

Many voxel based brain studies have been done in fibromyalgia. These studies, which measure brain volume, have found reductions in gray matter (the stuff that makes up the neurons) in many brain regions including the frontal, cingulate, insular and motor cortices plus the hippocampus, amygdala, brainstem and others. Plus, studies have also found increased volume in the frontal cortex (again!), the somatosensory cortex, nucleus accumbens, cerebellum and others. The findings, however, have been inconsistent. One study might find problems with the amygdala, while another finds issues in the motor cortex.
Researchers chalk those differences up to small sample sizes, heterogeneous patients, differences in age, disease duration or disease severity, etc. The point is that we really don’t know which abnormalities in brain volume we can trust.
Enter the Chinese researchers. By doing a meta-analysis of all brain imaging studies they hoped to give us a good foundation to stand on, regarding what’s going on with FM and brain volume.
Gray matter abnormalities associated with fibromyalgia: A meta-analysis of voxel-based morphometric studies. HaiCun Shi,MD1,a, CongHuYuan,MDb,1, ZhenYuDai, MDc, HaiRongMa, MD, LiQin Sheng,MD. Seminars in Arthritis and Rheumatism 46 (2016 )330–337
Their final analysis ended up containing 8 studies with 10 datasets containing some 300 FM patients and controls.
It indicated that decreased gray matter was reliably found in four areas: from anterior cingulate cortex (ACC) to the paracingulate cortex and medial prefrontal cortex (mPFc); from the bilateral posterior cingulate cortex (PCC) to the paracingulate cortex; from the left parahippocampal gyrus to the fusiform cortex, and from the right parahippocampal gyrus to the hippocampus (BAs 28 and 35; Fig. 2D). Increased GM was also seen in the left cerebellum.
That the anterior cingulate cortex popped out was surely no surprise. This area of the brain plays a critical role in pain regulation and decreased gray matter in the ACC is found in other chronic pain disorders. (That’s good news for FM patients looking for future treatments. The bigger the overlap between FM and other chronic pain disorders, the better chance a treatment will be found for both.)
One part of the ACC is devoted to the attention we give to pain and to the anxiety often associated with painful sensations. Another study suggests that people with fibromyalgia may have special problems with “anticipation”. Just about everyone in pain probably worries or anticipates that more pain is just around the corner. That’s a natural reaction, but that kind of anticipation surely sets the sympathetic nervous system (fight or flight) on edge, which, in turn, is associated with more pain.
One study found that FM patients don’t engage in pain anticipation more than other pain patients, but also suggested that FM patients’ brains may be more hard-wired to translate anticipation into pain. The study found equal amounts of anticipation in osteoarthritis and FM patients but increased activity of the insula in FM and increased levels of pain in response to a pain stimuli.
Given the increased rate of mood disorders found in FM, it’s perhaps not surprising to learn that gray matter reductions in one area of the ACC are highly associated with mood disorders.
A huge study analyzing 193 studies involving 16,000 patients with mental illnesses (depression, anxiety, schizophrenia, etc.) surprisingly indicated that portions of the brain (anterior cingulate, insula) associated with information processing and executive decision-making (not emotional issues) were common to all mental illnesses. These are the portions of the brain that involve attention, planning and decision-making and the ability to inhibit impulses. The authors of the study simply called them alarm bells in the brain that were not functioning well. It may be that in FM the alarm bells are not alerting the brain to problems with pain processing.
As people with FM know, FM is a complex disorder which causes much pain but which also affects cognition, mood and the senses, and that’s what the other analyses revealed.
Default Mode Network
Reduced gray matter was found in three areas of the default mode network (DMN). The DMN is a network in the brain associated with all sorts of activities including emotional processing, self-referential thought (day-dreaming), cognition and pain perception. DMN network problems have also been found in a variety of other disorders such as Alzheimer’s, anxiety, insomnia, depression, etc. That suggests that problems with the DMN may be associated in FM with poor sleep, cognition, and depression.
