



“This work opens a fresh path to both understanding the biology of CFS and, more importantly to patients, a robust, rational way to develop new therapeutics for a disease sorely in need of them.” Robert Naviaux
The Dafoe’s looked at each other in astonishment. They’d tested Whitney, their sick son, in every which way and had found problems but nothing that had reflected how ill he was – until now. His metabolomic results revealed row after row of abnormalities – some of which were levels of magnitudes off the charts. Instantly a new world opened up for them.
Two days ago the first metabolomics study in chronic fatigue syndrome (ME/CFS) using a similar approach was published. It may end up opening a new world for everyone with chronic fatigue syndrome (ME/CFS) as well. Ron Davis certainly thinks so. He believes “It is the most important and groundbreaking study of ME/CFS to date” and that Naviaux’s metabolomics research put us “finally on the right path to understanding ME/CFS”.

At some point Gordon, who was one of Whitney Dafoe’s doctors, suggested that Naviaux meet Ron Davis. Metabolomics had always been part of Davis’s “omics” core, but he hadn’t expected the results he’d gotten and it had become a major area of interest for him. When Naviaux met Davis a partnership with the Open Medicine Foundation (OMF) was borne. (Naviaux now sits on the OMF”s scientific advisory board, talks with Davis regularly, and the OMF is helping to fund Naviaux’s expanded ME/CFS study.)
Very few metabolomics studies have been done in ME/CFS and none on the level of the Naviaux study. What a piece of serendipity it was that these two figures – a short plane ride away from each other – ended up being connected through Ron Davis’s son.
The Study
Metabolic features of chronic fatigue syndrome. Robert K. Naviauxa,b,c,d,1, Jane C. Naviauxa,e, Kefeng Lia,b, A. Taylor Brighta,b, William A. Alaynicka,b, Lin Wanga,b, Asha Baxterf, Neil Nathanf,2, Wayne Andersonf, and Eric Gordon. www.pnas.org/cgi/doi/10.1073/pnas.1607571113
Naviaux began the paper touting the advantages he believes metabolomics brings for the analysis and treatment of complex diseases. At the most basic level there’s our genes and the environment and not much else. Throw these two together and you get metabolism and metabolites – the byproducts of cellular function. Measuring these metabolites gives you a snapshot of the cells physiology. Naviaux believes studying the metabolic by-products of our cells provides more biologically relevant information than any other approach and is more cost-effective as well.
In this study Naviaux, Eric Gordon, Neil Nathan and others examined 612 metabolites from 63 biochemical pathways in the serum of 45 ME/CFS patients (Fukuda / CCC criteria) and 37 age and sex-matched controls.
Twenty of the 63 biochemical pathways were highlighted in ME/CFS. Eighty percent of the metabolites that were abnormal were down-regulated. Nine of the biochemical pathways were altered in both men and women.
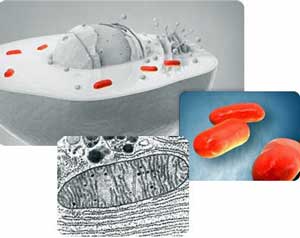
The Mitochondria and the Cell Danger Response
Mitochondrial metabolism is so fast that, like the canary in the coal mine, it’s the first organelle to detect danger or toxicity.
Naviaux believes the mitochondria are able to sense every kind of danger – from pathogens to pH changes to toxic elements from pesticides, heavy metals, etc. to inflammation. They sense trouble in the form of an infection when they detect a drop in voltage caused by the diversion of electrons (NADH / NADPH) to make viral components or respond to a broad variety of toxins.
In the cell danger response (CDR) the mitochondria respond instantaneously to that loss by decreasing their oxygen consumption – thus thwarting pathogens from using the building blocks of the cell to replicate. Because the oxygen is no longer being used, it builds up in the cells causing a oxidatively charged environment which interrupts viral synthesis. The CDR also stiffens the membrane of the cell to stop pathogens from exiting it, warns other cells of the danger, and emits ATP in order to warn other cells to get their defenses up.
Naviaux tends to think ecologically; where others see hardened cell membranes as a sign of damage, he sees them as a wall that the cell builds to keep the pathogens inside the cell. When others see the leakage of ATP, ADP, H202 and factors as a sign of cellular damage, Naviaux sees these substances as early warning signals to other cells.
Inside the cell ATP is an energy molecule, outside the cell it’s a “danger molecule”. Cells, Naviaux noted, work so hard to make ATP, that the fact that they would actually export it outside the cell was highly significant. Finding ATP outside a cell is a sign that something major has gone wrong.
Hunkering Down
“These facts suggest that CFS is an evolutionarily conserved, genetically regulated, hypometabolic state similar to dauer that permits survival and persistence under conditions of environmental stress but at the cost of severely curtailed function and quality of life.” Naviaux
Naviaux believes that sometimes survival means hunkering down; essentially shutting down the cell as much as possible. In the cell danger response you don’t engage the danger, you try to outlast it. Naviaux noted that many low energy states from diapause, hibernation, estivation, torpor, ischemic preconditioning, autophagy, caloric restriction have been described in the literature.
The fatigue in ME/CFS, Naviaux believes, is due to an active and purposeful inhibition of the mitochondria. The mitochondrial are not broken – they’re throttled back to a low idle. In the face of danger they’re shutting down and exporting ATP outside the cell to warn other cells that danger is present.
A Hypometabolic Disease?
There’s a lot of talk about subsets but these results suggest that a core hypo or low metabolic state may underlie all of them. No matter what kind of trigger started the disease or whether one was male or female, a core hypometabolic state stood out. The metabolites were a bit different in males and females but the core finding – a low energy state – showed up in both.
Naviaux’s isn’t the only study to find evidence of hypometabolism or to suggest that a hypometabolic state exists in ME/CFS. Marian Lemle first proposed a hypometabolic state was present in ME/CFS in a 2007 paper. (Read the paper here.) She published a paper, “Hypothesis: chronic fatigue syndrome is caused by dysregulation of hydrogen sulfide metabolism” suggesting that ME/CFS patients existed in hibernation-like/hypometabolic state in 2009. She proposed that the fatigued state ME/CFS patients were locked into protected them from the damages of overexertion. You can find more about her hypothesis in a 2009 interview Hydrogen Sulfide and Chronic fatigue Syndrome: The Originator Speaks.
The Zinn’s found ‘a global expression of CNS hypoactivation” Barnden found reduced brainstem activity. The Lipkin/Hornig immune and spinal fluid studies showed evidence of reduced immune activity in ME/CFS. Other studies have found reduced cortisol, reduced aerobic output, low blood volume, decreased parasympathetic nervous system activity and reduced natural killer cell functioning. Hypometabolism or hypoactivation seems to be the coin of the realm for ME/CFS.
Dr. Unger recently revealed, though, that ME/CFS patients display a wide variety of symptoms. Most people believe the disease is full of subsets – perhaps even different diseases. If the disease is at its most basic level homogeneous, where might the vaunted heterogeneity in ME/CFS come from? Ron Davis suggests that genetic polymorphisms might be one source and is working on a study that marries genes and metabolomics in ME/CFS. Davis has asserted that a mitochondrial shutdown operating at different levels in different systems could explain every symptom seen in ME/CFS.
An Evolutionary Hijack?
CFS is an evolutionarily conserved, genetically regulated, hypometabolic state similar to dauer that permits survival and persistence under conditions of environmental stress but at the cost of severely curtailed function and quality of life. Naviaux
Naviaux believes that the systems of people with ME/CFS have been hijacked by an evolutionary state that is adaptive during periods of great stress. The stressor in many ME/CFS patients is often an infection, but as Naviaux’s study showed can include chemical exposures, physical and psychological trauma, and no discernible trauma at all.
It appears that when Naviaux says evolution he means an ancient, genetically embedded response that first showed up in organisms far older than humans. In this evolutionary state the organism reconfigures its metabolism to use the least energy possible.
The closest animal state to what Naviaux’s results suggest is happening in ME/CFS occurs in worms which enter into a “dauer” state to survive harsh conditions. (Dauer is a German word for endurance). The ability of these worms to endure – they can live four-eight times longer in the dauer state than their usual lifespan – is so unusual that they’ve been studied extensively by biologists.
The metabolites altered in ME/CFS patients are similar to those seen in the cell danger response with one major difference: the metabolites that are upregulated in the CDR are down-regulated in ME/CFS and vice versa. (ME/CFS just had to be different.) The metabolic response in ME/CFS doesn’t look like the responses seen in inflammation, infection or metabolic syndrome – three processes that have been conjectured to be present in ME/CFS at one time or another.
The difference shows up most in metabolites called sphingolipids which accounted for almost 50% of the metabolic issues found. (Reductions in phospholipid metabolites were also prevalent. Many other alterations were found but these were the major ones.)

A “hypo” disease? The trendline in Naviaux’s and other studies has been down, down, down; reduced metabolism, aerobic functioning, NK cell functioning, brain activity, cortisol, blood volume, etc….
Sphingolipids play important roles in signal transmission particularly in nervous system tissues, and are believed to protect cell membranes against harmful environmental factors. Sphingolipid metabolites, such as ceramide – the most common disrupted metabolite involved in ME/CFS – are involved in signaling cascades involving stress responses, inflammation, cell death and much more.
Naviaux said he wasn’t surprised to find the sphingolipids reduced in ME/CFS – he’d found sphingolipid reductions in other hypometabolic diseases like autism and Gulf War Syndrome but he was surprised at how depleted they were in ME/CFS. No other disease he’s examined has had nearly the amount of sphingolipid reduction found in this one.
Naviaux believes this upside-down pattern “may represent a fundamental response to oppose the spread of persistent viral and intracellular bacterial infections.” In an MEAction blog that Naviaux was impressed with, Jaime described what may be happening. She suggested that ceramides might be down-regulated in order to disrupt the ‘lipid rafts’ that some pathogen use to enter the cells. It’s another method of locking down the cell. Jaime also proposed that Naviaux’s work suggests that Rituximab may be disrupting the same lipid rafts in ME/CFS.
A Living Death
A long-lived dauer-like state is clearly pathological and evolutionarily suboptimal in humans (how does one reproduce when one is in such bad shape?), but it could help explain a strange conundrum: how some people with ME/CFS get really, really sick without dying.
During a call Ron Davis mused on how ill people with ME/CFS can get without dying. In other diseases the kind of disability seen in the most severely ill ME/CFS patients is a prelude to death. Once people get THAT sick they’re usually going to die; a process has been started that’s going to result in death.
But that generally doesn’t happen in ME/CFS. People can remain functionally in what appears to be a near death state for a long time. That could suggest a way has been found to keep the body alive in a very low energy state. Naviaux believes the state may be protective against conditions like hypertension, dyslipidemia, central obesity, and insulin resistance.
There’s obviously many downsides to being a in low energy state. Naviaux stated that because it takes more energy to relax than to react, anxiety, tension and hypersensitivity are likely outcomes of being caught in a low energy state.
Diagnostic Test
Using just eight and thirteen metabolites in males and females, respectively, Naviaux was able to diagnose 95 and 96% percent of the male and female ME/CFS patients correctly. The metabolite signature in the ME/CFS patient relative to the healthy controls, was so different, in fact, that even using a single metabolite worked pretty well in identifying who was who.
If future studies can validate Naviaux’s findings, a biological diagnostic signature signaling that ME/CFS patient are in a hypometabolic state may have been found. Creating a true diagnostic signature will require comparing ME/CFS to other diseases, and those studies are underway.
Turning the Worm – Treatment
You can bring a mitochondria to oxygen but you can’t make them use it. Naviaux
Metabolomics reveals a new window into the underlying biology of CFS that makes us very hopeful that effective treatments will be developed soon and tested in well-controlled clinical trials. Naviaux
Naviaux doesn’t believe the answers are going to come from the usual treatments for damaged mitochondria. He spent the first part of his career studying people with genetically caused mitochondrial damage. People with ME/CFS, autism, and other diseases have mitochondrial problems, but they are completely different from people with genetically determined mitochondrial diseases. Their mitochondria are turned off, not broken. It’s a matter of getting them to turn back on.
Naviaux’s idea of ME/CFS patients being captured by some sort of aberrant evolutionary process seems reminiscent of Broderick’s idea of patients being caught in suboptimal state or a new normal. Given the embeddedness of this state, Broderick believes it will take considerable “force” (or better yet skill) to move ME/CFS patient back to health. Dr. Cheney – who floated the idea that people with ME/CFS were locked into a kind of protective state years ago – has talked of a similar push-pull phenomenon; he could push an ME/CFS patient towards health but it was as if their systems pulled them back again.
If Naviaux is right ME/CFS probably didn’t happen because of one breakdown; many changes needed to occur for this hypometabolic state to take over and it’s probably going to take careful, calibrated changes to entice the system back to normal.
Although all the metabolic abnormalities Naviaux found in ME/CFS could be a consequence of low NADPH availability, Naviaux cautioned

ME/CFS is just like a car that’s sat awhile – you can’t just turn the engine over and expect it to run well.
that simply adding NADPH wouldn’t work. Incremental improvements in NADPH production could theoretically be achieved by using treatments focused on folate, B12, glycine, and serine pools, and B6 metabolism but the clinical studies to show this have not been done.
He compared an ME/CFS patient to a car that’s sat for a long winter. You can’t just turn the car over and expect it to run well. You have to replenish the fluids and ready the car before starting the engine, otherwise you can damage it further. Treatment is not simply about replenishing the metabolites that are low. The low metabolites reflect a distortion of a network – they themselves are not the cause.
Antivirals, he and Ron Davis have cautioned, could do more than good when given to a person without a clear sign of infection. Antivirals and antibiotics, it turns out, can pound the mitochondria. (Statins, valproate, and metformin can do the same.)
Many antibiotics like tetracyclines, erythromycin, and the fluoroquinolones (eg, Cipro), and antivirals like acyclovir, fialuridine, AZT, and ddC also inhibit mitochondrial functions when used chronically (usually for more than about 3 weeks). Because mitochondria are descendants of free-living bacteria, their machinery for protein synthesis, RNA synthesis, and DNA replication are susceptible to many antibiotics, and for reasons unique to mitochondrial DNA synthesis, they are also sensitive to antivirals. Chronic use of these drugs can do more harm than good if there is no longer good evidence for an active infection. Naviaux
- Check out more about antivirals, treatment and other aspects of the paper in Naviaux’s ME/CFS Q & A here.
Ultimately, effective treatments will require approaching the system in an integrated fashion using nutrition, metabolism, uncovering triggers and stressors and understanding the role exercise plays. Understanding what happened to trigger the entry into a dauer-like state of low energy and how to get the system to exit that state will be critical.
Ron Davis envisions a core treatment regimen accompanied by more personalized treatments and suggests that Naviaux’s findings could explain why some treatments could work for some people but not for others. The different secondary pathways found in men and women suggests gender will effect treatment. Plus most of the metabolites (75%) altered in the ME/CFS patients were “personalized”; that is they were mostly unique to the individual, and these will help guide treatment regimens. Age matters as well. In fact, studies in which the participants are not age and gender matched will cause metabolomics results to wash out.
The proper treatment regimens for ME/CFS will clearly take some time – but perhaps not a lot of time – to be created. On the bright side Naviuax believes the evidence is there for all to see in the chemistry. It’s just a matter of figuring it out.
Rapidly Expanding Field
The good news is that the metabolomics field is rapidly developing. This study, Naviaux said, couldn’t have been done five years ago. In the next two years the capacity to efficiently study and uncover more metabolic compounds may double. The bad news is that the rapid growth in the field inherently brings some costs. Laboratories are developing new techniques that need to be standardized and cross-validated. Researchers need to know that study results done with X instrument will mean the same thing as studies done with Y instrument.
