain that the cause for everyone is exposure to some chemical that effects the nerves through skin contact. (aware or unaware of exposure) This would mean chemical exposure of some kind which does damage to nerves, damage to brain and hence causes inflammation. We need a systemic solution, not easy because one must clear the toxin from the body(not easy), repair damage to nerves and brain(not easy), and heal the immune system… the very bottom of the problem. The nervous system damage is the root cause, inflammation and pain are the symptoms along with all other symptoms. We need repair system wide to the entire nervous system. Any ideas?
Carrie; I believe it is quite possible that my suggestion (see above) of “lack of lubrication in muscle fibres” is caused in the first instance by some form of dehydration as the body is trying to rid itself of a toxin. This certainly fits my own case: my first sign of problems, that I did not even connect with the eventual FM (of course the medical people do not make the connection either) was chronic, long-period episodes of excessive urination. I thought I got it under control with electrolyte supplementation and also hair mineral analysis testing that showed what I was deficient in. But the onset of all the classic FM symptoms probably commenced from around that time.
The toxin in my case, seems to have been Cadmium, unfortunately. This does not show up in any testing until it has reached saturation in the renal system. It started to show up in hair mineral analysis testing years later. Part of my recent-years protocol that has gained me a lot of improvement, has had one result of successfully lowering the Cadmium manifesting in the hair tests; but it will probably require years of flushing for the renal system.
Where did I get poisoned by cadmium? It is years too late to prove anything now, and none of the known sources were present in my life.
Yes, this is a great article with some hope. I’ve had FM (and ME) for so many years I really can’t even point to a starting time anymore.
I’ve always believed the mitochondria (energy production), problems with Vo2 levels and high lactate in the muscles are the key to FM-but who knows. Adding on ME makes it all the more confusing.
I must constantly remind myself to breathe deeply as I do hold my breath without realizing it and my core muscles up to my neck are in constant spasms and pain no matter how many relaxation and stretching exercises I do. Some of my inflammatory markers are high so there is constant low-grade inflammation.
Sucks doesn’t it! 🙂
I do too – I hold that breath all the time – maybe that breath is what contributes to the particularly tight upper body muscles???
Yes, breath-holding may be one of multiple factors that predispose someone to eventual FM. Related in every case, to stress? Or not?
I definitely agree that somewhere in the process, the body’s lactate clearance mechanism gets disabled. Then ever-present lactate becomes one of the ingredients in the “glue” that causes muscle fibres to cease sliding against each other as they should, and get caught together in bands and knots and trigger points.
What researchers need to try and discover, is what sets off this series of dysfunctions. Including what COMBINATION of factors are like a pre-condition for it. So many normal people suffer exposure to one or more of the factors without “getting FM”.
This really caught my attention. I have been diagnosed since 1992 by the VA with FM. It is amazing since it is almost impossible to get anything approved by them especially with the vague diagnoses we seem to live with. I have always sought treatment outside of the VA system since diagnoses is one thing and progressive treatment is entirely different. Anyway, to what caught my attention. I had a mild heart attack back in October of last year and the doctors commented every time they talked to me about my very slow heart rate, at times 45 bpm. They wouldn’t even put me on the normal treatment of beta blockers because they were afraid it would just stop beating from them.
I can tolerate immunical. That is the only whey protein that works for me. What it does amazenly is get rid of most of the pain whien I am not pushing by body.
Dr Klimas office newer Doc, Dr. Vera I believe was so surprised at the fact I had almost no pain on trigger points. I can tell you however that without imminocal they come back. All over.
I have been using since 2000. It also practically gets rid of my insonmia and sleep issues. Taking it the morning after waking up helps to turn on my mind and body
I belueve it is because it increases glutathione production which scavenges lactic acid.
It also has a profound effect on neurotransmitters. Which helps with alertness and circadiam rythm.
I found it is important to determine the right amont to take. Too much of it backfires.
If in great excess it can increase inflammation significantly.
I was told to start slow and increase to 2 lacks per day. I can only tolerate 1 ti 1.5. In divided doses It needs to be provided to my body in regular intervals because it wears off in about 4 to 6 hours.
It is not perfect because it drops my blood sugat and I eat apples and chicken to help the drop and a transient neesd to eat animal protein. The need comes in about 15 to 30 min and it is essential that it be met. I wonder what is happening chemically.
But it works very well for me. Even with ups and downs. I tell my family they owe their substenance to my taking it. Enables me to work mentally for about 5 hours pet day taking braks laying diwn for 15 min or so every two hours.
Mr Raba
Cfs and POIS simultaneous sudden onset since 1993.
Oops name is immunocal. At amazon for 80 bucks per month. Depending on how much I take.
Mr Raba, that is good information–thank you for being specific. Might help someone else.
For my aching muscles, which keep contracting, I do both meds and movement. I take Gabapentin starting in the evening, then for sleep, and at the same times take Jarrow N-A-C Sustain, which is a glutathione precursor, and also l-Tryptophan. For movement, I stretch morning and night. Every other day or so I also use hard rollers–a “Ma-Roller”, and a large thick hard foam roller, on the floor. Using my weight, I get them to press into the painful places, especially where muscles attach to bone and sometimes right in the middle of muscles. A long methodical pressing, working over the body, is great. This seems to be opening up the contracted muscles to oxygen, circulation and waste removal (lactic acid removal).
That is interesting, Mr Raba.
I got an insight from something Cort posted about 3 years ago, about the role of lactic acid in FM. So I experimented with exercising strictly only at low intensities to avoid generating lactic acid; and I also went strictly very low carb diet. I made slow but steady improvement from that point. My threshold of tolerance for exertion has risen continually so that I can now sustain exercise of many kinds at a level that would have caused me a post-exertion malaise 3 years ago.
Medication that helps with lactic acid flushing is almost certainly going to be helpful for people suffering FM. But I have not tried anything, my own natural diet and exercise experiment seems to work very well. It is probably also important that I take lots of magnesium and also mineral supplementation intelligently guided by hair mineral analysis testing every few months.
I read a very interesting Story today a Woman diagnosed with CFS Fibro then diagnosed with Ehlers Danlos type 3 hypermobilty her entire Family was also diagnosed then she had Gastro test for sucrose which it was not she had fructose intolerance the was seen by a Metabolic Genetic
Doctor who ran his own test plus her Family all had a condition called ‘hereditary fructose intolerance’I sent the link to Dr Ron Davis’s Secretary…Fructose in numerous products fruits vegetables even home
cleaning items from dish soap shampoo soaps cleaners even in numerous candies…There is a bonafide blood diagnostic test available with Metabolic Genetic Doctors they all were Positives…
The study was made in Linköping in Sweden. For once Swedish resarchers make a positive contribution to biomedical resarch. A new ME clinic has recently been created at the Linköping University hospital. I keep my fingers crossed that Linköping keeps going in a positive direction. We need good biomedical research so badly, as well as clinicians specialised in ME.