Increased Gray Matter in Cerebellum
Finally, the meta-analysis revealed increased gray matter in the cerebellum, a part of the brain associated with both sensory processing and movement. Other research has shown that the filters used to process and make sense of sensory information aren’t working properly in FM. FM patients’ brains appear to have trouble disengaging from innocuous background noises as well.
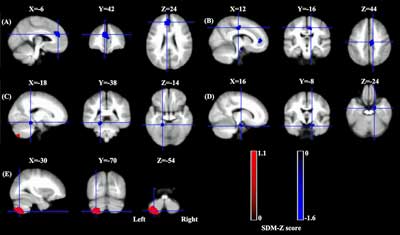
Grey matter results showing reduced volumes in some sections of fibromyalgia patients’ brains and increased volumes in others
All this points to the sensimotor regions of the brain scrambling to keep up with what may be torrents of sensory information hitting it. That could show up in people with FM having difficulty tolerating and being more fatigued in higher stimuli environments – something that clearly happens.
There is growing recognition of the importance that sensory problems play in FM. They help to make FM the complex disease that it is and differentiate it from some other chronic pain states. A recent MRI study examining brain activation associated with both pain and non-painful stimuli produced a brain signature with both high specificity (got the healthy controls right) and sensitivity (got the FM patients right). That suggests that the sensory problems in FM must be taken into account.
Treatment Implications
Gray matter is just one of the issues researchers have found in FM patients’ central nervous systems. At least four central nervous system problems are contributing to the pain and other problems in FM; windup and central sensitization in the spinal cord, gray matter losses, problems with blood flow and brain activation, and connectivity issues between different parts of the brain.
It’s not clear why these gray matter losses are occurring. They could be due to cell loss or the loss of nerve synapses or they may simply be caused by decreases in cell size or blood volume. They could also, at least in part, be simply the result of being in chronic pain, and that’s the good news. It turns out that even acute, temporary pain is associated with a degree of gray matter loss – which is reversible once the pain problems are resolved.
Problems in the ACC may help explain why CBT and other behavioral therapies can help in reducing the suffering, anxiety and to some degree the pain in FM. Developing effective brain stimulation techniques that target the ACC and other areas is an ongoing project.
Acupuncture doesn’t work for everyone, but an interesting study found that not only did it reduce pain but brain imaging indicated that it had actually reduced activity in different parts of the brain.
Alternative means such as acupuncture can be helpful. A recent Cochrane review found consistently positive results for tai chi, yoga, meditation and mindfulness-based interventions, hypnosis or guided imagery, electromyogram (EMG) biofeedback, and balneotherapy/hydrotherapy in FM. Inconsistent results were reported for qigong, acupuncture, chiropractic interventions, electroencephalogram (EEG) biofeedback, and nutritional supplements.
The multiple brain regions affected in FM suggest it’s a complex disease which will likely require multiple treatments for optimal effectiveness. Some treatment trials have begun to combine treatments in novel ways. Several studies are now combining FM drugs with CBT and other behavioral therapies to see if one therapy can help boost the other. Going a step further combining brain or vagal stimulating techniques with drugs, supplements or behavioral therapies such as CBT, meditation and/or neurofeedback would make sense.
The newest approach to pain, though, could eventually make drugs obsolete. Next up we look at a brand new approach to treatment being undertaken in the NIH’s SPARC project and what it might mean for FM.
As the brain scan data keeps rolling in – and we know it will in FM – ultimately researchers and doctors should be able to identify subsets and target treatments using them.






Very interesting, Cort. This article is somewhat related. I found it on a fed up with fibromyalgia blog.
It begins with: University of Colorado Boulder researchers have discovered a brain signature that identifies fibromyalgia sufferers with 93 percent accuracy, a potential breakthrough for future clinical diagnosis and treatment of the highly prevalent condition
http://www.chaffeecountytimes.com/free_content/neural-signature-for-fibromyalgia-may-aid-diagnosis-treatment/article_3f62712e-c7d7-11e6-976e-2f208ae9ed09.html
Great study! I actually linked to it in the blog. It’s the one that had high specificity and sensitivity. They combined pain processing areas and non-painful sensory processing in the areas in the brain to do that. That’s clearly important because FM is more than a pain disease.