Naviaux’s next ME/CFS study will be fifty percent larger and include people from across the U.S. It will also include a metabolomics center at UC Davis in order to hurry the process of validation and standardization along.
Has the light bulb come on for ME/CFS? Has the underlying problem been identified? Naviaux believes he’s found a basis for methodically plumbing a disease in which treatments even by the experts are too often hit and miss. I heard a well-known ME/CFS doctor once blurt out in a burst of honesty “We’re just guessing most of the time”.
Naviaux’s path is not an easy one and it won’t be completed in a day. It requires understanding scads of complex biochemical reactions, for one thing, but Naviaux believes that our growing ability to eavesdrop on our cells physiology will open the door to understanding and treating hypometabolic states like ME/CFS.
Time will tell.
Conclusions
- A biochemical signature has been found, which if replicated, could provide the first diagnostic biomarker for the disease
- A core hypometabolic state appears to underly the heterogeneity we see in ME/CFS.
- The hypometabolic state ME/CFS patients find themselves in has become pathological. it may derive, though, from evolutionary process designed to allow an organism to hunker down and conserve resources during a pathogen attack or other situation.
- From a hypometabolic state in the brain, to the reduced immune activity in longer duration patients, to the reduced aerobic functioning, the low cortisol and parasympathetic nervous system functioning, and now to the metabolism, a state of low functioning appears to be characteristic of ME/CFS.
- The hypometabolic state in ME/CFS differs from the kind of cell danger response seen in inflammatory diseases and infection but is similar to that seen in autism and related diseases. The degree of reduction in the sphingolipid metabolites seen in ME/CFS, however, was extraordinary and may reflect a different way of preventing the spread of infection.
- Treatment is a complex process which involves first adjusting metabolic pathways to allow the cell to slip out of the danger response and resume normal functioning, and then using the signaling processes to tell the cell that “the danger has passed”. Doing so will require more than refilling the tank of depleted metabolites. While the process is complex, Naviaux believes the chemical signals he is finding will ultimately lead to clear treatment pathways.
________________________________
More on the Study and Metabolomics
- New! Maureen Hanson Validates Naviaux’s Core Finding
- Ron Davis’s statement on the study
- Dr. Naviaux’s Q & A for the Metabolomics paper
- Dr. Naviaux – An Eye on the Mitochondria Man and Chronic Fatigue Syndrome (ME/CFS)
- The Mitochondria Man Gets His Money and the U.K. Goes Mega






Thank you Cort, once again you have done a great job. It hopefully will point to treatments other than life style changes.
I can say with confidence that it will certainly do that.
I believe it was metabolomics that took Whitney back from the brink. At one point his tests got so bad that they worried he was on his way out. That’s no longer so. He’s of course, very ill but his test results have improved significantly and he’s not in danger anymore.
Great news Cort. Do you think that Whitney got better because after the metabolomic study they already know a bit what to target and which treatement to use?
My understanding is that Whitney’s metabolomics test gave them ideas about new ways to treat him. I don’t know about the study. Whitney’s results were so far off the charts that they didn’t use them in the study. The same hypometabolic state was present.
I believe the metabolomics tests have been done on the participants in the OMF’s severely ill study and the next step is analyzing it.
That means we have that, the Naviaux/Davis OMF funded study and Maureen Hanson’s small study to look forward to, plus Naviaux’s comparison study involving ME/CFS and other diseases.
I’m SO happy to hear about Whitney being back from the brink. Maybe all the prayers helped.
Thank you for this article, Cort!
Thank you Court Johnson I understood it! So a job well done. I’m so happy that Whitney is out of danger X and good to know treatment is a real possibility for all. Just to let you know there are a lot of mum’s with very sick children that read your work in UK and you have helped many stay out of trouble. I’ll pass this on with joy! Take care Tina UK
What has he done to make such improvements in his test results? I apologize, but I’m not familiar with his story.
I appreciate your description of the early contact between Ron Davis and Robert Naviaux. That must have been a wonderful, hallelujah moment for the Dafoes.
“How much easier it would be if one core problem underlay all the others.” Yes.
I finally came up with my own name for CFS. It helps home health aides understand why the way they’ve been taught to care for CFS patients (encourage them to do as much as possible) can be harmful. I now call it Progressive Exertion-Induced Muscle Weakness and Exertion-Induced General Loss of Function Disease. They get it!
“…it takes more energy to relax than to react…”
Did you mean to write that?
I appreciate your description of the early contact between Ron Davis and Robert Naviaux. That must have been a wonderful, hallelujah moment for the Dafoes.
Yes, I really perked up when I heard Naviaux say that because while I didn’t understand it it intuitively made sense to me – since relaxation and I really don’t go together. I checked with him to make sure it was right. A body in an energy depleted state is hypersensitive and unable to relax.
I believe it!
Naviaux has been studying people with genetic mitochondrial problems for years. He said that when they die they go into rigor mortis really quickly.
This has so been my experience and that of so many people I know with CFS. Almost impossible to relax except sometimes with meditation or after prolonged periods of bedrest. May also speak to the sleep issues in some way.
I’ve seen this fast rigor….my poor dad. This illness is in our family. He suffered so. No longer is he in pain.
Issie
i’m a patient of dr. cheney’s and he recently said during an echocardiogram, that the heart uses energy to relax and doesn’t take as much to contract. that’s why we really at the heart level have trouble relaxing! i’m also a participant in the latest navieaux study..just got my blood done this week.
Yes, that’s really interesting…I love how Naviaux just jumped on that latest study and got it rolling. That is one big advantage of getting OMF funding = you can just start!
More specifics on Cheney’s explanation about heart relaxation (I’m a patient of his, too): He said that in order for the diastolic side of the heart to relax, the cells have to pump calcium out (of the cells), which takes tremendous energy – more than we have, of course, to do fully. He likened the diastolic relaxation process to the energy required to roll a ball up a ramp; and then the seemingly high-energy systolic response of pumping the blood out is simply the ball rolling back down. In CFS, we aren’t able to pump as much of the Calcium out, so there’s less relaxing/opening of the heart and less blood fill. And then the systolic side compensates with a far stronger than normal squeeze = the high ejection fraction we all have, which also leads to the venous reflux we almost all show. That’s why we evidence pure diastolic dysfunction without the corresponding systolic dysfunction that cardiologists are familiar with.
I’m pretty sure that it takes more energy to relax (than contract) all muscles, not just the heart. Due to the same calcium pumping energy requirement. Definitely explains why my muscles always feel partly contracted, which I have been saying for years! Even if I actively relax them, they just seize up again as soon as I stop paying attention☺
The amazing aha moment occurred before Rin Davis met Naviaux. It occurred in March 2015 when we got the first metabalomics results back from Metabolon and saw hundreds of levels way, way off of normal. We wept wit joy. Years of normal tests while being so sick. Finally these tests showed how very sick he was! After that Ron met Bob because Whitney was a subject in his study. Bob’s tests also showed Whitney off the charts. It was a true meeting of minds! Since then we have gotten Whitney off the PICC line and are feeding him through tube into gut. We have given him many things he was low in. His blood tests are much, much better but his CFS has not improved. He is still unable to eat, talk, be touched, or even to have any eye contact or noise. We have to figure out how to tell his body to turn back on. I CANT WAIT!!!!
We’re with you and the family Janet and sure hope getting Whitney off the PICC line is just the beginning.
Best of luck to you Janet. Will be happy to read all about it when that day comes as Whitney so deserves it! Feel very grateful to have people like Ron working on this and hopefully in the future the unecessary suffering can be avoided.
It really was serendipity that they meet. The other metabolomics papers hale from Japan and Australia and there these two guys are linked together by Whitney…The more money Ron and Bob Naviaux the better chance Whitney and all of us have.
Flo I love your name for cfs/me – Exertion-Induced General Loss of Function Disease!! I think that’s the perfect name! It tells people exactly what happens to us. I wrote it down so I can start using it myself so people will understand why I can’t do things.
I think its clear that these findings – should they be reproduced in ME/CFS and shown to be diagnostic with respect to other diseases – open the door for a new name. There’s certainly evidence for a low state of functioning in a number of systems.
A new name – how about Hypometabolic Syndrome?
Hypometabolic Syndrome is the best I have heard so far. Maybe “syndrome” could even be replaced by another term which reflects definite physical abnormalities rather than just a clinical pattern. We do have a clinical pattern but it is also a form of illness. What I am aiming at is getting away from any words which refer to subjective experience and going with words which refer to proven physical characteristics.
The new center for research at Cornell which is going to be called “Ennervating Neuroimmune Illness” doesn’t work well as a title either. The word “ennervating” is unknown to the average person who understands “nervous” as in overstimulated, which is just the opposite of the meaning of ennervating.
I hope that Hypo is the beginning of any designation our condition gets.
HD – Hypometabolic Disease, would be better. People do not take the word “Syndrome” seriously. However, the question is if a name is designed to make the public understand, or to make doctors understand. I think “the Living Death Disease” helps the public to understand pretty well what this is like, and the severity. But a name that points out the primary process, or causation, is better for doctors – so depending on what they find, Metabolomic Dysfunction Disease, or whatever specific pathways or DNA markers or whatever it is that they find to be consistently messed up. Very encouraging to read about the Hanson study that backed all this up, but via a different method.
After all these years stuck with Chronic Fatigue Syndrome which sounds like “Nothing” or “Neurotic Malingering”, I wish our condition had a medical name without “syndrome” or “dysfunction”. Hypo-Metabolic Disease might be ok. But as more is scientifically established, something even more appropriate may turn up.
I don’t know how they came up with enervating…it is easily misunderstood and the title of the Center is something that only a researcher could come up with; that said – it’s great to see her open a center:)
Maybe Chalder and White can tell the cell that there is no danger anymore 🙂
hahhha – good one, Gijs 🙂
maybe they can make a video to watch over and over again where they show the cells to relax and to take more and more energy oxygen now that the danger is gone. sounds funny but it is the base of hypno therarpy/ constellation work.
Another name for the disease- The living death disease
I think the same.Honestly, I really panicked the first years when I had an ,,attack,,: muscels getting more acid in the following 72 hours after exercise in the rehabilitationcenter untill the point I am not able to move them anymore. Then a like electricity hot current starts moving around the body which is very painful, especially in the heartarea. Heart beating much too fast for a longtime.Even when laying down.It takes away all your energy. Then you can t move anymore but you still realize what happens. Scary and very painful.
Rigor mortis in vivo…at that moment I say to myself now: keep calm, you survived the other attacks…but it is not easy.
Thank you for doing the research and good luck!!
I wonder if anyone can help me understand this a little more: ” The metabolic response in ME/CFS doesn’t look the responses seen in inflammation, infection or metabolic syndrome”… I was under the impression that several of us also have inflammation or inflammatory conditions as well as ME. How does this fit together?
That’s a great question and I don’t know the answer. Naviaux seems to be saying that there’s this metabolic response we see in infections and in inflammatory diseases and we’re not seeing that in ME/CFS (or autism, depression and some other disorders.)
The cytokine studies have been up and down and all over the place but in general it’s been assumed that ME/CFS is an inflammatory condition.
I think it may perhaps be possible for cytokine levels to be down overall but for anti-inflammatory cytokines levels to be down more than pro–inflammatory cytokines and perhaps that leads to an inflammatory state ? (Maybe?).
The immune system is really complex. I certainly don’t have a handle on what’s going on.
I wonder if it is because most people think of illness as involving more inflammation, fevers, that sort of thing, combined with our knowledge that we are sick?
It could also be, as Hornig discovered, that the immune signatures changed with long term ME/CFS. Initially those studied–and weren’t they folks who started with a bad infection?–showed more immune arousal/higher levels of certain elements, but then past the 3 yr mark, those levels went way down to more of a hypo state.
In my case I relate to this because I had lots of infections in my early years with this “condition”, but then I stopped getting those infections to the point where I have fewer than most people. Yet do I ever have a hypo state–
Ron Davis talked about the fact that Whitney and others hardly ever experience colds. Naviaux – as illustrated by Jaime in her blog – does believe that the low sphingolipids he found could reflect a system trying to ward off pathogens in a different way.
I don’t really know anything about sphingolipids, so I was reading and came across this study which says, “scientists have recently demonstrated that inhibiting enzymes controlling sphingolipid synthesis has beneficial effects in rodent models of atherosclerosis, insulin resistance, diabetes, and cardiomyopathy.
Doesn’t it seem odd that so many of us have those exact problems with our ME/CFS? Increasing sphingolipids would only seem to make them worse. I know that they have not made any treatment suggestions yet though.
Thanks Remy. That follows what Naviaux suggested – that this this hypometabolic state does have its advantages. Cheney was the first to show diastolic problems in ME/CFS (and he suggested years ago that ME/CFS was in some sense protective). Usually diastolic problems end up with cardiomyopathy- and a very nasty result – but they don’t with ME/CFS. Maybe this is why (??)
They acknowledged that Cheney read and commented on the study and the followup study is, I believe, using some of his patients.
Interesting about Whitney’s colds. I recently got much better after over 20 years of ME/CFS and after about 8 years with no colds, I had 2 in the first 8 weeks.
Marilyn, I have to ask…did you do anything that you think made you get better? I know everyone else will want to know too. So glad you are better!!!! 🙂
Marilyn, after 20 years you just recently got much better with CFS? what did you do differently?
http://phoenixrising.me/archives/24936
This is a bit of an oldie, but I think very relevant to the above statements. It would make a certain amount of sense that brain inflammation , due to viral or other triggers, could send some sort of cascade that induces dauer type reactions in cellular pathology.
Do you know if the findings of the study discussed in the Phoenix Rising article were ever replicated?
Well one other option may be cfs/me are comorbid often with inflamatory autoimmunes, etc… It could be a secondary process ie..
Cfs with inflamation response or without. Or it could be an aditional layer… I has autoimmune disease before I had CFS and came to this community later than a/i communities. Over in a/i most of us are falling apart from the combined massive number of diagnoses we receive, and some cfs/mers are similar in that reguard.
The metabolic response not resembling inflammation only means there is no abnormal inflammation. Inflammatory conditions can still be caused by inflammation sensitivity without an abnormal inflammation. And whatever is causing the sensitivity could be causing the metabolic response opposite to the response to inflammation.
Cort, thank you so much for writing this article, bringing us this great news! I have thought of my case of ME/CFS as a hypo state for a long time. Everything is low, yet I continue.
“It takes more energy to relax than react” is such an interesting idea. It seems paradoxical yet I could recognize this in the way I have less pain, both in terms of oversensitivity as well as muscle contraction, when I am more rested and balanced than when overtired. Also this explains the dysfunctional loop that happens with poor sleep causing more contraction and sensitivity which causes more wakefulness, etc.
I would like to hear more about your observation that it takes more energy to relax than to react.
Thanks again!
I don’t know how it works physiologically but it certainly makes sense empirically. I walked too far with the dogs today. (I should never walk in the morning) and here I am – depleted with my muscles – not worn out and limp but in a seeming state of contraction! They feel unflexible, hot and angry!
If I keep this up I’ll have trouble sleeping – really relaxing.
I do remember Dr. Cheney’s statement that it takes a lot of energy to relax the heart muscle so that it expand and take in more blood.
I have heard that the default state for the autonomic nervous system is to be “on” – for the sympathetic nervous system to be engaged. That’s so that important fight/flight system can be ready to go at a second’s notice.
Turning it off requires the parasympathetic nervous system to jump in and inhibit it. In that case it sounds like it indeed takes more energy to relax – to enter into the rest and diges t response…
I would love to learn more about this.
I had found with mysef, having HyperPOTS, which causes extreme sympathetic respone and high NE with standing—treating that response was the wrong thing for me. It made me more sick when I suppressed that response with meds. I found most all meds traditionally used for POTS to not be helpful for me. Having tachycardia is very uncomfortable and at times very scarey, but it helps to get more blood and oxygen to my heart and head.
Also having Lyme and Protomyzoa Rehumatica and plenty of biofilm caused by them —I’ve often thought which is better. Breaking down the biofilm that houses them to cause an immune system attack (if the immune system will even recognize them – Apparently, they can take on some of our own DNA to evade recognition.) Or considering it as a protection in a sense to what’s outside of that. Most Lyme docs are now saying the herx we get is from a release of to many cytokines. Our body not being able to process that much at once causing an inflammatory response.
If we could get our bodies to live in symbiosis with the pathogens and keep in a certain amount of balance…..we would be as those who are carriers of things with no or little illness. My doc said he has patients that are this way. We need to be able to coexist.
I found it interesting the comment that some meds may in fact do more harm than good. We don’t want to suppress a function/symptom if it is a compensatory response and actually may be saving us from a worse evil.
Great, understandable write up Cort!
Issie
I have a few thoughts. One is that although Howard Bloom’s protocol wouldn’t be appropriate for most, These researchers should have a serious talk w him. He went from bedridden CFS where he couldn’t have someone turn newspaper pages in the apt and where, he joked, even the suspense of a comic Golden Girls episode was too stressful and could initiate a relapse. His protocol quenched and drenched the singed hyper reactive cns w stuff like Valium oxytocin and possibly neurontin, I can’t recall . He completely recovered.
Just giving nutrients without inducing rest may not “wake” one out of a hibernation in which no real rest or relaxation was achieved.
I wonder how ketamine would work. It has been life saving to those with refractory severe depression. It induces blissful relaxation. I would like to see it studied in moderately severe, not truly severe patients. Depression also looks like hypo metabolism in some ways.
I try to explain to my partner that if he interrupts me or makes noise when I get the feeling I must nap or sleep, I lose the window and then my body gets hyper and I sleep poorly later on. There are times when I’ve had too much stimulation for a few days and I just decide to take the day and entirely rest (best done in a forest camping away from the madding crowds). Eventually I truly relax and drift off to sleep and regain my sleep cycle. This was never the case before tick bites; I was a great and easy sleeper.
Dr Veech has mentioned this a number of times in his reasearch on the Krebs cycle and ketosis. I’ll try to find the link to the podcast.
Makes sence Hypometabolit, goes with the Hypopituitism that followed my illness, unless I wrong about the low lipids which would also be my low vitamin D, A, cholesterol-and low good cholesterol low potassium, hypoglycemia ,low Igf1, and igfb3, which lead to low Hgh .Which mine is now 37 at age 55 female, it seems that it could still lead to death in some of us unless treatment is found and administrated.
I will watch and see, though It does sound just like my illness. Stress mentally, Infection started MRSA, multiple months of Antibotics, do we sit and wait watching on sidelines as we have been doing? Or is there something we can try? Even minor to start fixing the automobile? As it’s usually takes interconnected steps to complete.
Well-written. Good job.
I disagree with the basic thesis (dauer). I do think there’s dauer, but it’s because there is ongoing danger ie chronic infection (think Ebola, HIV, lyme as reasonable models. Or undertreated TB). Nonetheless, there are many aspects of his understanding that are deep and interesting (still–I think he’s missing the elephant in the room. A huge # of people are sick–why would so many people worldwide be in this ‘dauer’ state, maladapted to a hit and run commonplace initiating trigger?)
Well something is going on to keep those cells in whatever state they are in. I hearken back to Nancy Klimas’s realization that something in the blood is causing the natural killer cells to turn themselves off. I believe that both Klimas and Ron Davis are looking at this. It sounds very similar to Naviaux’s idea that some signal – I guess in the blood – has caused ME/cFS patients cells to hunker down and turn their mitochondria off. What it is is, of course, the big question.
Either the cells are not responding to the dismissal of the signal or the signal is still there. I hope it’s still there as I think it will be easier to fix that.
Since some people do respond well to antivirals I assume that an ongoing chronic infection is the problem for them – unless the antivirals are doing something different.
I was reading up that some antivirals can actually supress microglia as well as potentially be active against viral agents. I also have great appreciation for this study, but also many questions as well. Especially in light of things like this:http://phoenixrising.me/archives/24936 I could understand a organ specefic hypometabolism, but, unless I missed something, how could microglial cells be so activated? Unless for some patients, this is not the case whatsoever. Again, I might indeed be wrong…
It was just reported in the Health Rising’s Forums that in her Solve ME/CFS Initiative webinar Maureen Hanson said that in small study that she’s validated some of the Naviaux’s results…(!)
https://www.healthrising.org/forums/threads/solve-me-cfs-webinar-with-maureen-hanson-sept-1.4788/
Cort- fantastic job on pulling together the whole story and communicating the relevant detail to ME’rs. Most of the reports I’ve read have been low on detail or, the original study document, too much! As always, your own knowledge base in the field and the players gives a story with depth.
Thanks!
Thank you, Cort!!
If you are able consider a donation to prof. Davis/ Naviaux team and ask also your friends and family. We need to speed up this research and the only way is the patients donations. The sooner we get more money for them the sooner we can see a treatement. It´s pity to lose every single day.
You can donate here to the Open medicine foundation which support financialy this project. Thanks
http://www.openmedicinefoundation.org/donate-to-the-end-mecfs-project/
I would note that both Naviaux’s ME/CFS study and all of Ron Davis’s work at the Open Medicine Foundation and his own Foundation are all supported entirely by private donations! No NIH grants yet.
I believe that the amygdala retraining people have answers to the body being in a continual sympathetic state. Perhaps many of us had pathogens but even though they may have gone our brains have stayed switched on to the “cell danger mode”. I am trying the Gupta program because this makes perfect sense to my story.
Good luck with it Jo.
I have lesrned how to relax my body with guided meditation. Also the soften and flow technique. The programming part seemed not to work welk for me. Made me more anxious. Found it illogical.
Hiwever after 8 years of just meditation I Improved significantly. I can relax at will now by doing taking 20 min to meditate. Doing guided meditation was key.
I used to poo poo Gupta training stuff, but now, in light of success stories with other neural modulating type therapies, I can see how it could have good effect in training the body for a calming type state. I wonder what effect Gupta could have on Microglia?
PMCID: PMC4892433
NADPH oxidases as electrochemical generators to produce ion fluxes and turgor in fungi, plants and humans
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4892433/
My doctor just prescribed Statins for me and my “gut” keeps telling me not to take them. It is worrying me to death. I see where it was said that they beat up the Mitochondria. Not sure what to do. I think I made my doctor angry when I tried to talk her out of it. Can anyone help me with this? What should we do?
I really don’t know. Is your doctor urgently requesting that you take them or are they considered that something that would be helpful but that you could put off for a time?
She is urgently telling me. My cholesterol and lipids are high but I am terrified of the Statins and what they may do to my CFS. I am already so weak. Anyway, thank you so much for telling us what is going on in terms that all can understand. I tried to read the original article but could not understand any of it. You are a wonderful writer! I am trying to eat differently to lower my numbers but am afraid it may not work anyway. I think my high cholesterol is somehow linked to this illness and not being able to exercise enough. If that makes any sense?
I used to be very active as I think we all were.
Glory, i can tell you that Dr. Cheney is against statins esp for CFS patients.
I do feel like it is a bad thing for us but I don’t know why. Glad to hear that a doctor of CFS agrees. I just think it may cause more imbalance in an already imbalanced body. Thank you so much for telling me this.
Don’t want to give Gloria bad advice by mistake – but counter-intuitively, many people (including me) who go on a low-carb, ketogenic diet, end up with their cholesterol levels falling even though they are living on fat. Quite possibly it is BECAUSE they are “living on fat”, the body is burning fat for energy instead of sugar. I suspect that some of us have a metabolism that refuses to burn fat for energy at all, as long as there is sugar coming into the system. As soon as the sugar is depleted, we get cravings for more. The first 3 days of going off sugar – and that means “carbs”, period, involve quite intense withdrawal symptoms. Then a new balance seems to be found.
Other than the cholesterol levels falling (mine are already low (lol)) how did the diet do for you? I’m in the middle of the adjustment period.
My overall cholesterol was lower but especially the triglycerids were high. then I was on ketogenic diet and I got my overall cholesterol little bit higher over the norm but my triglycerides were perfect. But after 4 months without any problem on ketogenic diet I started to feel strang (I think hypoglycemic) and I had to stop it. Now I try to reduce carbohydrates but not in a drastic way – so it´s even not paleo now. I think it´s worth to try to reduce carbohydrates – i felt also more energy after doing it. It will influence also your lipid profile.Maybe it´s better to start not drastically and after a 3 months periode you always check your results
Thanks Tuha, that sounds good to me. I have really bad gut problems so sometimes I just have to eat whatever I have on hand quickly because I lose so much nourishment suddenly. Another thing to work out I guess.
Besides the reduced cholesterol, going ketogenic really got excess weight off (no other diet does this for me), and I also believe it led to improvement in fibromyalgia. My hypothesis is that burning sugar for energy produces muscle waste by-products that are more toxic than those from burning fat.
I don’t know if everyone with FM also has my extreme metabolic reaction to carbs: I say my body refuses to burn fat for energy, it uses up the available carbs and then crashes. In fact I got carb cravings constantly, even when so full of food that I had indigestion.
I believe going ketogenic in diet, after 3 days of withdrawal symptoms, my body finally switches over to burning fat for energy, including stored fat.
There is a hazard from this if you are carrying a lot of excess fat as I was: fat is apparently a favourite place for the body to store toxins, and when you lose the fat, the toxins have to go somewhere. The renal system will be under strain, and all sorts of symptom flare-ups can happen. In hindsight I would have lost weight more slowly. Hair tissue mineral analysis was extremely important to guide me about what imbalances were happening as the great flush-out was occurring. I needed to increase my magnesium dose repeatedly to keep cramp attacks at bay. Magnesium “oil” applied externally to the calf muscles, was a godsend.
Philip, I have the same problem with burning fat – as soon as my carb stores start to drop I get more fatigued, slow-witted, persistently low body temp. When I went on a low-carb (not no-carb) diet it took over a month before fat-burning started, then it seemed to be done through adrenaline: tingling hands, reduced sleep, high blood pressure, desperately hungry ALL THE TIME. But I did have more brain. I don’t know which is worse.
That’s a tough one LondonPots…I’ve found that I have to have lots of fat and a good amount of protein on these diets
Email this question to Bob Naviaux and ask him to add it to his Q and A. He is adding to that gradually. Make it a generic question if you can.
Thank you, I will try to do that. If I just had a professional to back this up it would be helpful.
Do you have Bob Naviaux’s email address or know where I could find it?
Google him at UCSD
naviaux@ucsd.edu
Sometimes cutting sugars and grains out of the diet will lower chlosterol levels. May be worth trying.
Thank you Issie. Certainly worth a try!
I missed the tv programme on UK last night,but I think they saw a fall in cholesterol by drinking apple cider vinegar….a tablespoon in water once a dayI use a glass straw to protect my teeth…..just a thougth
Quality fats can have the reverse effect of conventional fats. That is, butter from 100% grass-fed cows lowers cholesterol and improves cytokine profiles, whereas butter from conventionally raised cows increases cholesterol and can increase inflammation. The bovine species is actually allergic to the corn it gets fed; that allergy creates an inflammatory response throughout the animal’s tissues, (as with us), which leaves the animal’s products in this inflammatory-friendly state. FWIW, Kerrygold Irish butter is 100% grassfed and not much costlier than the regular kinds. I find that about half a tablespoon does me as much good as a pain pill, and I have Complex Regional Pain Syndrome, FM, dysautonomia, and other fun stuff.
Likewise for rooting pigs, scratching chickens, and wild game. Animals that are raised on whatever their species was actually made to eat, yield much healthier food for us. Who’d have thought!
The remark on relaxation being harder makes sense, both at the ionic level (calcium slope) and the central nervous system level. The organism must be safe before relaxing, or the CNS can’t let it happen. When we’re deeply ill, it is hard to feel safe.
Gloria, just to say that statins gave me a severe three-month relapse, although I stopped them within days. The strange ‘gasping’ sensation they caused in my muscles immediately prior to the relapse was identical to the ‘over-done-it-relapse-imminent’ sensation that exercise triggers. My cholesterol is very high, but I certainly won’t take statins again.
Try tocotrienols, but get all 8 vitamin E isomers as well. There’s a nice literature all pert reviewed, university driven, on tocotrienols and how they impact the mevalonate pathway but in a much more benevolent fashion. Also, you can visualize arterial plaque deposits w sonography and if you don’t have dangerous and thick plaque your high cholesterol is no big deal. If you do have arterial blockage at least you’ll know.
Well, statins and LDL are proven by the evidence. Statins and CFS, on the other hand, is mostly a “gut feeling” for now. Why not try it and see if it makes your CFS worse? You could always stop it if makes you feel worse. Unless you are worried the damage could be permanent, that is. The danger of high cholesterol is real though.
Aren’t the overall very low density lipid (VDL) numbers the important one concerning the connection to heart attack and death? Isn’t there a theory that statins reduce those through an anti-inflammatory mechanism rather than by reducing fats in our system? I don’t know enough, but it seems like we need to take more into account than just the lipid numbers before taking statins. On the other hand, I think I recall that statins tend to have few negative side effects for the normal healthy population, so it seems easy for a doctor to recommend them. They just might not be appropriate for some CFS sufferers. It might be worth trying for a short run, since we’re still largely stuck with good ol’ trial and error.
I flat out stopped taking statins because I was worried about lowering my steroid hormone and cortisol production. (Cortisol is in there, right?). I’m pretty sure my triglyceride numbers all improved when I went on low carb diets (anti-Candida and autoimmune paleo diets) and maybe in part because i lost weight on those diets. So stopping them worked out for me, but everyone’s different.
You are correct. Doctors that prescribe statins simply to lower cholesterol are practicing outdated medicine. I would stay away from them if I were you. Our bodies need cholesterol, and ME patients need all the nutrients they can get….
Gloria,
I tried statins and reacted very badly. Then i tried the natural alternative (red yeast Rice) and reacted badly to that too.
It seems statins deplete Q10.
I’m not taking them ever again.
Red yeast rice was prescribed by a naturopath dr. I kept telling her of the severe pain and she insisted that bc it was natural it could not be that. I persevered on it for 3 mos. Till I could not bear the pain and was told by a naturopath in training to stop taking it and I did and felt the results for better the very next day
I’ve slowly become intensely sensitive to carbs. After 2 years of no carbs on the GAPS (gut and psychology syndrome) I changed last March to a zero carb way of eating because I was starting to have problems even with green veggies etc. ZC is meat only. Sounds crazy but there are folks who have been on this for 8, 10, and 50 years and for whom it has made a huge difference in weight as well as health. I haven’t had cholesterol problems but my HDL still increased from 96 to 119 (this is the protective type of cholesterol molecule) and most folks on ZC I’ve been reading (there are a couple Facebook groups you can join) have had great success and support with this way of eating. As have a few with CFS and CFS-type symptoms. It took me a few months to stop truly craving carbs (and if I could eat them now without penalty I still would).