Things are definitely moving forward in the brain scanning research in FM.
The brain, mind and the body are linked. The brain IS part of the body. When I read about these studies I can’t help but think about the research that intractable pain specialist, Dr. Forest Tennant has done which shows how destructive ANY long term pain is to the brain. Is it not conceivable that FM is (at least partially) a feedback loop, reinforcing itself? Of course if one has pain, one worries (about keeping a job, dealing with life, how it will affect relationships, getting treatment, being able to sleep through the night and more) and perhaps that further augments the pain–and the cycle continues–and the brain ‘shrivels’ and psychiatric diagnosises are made…
And the question is how or where to break the chain…
The Lightning Process teaches you how to break the chain. I did the training and it worked for me and the other people on my training also.
Congratulations Lucinda. How would you say you are doing now? With regards to pain (or any other symptoms) on a scale of 1-10 how is it now and how was it then?
Lucinda would you kindly let me know where I may find out about the Lightening Process. I have had FM since 1999 and would be really grateful if you could let me know. Many thanks Marianne
Good point. Dr. Martinez-Lavin believes FM is a disease in which stress causes distress and an activated sympathetic nervous system (fight and flight) is key.
Hi it’s all linked in with hormones as all part and parcel of one thing but many Quacks try to compartmentalise the body it don’t work.
Just like a car can have a pile of parts in garage bits everywhere but till it’s put together as one it’s just scrap!
We are just the same as have to consider everything not just one part to get an accurate view of the matter plus everyone is different in genetic make up so you can have a core issue but so many other things round it are different for everyone.
why you have a list of symptoms which some will have this others that and some all of them.
But we are like a cake! with plain flour/self raising.eggs more/less or none.sugar more/less plus brown.fruits.baking soda.and a whole list of ingredients in various amounts etc
but once baked all a cake unless cooked wrong then always an issue.
So all varied ingredients and recipes to get there but all a cake in the end.
Funny thing was i found a thing with hormones helped mine as changed it some things came back quickly others stayed away for long while but also it changed many of the problems i had inc the way i felt with brain!
It is quite an awful illness but also very interesting to study it’s in my family
It is interesting that you should mention how hormones have helped stabilize your moods. I noticed the same thing myself. After trying many antidepressants, my ‘mood disorders’ vanished when my hormones got ‘straightened’ out. And Dr. Tennant, as I mentioned before, also emphasizes hormone testing for all chronic pain patients. (And taking opioids also can also deplete the body’s hormone balance).
Unfortunately, the fatigue remains… which is why I am always visiting this site to glean more information from this corner of research (I’m an EDS girl).
Cort, thank you for all your efforts! I have forwarded many of your reports to the EDS community.
Hi i tried one called Zoely as researched into many things about how fibro type things work/manifest themselves plus other things around it and interface with it etc
Plus way the body changes with effects of it.
Tried it for 2 weeks noticed changes pretty quickly like could walk far better instead of like a pair of flipper my gait improved walked a fair way felt tired later but not in the same way i also lost pain in base of spine water works improved lost that urge ibs was more in the middle/work in progress as need to study that more!felt far better pains was far less like hands was cold but not painful slept far better actually go through the night lost that keep waking up every 5/10/15/20 mins etc thing i got.brain was better in felt more clearer with thought process so many things improved with it it also brought my T levels up from 7 to 11 when went to Endo which just dismissed my findings.
Yet they put me on T hrt which caused lots of issues apart from being back in pain ended up having a TIA/mild stroke type thing from it as my BP went through roof! plus all the pressure point pains was high ho plus got breast growth!
but they was like could only think in there little box it was this and can only be this! but we are all so varied they give you things without looking at the basics as speaking to a lady at RLHIM she has very high T levels yet has children and if took her E levels high would probably cause her many issues?
Also know males with very high E yet they live ok like it and if gave them lots of T would probably become very ill.
So they have to find whats right for us not whats right for there box on there pc’s
As it’s all part and parcel of a chain all inter linked between each other with one part supporting another so take too much away from one area causes another to go wrong which starts a chain event.