I had scary high cholesterol numbers, & couldn’t tolerate statins, which also scare me. My endocrinologist suggested a low dose statin once a WEEK. Pain increased (but not dibilitating) after about 2 months, But my numbers are as good as on daily statins, so this works for me. I skip or stretch out an occasional dose as needed.
MaryL,
That sounds like a good plan to me. Trying to change my diet but have a bad feeling that won’t work too well. I am sure if I do take them I will try your way first. Thanks so much for your reply.
Just so sick already without adding a new drug to the mix…
Gloria, could you take phytosterols instead of the statins?
They are sold in the cholesterol-lowering section of health food stores.
I know supplements don’t work on everyone, but it might be worth a try.
Thank you, I will look for them as soon as I can. I also have trouble now swallowing pills. Seems like if it’s not one thing it’s another!
when I experience swallowing issues, usually due to thyroid/cortisol inbalance (can either be too much or too little)
Don’t do the statins – diet will work. Look into a Paleo, alkaline, or SCD diet. Your cholesterol will come down and this illness is not the cause of it. Also, look into finding a doctor of integrative medicine to help guide you.
Saw a TED talk where the doctor said every drug has a “NNT”ie number needed to treat…..so for statins its 300 treated for 1person to benefit!…..every drug has an NNT number which your doctor should tell you if you ask….so I don’t think that’s good odds coupled with the fact that 50%of those on statins suffer side effects…
Gloria, About 18 years ago I was where you are now–feeling the same fears & receiving intense pressure from cardiologist that I saw for presurgical clearance. In fact, he did a heart cath that really should never have been done. It was virtually negative. Preliminary Treadmill nearly killed me and only showed a slight murmur-like occurrence that he couldn’t explain (though my gyn doc had heard it for years :-)).
Next he insisted I take a fairly large dose of Crestor for high cholesterol and refused any discussion about the fact that a trial of low dose Lipitor made me violently ill and weak. I took 1/4 of his prescribed dose, 2 or 3 times a week–not every day. In 4 weeks my reading was normal w/high HDL’s. But I had read so many accounts of statins causing muscle break down, weakness & other problems that NOT taking them anymore was my final decision.
After researching the many health benefits of cholesterol in the human body, I decided to be as active as CFS/FM would allow, and continue healthy eating (except for the occasional necessary ice cream binges)and go forward on the assumption that my body was making extra cholesterol because it was needed.
BTW, I discovered the cardiologist was doing trials for the pharma that produced Crestor, hence he would never entertain alternative methods. My suggestion would be to breathe, do your research, pray or meditate and Always follow your intuition!
Lynn-Z,
Thank you so much for your detailed response. That is exactly the way I feel about it all. I also was against taking anti-depressants 10 years ago that they really pushed on me. I did not take them and now am so glad I did not. It is just so hard to go against a doctor’s advice. Sounds like you have done o.k. since it has been 18 years. I do just feel like my body is trying so hard to protect itself from the CFS in ways I don’t understand but I know those Statins are going to make me sicker. I may regret it perhaps but somehow I don’t think so. It really helped me to hear this and I thank you so very much for taking time to share your story with me.
Ha! Love “…except for the occasional necessary ice cream binges.”
Great reporting, Cort, thank you! Encouraging!
I’ve just managed to reduce my cholesterol in 3 months from 8.5 down to 5.3 (British cholesterol figures) by a strict regime of 1 teaspoon of chia, sunflower, pumpkin and sesame seeds. 2 teaspoons of oat brain, 1 teaspoon oats, 2 teaspoons flaxseeds, with baked apple usually about 1 Apple, soya Alpro yoghurt x 3 dessert spoons for breakfast. 3 teaspoons physllium husks in water morning and afternoon. For supper / late afternoon a small bowl of a mixture of beans (butter, pinto, kidney etc), broccoli, cauliflower etc. and a mix of grains such as quinoa, red rice. Usually then another soya yoghurt. Handfuls of blueberries as mini snacks. This has also helped reduce my weight and obviously this is a high fibre eating regime that helps good cholesterol and drags out the bad cholesterol. I’ve done this as determined not to be put on statins. I love the food as well which helps. Sally
Thank you, thank you, thank you Cort for the info you pass along so continuously and in a way I can comprehend. I have to admit I’ve had tears reading this. Two things really jumped out at me. “Easier to react than relax” and as someone called it “the living death disease”. These among other things cited so describe my experience that it does give me some hope that we are on a more positive road. I certainly pray this is so.
The good news is that we can expect to have at least three more metabolomics done this year; the Davis/Open Medicine Foundation severely ill study, the Naviaux/Open Medicine Foundation funded expanded, follow up study and the Hanson metabolomics study. The Solve ME/CFS Foundation is also working on a mitochondrial study – the basis of which I don’t remember and the Center for Infection and Immunity under Maureen Hanson and Ian Lipkin is looking at metabolomics in connection with their gut studies.
So metabolomics really seems to be a growth field! We should know a lot more about how effective it will be in answering questions about ME/CFS pretty soon….
(Unfortunately there are no talks that I am aware of on metabolomics at the IACFS/ME conference.)
“Easier to react than relax” – it is not exactly “easier” in terms of the damage to the body, it is “easier” for the “control mechanism” in the first place.
It is like a throttle pedal that relies on a return spring to keep it “off”; when the return spring is broken, it is “easier” for the throttle pedal to fall into “wide open” position, but it is not easier for the engine!
I am not sure if it will be about metabolomics but they added prof. Davis to the IACF/ME conference
2. Mitochondrial Dysfunction: A Potential Etiology for ME/CFS?
Moderator: Jon D. Kaiser, MD, University of California Medical School, San Francisco
Speaker Panel: Ron Davis, MD, Stanford University Medical School
Nancy Klimas, MD, Neuro Immune Institute, NOVA Southeastern
Dikoma Shungu, PhD, Departments of Radiology, Neurology
and Neuroscience, Weill Cornell Medicine
Mitochondrial dysfunction is an etiologic mechanism that may explain the multisystem range of symptoms experienced by CFS patients. Electron micrographs of muscle biopsies have revealed abnormal mitochondrial degeneration. Evidence of oxidative damage and increased activity of antioxidant enzymes have also been chemically detected in muscle specimens of CFS patients. The classic presentation for an illness manifesting mitochondrial dysfunction is one that involves multiple symptoms spanning many domains. These typically include fatigue, cognitive impairment and other brain-related challenges, muscle weakness, exercise intolerance, and gastrointestinal problems. The broad symptoms profile found in ME/CFS is consistent with this description of a mitochondrial dysfunction disease.
Great job on reporting this for us! Thank you, Cort. After the article about Canadian health , this was so welcomed.
Indeed! It made me forget that weirdness happening in Canada… (https://www.healthrising.org/forums/threads/the-dark-north-canada-denies-me-cfs-grant-because-disease-is-not-real.4819/#post-23547). Hopefully, we and Davis and Naviaux and the other researchers will get the funding we need and stuff like that will be a thing of the past in not too distant future.
Hi Cort, thank you for the great write-up. After suffering with CFS for over a decade I am so hopeful that our neglected community will soon get the assistance it so desperately needs. Speaking of which, do you have any idea when NIH could announce whether they’ll allocate solid funding to CFS research? Like, does it announce a yearly budget or anything?
Also, I found it interesting that both Naviaux and Davis have expressed concern about anti-virals and antibiotics possibly causing harm to CFS patients’ mitochondria when used chronically. In Naviaux’s ME/CFS Q&A, he states: “Many antibiotics like tetracyclines, erythromycin, and the fluoroquinolones (eg, Cipro), and antivirals like acyclovir, fialuridine, AZT, and ddC also inhibit mitochondrial functions when used chronically.” I noticed he didn’t mention Valtrex, which is frequently used to treat CFS patients with high EBV titres. Do you happen to know if he intentionally omitted Valtrex, perhaps because it’s safer than acyclovir, etc.?
I don’t know. Check out his further explanation on the link provided. It seems as if antivirals in general have this issue but I don’t know about specific ones.
Check out this blog – The NIH’s Big Change: Is it Coming For Chronic Fatigue Syndrome (ME/CFS)? for more on the NIH situation. The announcement for the RFA is months overdue but unfortunately they still can’t give a general idea when the funding package will be approved. That’s not really a great sign! The longer it lingers the more chance it has of being whittled down I would think. We shall see!
Participating in this action – http://www.meaction.net/2016/08/25/urgent-take-part-in-the-us-congressional-call-to-action/ – will help keep the pressure on.
Gary Moller (naturopath) swears by Artemisia Annua as a natural anti-infection medication – but I wonder now, does it help or hinder the mitochondria?
I used Arteminsin SOD along with low dose Doxycycoline for about 3 years for my protozoa. It made a huge difference for me. At same time went Vegan. Since I also have MCAS, used GastroCrom (helps immune system at gut level and is a mild calcium channel blocker). Those things seemed to pull me out of the horrible place I was. Then I got a prolonged exposure to mold and severe stress (parent care and both died), it was like every advancement I had made was back to square one. I’m in a bad flare and having a time with detox.
The antibiotics and Artemisinin no longer working. I think that long of use disrupted my gut flora and now having issues with getting the balance. Lots of inflammation. But I do feel they helped give me more life for awhile.
Issie
How can I be included in the next metabolite study? I’ve collected data – lab results, wt, what has/has not worked, qualitative & quantitative data since 1993 when I got mono and never returned to normal. I currently have hi EBV counts.
I’ve always felt that no matter what I do to get well, my body was down regulating. PLEASE HELP. I have extensive, comprehensive data in electronic form that is easily searchable and would be a researcher’s treasure trove.
Just stayed tuned. Something is coming up. 🙂
Thanks so much for writing this article. If a reliable biomarker can be determined, it would finallyy and unequivocally validate to the entire medical community what we patients have known for years.
Hey Cort!
I asked a doctor to give me an organic acid urine test a few months ago. It came back with a bunch of irregularities. The doc wasn’t much help explaining it. I read that organic acid tests have to do with metabolism. Any idea if my funky test could be related to my CFS? Based on these new findings?
I would certainly think so but I am such an amateur at this. Other people would probably know better. Naviaux, though, is testing many more compounds so while I would guess its related he’s taking a much more comprehensive approach.
Hi, Sipora. I’m not a regular on the Phoenix Rising forums, but so many people there have so much knowledge and have had those types of tests done that I bet they can answer lots of questions if you’re willing to post your results to them. I had the Great Plains Labs OATS test done recently and it has tons of fascinating results and some explanations to look through. Luckily, after two decades of this, I finally found a doctor here in Virginia Beach (Dr Charles Parker) who knows this stuff and he’s just five minutes up the road. Right here the whole time. Crazy. He also had me get the DHA Labs Walsh Protocol tests done to check methylation status, copper & zinc levels, and pyroluria makers. I’m only about a month into my treatment so the jury is still out on that one. Walsh info is on Dr Parker’s website here: http://www.corepsych.com/walsh-resources/
I listened to a webinar by a Dr. David Brady and that’s when I first heard of the organic acid test – he said he couldn’t practice without it. He’s in Fairfield CT if anyone is close.
Thank you, Cort! I’ve had this disease for 29+ years and have often given up hope that they’ll find anything during my lifetime. This is indeed a glimmer of hope. I’ve always felt like this is the ‘slowest’ death, one cell at a time. If this is true, I wasn’t off by too much, but instead of dying, the cells go into a deep ‘sleep’. May be Dr Naviaux will be the young prince to wake us up?! However, I disagree with the ‘Dauer’/Hibernation theory, since I don’t believe people developed from single cell organisms or worms or even monkeys. Monkeys don’t hibernate and evolution is an unproven scientific lie. Aside from that, I pray they’ll come up with biomarkers and some answers fast.
Just wanted to add that I’m going to look into Metabolomics. They sure didn’t have them, when I went to medical school. I don’t remember much of my four years in med school, because of my memory problems, but I can generally figure things out. So I want to offer my help, if you ever need it. Thank you, Cort!
Great blog, Cort.
Let us hope …
Threads like this always make me, a Fibromyalgia patient, wonder “how relevant is this to FM, or is there a crucial difference”?
I have come to strongly believe that FM “is” a problem with the myofascia ground substance losing its lubricant properties and hence muscle strands adjacent to each other end up sticking, and ripples and knots form in muscle tissue. Inability to clear post-exertion muscle waste products as fast as normal people; vaso-constriction; dehydration, fluid and electrolyte dysfunction; all also feature. But in what order these occur as the condition “starts to set in”, what was first, and what was “the cause” – I have no idea.
Infections and toxins seem to have been part of the mix with everyone, but did these cause dehydration as the body tried to flush them out, or was the vaso-constriction a kind of auto-immune response; or what? Whatever started it, it does seem to become a vicious circle from there.
I wonder if FM needs its own Metabolomics study. It is possible that FM is a completely different condition, if my hypothesis is correct – FM has the tension and pain foremost, rather than the tiredness, which logically could be a consequence of the muscular and cardio-vascular malfunctions. As long as most people with CFS do not have the myofascia-related trigger points and knots and ripples in the muscles, then I would say they are different conditions.
But some people could have both FM and CFS. Metabolomics could resolve whether they are totally different conditions, or the same thing with different symptoms coming out in different magnitudes.
Hornig said that 40% of the ME/CFS patients in their study have FM also. Dr. Bateman thinks they’re both on the same spectrum. I’ve been diagnosed with both and with my pain levels I’ve got to think that I’m a fibro’ey ME/CFS patient. I definitely think FM deserves a metabolomics study and, if this work goes far enough for it produce something that might be a diagnostic biomarker, they will have to compare people with FM and ME/CFS. So hopefully you’ll get your FM metabolomics study.
Yes, but I wonder whether pain levels in CFS are related to CFS-specific malfunctioning, while FM pain is related to its own unique malfunctioning, that of myofascial dis-lubrication?
I would argue that CFS quite logically leaves people in pain as well as fatigued, but if they don’t have stuck, knotty, corrugated, “tearing sensation” myofascia, then they don’t have FM.
Maybe we need some new labels, because “FM” has come to mean no more than “certain touchy spots on the body”. When these can be caused by both muscle tissue hypermobility (Ehlers Danlos Syndrome) AND by the far more common myofascial tightness, then a diagnosis of “FM” is useless as a guide to actual treatment. It almost seems the medical profession would rather be lazy and stick a whole bunch of sufferers into a “too hard” pigeon-hole, rather than diagnose an actual underlying problem in each case.
I think the myofascial dysfunction is so much by far the most common underlying problem in people specifically diagnosed with “FM” and not something else that should be obvious, that “FM” should be restricted to MEAN the myofascial dysfunction – and if someone does not have that, the medical people need to find what is the condition they DO have. If it is CFS, then it is CFS. If it is EDS, then it is EDS. It is not FM.
I also have ME/CFS, and Fibro. My daughter has Fibro and MS. My daughter and I have similar pain. We both happen to have muscle knots and extreme tightness, but according to our doctor, a Fibro diagnosis only requires 11 of 18 tender points & bodywide pain without other medical explanation.
I had severe allergy & asthma in childhood. But my illness started with a combo of chronic sinus infections, childbirth, shingles & emotional stress. My daughter’s illness started with abuse by a friend, and two cases of mono.
Cort, I do not know how your ME/CFS and Fibro got started. Are you willing to share what triggered your illness?
Any one have any knowledge if the researchers referenced in this report are aware of Dr Terry Wahls research on the mitochondria as associated with MS/ autoimmune disease and chronic illness. She states her belief that ALL illness/disease starts at the mitochondria level and has controlled studies of her own going as well.
It would certainly be interesting to know if the paleo diet that worked so well for Dr. Wahls would be on the list of the generic things that could be done to help move the mitochondria out of their sleep so to speak.
I attended the Institute for Functional Medicine’s CE on energy in July where she gave a very impressive presentation. Functional medicine holds terrific promise for people with ME/CFS as the approach is to address the wide array of underlying problems that can give rise to energy depletion. Perhaps if you can sort out 75% of an individual’s problems the body may begin to heal itself.
I have heard her addressed as ‘that diet guru’ in a demeaning sort of way, however, her long and personal research certainly brought her out of the wheelchair and has help many others get their functional lives back. She is very strict and seemingly successful with her study groups. Again ~ every one is different…it seems to never be a ‘one size fits all’ I was just personally struck by her statement early on in her research that ALL disease, not matter what the diagnosis starts at the mitochondria level~ this new research will be so interesting to follow, she was certainly motivated as well.
Thank you so much for this article, Cort, and for you blog in general. This latest work makes the most sense of anything I’ve read about ME/CFS. It certainly would “explain” how we feel, how we function and why all those usual tests come up normal. I was impressed by Naviaux’s ecological thinking about this illness, looking at the body as an intelligent system with intelligent and protective functions we inherited from our evolutionary history. It made me contemplate that ME/CFS might be a protective function, keeping us alive waiting for the danger to pass. Looking at this in an ecologically bigger perspective, we humans as a cell of a living Earth, understanding the body holistically as Naviaux does, we PWC’s are reminders that what happens in small parts of the System also affects big parts too. We really ARE the canaries in the bigger coal mine of planetary health. Some philosophical pondering as I celebrate a 20 year anniversary of this illness this month. Blessings…
Could this dauer-state be caused by hydrogen sulphide? H2S induces hibernation in animals and it has also been linked to ME/CFS.
I think it can be produced endogenously by the body, but it can also be produced by bacteria.
http://www.rug.nl/research/portal/en/publications/the-role-of-endogenous-h2s-production-during-hibernation-and-forced-hypothermia(d7d7de5d-34d8-4890-aa8b-3646d2a02a45).html!null
Poppi, of course it can. I started the whole notion of hibernation induced in humans by hydrogen sulfide with my paper “Hypothesis: Chronic Fatigue Syndrome, Mitochondrial Hypo-function, and Hydrogen Sulfide.
Perhaps hydrogen sulfide should be freshly considered as “The Hydrogen Sulfide Response”. I’d like to hear Dr. Naviaux’s thoughts on H2S. There’s a reason why all those sulfur amino acids are mentioned at the end of his Q & A.
Cort, in a number of ME/CFS groups, people are pretty upset about Naviaux presumably following up with comparing CFS to depression and PTSD. Do you know if he will be doing this? If so, do you think he is trying to psychologize our disease, tease out the differences or do something else with the comparisons?
Gail, I think he is going to find any potentially useful similarities and also tease out the differences. The idea of there being a clear distinction between psychological problems and physiological problems is now outdated. People with PTSD have reduced end organ receptivity to cortisol (problems with cortisol receptors inside the cells), as do people with CFS, so there are some similarities which may be interesting. Of course, there are also many differences – PTSD is caused by a traumatic event/series of events, CFS can be but often is not. He is not saying that CFS is necessarily related to psychological trauma, don’t worry!
No worries there. Depression and PTSD are just a couple of the diseases that he is comparing to ME/CFS. Lyme disease, autism, Gulf War Syndrome and an immune disorder (with a long name) and others which I can’t remember are also hypometabolic plus my understanding is that Naviuax will be comparing the metabolomic signatures of diseases like MS and similar diseases to ME/CFS as well. I hope he can get Alzheimer’s in there as I just read that the brain is hypometabolic in Alzheimer’s as well.
Plus we know that a substantial percentage of depression is the result of inflammation – not psychology.
Plus Naviaux with his PhD in virology and genetics and his rather remarkable understanding of biochemistry sees this disease a biochemical phenomenon and he’ll be addressing it that way.
I wish the ME/CFS community would stop beating itself up about ME/CFS and psychology. I totally agree that the “all in your head” thinking is horrible. However, if we’re in a hypo metabolic state due to psychological stress or physical stress, does it really matter which? We’re still stuck in a hypo metabolic state, with the physical things we can be measured for. This psychology vs. physical thinking is outdated anyway- it’s all both psychology and physical, although a lot of researchers and medical professionals are having trouble dropping the old way of thinking.
I think , Marilyn, that you maybe haven’t experienced the decades of abject cruelty at the hands of both doctors, media, and friends, family ,etc…that have occurred to many of us long term sufferers because CFS was termed a lazy persons excuse to stop working, or we were all a bunch of hypochondriacs and needed to just get a life. I am still afraid, after almost 40 years of still being sick, to tell a doctor I have CFS. We almost have PTSD from the abuse, ridicule and meanness we have encountered. I can’t tell any of my current friends that I have this illness. Now why do you think that had happened? No wonder we are desperate for a real diagnosis based on physical findings with no hint of anything psychological about it!!!
The brain is part of the body and vice versa, to an extent barely recognized in modern science. (Dates back to Descartes distinguishing science from religion by distinguishing the physical from the nonphysical. It saved a lot of scientists at the time but, these days, it’s killing a lot of patients.)
I study CRPS, a peripheral/central processing disorder which can lead quickly to hosts of devastating comorbidities, including FM, lupus, cancer, and things that look remarkably like ADD and CFS/ME. There is clearly something metabolomic going on there… But, if you just look at the parts of the brain affected, you see maps that look similar to several brain+behavioral diseases, like ADD, schizophrenia, and c-PTSD. If you just look at peripheral nerve and surrounding tissue disruption, you see something like diabetes. Doesn’t mean we have diabetes and it doesn’t mean we have any of the types of schizophrenia; having said that, I won’t diss mental diseases, especially since one of my dearest friends, who saved my life in the pit of CRPS, died due to his schizophrenia.
There’s a terrible and terribly unfair additional burden borne by those with mental illnesses, and it’s the social permission to think less of those who have mental illnesses.
This selective blindness around above-the-neck illnesses is exactly the root cause of the disgusting dismissiveness of the “it’s all in your mind” brigade. If they had no prejudice against mental illness, they wouldn’t be so ready to dismiss those of us with “invisible” diseases of pain and exhaustion, which — for inescapable medical, physiological, even anatomical reasons — have affective effects.
I have a category of issues in my blog called “it’s not imaginary.” It’s a big darn category. I’m hugely grateful for all the science that has come up in the past 15 years that has supported, over and over, my contention that these wretched diseases are not, in fact, imaginary. Mine *are* largely in my head — that’s where the bulk of the CNS is! — but they are definitely not imaginary.
Nicely said Isy Aweigh and a great example given that the problems caused by CRPS are so physically obvious. Let’s get rid of the mind/body duality…
Jeanie Pochatco I totally know what you mean! I’ve had the illness for 23 years and have experienced all kinds of negative attitudes during that time- that I’m lazy, that I’m not really sick, that I just need to eat more meat…, etc. etc, etc. Nonetheless, I stand by my statement. If we’re stuck in a hypo metabolic state, that is something totally different from the above, even though it of course involves the brain. Let’s just figure out what is going on, accept it, whatever it turns out to be, and move towards better health.
Returning to Cort’s article on Naviaux’s ground-breaking study–with the most significant findings on ME/CFS to date–I can only think of Dr. Paul Cheney’s work, in which he too hypothesized that this is a down-regulated state which is protective. He lectured in detail on his research and findings in videos from 2013 which are still available, though can be hard to find. I found them on google via the website of an MD with ME/CFS. Dr. Cheney has been one of the most insightful and pioneering of our experts, who has been searching for the trail of understanding for what is really going on, ever since he began with the Lake Tahoe outbreak in the 1980’s.
I don’t think he is saying cfs/me is psychological at all. However, it can be useful to bring up what symptoms or what appear to be similar “traits” of an illness so you can get doctors to recognize they shouldn’t jump to conclussions. We know also that autoimmunes sometimes create processes that mimic psychosis, depression and anxiety… But to say those diseases are psychological based on that would be silly!- autoimmune is when your body attacks your own cells.
I am sure cfs/me will get respect from this group of research- but we can’t reject good science from reliable doctors on the notion that they bring up a comparison about how the body works for another illness just because it reminds us of being dismissed for our very real real physiological problems.
Another thing to note is usually the dismissive doctors who tell us “its just depression/in your head” really are downplaying depression and its causes, effects, etc as well, and over playing treatment options. They really don’t know how to help depressed people for real, make no mistake, they just pretend they do. Imagine being one of us who hasn’t been helped by the options thet give us for depression… It honestly feels like having any disease that doesn’t get better from one pill- you get blamed, told to exercise, etc. Not helpful!
Any doctor who jumps to “in your head/mental illness” for physical problems first is negligent and useless. Any who says “just depression” and talks down to you like a child is useless. (Also children deserve respect too docs, get with the program!)
One researcher told me that we always have to include depression (or tests for depression) in our studies because everyone expects it..If we didn’t do that people we were hiding something.
Yet ‘another theory???… We’ve been down this path many a time.
Time will tell!
Actually, is a variation on an old one that I pioneered back in 2007 with Hypothesis: Chronic Fatigue Syndrome, Mitochondrial Hypo-function, and Hydrogen Sulfide. Instead of dauer, I used the word hibernation.
they described more hypothesis but the metabolic findings are real and they can help to understand the disease
🙂 Indeed it will! and hopefully soon. At some point the right hypothesis will come a long. Hopefully this is it or at least part of it.
Thanks for writing this article. It has given me new hope. I noticed at the end of the study there was a mention of vitamins and amino acids possibly being helpful, but that they needed to study this in depth. It mentioned active forms of B5, B6 and B12, as well as lysine and serine. It seems that they are talking about a methylation protocol. Am I right?
Naviaux talks more extensively about methylation in his Q and A – https://www.healthrising.org/forums/resources/robert-naviauxs-q-a-for-the-2016-me-cfs-metabolomics-paper.382/
Given the type of CDR in CFS seems “similar to that seen in autism”, does that indicate that the drug ‘suramin’ might also be useful for CFS, if efficacy is shown in Naviaux’s trail with autistic children?: http://naviauxlab.ucsd.edu/science-item/autism-research/
Is Naviaux having to be a little coy, since the study is due to be published this December? (And to perhaps avoid raising hopes, here.) Or do the unique metabolic features he found in the CFS patients mark our CDR state out as too different.
(Also, fantastic write-up Cort. 🙂
I asked Naviaux about autism. All I can say is that there is definitely a connection about the two diseases and we’ll find out a lot more about that later. The Suramin connection is interesting and may be part of the equation for one gender. I think they showed up in a fairly prominent way for one gender but not the other. The role purines play could separate autism from ME/CFS – they may be more prominent in autism.
I wrote a bit about Suramin in a blog
https://www.healthrising.org/forums/threads/an-eye-on-the-mitochondria-man-robert-naviaux-and-chronic-fatigue-syndrome-me-cfs.4163/#post-17323
Suramin acts on the membrane, as does hydrogen sulfide. If hydrogen sulfide senses hypoxia, it can reversibly reduce mitochondrial oxygen consumption and ATP production in the body. It also affects glutathione levels.
You can think of it as keeping the lights on in the body, but at a dialed down level if necessary. Its effects are largely positive, but is is Janus-faced. It is deadly at high concentrations. B-12 hdroxycobalamin is an antidote to H2S poisoning.
.
Thanks! Ah, of course you’ve already covered it. 🙂 Good work (I probably read and forgot). :-s
Yeah, suramin doesn’t sound like a great treatment in itself, then. And wikipedia certainly makes it sound scary: “About 90% of patients will get an urticarial rash […] greater than 50% chance of adrenal cortical damage, but only a smaller proportion will require lifelong corticosteroid replacement.”!
But do wonder if a short course might be enough for some to escape a catch-22 CDR loop. Perhaps those with post-infections CFS? We’ll see…
And certainly the male/female, autism/CFS divide is compelling – gender separated failure modes of the same issue. Particularly from my perspective of gradual onset CFS with ADHD-PI, (dyslexia), and knee deep on ‘the scale’. 🙂
Not sure how related this is, but I feel a bit better for a short time when I take Glutamic acid, but it causes gout to form in my left foot. I also get hives sometimes and the brain fog is worse when those appear.
I was guessing that the glutamate was helping with ammonia detoxification and the urea cycle cleared it out, but maybe the glutamate was helping directly as a neurotransmitter or by increasing glutamine stores in my brain cells?
I guess the uric acid and gout is due to more glutamine being made from glutamate and that had something to do with purines and eventually becoming uric acid? It’s like my body is primed to make uric acid if I take about 3 or 4 “00” capsules of Glutamic acid each day. I was happy to take the misery of gout if it comes with even a modest bit of relief from CFS, but luckily I found that taking an arginine + ornithine supplement tends to keep the gout in check.
Iremember a mention of using reservatrol and tocotrienls. Which I bought.
Remeber that some Brazilian physucians reversed (was it autism in mice) with that?
https://www.healthrising.org/forums/threads/an-eye-on-the-mitochondria-man-robert-naviaux-and-chronic-fatigue-syndrome-me-cfs.4163/
Brilliant write up Cort, thank you. Of everything that I’ve read on CFS this paper resonates the most. The idea of the body being in hibernation as a protection mechanism is exactly how I’ve seen this illness for a long time and its been really amazing to have some evidence to back this up. Now we just need to find a way to flick the switch back again. I think it’s probably going to be a multi-pronged approach with no one-pill solution and likely to be a little different for each of us. Having validation and back up from the medical community is very valuable in itself… and then hopefully there’ll be some treatment options that will be the final push our bodies need to heal! I do take heart from is the idea that if we are hibernation, we are poised and ready to awaken at any time… like a zombie apocalypse!! And also, think of how much the research into our illness is going to contribute the the general understanding of illness, how many other illnesses it might shed light upon. This might change the entire model of medicine as it stands today. I am so grateful to the team involved, what great work.
Good point! Being put in hibernation does suggest that you can come back from it. I distinctly remember taking transfer factor a long time ago and being zapped back into complete normality temporarily. The zombie work up!
Ron Davis thinks solving this disease will have impact on many others. You are in good company!
Lol, I’d love to be part of this zombie apocalypse?
I often tell my daughter I feel like a zombie 🙂
This is fantastic news! Does anyone know how this explains post exertional malaise i.e why symptoms don’t kick in til a day later?
I believe Dauer is very real and is key to our disease. But I believe the symptoms we experience are not the side effects of Dauer but the side effects of a lengthy chain/cascade of things that (increased Dauer due to) over-exerting sets into motion. I am in what I hope to be a VERY early stage of recovery thanks to learning to recognize early markers for over-exertion, seeing repetitive patterns that resemble a lot a cascade of effects that follow each other up in time and finding some ways to dampen this cascade.
Today it is far too early to go into details as I am uncertain of way too many things including if it is actually happening or nothing more than a mirage. If it would continue to grow into something real I’ll go into detail.
I feel confident to talk about one early marker for over-exertion I learned only a few months ago and helped me time and again since: if I feel suddenly getting more and more nervous at a very quick rate for no obvious reason while doing something (exercising, peel an apple, talk or listen…) then I need to quit and slow down immediately (or sometimes better: don’t go full stop but warm-down). Going on for as few as five more minutes sometimes makes my post exertional malaise worse by a factor of two! Avoiding that does make a meaningful difference to me.