Being that im under the Autism umbrella they found having Asperger’s i can see/sort/go through things quickly working things out how/why/where etc as can read between the lines on things
I had to look up Zoely and discovered it is a birth control pill available in the U.K. I am way past birth control pills, but do echo your complaint that often ‘ranges’ used to access whether someone is in the ‘normal’ or ‘not’ spectrum, can be problematic. The question is, what is ‘normal’ or rather optimal for you? That is why I think more and more patients are seeking ‘functional medical doctors’ for treatment, rather than the standard allopathic model.
It is unfortunate that in order to access ‘health care’ one has to pass through the gates of ‘insurance company regulations’ which are often guided by the profit motive. It just takes too much time to niggle around adjusting doses and trying various treatments, especially when doctors often have 15 minute appointment slots.
That’s why research (especially on these underserved conditions such as CFS/ME/SEID and Fibromyalgia) is so important. If doctors are not allowed to practice the time consuming ‘art of medicine’ at least research can guide them towards therapies that work.
And hopefully, with genetics, medicine will eventually evolve into personalized, individualized treatment.
Hi yes it is but it’s a natural type E being 17B not the very synthetic type which causes issues.
The funny thing is which Quacks didn’t/couldn’t grasp is if take E&P together in males the progesterone cancels the feminising effects out on us but increases the T(why they say not to take together when going M2F TG)
My way i worked out was it sort of rebalances/kick starts system bit like a reset! bit like when they give to a vaccine!
Did have an interesting chat with a lady who is part of a research course into shaped genetic medicine stating similar to what your saying so shaped/aimed at each person rather than generic/mass.
but yes USA side is a mess with Med.co involved you have great research into Fibro etc years ahead of the UK but your treatments are lagging far behind once get to that level as yes insurance (Robbery without a mask)is the size 12 boot in the works!
so once there involved in anything it all goes wrong!
I did contact MSD who market Zoely about my findings as im sure a short dose would help esp males in rebuilding there system back up
I wonder how it relates to the previous study about enterovirus and brain damage for CFS/ME patients? And is there a relationship to Gulf War Syndrome which has symptom overlap?
Canvas Memantine fix this?!
I believe that Memantine may be able to reduce neuroinflammation and microglial activation. If inflammation is contributing to the gray matter loss in FM then it or another anti-inflammatory that’s able to effect the brain could help out. I know that gray matter loss sounds scary but I want to point out that studies thus far suggest that the gray matter loss present is reversible.
Thank you for your answer. On January 18, I will meet with Sweden’s foremost neurologist and then I will take up the studies I found on Memantine for thus justifying my proposal that I want to try Memantine. I will also ask to try the medical plastic Qutenza (capsaicin – Substance P) against my allodynia underfoot, which is difficult to live with, despite Cymbalta. I have developed a comprehensive basis, perhaps added 40 hours to put me into it and write me. Overall, I have put about 4,000 hours over two years to try to understand everything about Fibromyalgia.
Daniel, may I ask about the pain you have underfoot? How did it start and is it in the arch?
Thx for your info. I’m very new but ecstatic at finding this blog. Particularly interested in Qutenza. I’m also trying to find a ” biological MD” who can find everything in your body.
I have peripheral neuropathy & 1 of my MDs thinks I have an “longstanding Lyme disease” but keep getting herxheimer reactions to the smallest dose & to Samento also!
Yes my ENDO would only test TSH & free T3 T4 & in normal range. However complementary & alt MDs use much smaller NL ranges.
The most well known MD for thyroid, FM, etc in my area is extremely arrogant & expensive & insurance doesn’t pay.
Thx for all the research you’ve done.
https://www.youtube.com/watch?v=Eo_0U34n2qc
Mood disorders are glial disorders
Interesting,
Other braing studies have demonstrated very similar neurological abnormalities in tsp/ham( htlv1 retrovirus associated melopathy, also hiv have show similar neurologicals abnormalities, not thesame but similar, i wonder why NIH don’t look at this possibility, especially knowing that most mecfs have also major immune deficiency.