If someone reading this tries and sees if this could help as an early warning signal, please post both positive or negative experiences. It could become a minor but helpful extension of the pacing (not PACE!) protocol.
Feeling nervous without doing any activity is not part of the observation, only a sudden rise in nervousness while doing any kind of activity. Of course, this won’t help either for those who lost their ability to be nervous (as I had during some of my worst periods).
Kind regards,
Jurgen
I forgot about how the immune system has a role in recovery. One example, if I’m remembering correctly, is that interleukin-6 gets released in increasing amounts the harder we workout our muscles. I guess cellular damage our stress from any cause, sometimes including normal use of our cells, has to be cleaned up and repaired which is at least partly done or mediated by the immune system, right?
When I studied sickness behavior a little, I read that it’s triggered by combinations of interleukin-6, interleukin-1 (maybe beta?) and TNF-alpha, I think. If our bodies are in a state where we’re already primed with IL-1 and TNF-a (or some kind of equivalent state or susceptibility) and we’re not already overflowing with IL-6, then a workout that keeps producing IL-6 during the muscle repair process would put us in a world of increased sickness during repairs.
I’m not sure what immune response other types of exertion cause or what cytokines/signals get produced, but maybe any repair process that results in blood (or maybe CSF?) elevations of some cytokines or molecules that can mimic them would set off (or increase the intensity of) a sickness or dauer state? If I stay awake too long or try to concentrate and/or clean/work too long and past my limit, then I can expect payback for two days. Shoot, if I exercise to the point where in start tasting lactic acid, I usually go into shock or something painfully and nauseatingly close to shock. I think that’s called something like exercise-induced anaphylaxis or something. If a bunch of us have that, it might make an interesting presentation for one of the SolveCFS organization’s governmental lobby days.
Exercise can induce a mast cell degranulation and may be what you are experiencing with an anaphylaxis response. Many if us with MCAS have this issue.
Issie
Great stuff! This would explain why on a trip to Park City my husband struggled with the altitude and I felt no difference.
My daughter’s titer tested negative for varicella zoster even though she had chicken pox before. I am approaching this from a pathogenic angle when the body’s immune system is compromised in a way that causes some aspect of the mitochondria function to hunker down as a defensive response. Younger’s question still remains. Why is there variability in the body’s response? Perhaps a study to track the individual’s metabolites over time on good and bad days, will also help narrow down the pathways. Even if we know which metabolites are causing the symptoms, we still need to discover the causative triggers. It could be a combination resulting ftom the epigenetics of the disease.
This has also been true for some with Lyme disease. I have a friend who continually tested negative until she had done IVIG and antivirals for a bit and finally her immune system detected it. In the POTS community I got quite the pushback when I found that I had Lyme and Protomyzoa Rehumatica and suggested it as a strong contributing factor. But addressing that and mold has made huge improvement for me. Having it chronically (Dr Fry doesn’t know of a way to completely get rid of Protomyzoa Rehumatica. We just try to co exist and maintain it.) However, it may be a lifetime fight.
Issie
Many patiënts are very excited by this news. But i think that if it is true -that we’re stuck in a hypometabolic state- it is going to be a hell of a job to get us back in a normal state. So it is much worse for recovery then most patiënts are thinking. That is no good news at all.
Cort, this is the first time I have a reason to explain why there have been times when even if the house was burning down , I lay there and felt I it would have been impossible for me to get out of bed to get up. It felt as if I were in an almost coma. Fatigue doesn’t even describe what it felt like. A total collapse, a shutdown of physical and mental capability to act.
I’ve never seen so many people commenting before. This is resonating with so many of us! Thank you, Cort.
Well said Jeanie….a shutdown is a much better description….that resonates more for me than “fatigue” which suggests that you can just push through it doesn’t it? May be that’s one of the problems with that term.
And yes, this has got to be the most commented post ever – it is striking a chord.
The next post in the series on metabolomics is here by the way – https://www.healthrising.org/forums/threads/hansons-metabolomics-me-cfs-study-validates-naviauxs-core-finding.4846/
I found the reference to tetracycline interesting. When I came down with CFS, a doctor put me on this antibiotic (in case I had Lyme disease), and I almost died. My condition worsened dramatically but improved when I took myself off the drug.
It does bring to mind some people who do poorly on antivirals….
Re anti virals possibly being harmful unless there’s a current infection, does anyone know if a high early antigen Epstein Barr would be considered as such? I’m told that it shows an old infection has recurred but it’s not a new infection which I understand is IgM vs IGG. My PCP doesn’t even test for early antigen anymore because she says she’s seen no difference in those who have high levels who are healthy vs those who aren’t, so that sounds to me like it’s not too significant. I’m currently taking acyclovir to no avail at 2 bucks a month and was going to start on Famvir today at 100 bucks a month so wondering if I should even bother. Thanks for any thoughts…
Thanks Cort!
My personal guess (not a doctor) is that this might relate to identifying the disease process and most patients, but I also have a feeling it is not causal… Being that I am not a scientist I couldn’t give you a sound reason why. Either way eagerly waiting to see where this goes!
I agree Shy. I think the cause can still be the parasympathetic nervous system. The body can’t relax and is going into the dauer state to save enegy.
Well, this finding by itself may be exciting, but the dauer hypothesis still needs to explain all symptoms and all other previous findings, eventually. How does it explain orthostatic intolerance, insomnia or brain fog, for instance? And 24 hour delayed post-exertional sickness? How does it work with findings like gut microbiome change, white matter atrophy, HPA Axis dysfunction, etc, etc.? At some point, someone will have to put all these puzzles together and come up with a testable “unified theory”. For now, it seems like blind men and the elephant.
It a very complex disease as you point out and anyone who comes up with a unifying hypothesis is going to have a lot of work to do. It’ll be REALLY interesting to see what Ron Davis finds out when he tries to merge genetic data with metabolomic data. Will it be able to explain why some people have OI while others don’t? Or why some people who are really, really fatigued have little or no pain while other people with less fatigue are in a lot of pain?
Hopefull it will be a start to explaining that.
Sleepless nights for Wessley & Co.!
NOT “hibernation,” but “dauer” – different concepts. The OMF & Dr. Naviaux provide a very helpful and informative Q & A page here: http://www.openmedicinefoundation.org/2016/08/30/metabolic-features-of-chronic-fatigue-syndrome-q-a-with-robert-naviaux-md/
Ya know, I never made a “bucket list” b/c I knew I was too sick to ever do any of it. But now I have one:
1. See a recording of the moment Dr. Naviaux realized what he had discovered.
2. See/hear a recording of the moment Dr. Naviaux relayed the information to Ron Davis & Janet Dafoe.
3. See/hear a recording of the NIH’s responses when they realized they’d been exposed.
4. Ride a horse again – after Dr. Naviaux’s paper was published on Tuesday, I even dreamed about riding a horse for the first time in over 10 years.
I am forever grateful to Dr. Naviaux and his team, and OMF – thank you and God bless you all.
Could the dauer-like state be the mechanism that results in what’s called “sickness behavior”? Is sickness behavior triggered by the mitochondria (cell danger response) or do they have a significant role in it? (Long shot, but is it worth checking to see if the shutdown part of our immune response derived from something like the dauer state?)
I’m also wondering what happens when something like the cell danger response triggers but the targets for it aren’t there. Would the metabolites that are usually present after the CDR activates and meets infectious agents (or something) be low or missing if those weren’t present?
I do find it hard to believe how little I’ve seen the term “sickness behavior” turn up when trying to research ME/CFS, fibro, etc. Is there a proper term for the mechanism that results in the sickness behavior portion of being ill or having an inflammatory response?
Doesn’t sickness behavior describe (from an external observational viewpoint) the “flu-like illness” that shuts us down and often makes us bed-bound? I think I read that it’s the evolutionarily inherited (across many species) adaption or tactic that would increase both an individual’s and community’s chances of survival by preserving energy and resources for an individual to heal with and possibly to help the community by not spreading disease. Is that what we’re going through?
Then wouldn’t the cause be hard to detect since the “fatigue” aspect would result from normal immune functioning? If it’s largely normal functioning, then the disorder might be the part that keeps us perpetually in this sick state. That could be caused (or partly caused) by an inability to leave the sickness state. Or it could be partly due to perpetual immune activation, which could have many cumulative sources considering how many entry paths there are that trigger immune response. And many of those would also be considered normal according to the tests. I bet I don’t have convince many here about how disappointing it is to get back tests that tell us we’re normal.
Seriously though, is there a proper name for the evolutionary adaption that shuts us down and turns us into zombies when we get sick? People can sympathize with that much more than “fatigue”. Not that I’d want to use “sickness behavior” since “behavior” means something a bit different in psychology that people will connect with choice. I was thinking something like “sickness signalling” “immune shutdown”, but maybe there’s already a proper term?
Anyways, this article has me excited. There’s finally some indication that there are tests that dig past the usual methods that search for specific causes/makers of disease to look deeper into what appears to be normal functioning. And maybe there’s a strong connection of this mitochondrial functioning to sickness shutdown which gives us a target to fight back against.
I also want to mention that when I tried to research sickness behavior, it was hard to find info, but what I found said that there are two paths that signal it: 1) a humoral path using cytokines and 2) a fast transmission path through the peripheral nervous system, especially the vagus nerves. I have no idea if these are relevant, I just wanted to pass along that info in case they could be contributing factors that might get overlooked.
How do you explain according to these findings that 80 percent are woman? And did this cohort use medicine? Or had a diet? I don’t read this in the publication, anyone?
Dr. Cheney has a theory or rather data that women are naturally more catabolic and men are naturally more anabolic (a male lion lying under a tree is building muscle). This disease is catabolic…we are stuck in that state.
I wonder what Dr. Cheney means in terms of healthy men and women? Either generally or technically–
I wonder if the fact that mitochondrial DNA is only passed from the mother could have any bearing on the preponderance of females with ME/CFS, since this is largely an illness in which the mitochondra get hammered? I can’t analyze or think well today, and don’t know much about human biology anyway, but maybe there is some relevancy to the way mitochondrial DNA is passed down.
Men & women differ on different levels:
-immune system
-brain wiring
-metabolism (catabolic-anabolic)
All of which are crucial in ME.
This article and the comments are fascinating. I wish I could understand how this theory could explain the way that each and every one of the things that work for me, work, and why the things that don’t, don’t. I do get from this though, why no one thing that works ever works so much overall that I’m cured, but why a cumulative effect of many things that help a little, all together and over time, can help to shift the body’s function in a major, and possibly permanent way. I wish I knew what kind of protocol we could glean from this that would be guaranteed to work for a majority of the population. I guess though that do anything that gives the body a sense of relaxation and well-being, if you find any means of doing so, could have a positive effect on the cells to repair themselves?
Does this metabolic dysfunction explain cognitive dysfunction? I don’t get the process that relates them… unless it is a direct result of inflammation in the brain, which is a direct result of problems that lead to inflammation.
Incidentally, I will add another vote here for calling it “Living Death Disease.”
Does someone have a link for the next IACFS/ME Conference information? I am interested in the lineup which now includes Dr. Davis.
Also, is there any longer a video showing Dr. Paul Cheney talk about the abnormalities he found in the heart, as these, it turns out, relate to the hypometabolism currently being found, and suggest its at least partially protective effect
Hypometabolism and reduced blood flow to the brain easily makes sense; what I’m still trying to bring together is hypometabolism and neuroinflammation.
Good question….the body is nothing but complicated…I did just read that Alzheimer
‘s patients, not surprisingly, display a hypometabolic brain and I assume there’s neuroinflammation there. Perhaps if the cells are in a hypometabolic state they can’t protect themselves against oxidative stress? I do remember that not using oxygen in mitochondria leads to a build up of it in the cell. Oxygen is a free radical and that increases oxidative stress which is presumably used to kill pathogens…So hypometabolism and oxidative stress seem to go together (?)
The blood flow is not reduced in a constant manner: it gets much worse during (and after!) exertion for example. This may well lead to “moderate and temporary brain ischemia”.
According to: https://en.wikipedia.org/wiki/Brain_ischemia
“Brain ischemia (aka cerebral ischemia, cerebrovascular ischemia) is a condition in which there is insufficient blood flow to the brain to meet metabolic demand”.
That resembles our state somehow. Now, Dauer could be a “kinder” solution to the inability to meet metabolic demand than brain cell loss as that is quite permanent and irreversible.
The only thing worse than brain ischemia is reperfusion injury. See the section in previous linked article: “Reperfusion injury is classified as the damage that ensues after restoration of blood supply to ischemic tissue” and following link to more info: https://en.wikipedia.org/wiki/Reperfusion_injury
Remark “The absence of oxygen and nutrients from blood during the ischemic period creates a condition in which the restoration of circulation results in inflammation and oxidative damage through the induction of oxidative stress rather than restoration of normal function.” in the second article. Sounds somewhat familiar too?
I believe this continuous cycle of “moderate ischemia” and “reperfusion-like damage” is a major part of the cascade delaying over-exertion from post exertion malaise.
Summed up: Dauer may be able to trade more permanent brain damage for a mixture of some permanent brain damage, some neuro inflammation and truckloads of highly unpleasant Dauer.
Note: I do not believe reduced blood flow is cause nor result, it is merely a chain in the endless and complex cycle of passing the hot potato in order to “manage and minimize in some kind” the damage this devastating disease/endless cycle does.
Kind regards,
Jurgen
Thanks for writing this Cort.
I really appreciate reading all the comments too.
At age 55 1/2 it feels like a lifetime of being sick and I am so anxious for a cure. After reading this article I just felt like crying, how many more years before treatment? My patience is running out. It is exciting don’t get me wrong, but I just want a life back.
Again thanks for the great article and your great website.
I don’t know but I can tell you that Naviaux already has ideas about treatment. ME/CFS is not a black box and hopefully he’ll be able to begin some small treatment trials in the not to distant future.
Ron Davis has talked about core treatment regimens and then individualized ones. I imagine the Naviaux has some good ideas about core treatment regimens for ME/CFS
Stay tuned about metabolomics as well – something exciting is coming up 🙂
At the point we were discussing antimicrobials, statins, etc as harmful to mitochondria in the views of Dr. Davis and Dr. Naviaux, and not recommended by them unless there is very clear evidence of infection and need–which by implication seems even more important, I want to say that we are most likely to have choices to make, a cost-benefit analysis, rather than an ideal treatment scenario. We wish, I believe, to end up with a treatment which can reverse this retreat into a hypo-state, a treatment that not only works but causes no harm. But before science gets there, if it will even succeed, what we have now will be choices between better and worse. Science hasn’t arrived at the point of clear treatment recommendations but we are always there–at the point of needing to decide how to handle our conditions. We will need to try to measure priorities because we may not be able to protect the health and functioning of mitochondria and treat those other infections and conditions at the same time.
I assume that mitochondria can recover after those medications but I don’t know that. Do they take a dive that is just temporary or is it permanent or is this entirely unknown? When you think of chemo for cancer, the negative “side effects” can be temporary, long term or permanent. As they keep coming up with new forms of chemo, they usually don’t know what the side effects will amount to. These also vary individually. The question is the cost-benefit ratio.
So I guess my point is for us not to expect either success or if there is harm, only temporary reversible harm. There can be irreversible harm so it may be better to abstain from treatments which are uncertain in our cases.
My first thought when I read this published study was “I wish Rich Van Konynenberg were here to read this.” I would love to have heard his thoughts on it.
The idea of our mitochondria being stuck in idle makes sense to me because I have always felt that whatever was going on, it was happening in every cell in my body.
I love that Dr. Naviaux and Dr. Lipkin are not ruling out the possibility of fungal toxins having something to do with the cause of our illness.
And I love your thoughts, Simonne. What if our bodies are reacting to the toxic global environment we humans have created for ourselves?
How possible would it be to ask everyone to please stop putting poisons into the environment, so that we could heal? And I wish more researchers would study how poisonous chemicals put into the environment lead to fungi making stronger and more harmful toxins.
I was horrified when I heard how many thousands of chemicql compounds were let loose on the earth each week. This has been going on for decades. Who knows what effect they all have?
Combine that with the estrogen mimicker effect of many of them, it’s not surprising I guess that our immune systems have gone haywire.
Estrogen excess affects men as well as women.
Oh for a return to sanity! These corporations full of greedy dills have ridden roughshod over the earth and over us who depend on it for long enough.
Here’s to our hopeful return to health *clink* (non-alcoholic beverage of course)
“I love that Dr. Naviaux and Dr. Lipkin are not ruling out the possibility of fungal toxins having something to do with the cause of our illness.”
I couldn’t agree more. Those of us who have been through the nightmare of chronic intestinal candidiasis (caused by oral tetracycline over-use in my case) know all too well how deeply embedded it can be in ME/CFS. I’m sure the connection will become more evident to these researchers as they uncover the roots of this disorder.
I loved your summary Cort – what an exciting, ground breaking study.
I think our understanding of the long-term effects of trauma will help provide a very broad and comprehensive underlying mechanism that fits with Naviaux’s findings and with many, many of our symptoms as well as the variations we each have in how they emerge, what we indivdually respond to (and don’t) etc.
The research in our understanding of how trauma affects biochemical pathways and causes an intelligent change of nervous system states is emerging: Rachel Yehuda, Alexander McFarlane in trauma; Michael Meaney in epigenetics; Stephen Porges with the role of the social nervous system branch of the PNS suppressing the baseline metabolic states of the sympathetic but the Dorsal vagal or “freeze” branch of the PNS suppressing both and leading to the state of hibernation humans are not designed for; Peter Levine (“Waking the Tiger” and “In an Unspoken Voice” showing how trauma has long term effects that start with high sympathetic arousal after trauma and low cortisol / low energy / brain fuzz / difficulty relaxing etc late stages of trauma… and more.
My sense from Nav’s work is that these hypometabolic states reflect a common history of accumulated traumas (big and small, visible and invisible) over a lifetime (prenatal, birth, adverse childhood experiences or “ACEs” such as abuse and neglect but also being bullied and losing a parent etc; accidents, surgery etc). Some of us recovery from trauma, some of us get stuck in states of hibernation / freeze like c. elegans in dauer. Some of us end up with CFS, others develop Alzheimer’s or autism.
I think our illnesses come from an intelligent but no longer adaptive state of shutting down and waiting until it all blows over. We’re not broken. It’s that our systems are stuck in the wrong gear for living.
The huge variety of treatment solutions that work differently for each of us reflect that there are many ways of actually healing from trauma (think of Norman Doidge huge variation of treatments described including light therapy, sound therapy, feldenkrais, trauma therapy in his book The Brain’s Way of Healing)… These approaches – when combined with diet, activity levels that work to oxygenate rather than tire, with regulation through activities such as meditation etc – can all help CHANGE the underlying nervous system states. I don’t think there’s a pill. or a quick fix. But it seems to me there is a way.
I’m working on these approaches myself with my 20 years of CFS. It is slow. But when I look back it also took me decades to get sick. I’m thinking that the trauma piece is larger than we realize or recognize and the outdated but still ongoing blaming of it (and CFS) on psychological / psychosomatics / all in our heads has done us a huge and painful disservice.
Phew. I didn’t mean to go this long and got into what is near and dear to my heart! That’s how exciting these new findings are 🙂 I can’t wait to hear more!
Nice one, Veronique. I’m fascinated by the way our bodies have handled the onslaught too. Exploring the ways my body has sequestered away my trauma, the same way it does with toxins, and how it works to heal those states just as soon as it can, has given me a real admiration for our bodies’ intelligence.
I agree, the “it’s all in your head” brigade have done us a severe disservice when it comes to the bodywork side of things.
Thank you Veronique! I resonate with your articulate assessment of the role of trauma in all this. The suggestion that this dauer state is protective makes sense. I wish trauma therapy was more recognized and available. Thanks for the suggestions and book titles.
I don’t have a sense that trauma contributed to my illness but it certainly must be one pathway to sympathetic nervous system arousal which I believe is key to this illness. I imagine that there are several pathways to this end state.
Since after ME/CFS almost everything seems traumatic in a weird way I imagine that the trauma aspect starts there for many people.
I remember all those years the psych lobby kept studying us and trying to establish a link between us and trauma or mental illness. They never succeeded. Our population turned out to be average or unremarkable in those respects. That doesn’t mean there can’t be stress or mental illness but only that the levels aren’t higher than “normal”.
I didn’t have trauma as an immediate precursor either, Cort, but think I may understand what you mean about everything since this illness began as being traumatic in a sense. I wonder if this has to do with how you wrote that it is easier for the body to react than to relax? Muscles contracting and heightened sensitivities, more insomnia, etc. are worse in a lower energy state. So the more tired, the more that ordinary stressors are too much. I know when I (rarely) try to fly somewhere, getting to the airport on time, standing in lines, hanging onto my ids, being wedged into tiny seats with no leg room, etc. all bring about such a state of stressful arousal that it takes five weeks to recover. Loud noises, bright lights etc. too can also feel like something of a catastrophe.
An amazingly accurate description of what happens to us. Thank you for writing this!
Thanks for the response Cort. My illness did not start with trauma either. It started with an infection (a severe gastroenteritis). I am currently doing some trauma therapy though, and what Veronique is saying makes sense to me. The effects of trauma lodge in the body and it is a great disservice to the complex workings of the triune brain and mind-body to call it a purely “psychological problem” as the psychiatric CFS camp does As a victim of the PACE protocol which is/was disastrous, the trauma therapy I’m doing now is the most promising thing I’ve done so far. I’m not saying it’s a cure but something seems to be happening. It is long and expensive though and results tenuous so far. Maybe it just helps with coping but any port in a storm, I’d say.
One thing that crossed my mind about the “dauer state”. If this state is indeed adaptive/protective, might bringing the body out of it be risky, if in fact the “danger” (and we don’t really know what that danger is) is still present? There are still so many unanswered questions. Right now I am excited to even get a diagnosis as that legitimizes the illness at least and could lead to more support for our struggles with the illness and more research funding.
What is the trauma therapy you are doing?
So well said Cecelia….It’s the wired but tired thing. A system that is under strain ALL the time and then folds when small outside stresses are applied. It certainly sounds and feels like an exhausted and very twitchy system…
Hi Cort,
I too believe there are many pathways and I suspect this is why we each have such variations in our symptoms and in our symptoms over time.
As for trauma, it certainly may not contribute to everyone’s illness. I’m curious, however, about the degree to which it’s role may be underestimated in all kinds of chronic illnesses (not only CFS but also MS, type 1 diabetes, autism, Alzheimer’s etc) because there are a number of factors I’ve been learning about in my research that I never knew about as a physician, are not yet recognized in medicine and remain outside of our cultural awareness that make many of us think we haven’t experienced it in our own lives. And because of how much we (ie: the medical system) has blamed and shamed and stated that trauma is only associated with psychological symptoms when what we’ve been learning is that it has remarkably significant effects on our biochemistry (as Naviaux’s work may be suggesting).
In my own research I’ve been looking for links to mental and physical illnesses and their causes. I’m not sure the causes are different (similar to Pat Hand’s reference to Teri Wahls belief in this as well). Rather, I suspect it’s the timing of early traumas and our genetic predispositions and epigenetics that influence which illness(es) we develop. There are fields of research supporting all of the info below but they’ve not been taught in medical schools or thought to related to chronic illness. Perhaps this will resonate with some?
Some of the under-recognized characteristics of trauma we may not recognize include the following:
1) That developing a chronic illness is likely the effect of an accumulation of traumatic events and not a single event:
– starting with trauma in our parents’ lives (war and abuse but also loss of loved ones, accidents, illnesses, miscarriages, jog loss etc), which can affect the next and subsequent generations (3 generations even or more) via epigenetics (Rachel Yehuda’s work)
– experiencing prenatal trauma (parental but especially maternal stress, illness, or accidents, maternal loss of a parent or other family member, illness as a fetus, premature birth (many of which can be life-threatening for the baby and therefore potentially inherently traumatic)
– birth trauma (emergency cesareans for life-threatening events, complicated births, the need for intensive care or time in an incubator…)
– adverse childhood events or “ACEs” (physical / sexual or emotional abuse or neglect, having a parent with a mental illness or substance abuse, loss of a parent or other loved one – this is from Vincent Felitti’s research – or from illness or hospitalizations, being bullied etc)
2)That traumatic events are not just related to “big” things (surviving war, assault, car accidents) but are often remarkably subtle, such as falls, being vandalized, losing one’s home, etc. One of the most under-recognized forms of trauma is what I think of as “invisible ACEs” (it is referred to in the literature as “developmental trauma” because it occurs in childhood during critical periods of development of our brains and other organ systems). This arises with parents who are not abusive and who are often seen as very normal but who are not particularly involved or present/loving/nurturing/connecting with their children. Such behaviors tend to stem from their own trauma (this is cited in research such as by Robert Maunder) and they influence the development of that PNS part of our nervous systems so that it doesn’t learn how to dampen the SNS as much and instead either facilitates more vigilance (high SNS) or freeze states (the dauer or hibernation response to inescapable threat) or a combination of both.
3)That the stressful events that trigger our illnesses are often a last straw rather than the cause. Such events (infections, vaccinations, toxic exposures and other environmental factors) take a nervous system already primed from previous challenging life events for greater sensitivity and responsivity to threat and tip it over an edge into more overt biochemical patterns of defense and self-protection or hibernation (as suggested by Naviaux research and theories). For some of us, these changes show up as a chronic illness.
Very informative post! The mind & body are not separate, so it makes little sense that trauma would affect people psychologically but not physically. It is also intuitive that traumas would be cumulative. I’ve seen it in my own life, and in relatives & friends. Thanks for posting!
I totally agree Veronica. I feel that the important thing to emphasise whenever we talk about a link between ME/CFS and trauma, is that trauma takes many forms – it might be a physical trauma/a virus/or extreme emotional trauma that provokes this reaction in the body.
I personally had developmental trauma followed by an extreme shock trauma which resulted in PTSD, followed by assaults to my immune system including bad flu and immunisations and travel abroad, combined with what I suspect to be a genetic predisposition. So I am completely on board with the trauma explanation and understand the physiological effects of trauma and I’ve read many of the books you reference.
But I can imagine that for someone who has been fine and then come down with glandular fever and never recovered, even the use of the word trauma might be inflammatory, and rightly so… because if we talk only about developmental or shock trauma then we are not giving the whole picture.
We need to get across that the body doesn’t always know the difference between different types of trauma – an attack is an attack whatever form it takes. Somebody can have no known history of ‘trauma’ (or less than average, I think we all have some), and come down with flu and their body reacts as though they’re being attacked and maybe in the same way as if they had just been through a major life trauma. This doesn’t mean that they have experienced ‘psychological’ trauma, but the underlying physiological response may be the same and this is what we need to concentrate on.
Hi Tia,
Thanks for your feedback. I love the perspective you’ve added about the many forms threat can take.
This is a tough one for people with ME/CFS to get because we are so wary of being labeled with a psychological disorder. I think we just need to understand, again and again, that trauma has been shown to increase the risk of many biological diseases.
Some of us manifest in a way where we can be terribly fatigued or fluish a large amount of time, but other times feel totally normal during which we are joyful, engaging, interested, happy – and no one would have a clue there was anything wrong with our health. So I wonder, if a psychotherapist who studies these connections has a group of say 60 people, 30 healthy controls and 30 diagnosed with CFS who 10% of the time feel well and don’t have any significant trauma they can think of and had wonderful childhoods, could a therapist tell with anywhere near 96% accuracy if she had talked to a healthy control or one with CFS during that 10% healthy/happy/engaging/joyful time?
I don’t believe pwme avoid psychology at all. I went to a neuro-psy to make sure bc there were so many questions without answers. then later on to a psy to deal with the grief of being ill … There simply was no trauma before getting ill. It’s not a touchy subject at all for me. If there wasn’t then there wasn’t.
Many people (sick & healthy) had trauma’s in early life or in adult life. That’s more normal than having none imo.
It sure is a Major stressor & won’t do any illness any good of course.
But time & time again it has been studies & pwme do not differ from average populations re trauma etc.
Parkinson, MS, alzheimer, crohn’s, … the cause is not trauma & neither did it play a role in the start of patients getting ill.
If ME is a genetic immune dysfunction (NKcells & innate immune system) leading via infection to a metabolic standstill, w/ lowered cardiac output, brain connectivity problems, CNS & HPA dysfunction, etc etc , where does trauma fit in then? In the ‘cycle’ itself perhaps but not in the beginning of …
Thank you for this, Veronique. It makes so much sense. My trauma therapist (who practices SRT) would totally agree with you. She says much the same things.
Sipora Weissman: My doctor referred me to a counsellor for help in coping with severe back pain from a car accident 2 years ago when I had run out of treatment options. The counsellor happened to also has training from here:
http://www.cftre.com/courses-seminars/what-is-self-
regulation-therapy/#whatsym
It helped the pain when nothing else did. But she also acknowledges that other chronic illnesses can be helped too.
https://acestoohigh.com/2016/09/08/7-ways-childhood-adversity-changes-a-childs-brain/
Hi Veronique – You seem like a very thoughtful, nuanced person, and even better, full of kindness, so I somewhat feel bad about the comment I’m about to make. But I am itching…
I too am very interested in the impact of trauma on a person’s existence. Huge impact.
That said, it seems that whenever a solid biological finding on this illness comes up, “psychogeneticians” suddenly manifest themselves.
Maybe because the biological news threatens to make them loose popularity? Or – worse – they just use the new spotlight on the illness brought about by the biological news to sell their non-biological theories (and books, Cds , seminars…).
Yes, you have an integrated view of all possible aspects involved in an illness, so on appearances you don’t fall in the narrow psychosomatician categoy. But the overall message of what you write is:
“ME/CFS? Look for psychological trauma”.
YOU may be more nuanced; but the average ME/CFS skeptical readers won’t be. And most of them, after an excellent write-up like the one Cort just did, will go right to the comment section to make an opinion – that is, to look for a confirmation of their preconceived ideas, ideas which do not stand a chance against the write-up alone…
All it takes is one comment below that consolidates their view.
Believe it or not I have just read today another excellent piece on Dr Naviaux’ s findings in The Economist, but the very first comment speaks of trauma yet again. A certain Veronique Mead, MD…
Nothing wrong there a priori, I mean it; everyone is allowed to make a living or cease occasions and opportunities that favor that.
But – and this is the crux of the matter – a sick and suffering ME patient whose family members are skeptical about the reality of their illness, well, just because of that comment below, that patient better not send them that otherwise excellent article.
We are killing ourselves getting something like PACE off our backs and to consolidate a solid physiopathological view of this illness, in the pubic image and governmental policies.
So please, if you want to promote your theory, please, use other outlets than media coverage of Dr Naviaux’ s findings, or the upcoming ones from Ron Davis and the like.
Unless, of course, you feel you can help Janet Dafoe and Ron Davis understand what is happeneing with their son Whitney. He really needs help.
Wow! What a great reply you gave to Veronique! Thank you for so well stating what all of us who have suffered so much dismissal feel !
Thanks for excoriating me / my theories so gently Christian, and for the kindness of acknowledging my intentions that are as far from dismissal as I could imagine. And giving me a heads up. I very much appreciate that.
Sometimes I am grateful for the fact that I can at least speak to this perspective from having long-standing ME/CFS myself, including having spent almost a year with difficulty sitting up for more than a few minutes at a time.
Do none of the biological / epigenetic and other physically-based findings and newer studies showing that trauma influences our physiology / biochemistry / nervous systems/ immune systems / brains and more provide any support to negate the horrifying legacy that all trauma is psychological and therefore ME/CFS and our histories is all in our heads? And I ask this question, like yours, very honestly.
Is it more about the risk of feeding the skepticism that our disease is not real – even when citing large bodies of research with solid backup in physical fields?
Would it make any difference if I thought that different types of trauma were a risk factor for other diseases too (which I do) and not just ours?
As for whether this theory could possibly help explain the complexity of risk factors leading to ME/CFS and the terrible extent of incapacity that is experienced by some people like Whitney Dafoe (and all it has meant to his and other people’s families and loved ones) – as well as others with different chronic illnesses – I’ll take the risk of saying that I have written about 11 characteristics of trauma that appear to contribute to the evolution of very real physical chronic illnesses – from ME/CFS to type 1 diabetes and MS and others – from the perspective I refer to. For some it offers insight into variation in symptoms, severity of illness, speed of onset, degree of trauma and sensitivity to the environment after onset, delay between a “final stressor” and onset, an intro to mechanisms, and a few more. If you have any interest in reading it I’ve attached it to my name here. For those for whom it is a topic that does not fit and/or will be offensive there’s no need to go to it.
PS – Re the Economist – I see your point. It’s a valuable perspective, and I agree with you. It will make me be more careful in the future.
Thank You Christian for saying this so eloquently.
I can say it a hundred times ‘trauma was never a part of my life untill i got ME’.
Please let Biomedical research take the stage for once without adding yet again psychological factors.
Psychology had the stage for decades and it did not help any of us who have ME.
Well said!!
Well said Christian! I was offended by Veronique’s attempt to sabotage a great research study by attempting to reduce this devastating disease to trauma. I wish she would keep those sorts of comments to herself until it’s firmly established in people’s minds that this disease is not the result of cumulative trauma. I think they are destructive. The psychologizers have done enough to destroy our credibility. We don’t need her to add more fuel to the fire.
I’m grateful for the people who challenged her clear bias. And she has an MD after her name?! Frightening.
I realize this is a difficult subject and I agree that having a trauma comment at the top of the queue in the Economist article was a bit unnerving. Adverse childhood incidences have, however, been found in many studies to increase the incidence of physiological disorders. Veronique has never said that trauma is the sole cause of ME/CFS – she has suggested that it may put in place physiological changes that increase the risk of ME/CFS years later in some people (including herself). That’s the same scenario shown to be true for autoimmune and cardiovascular diseases http://www.ncbi.nlm.nih.gov/pubmed/26289252 .Unless people with ME/CFS are somehow different from those people I don’t now why that wouldn’t be true in ME/CFS as well.
Author and autoimmune disease patient Donna Jackson Nakazawa, for instance, has an autoimmune illness so severe that it twice temporarily paralyzed her. She believes the death of her father may have helped introduce the immune changes that decades later contributed to her illness and the research backs this up. She wrote a book how that was so.
How do you scientifically study the trauma factor though? Donna or others may think there’s a connection to some trauma in the past, other’s don’t see any. How could double blind studies be done? Seems to me this aspect can be only subjective guesswork?
I think you have to go back and do retrospective studies in ME/CFS. I think the evidence in mixed in ME/CFS but even if a strong connection is not found – and a strong connection has not been found in my knowledge – that doesn’t mean it’s not a factor for some people.
In response to Betsy’s question about trauma research and chronic illness – and as Cort mentions – some such studies are retrospective:
One large body of research was initiated by Dr. Vincent Felitti of Kaiser in collaboration with medical epidemiologist Robert Anda of the CDC and first published in 1998. Over 60 additional studies have been published since and 32+ states across the country have reproduced similar results (this is another way of supporting findings). The folks at Kaiser have since followed more than 400,000 people for 15 years and found the same results.
These are called the Adverse Childhood Experiences or “ACE” studies and started with a questionnaire sent to over 13,000 adult Kaiser patients. The Q asked about 7 (now 10) specific types of trauma experienced before the age of 18. People scored 1 point if they’d experienced any type of trauma in a particular category.
The types of trauma picked were based on issues being addressed by national programs in the 90’s instead of trying to cover every type of trauma. The researchers were stunned to find a graded relationship to adult health issues, including cancer and chronic illness such as heart disease and autoimmune diseases. The higher the score the greater the risk.
“Risk for the 80 or more types of autoimmune diseases increase as ACE scores rise. For every increase in the ACE score of 1 point, risk for developing an autoimmune disease such as type 1 diabetes, lupus, rheumatoid arthritis and many, many others goes up by 20% (study by Dube, 2009). An ACE score of only 2 or more increases the chances of being hospitalized for an autoimmune disease by 70 to 80%.”
Here are 2 great articles on a blog called ACEs Too High that focuses on ACEs and lists the 10 questions/types of trauma:
ACES 101: https://acestoohigh.com/aces-101/
ACEs and chronic illness: https://acestoohigh.com/2016/08/10/childhood-trauma-leads-to-lifelong-chronic-illness-so-why-isnt-the-medical-community-helping-patients/
I’ve also written specifically about ACEs and the trauma perspective, using the movie Boyhood as an example of how we think of many difficult early life events as just being “normal” and the ACE studies suggest there’s more impact than we’ve realized.
http://chronicillnessblog.com/adverse-childhood-experiences-and-chronic-illness-boydhood/
In this post I refer to the fact that some people with chronic illnesses, myself included, have an ACE score of “0.”
Since the Q is up regarding possible links between transgenerational trauma and chronic illness – and Betsy’s question of how this topic is researched – there is another large body of research that has followed people who’s mothers were pregnant during a siege in WWII known as the Dutch Hunger Winter. They found such experiences affect long term health, including risk for heart disease and other symptoms associated with metabolic syndrome (high blood sugar and type 2 diabetes, high cholesterol, high blood pressure, obesity). These effects often carry forward for more than one generation.
One good reference on the topic is a book called Life in the Womb. While this body of research, referred to as the Fetal Origins of Adult Disease, focuses mostly on lack of nutrients as the risk factor there would clearly have also been a component of psychological trauma:
https://www.amazon.com/Life-Womb-Origin-Health-Disease/dp/0916859568/ref=sr_1_2?s=books&ie=UTF8&qid=1473512150&sr=1-2&keywords=nathanielsz%2C+peter
A 2013 article in Discover magazine does a wonderful job of highlighting what we’ve since been learning about epigenetics and how such early trauma as well as early relatinship experiences have an impact and can be transferred across the generations:
http://discovermagazine.com/2013/may/13-grandmas-experiences-leave-epigenetic-mark-on-your-genes
And this 3rd article from 2014 describes Rachel Yehuda’s work (among others). She has been looking at the impact of the Holocaust on later generations. While she’s looking primarily at PTSD here some of her other research shows an impact on physical health and biochemistry / biology:
https://newrepublic.com/article/120144/trauma-genetic-scientists-say-parents-are-passing-ptsd-kids
I think all of this has potential relevance to chronic illnesses of all kinds,including ME/CFS, at least in my own case even though my parents did not experience Holocaust-type trauma and didn’t starve when pregnant with me.
Thanks for your reply Veronique – I’ll read the links you posted. Trying to keep an open mind even though in my little world I am sick with 0 ACE’s and know people with some big ones who have great physical health/energy, so hard to swallow this concept from my perspective although the info you’ve posted gives pause.
Hi Betsy,
Yeah. I have a 0 ACE score too.
I think it’s remarkably really complex and there are protective factors that help “buffer” risk as well, such as sometimes happens for those who had horrendous trauma but had someone they could talk to whereas others had minimal overt trauma but no real supportive connections with anyone (and that brings up a whole other body of research).
Thanks for your response and Issie’s and all the others in this really fascinating conversation. I find it’s an ongoing learning process that we are helping one another with because there is just no clear “answer.”
Well put Cort.
Also, there is now some studies going on into generational epigenetic changes due to trauma. Some docs are connecting within families a trickle down affect. It may cause a turn on or turn off of certain genes or reactions in multiple generations. I don’t completely understand it but am open minded enough to consider it.
And, I have texted with Veronique in the past. She is a lovely lady, very sincere and tries to be helpful. She isn’t judgmental or dismissive. She has been very, very sick herself. If she thought her views were dismissive or disrespecting those of us to a mere idea of “thought”, she would be including herself into that picture. She is in the boat with us.
The mind is a powerful thing and there is no way that it isn’t somehow involved if for nothing else with neurotransmitter dysfunctions somewhere in our illness path. Sadly, too many people try to disconnect our heads from our bodies. Our head and brain are so much a part of our body and can’t be disconnected. We have to be willing to look at the whole body not just the function of one part of it.
Even if we may have had some trauma that caused an epigenetic change in how our bodies work, that doesn’t take away from the fact that it is a real epigenetic change and…….very real.
As Cort so eloquently brought out, this is just one possibility for some. There can be many causes. But if we disallow this as one “cause or contributor” we isolate those who have CFS and FMS from our illness. And for them, CFS and FMS is just as real, painful and debilitating as it is for the rest of us. Those want a “cure” too.
Sadly those who don’t allow for the thought of trauma connection are being just as “critical and judgemental” of those who feel it is playing a part in their illness as you feel that statement challenges the validity of “the” illness. You make them just as hesitant to share their illness because of not having understanding or sympathy. They are in the boat with us…..it’s real…it is true for them.
Over the years, I have found that we all are in different places with our knowledge of our body and how it works. We research in a certain direction and try to understand parts of our anatomy. (Doctors become specialist, because the body is so grand.) We can’t possible understand everything. But the more I learn, the more pieces fit together to make up the picture of our wonderfully created body. I also realize, that something someone told me in the past that I didn’t completely agree with or grasp what they were trying to tell me—now, makes sense. It’s a learning process and I try to understand and entertain the possibility that I don’t have the whole picture and allow for different exploration.
Issie
Well put Issie. The intergenerational concept is wild and there was a time I’d have totally “poo pooed” that idea but I’ve been listening to stories of kids who have lived before and there’s just no way they could know what they do about the past person’s life. The doctor studying these cases thinks somehow the energy of the person who has passed gets transferred to the child, so maybe something like that could happening here. I realized it was pretty arrogant of me to think there was nothing beyond what we humans can see/understand. I think it’s great that Christian, Veronique etc can discuss with respect this polarizing issue.
How about a name change from ME/CFS/SEID to Naviaux’s Disease?! Very exciting research
YES!!!! A great idea, and I completely agree! (Assuming the follow-up study replicates these findings, of course …)
Dr. Hanson already did confirm the core findings
Really interesting- thanks Cort for this and everything you do in bringing the latest research to our attention. I was discussing with a GP this weekend about diagnostic tests for CFS; the difficulties of the multiple presentations and varied aetiology of the condition and the need to understand what was homogenous about CFS.
It’s always seemed to me that as well as seeing CFS as caused by one, or a number of, vectors- and so focus on the vectors- we need to widen our focus to see it as a physiological response process within the body to those vectors. These findings really highlight some fascinating opportunities for understanding what’s going on at a metabolic and sub-cellular level.
Cort, I wonder if you might write an article for us on mitochondria? I gathered from Dr. Naviaux that they are not only the cells energy system/conveyors, but also that they are needed to turn genes off and on to deal with all kinds of physiological purposes. I find I really want to know more about what it means physically when the mitochondria are “stuck on idle”. I understand that the research isn’t in yet on just what is happening in ME/CFS or FM, etc., but at least if we can start to learn more about the mitochondria and their many roles, we could be farther along in understanding.
Cort, I forgot to say once again, thank you!!
i to have cfs and fibro starting on my 5th year seems like a lifetime of suffering i hope and pray this is a major breakthrough for all of us with this awful disease i hope this opens a breakthrough thanks cort
Just got this in my email. All I can say is WOW!!!!!
http://relief.news/adenosine-a-molecule-that-causes-and-relieves-pain/
Issie
Washington Post publishes article on the study – https://www.washingtonpost.com/news/to-your-health/wp/2016/09/06/chronic-fatigue-syndrome-may-be-a-human-version-of-hibernation/
So pretty much what I am doing right now for my CFS by optimizing my MFTHR pathways. I would had L-citrulline to that list. It works on the Nitric Oxide pathway. I take 3g of it everyday with a 70% improvement.
I just ran across another blog giving a little more clarification of what these researchers have found with the dysfunction. They are connecting it to issues with citric acid pathways and B vitamin pathways. I know the B vitamin pathways has to do with methylation based on reference to folate and B 12. But didn’t realize the citric acid cycle and it’s connection to Biotin.
It just may be that we correct the dysfunction of basic metabolism, the gut (where most of the immune system stems from), diet to tweak our immune system and getting down inflammation…….could we be at least made better. Hoping so!
http://www.meaction.net/2016/06/04/ron-davis-errors-metabolism/
Issie
Me too!
Wow. Took a while to get the end of comment line. ? Lots of interet in this article.
My view is that we should not assume the response is maladaptive. It could be protecting us.
Like slowing down a autoimmune reponse just enough to keep us alive.
Many people have recovered with Rituximab. Which seems to indicate that ince the autoimmune reponse is off, many feel normal or almost. Some in full remission.
http://www.mdwithme/blogspot.com April 27, 2013 is where I found the videos of Dr. Paul Cheney speaking about his research and findings, which are so in line with the thrust of Dr. Naviaux’s study and findings. His findings from studying the heart and circulation patterns in his patients with ME/CFS show this illness to be a down-regulated, protective state too. He describes here the abnormalities in the heart function and how they are related to hypotension, weakness, problems with liver detoxification as well as poor circulation to the brain. Dr. Cheney was ahead of the pack and still may be, so for those interested in what is going on with this down-regulated state, I would recommend a look back into Dr. Cheney’s work!
http://www.ctvnews.ca/health/stigmatized-chronic-fatigue-syndrome-sufferers-seek-recognition-1.3067130 The doc in the vid basically echoed the Naviaux scenario.
Such a great write up & such a great study. thank you so much for explaining this all so well.
I do just want to ask you if you would consider rethinking your inclusion of Autism as a ‘disease’ – when you talk about Naviaux’s research into “other diseases such as autism depression…” etc
Many Autistic people would find such a representation of themselves painful or even offensive. see here… http://www.independent.co.uk/life-style/health-and-families/autistic-pride-day-2016-why-we-are-proud-to-have-autism-neurotypical-a7085066.html
And I feel as members of a group of people containing some of the most misunderstood & abused people in the world, we ME/CFS sufferers & our advocates need to endeavor to be sensitive to other misunderstood & minority groups of people, & seek to understand them and their issues in the same way we wish people would learn about us.
Just a thought.
Thanks for your comment and suggestion. How should autism be referred to?
What happened to Suramin? After that tiny but succcessful sudy with 5 lucky kids with some autism, I thought we were next in line for a trial; did Naviaux submit a request for a grant to the NIH ubut get turned down?